Abstract
Purpose
Full-thickness cartilage defects if left alone would increase the risk of osteoarthritis (OA) with severe associated pain and functional disability. Articular cartilage defect may result from direct trauma or chronic degeneration. The capability of the mesenchymal stem cells (MSCs) to repair and regenerate cartilage has been widely investigated. This review describes current trends in MSC biology, the sourcing, expansion, application and role of MSCs in chondral defects of human knees.
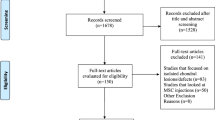
Methods
The studies referencing MSCs and knee osteoarthritis were searched (from1998 to 2020) using PubMed, EMBASE, Cochrane Library, Web of Science and the ClinicalTrials.gov with keywords (MSCs, chondral defects or cartilage degeneration of knee, cartilage regeneration, chondrogenesis, tissue engineering, efficacy and safety). The inclusion criteria were based on use of MSCs for treatment of chondral defects and osteoarthritis of the knee, English language and human studies.
Results
The history of MSC research from the initial discovery of their multipotency to the more recent recognition of their role in cartilage defects of knee is elucidated. Several studies have demonstrated promising results in the clinical application for repair of chondral defects as an adjuvant or independent procedure. Intra-articular MSCs provide improvements in pain and function in knee osteoarthritis at short-term follow-up in many studies. The tendency of MSCs to differentiate into fibrocartilage affecting the outcome is a common issue faced by researchers.
Conclusion
Some efficacy has been shown of MSCs for cartilage repair in osteoarthritis; however, the evidence of efficacy of intra-articular MSCs on both clinical outcomes and cartilage repair remains limited. Despite the high quality of evidence to support, MSC therapy has emerged but further refinement of methodology will be necessary to support its routine clinical use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cartilage of each human joint is a highly specialized tissue acting as a shock absorber, enabling synovial joints to articulate with low frictional forces. It has limited repair potential since it is not vascular, nor it has lymphatics and is largely aneural [1]. Full-thickness cartilage defects if left alone would increase the risk of osteoarthritis (OA) with severe associated pain and functional disability. The capability of the mesenchymal stem cells (MSCs) to repair and regenerate various mesenchymal tissues in the human body has been widely researched including cartilage defect regeneration [2,3,4,5,6]. Over the past decade, an increase in the use of biological agents, including cell-based therapies, was applied in the sports medicine community with cartilage injuries.
The current methods for articular cartilage (AC) repair include non-surgical and surgical alternatives. A wide range of surgical approaches are being practiced. The spectrum includes use of arthroscopy with microfracture and microdrilling, soft tissue grafting, osteochondral transplantation and autologous chondrocyte implantation (ACI) [7,8,9]. Brittberg [10] first transplanted patients own chondrocytes into the articular defect site of a knee. AC is a tenacious and tensile load-bearing connective tissue that covers the surface of joints. Studies have shown multiple issues faced by the application of chondrocytes, i.e., donor site morbidity, generating insufficient chondrocytes, low cell density of native cartilage, slow cell growth, etc. [11, 12].
AC defect may result from one of the following mechanisms: (1) trauma (direct or indirect); (2) mechanical overloaded (chronic degeneration); and (3) subchondral bone changes (osteochondritis dissecans, avascular necrosis). The potential for spontaneous regeneration of the cartilage is low. The cartilage breakdown occurs due to production of redundant proteolytic enzymes. The inflamed synovium produces catabolic and proinflammatory factors (prostaglandin E2, Nitric Oxide) which alter the equilibrium of cartilage matrix metabolism [13]. The subchondral bone plays an important role in healing of profound defects through the presence of mesenchymal elements. These elements proliferate to form a connective tissue of fibrous nature, which gradually differentiates into a lower-quality fibrocartilage. This is a valid reason for the ongoing research for healing of articular surface defects with hyaline cartilage (normal cartilage of joints). The repair of damaged cartilage may be achieved through transplantation of cells (chondrocytes, mesenchymal stem cells) and tissue engineering [14].
Tissue engineering science has progressed in the last decade. Successful tissue engineering in articular cartilage repair has four components: (1) Specific cell types which can proliferate, differentiate and maintain the phenotypic properties; (2) a scaffold to provide an adequate 3-dimensional environment for the cells to grow; (3) addition of appropriate chemical factors such as growth factors, cytokines or hormones as a suitable stimulus for specific lineage differentiation of the cells; and (4) cells require a microenvironment (physical and biochemical factors to regulate MSC behavior) which withstands the mechanical and biochemical state of the joints [15].
Role of Mesenchymal Stem Cells (MSCs)
Stem cells have the potential for self-renewal and differentiation into multiple cell lines. Stem cells are classified into three main categories: embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs) and adult or somatic stem cells [16]. Adult stem cells may be derived from bone marrow, adipose tissue (fat), muscle, placenta, umbilical cord, synovial membrane, tendons and cartilage. The worldwide current practice is to use the acronym, MSC, for both cell populations, i.e., mesenchymal stromal cells and mesenchymal stem cells [17].
MSCs are the most representative adult stem cells and can be induced to differentiate into different mesenchymal lineages such as bone, cartilage, fat, ligament, tendon, and other connective tissues. Stem cells secrete mediators that promote endogenous growth, stimulate self-proliferation of progenitor cells, and inhibit chondrocyte apoptosis or cartilage degeneration, promote angiogenesis and decrease oxidative stress through regulating TGF-β, VEGF, ADAMTSs MMPs, TIMPs achieving cartilage regeneration and cartilage protection [18].
The majority of the studies used bone marrow-derived MSCs (63%) followed by adipose tissue (33%) [19]. Bone marrow-derived stem cells (BM-MSCs), adipose stem cells (ASCs) and induced pluripotent stem cells (iPSCs) are promising stem cell sources which have many advantages for clinical applications due to their chondrogenic potential. BMSCs may allow better differentiation of the deep calcified articular cartilage zone adjacent to healthy bone [20]. Thirty-one published studies by 15 different groups looked at clinical applications of MSCs. One used allogenic stem cells and the rest autologous stem cells [19]. A recent report which evaluated the clinical outcomes for ACI and MSC therapies during 10-year follow-up demonstrated that MSC implantation appears to be equivalent to ACI with no apparent increased tumor formation risk [21]. In another study, autologous MSC therapies are safe and may have the potential to prevent progression of OA Knees [22].
It was observed that BM-MSCs had superior chondrogenic differentiation capacity as compared to MSCs from other origins [23]. Pellet culture system and chondrogenic medium containing TGF-β1 were used to induce chondrogenic differentiation. It is postulated that the stimulus for cartilage regeneration is induced by paracrine effect of cells transplanted on the damaged host joints [24]. When cultured in vitro without the presence of regulatory cues, MSCs often behave and function differently. In vivo studies show that the regenerated cartilage is similar to fibrocartilage with inferior mechanical properties, healing capacity and requires sufficient cell numbers with chondrogenic potential [25]. These limitations could be circumvented by use of iPSCs [26]. iPSCs could be committed to the chondrogenic lineage in high-density pellet culture systems, enhanced by the addition of growth factors from the TGF-β superfamily or seeding iPSCs into scaffolds [27]. iPSCs can proliferate indefinitely and support chondrogenesis both in vitro and in vivo. Using a defined quality control process and a chondrogenic differentiation protocol, hiPSCs (human induced pluripotent stem cell) may be the ideal cell source for cartilage tissue engineering [28]. But patient-specific autologous hiPSC generation and transplantation is expensive.
Enhancing Chondrogenesis
MSC Harvest, Isolation and Scaling-up
In studies using bone marrow concentrate, approximately 60 ml of bone marrow aspirate was harvested and concentrated down to a volume of 2–4 ml before use [29,30,31,32]. BM-MSCs isolated from a 2-ml bone marrow aspirate can be expanded 500 times in approximately 3 weeks. These cells can retain their pluripotency for at least further 6–10 passages in culture [32].
Density gradient centrifugation is used to obtain mononuclear (MNC) fraction of cells from bone marrow aspirate. The collected cell fractions are washed and rinsed followed by plastic adherent plating of cells. This will enable removal of non-adherent cells and allow for MSC cell growth [29]. Nowadays, fluorescent or magnetic activated cell sorting is available for generating more pure population of MSC [29]. For achieving high clinical efficacy, the estimated dosage of MSCs required is approximately 40 to 100 × 106 cells per patient [31]. Therefore, ex vivo cell expansion is a key step in the development process [33,34,35].
Mesenchymal stem cell expansion can be induced by bioreactors of two kinds, i.e., static planar system or dynamic systems. The static planar systems are easy to transfer from laboratory level. It is labor intensive and requires large physical space [34]. Dynamic bioreactor systems for large-scale expansion of cells are of two types: (a) medium recirculation reactors in which cells remain attached to solid substrate rendering them static while the growth medium flows through the cells supplying nutrients and oxygen; (b) suspended micro-carrier (MC)-based reactors (such as stirred tank) in which cells grow on small particles (micro-carriers) suspended in the growth medium by stirring [35, 36]. MC-based stirred bioreactors are necessary to generate large amounts of clinical-grade MSC. MC-based stirred bioreactors provide large surface area per unit volume. This helps in process monitoring and control of nutrients and gaseous diffusion that makes the bioreactor culture attractive [35, 36]. MSCs harvested from expansion systems can be delivered to the site of the damaged cartilage by two methods. The methods are (a) cells mixed with gel glue (sealant-based) or (b) embedded on biocompatible scaffolds (scaffold-based) [37]. Implantation of TEC (tissue-engineered construct) could potentially yield more long-term safety and efficacy due to the scaffold-free nature of their in vitro generated structure [37, 38].
Cell Seeding
Healthy AC naturally contains 9.6 × 106 chondrocytes/cm2 [39]. It has been reported in clinical studies that scaffolds seeded with 5 × 106 cells per scaffold induced the highest chondrogenesis [39, 40]; chondrogenesis appeared to be most pronounced with seeding densities of 5–10 × 106 BMSCs/cm3 and 50 × 106 BMNCs/cm3 for 2D and 3D expansion protocols, respectively [41]. Yokoyama et al. [42] reported that a MSC density of 5 × 107 or 5 × 108 cells/ml embedded in a collagen gel had more proteoglycans than lower cell densities, better facilitating chondral defect healing and supporting the need to identify a MSC source with a high proliferation potential.
Growth Factors
The most potent chondrogenic differentiation inducers are transforming growth factor-β, bone morphogenic protein, fibroblast growth factor, and insulin-like growth factor-1 [4, 43, 44]. The induction process can be enhanced by steroids. Thirty-two studies (29%) assessed the effect of growth factors on MSC chondrogenesis. Seventeen out of 38 (44%) used TGF-β1/3, the majority of which show a positive effect on chondrogenesis [19].
Stem Cell Implantation
Sealant Based
Most common sealant gels are collagen and fibrin having gluing properties and are biodegradable. Sealants may be natural or synthetic. Natural ones include collagen, gelatin, alginate, chitosan, chondroitin sulfate, agarose, hyaluronic acid (HA) and silk [45]. They are biodegradable, biocompatible and reduced immunogenicity. Synthetic ones are polyethylene glycol (PEG), polyurethane (PU) and polyester which are biocompatible, strong adhesive and biodegradable. In the last 5 years, phase III trial in the USA is carried out using CARTISTEM® from Medipost Co Ltd (human umbilical cord blood-derived MSCs with hyaluronic acid hydrogel) in which cell treatment is done together with microdrilling at arthroscopy [36].
Scaffold Based
A scaffold is commonly used to facilitate in vitro chondrogenesis for tissue engineering. Some characteristics of ideal scaffold have been suggested such as having similar characteristics to the native tissue, being a source of cells that could promote tissue regeneration, highly porous to permit cells penetration and tissue impregnation, high permeability for allowing delivery of nutrients and gas exchange, biocompatible and biodegradable once the functional tissue has been formed. Biodegradable polymers can be natural or synthetic. Natural biodegradable polymers are polynucleotides, polysaccharides and proteins, whereas synthetic biodegradable polymers include poly-lactic acid (PLA), poly-glycolic acid (PGA) and poly-lactic-co-glycolic acid (PLGA) [46]. Scaffolds are derived from animals; thereby, the risk of disease transmission and immune reaction increases.
Scaffold-based MSC constructs have their advantages and disadvantages in the treatment of full thickness cartilage defects. The advantage is that they are capable of withstanding the in vivo loading environment and protect the embedded cells within from any mechanical stresses [47]. Disadvantages are leakage of cells, poor cell survival, poor cell differentiation, inadequate integration into the host tissue, incorrect distribution of cells and dedifferentiation of the normal cartilage. The new improved scaffolds are being developed, e.g., PCL microcarriers and modified PLGA scaffold showing many possible advantages [36]. Composite materials for tissue engineering scaffolds are being made of combination of biodegradable polymers and bioactive ceramics [48].
A systematic review observed 53 in vitro studies; natural scaffold (26), synthetic scaffolds (9) and hybrids (18). They found the most popular being a fibrin-polyurethane scaffold [19].
Scaffold Free 3D Culture
Before the emergence of scaffolds, scaffold-free 3D culture systems were generally used for chondrogenesis. The popular methods used for cell-based therapy are pellet culture and micromass culture. The distribution, density and matrix composition of cells in pellet culture are similar to native AC [49]. High-density micromass culture induces cell–cell interaction aggregating into a high-density pre-cartilaginous core [50].
Some studies have shown that human serum culture medium has the potential to increase MSC proliferation without the disease transmission or immune reaction risk of an animal source [51].
Intra-articular Delivery of MSCs (Clinical Trials)
The method used to deliver MSCs to an articular defect is highly technical. The objective of surgical implantation is to create a 3-D environment that optimizes cell proliferation and differentiation.
Intra-articular Injection (Cell Therapy)
The easy and less invasive implantation method might be intra-articular MSCs injection. Centeno et al. [52] reported for the first time a case showing promising functional outcome after injection of expanded autologous MSCs in a knee joint. MRI confirmed an increase in cartilage and meniscus volume. But they could not determine the nature of regenerative tissue, i.e., fibrocartilage or true hyaline. Later researchers used MRI T2 mapping to define the nature of regenerative tissue [53]. Davatchi et al. [54] demonstrated no complications following injection of cultured BM-MSC and reported good outcomes (improved pain and function) of the four patients complaining of Grade III to IV bilateral knee OA. Following their report on six patients injected with BM-MSC, Emadedin et al. [55] observed that BM-MSC injection would be effective for 6 months. Complete cartilage coverage has been reported in nine patients in the cell-recipient group in a double-blind randomized trial [56]. However, the injected MSCs adhered to synovial tissues may increase the risk of synovial proliferation. In addition, cellular adhesion to synovial tissue may result in less cellular adherence to the chondral defects. The development of minimal invasive technique of MSC delivery system is now investigated for the use of cells coupled with magnetic beads in association with an external magnetic force to direct the cells to the desired location, i.e., chondral lesion [57, 58].
Early clinical data suggest bone marrow aspirate concentrate (BMAC) may help stimulate a hyaline cartilage repair through both chondrocyte differentiation of MSCs and paracrine functions [59]. Soler et al. [60] obtained excellent clinical and quantitative MRI outcome measures with no adverse events after intra-articular injection of 40 × 106 of autologous expanded BM-MSCs. Lamo-Espinosa et al. [61] concluded that single intra-articular injection of 100 × 106 in vitro expanded autologous BM-MSCs together with hyaluronic acid is a safe and feasible procedure that would result into a clinical and functional improvement for knee OA. In another study, 18 patients had intra-articular injection of autologous MSCs for knee OA. The outcomes showed intra-articular knee injection of 100 × 106 autologous MSC improved function and pain as well as healing of cartilage defects by regeneration of hyaline-like articular cartilage [62].
One study compared the use of MSCs obtained from peripheral blood with MSCs obtained from bone marrow for treatment of large (> 4 cm2) osteochondral lesions. The BMAC was combined with a collagen membrane. Significant improvement with good outcomes was reported in 86% [63].
In a systematic review, the age range of patients with chondral lesions in the knee was investigated for BMAC injection treatment [64]. Out of 11 studies, eight focused on the treatment of focal chondral defects. All eight studies evaluated BMAC in combination with or without microfracture or as isolated treatment compared to ACI. The patient age in these eight studies ranged between 17 and 58 years [8, 29, 63, 65].
Recently following a systematic review of 17 studies, the evidence of efficacy of intra-articular MSCs on both clinical outcomes and cartilage repair remains limited. All but two studies reported significantly better clinical outcomes in the MSC group. Therefore, some efficacy of MSCs for cartilage repair in OA was shown [66]. Although many authors suggested the good outcome with injectable treatment, current evidence does not support the use of intra-articular MSCs for improving cartilage repair in knee OA [67].
The safety of MSCs has been in question. The most common complications reported were swelling (92%) and pain (41.3%) [68]. Centeno et al. [52] reported joint swelling and pain in 5.3% patients, while Gobbi et al. [65] reported two patients with joint stiffness.
The contradictory evidence of injection treatment suggests that scaffolds may be required for the regeneration of cartilage and could act as a cell carrier.
Surgical Implantation (Cell Scaffold Combination)
Kuroda et al. [69] first assessed the effectiveness of autologous MSC, embedded within a collagen polymer, to repair a full-thickness articular cartilage defect (20 × 30 mm) in the medial femoral condyle of a 31-year-old athlete. The implant was covered with an autologous periosteal flap. After a year, a hyaline-like cartilage tissue had formed on histological examination. The clinical symptoms had improved significantly and attained his previous activity level. Wakitani et al. [39, 70] presented their results after the treatment of nine cartilage defects (patella femoral joints) in three patients. They introduced BM-MSCs on collagen gel covered with periosteum in one case and synovium in the other two cases. Clinical improvement was reported at 7–21 months. In five patients with isolated patellofemoral joint chondral defects treated with MSCs, decreased pain and improved walking ability at 6 months were reported to last long. de Windt [71] reported one surgery two cell technique (combined allogenic MSC with recycled autologous chondrocytes and native pericellular matrix) in knees with OA. At 12 months, all the patients (10 patients with age between 18 and 45 years) showed significant good functional outcome. Histological analysis indicated hyaline-like cartilage with a high concentration of proteoglycans and type II collagen. Akgun et al. [72] compared the outcomes of matrix-induced autologous chondrocyte implantation (m-ACI) with matrix-induced autologous mesenchymal stem cell implantation (m-AMI). They randomized 14 patients with isolated full-thickness cartilage defects of the knee of > 2 cm2. At two-year follow-up, patients with m-AMI were observed to have significantly better functional outcome than patients with m-ACI (p < 0.05). Kim et al. [73] retrospectively evaluated 54 patients (56 knees) with second-look arthroscopy following MSC implantation for chondral defects in OA knees. A total of 37 patients (39 knees) were treated with MSC implantation without a scaffold (group 1), and 17 patients (17 knees) underwent MSCs implantation with fibrin glue as a scaffold (group 2). At final follow-up of 2–3 years, the mean IKDC score and Tegner activity scale in both groups improved significantly.
Nejadnik et al. [74] reported BM-MSC transplantation into 36 AC defects and followed up for 2 years comparing the results with those of 36 ACI. They concluded that BM-MSC transplantation showed outcome comparable to ACI. They suggested that BM-MSC transplantation was a good procedure because it required single surgery, reduced costs for patients, and minimized donor site morbidity. Emadedin et al.’s [75] triple-blind, placebo-controlled RCT demonstrated the safety and efficacy of a single intra-articular implantation of 40 × 106 autologous MSCs in 43 patients (mean age of 54 years) with knee OA (KL grades 2, 3 and 4). The procedure provided significant and clinically relevant pain relief over 6 months versus placebo. Gigante et al. [76] reported five patients with symptomatic medial femoral condylar defects of the knee who had arthroscopic microfracture and implanted a collagen type I scaffold seeded with BMAC in an attempt to augment the outcome of the autologous matrix induced chondrogenesis (AMIC) technique. At 12 months follow-up, clinically all these patients had significant functional improvement. Histological examination revealed hyaline-like matrix in one case, a mixture of hyaline/fibrocartilage in one case, and fibrocartilage in rest of three cases.
Nine patients with focal lesions of the knee were consecutively treated with arthroscopic microfractures (MFX) and autologous bone marrow concentrate (BMC) from the iliac crest immersed in a collagen membrane. Of the four patients consenting for 2nd look arthroscopy, hyaline-like cartilage was found in one knee [29]. Gobbi et al. [65] prospectively analyzed at five years, 50 (fifty) physically active patients (mean age, 45 years) with grade IV cartilage injury of the knee (lesion size, 1.5–24 cm2) who were treated with HA (hyaluronic acid)-BMAC or microfracture. The outcome scores were significantly improved in both groups at 2 years (p < 0.001). HA-BMAC implantation for cartilage repair can lead to successful medium-term outcomes independent of age or lesion size. Gobbi et al. [77] also observed hyaline-like cartilage in 80% of patients seen on magnetic resonance (MRI) imaging.
Buda et al. [78, 79] reported 20 patients with osteochondral lesions and associated other morbidities in the knee. All associated morbidities were repaired. Histology showed cartilaginous tissue containing predominantly type II and proteoglycan-rich matrix. Haleem et al. [80] reported five patients treated with MSCs transplanted on a scaffold of platelet-rich fibrin glue (PR-FG) for chondral defects of knees. All patients had successful outcome. They concluded that PR-FG may be an ideal MSC scaffold since platelets (secretory granules) contain both TGF-1 and IGF-1. Koh et al. [81] transplanted autologous MSCs to full-thick articular lesions in 37 knees of 35 OA patients and retrospectively evaluated the knees using second look arthroscopic surgery. 94% patients manifested good to excellent satisfaction. Wakitani et al. [82] in the longest follow-up of 10 years in patients with transplanted autologous BMSC reflected that this is a safe procedure without any tumor formation.
Goldberg et al. [19] in their systematic review observed that majority of studies (42%) used MSCs to treat knee osteoarthritis. Most commonly used outcome measures for treatment efficacy were radiological (77%) and arthroscopic assessment (61%).
A nonwoven 2 × 2 cm or 5 × 5 cm biodegradable hyaluronic acid-based scaffold for hyaline-like cartilage regeneration is used in an upcoming trial for the repair of AC in the knee in the USA (NCT02659215) [36].
A systematic review of 33 clinical studies investigates the use of BM-MSCs in knee cartilage repair. All studies together with 724 patients of mean age of 44.2 years were eligible. Approximately 50% of the patients received cultured BM-MSCs. All patients implanted with BM-MSCs had improvement in pain, function and histological regeneration. They suggested a guideline which includes study design, patient characteristics, BM-MSC characteristics, delivery technique and postoperative assessment [83]. Clinical studies with larger sample sizes and longer follow-up periods are required to test the effectiveness and safety of stem cells for cartilage repair [84]. In the last few years, the high quality of evidence to support MSC therapy has emerged, but further refinement of methodology will be necessary to support its routine clinical use [85].
Future Directions
MSC Exosomes
Exosomes are extracellular vesicles secreted through the fusion of multivesicular endosomes with the cell membrane. Recently, exosomes have been shown to play a leading role in the efficacy of MSC-based therapies in mediating tissue repair. MSC exosomes provide new perspectives for the development of cell-free and ready-to-use therapy for treatment of cartilage lesions and OA. Zhang et al. [86] first reported the effects of human embryonic MSC (EMSC) exosomes on cartilage repair. MSC exosome therapy has not been used in clinical trials.
Genetic Engineering
Gene transfer to cartilage defects can be achieved by either direct vector administration to cells located at or surrounding the defects, or by transplantation of genetically modified chondrogenic cells into the defect [87]. Despite promising results, for an effective gene-based therapy of cartilage defects many barriers need to be crossed before clinical translation in patients. The barriers include impaired gene transfer and expression in vivo. There may be presence of agents that may interfere with gene vector adsorption on cell targets [88]. Controlled release of gene therapy vectors through scaffold guided gene transfer systems may also allow to overcome the existing physiological barriers, but all these are in experimental phase [89].
Epigenetics
Epigenetic gene regulation commonly refers to a heritable and long-lasting process by which gene expression is handled at chromatin level without alterations in DNA sequence, i.e., post-genetic or non-genetic regulation [31, 90, 91]. The post-transcript modification can evenly affect the gene expression without changing the gene sequence. Epigenetic regulation of MSCs could be achieved through DNA methylation, histone modifications, chromatin remodeling or micro-RNA. These mechanisms are considered as epigenetic marks that allow coordinating transcription programs [31, 91]. The epigenetics of MSCs is an intriguing area of investigation holding great promise for both basic and applied researches in tissue engineering [91].
Summary
Cell-based therapies are emerging as a means to regenerate cartilage. One of the points to consider is the stability of the cells before use. However, there are still unknown mechanisms of tissue repair using MSCs; for instance, it is not yet known whether the transplanted MSCs directly fill the lesion and regenerate the defect in the AC or they indirectly stimulate through their paracrine functions. The tendency of MSCs to differentiate into fibrocartilage affecting the outcome is a common issue faced by researchers. The delivery of factors stimulating chondrogenesis and maintenance of the AC phenotype need to be more efficient than purely exogenous administration for regenerating a stable hyaline-rich cartilage. At present, MSC-based therapies are not suitable for regeneration of large cartilage lesions in severe OA patients and the criteria of optimal scaffold, cell dose, injected times and intervals are not definite.
The challenge for the future consists in addressing specific researches providing more insights into the MSC exosomes, genetic engineering and epigenetic regulatory mechanisms governing MSC biology.
References
Oldershaw, R. A. (2012). Cell sources for the regeneration of articular cartilage: the past, the horizon and the future. International Journal of Experimental Pathology, 93(6), 389–400.
Redman, S. N., Oldfield, S. F., & Archer, C. W. (2005). Current strategies for articular cartilage repair. European Cells and Materials, 9, 23–32.
Magne, D., Vinatier, C., Julien, M., Weiss, P., & Guicheux, J. (2005). Mesenchymal stem cell therapy to rebuild cartilage. Trends in molecular Medicine, 11, 519–526.
Koga, H., Engebretsen, L., Brinchmann, J. E., Muneta, T., & Sekiya, I. (2009). Mesenchymal stem cell-based therapy for cartilage repair: a review. Knee Surgery, Sports Traumatology, Arthroscopy, 17, 1289–1297.
Scharstuhl, A., Schewe, B., Benz, K., Gaissmaier, C., Buhring, H.-J., & Stoop, R. (2007). Chondrogenic potential of human adult mesenchymal stem cells is independent of age or osteoarthritis etiology. Stem Cells, 25, 3244–3251.
Hui, J. H. P., & Marchie, A. (2003). Current management of cartilage defect: a review. APLAR Journal of Rheumatology, 6, 170–177.
Medvedeva, E. V., Grebenik, E. A., Gornostaeva, S. N., Telpuhov, V. I., Lychagin, A. V., Timashev, P. S., et al. (2018). Repair of damaged articular cartilage: current approaches and future directions. International Journal of Molecular Sciences, 19(8), 2366.
Gigante, A., Cecconi, S., Calcagno, S., Busilacchi, A., & Enea, D. (2012). Arthroscopic knee cartilage repair with covered microfracture and bone marrow concentrate. Arthroscopy Techniques, 1(2), e175–e180.
Orth, P., Gao, L., & Madry, H. (2020). Microfracture for cartilage repair in the knee: a systematic review of the contemporary literature. Knee Surgery, Sports Traumatology, Arthroscopy, 28(3), 670–706.
Brittberg, M., Lindahl, A., Nilsson, A., Ohlsson, C., Isaksson, O., & Peterson, L. (1994). Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. New England Journal of Medicine, 331, 889–895.
Matricali, G. A., Dereymaeker, G. P., & Luyten, F. P. (2010). Donor site morbidity after articular cartilage repair procedures: a review. Acta Orthopaedica Belgica, 76(5), 669–674.
Tallheden, T., Bengtsson, C., Brantsing, C., Sjogren-Jansson, E., Carlsson, L., Peterson, L., et al. (2005). Proliferation and differentiation potential of chondrocytes from osteoarthritic patients. Arthritis Research and Therapy, 7(3), R560–R568.
Goldring, M. B., & Berenbaum, F. (2004). The regulation of chondrocyte function by proinflammatory mediators: prostaglandins and nitric oxide. Clinical Orthopaedics and Related Research, 427(Suppl), S37–S46.
Caplan, A. I. (2010). Mesenchymal stem cells: the past, the present, the future. Cartilage, 1(1), 6–9.
Punwar, S., & Khan, W. S. (2011). Mesenchymal stem cells and articular cartilage repair: clinical studies and future direction. The Open Orthopaedics Journal, 5(Suppl 2-M11), 296–301.
Park, S., & Im, G.-I. (2014). Embryonic stem cells and induced pluripotent stem cells for skeletal regeneration. Tissue Engineering Part B: Reviews, 20(5), 381–391.
Horwitz, E. M., Le Blanc, K., Dominici, M., Mueller, I., Slaper-Cortenbach, I., Marini, F. C., et al. (2005). Clarification of the nomenclature for MSC: The International Society for Cellular Therapy position statement. Cytotherapy., 7(5), 393–395.
Zhang, R., Ma, J., Han, J., Zhang, W., & Ma, J. (2019). Mesenchymal stem cell related therapies for cartilage lesions and osteoarthritis. American Journal of Translational Research, 11(10), 6275–6289.
Goldberg, A., Mitchell, K., Soans, J., Kim, L., & Zaidi, R. (2017). The use of mesenchymal stem cells for cartilage repair and regeneration: a systematic review. Journal of Orthopaedic Surgery and Research, 12(39), 2–30.
Steck, E., Fischer, J., Lorenz, H., et al. (2009). Mesenchymal stem cell differentiation in an experimental cartilage defect: restriction of hypertrophy to bone-close neocartilage. Stem Cells and Development, 18(7), 969–978.
Teo, A. Q. A., Wong, K. L., Shen, L., Lim, J. Y., Toh, W. S., Lee, E. H., et al. (2019). Equivalent 10-Year out comes after implantation of autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation for chondral defects of the knee. American Journal of Sports Medicine, 47(12), 2881–2887.
Freitag, J., Bates, D., Wickham, J., Shah, K., Huguenin, L., Tenen, A., et al. (2019). Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: a randomized controlled trial. Regenerative Medicine, 14(3), 213–230.
Danišovič, L., Boháč, M., Zamborský, R., et al. (2016). Comparative analysis of mesenchymal stromal cells from different tissue sources in respect to articular cartilage tissue engineering. General Physiology and Biophysics., 35(2), 207–214.
Kuroda, K., Kabata, T., Hayashi, K., et al. (2015). The paracrine effect of adipose-derived stem cells inhibits osteoarthritis progression. BMC Musculoskeletal Disorders, 16(1), 236.
Kretlow, J. D., Jin, Y. Q., Liu, W., et al. (2008). Donor age and cell passage affects differentiation potential of murine bone marrow derived stem cells. BMC Cell Biology., 9(1), 60.
Monaco, M. L., Merckx, G., Ratajczak, J., Gervois, P., Hilkens, P., Clegg, P., et al. (2018). Stem cells for cartilage repair: preclinical studies and insights in translational animal models and outcome measures. Stem Cells International, 2018, 9079538. https://doi.org/10.1155/2018/9079538.
Guzzo, R. M., Gibson, J., Xu, R. H., Lee, F. Y., & Drissi, H. (2013). Efficient differentiation of human iPSC-derived mesenchymal stem cells to chondroprogenitor cells. Journal of Cellular Biochemistry, 114(2), 480–490.
Nam, Y., Rim, Y. A., Lee, J., & Ju, J. H. (2018). Current therapeutic strategies for cell based cartilage regeneration. Stem Cells International, 2018, 8490489. https://doi.org/10.1155/2018/8490489.
Mushahary, D., Spittler, A., Kasper, C., Weber, V., & Charwat, V. (2018). Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry, A93, 19–31.
Enea, D., Cecconi, S., Calcagno, S., et al. (2013). Single-stage cartilage repair in the knee with microfracture covered with a resorbable polymer-based matrix and autologous bone marrow concentrate. The Knee, 20(6), 562–569.
Lee, W. Y., & Wang, B. (2017). Cartilage repair by mesenchymal stem cells: clinical trial update and perspectives. Journal of Orthopaedic Translation, 9, 76–88.
Pountos, I., Corscadden, D., Emery, P., & Giannoudis, P. V. (2007). Mesenchymal stem cell tissue engineering: techniques for isolation, expansion and application. Injury, 38(S4), S23–33.
Mizukami, A., & Swiech, K. (2018). Mesenchymal stromal cells: from discovery to manufacturing and commercialization. Stem Cells International, 2018, 4083921. https://doi.org/10.1155/2018/4083921.
Panchalingam, K. M., Jung, S., Rosenberg, L., & Behie, L. A. (2015). Bioprocessing strategies for the large-scale production of human mesenchymal stem cells :a review. Stem Cell Research and Therapy, 6, 225.
Rowley, J., Abraham, E., Campbell, A., Brandwein, H., & Oh, S. (2012). Meeting lot-size challenges of manufacturing adherent cells for therapy. Bioprocess International, 10, 16–22.
Lam, A. T. L., Reuveny, S., & Oh, S. (2020). Human mesenchymal stem cell therapy for cartilage repair: Review on isolation, expansion, and constructs. Stem Cell Research, 101738, 1–14.
Shimomura, K., Ando, W., Fujie, H., Hart, D. A., Yoshikawa, H., & Nakamura, N. (2018). Scaffold-free tissue engineering for injured joint surface restoration. Journal of Experimental Orthopaedics, 5(1), 2.
Ando, W., Tateishi, K., Hart, D. A., Katakai, D., Tanaka, Y., Nakata, K., et al. (2007). Cartilage repair using an in vitro generated scaffold-free tissue-engineered construct derived from porcine synovial mesenchymal stem cells. Biomaterials, 18, 5462–5470.
Wakitani, S., Nawata, M., Tensho, K., Okabe, T., Machida, H., & Ohgushi, H. (2007). Repair of articular cartilage defects in the patello-femoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. Journal of Tissue Engineering and Regenerative Medicine, 1(1), 74–79.
Li, Z., Kupcsik, L., Yao, S.-J., Alini, M., & Stoddart, M. J. (2009). Chondrogenesis of human bone marrow mesenchymal stem cells in fibrin-polyurethane composites. Tissue Engineering Part A, 15(7), 1729–1737.
Bornes, T. D., Jomha, N. M., Mulet-Sierra, A., & Adesida, A. B. (2016). Optimal seeding densities for In Vitro chondrogenesis of two- and three-dimensional-isolated and—expanded bone marrow-derived mesenchymal stromal stem cells within a porous collagen scaffold. Tissue Engineering Part C: Methods, 22(3), 208–220.
Yokoyama, A., Sekiya, I., Miyazaki, K., Ichinose, S., Hata, Y., & Muneta, T. (2005). In vitro cartilage formation of composites of synovium-derived mesenchymal stem cells with collagen gel. Cell and Tissue Research, 332, 289–298.
Yu, D. A., Han, J., & Kim, B. S. (2012). Stimulation of chondrogenic differentiation of mesenchymal stem cells. International Journal of Stem Cells, 5(1), 16–22.
Dave, L. Y. H., Nyland, J., McKee, P. B., & Caborn, D. N. M. (2012). Mesenchymal stem cell therapy in the sports knee: where are we in 2011? Sports Health, 4(3), 252–257.
Armiento, A. R., Stoddart, M. J., Alini, M., & Eglin, D. (2018). Biomaterials for articular cartilage tissue engineering: learning from biology. Acta Biomaterialia, 65, 1–20.
Xu, Y., Kim, C. S., Saylor, D. M., & Koo, D. (2017). Polymer degradation and drug delivery in PLGA-based drug-polymer applications: a review of experiments and theories. Journal of Biomedical Materials Research, 105, 1692–1716.
Rai, V., Dilisio, F. M., Dietz, N. E., & Agrawal, D. K. (2017). Recent Strategies in Cartilage Repair: A systemic review of the scaffold development and tissue engineering. Journal of Biomedical Materials Research Part A, 105(8), 2343–2354.
Rezwan, K., Chen, Q. Z., Blaker, J. J., & Boccaccini, A. R. (2006). Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials, 27(18), 3413–3431.
Tare, R. S., Howard, D., Pound, J. C., Roach, H. I., & Oreffo, R. O. C. (2005). Tissue engineering strategies for cartilage generation—micromass and three dimensional cultures using human chondrocytes and a continuous cell line. Biochemical and Biophysical Research Communications, 333(2), 609–621.
Johnstone, B., Hering, T. M., Caplan, A. L., Goldberg, V. M., & Joo, J. U. (1998). In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Experimental Cell Research, 238, 265–272.
Nimura, A., Muneta, T., Koga, H., et al. (2008). Increased proliferation of human synovial mesenchymal stem cells with autologous human serum: comparisons with bone marrow mesenchymal stem cells and with fetal bovine serum. Arthritis and Rheumatism, 58, 501–510.
Centeno, C. J., Busse, D., Kisiday, J., Keohan, C., Freeman, M., & Karli, D. (2008). Regeneration of meniscus cartilage in a knee treated with percutaneously implanted autologous mesenchymal stem cells. Medical Hypotheses, 71(6), 900–908.
Orozco, L., Munar, A., Soler, R., et al. (2013). Treatment of knee osteoarthritis with autologous mesenchymal stem cells: A Pilot Study. Transplantation, 95(12), 1535–1541.
Davatchi, F., Abdollahi, B. S., Mohyeddin, M., Shahram, F., & Nikbin, B. (2011). Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. International Journal of Rheumatic Diseases, 14(2), 211–215.
Emadedin, M., Liastani, M. G., Fazeli, R., et al. (2015). Long-term follow-up of intra-articular injection of autologous mesenchymal stem cells in patients with knee, ankle, or hip osteoarthritis. Archives of Iranian Medicine, 18(6), 336–344.
Wong, K. L., Lee, K. B., Tai, B. C., Law, P., Lee, E. H., & Hui, J. H. (2013). Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years' follow-up. Arthroscopy, 29(12), 2020–2028.
Kobayashi, T., Ochi, M., Yanada, S., Ishikawa, M., Adachi, N., Deie, M., et al. (2008). A novel cell delivery system using magnetically labeled mesenchymal stem cells and an external magnetic device for clinical cartilage repair. Arthroscopy: The Journal of Arthroscopic and Related Surgery, 24, 69–76.
Ikuta, Y., Kamei, N., Ishikawa, M., Adachi, N., & Ochi, M. (2015). In vivo kinetics of mesenchymal stem cells transplanted into the knee joint in a rat model using a novel magnetic method of localization. Clinical and Translational Science, 8(5), 467–474.
Cotter, E. J., Wang, K. C., Yanke, A. B., & Chubinskaya, S. (2018). Bone marrow aspirate concentrate for cartilage defects of the knee: from bench to bedside evidence. Cartilage., 9(2), 161–170.
Soler, R. R., Munar, A., Soler, R. F., et al. (2015). Treatment of knee osteoarthritis with autologous expanded bone marrow mesenchymal stem cells:50 cases clinical and MRI results at one year follow-up. Journal of Stem Cell Research and Therapy, 5(6), 2–7.
Lamo-Espinosa, J. M., Mora, G., Blanco, J. F., et al. (2016). Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: multicenter randomized controlled clinical trial (phase I/II). Journal of Translational Medicine, 14(1), 246. https://doi.org/10.1186/s12967-016-0998-2.
Jo, C. H., Lee, Y. G., Shin, W. H., Kim, H., Chai, J. W., Jeong, E. C., et al. (2014). Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells, 32, 1254–1266.
Skowroński, J., & Rutka, M. (2013). Osteochondral lesions of the knee reconstructed with mesenchymal stem cells—results. Ortopedia, Traumatologia, Rehabilitacja, 15(3), 195–204.
Chahla, J., Dean, C. S., Moatshe, G., Pascual-Garrido, C., Serra Cruz, R., & LaPrade, R. F. (2016). Concentrated bone marrow aspirate for the treatment of chondral injuries and osteoarthritis of the knee: a systematic review of outcomes. Orthopaedic Journal of Sports Medicine, 4(1), 2325967115625481. https://doi.org/10.1177/232596711562548.
Gobbi, A., & Whyte, G. P. (2016). One-stage cartilage repair using a hyaluronic acid–based scaffold with activated bone marrow—derived mesenchymal stem cells compared with microfracture: five-year follow-up. American Journal of Sports Medicine, 44(11), 2846–2854.
Ha, C. W., Park, Y. B., Kim, S. H., & Lee, H. J. (2019). Intra-articular mesenchymal stem cells in osteoarthritis of the knee: A systematic review of clinical outcomes and evidence of cartilage repair. Arthroscopy, 35(1), 277–288.
Kim, S. H., Ha, C. W., Park, Y. B., Nam, E., Lee, J. E., & Lee, H. J. (2019). Intra-articular injection of mesenchymal stem cells for clinical outcomes and cartilage repair in osteoarthritis of the knee: A meta-analysis of randomized controlled trials. Archives of Orthopaedic and Trauma Surgery, 139(7), 971–980.
Kim, J. D., Lee, G. W., Jung, G. H., et al. (2014). Clinical outcome of autologous bone marrow aspirates concentrate (BMAC) injection in degenerative arthritis of the knee. European Journal of Orthopaedic Surgery and Traumatology, 24, 1505–1511.
Kuroda, R., Ishida, K., Matsumoto, T., Akisue, T., Fujioka, H., Mizuno, K., et al. (2007 Feb). Treatment of a full-thickness articular cartilage defect in the femoral condyle of an athlete with autologous bone-marrow stromal cells. Osteoarthritis and Cartilage, 15(2), 226–231.
Wakitani, S., Mitsuoka, T., Nakamura, N., Toritsuka, Y., Nakamura, Y., & Horibe, S. (2004). Autologous bone marrow stromal cell transplantation for repair of full thickness articular cartilage defects in human patellae: two case reports. Cell Transplantation, 13(5), 595–600.
de Windt, T. S., Vonk, L. A., Slaper-Cortenbach, I. C., van den Broek, M. P., Nizak, R., van Rijen, M. H., et al. (2017). Allogeneic mesenchymal stem cells stimulate cartilage regeneration and are safe for single-stage cartilage repair in humans upon mixture with recycled autologous chondrons. Stem Cells., 35(1), 256–264.
Akgun, I., Unlu, M. C., Erdal, O. A., Ogut, T., Erturk, M., Ovali, M., et al. (2015). Matrix-induced autologous mesenchymal stem cell implantation versus matrix-induced autologous chondrocyte implantation in the treatment of chondral defects of the knee: A 2-year randomized study. Archives of Orthopaedic and Trauma Surgery, 135(2), 251–263.
Kim, Y. S., Choi, Y. J., Suh, D. S., et al. (2015). Mesenchymal stem cell implantation in osteoarthritic knees: is fibrin glue effective as a scaffold? American Journal of Sports Medicine, 43(1), 1–10.
Nejadnik, H., Hui, J. H., FengChoong, E. P., Tai, B. C., & Lee, E. H. (2010). Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. American Journal of Sports Medicine, 38, 1110–1116.
Emadedin, M., Labibzadeh, N., Liastani, M. G., et al. (2018). Intra-articular implantation of autologous bone marrow-derived mesenchymal stromal cells to treat knee osteoarthritis: a randomized, triple-blind, placebo-controlled phase 1/2 clinical trial. Cytotherapy., 20(10), 1238–1246.
Gigante, A., Calcagno, S., Cecconi, S., Ramazzotti, D., Manzotti, S., & Enea, D. (2011). Use of collagen scaffold and autologous bone marrow concentrate as a one-step cartilage repair in the knee: histological results of second-look biopsies at 1 year follow-up. International Journal of Immunopathology and Pharmacology, 24, 69–72.
Gobbi, A., Karnatzikos, G., Scotti, C., Mahajan, V., Mazzucco, L., & Grigolo, B. (2011). One-step cartilage repair with bone marrow aspirate concentrated cells and collagen matrix in full-thickness knee cartilage lesions: results at 2-year follow-up. Cartilage, 2, 286–299.
Buda, R., Vannini, F., Cavallo, M., et al. (2010). Osteochondral lesions of the knee: a new one-step repair technique with bone-marrow derived cells. Journal of Bone and Joint Surgery. American Volume, 92(Suppl 2), 2–11.
Buda, R., Vannini, F., Cavallo, M., et al. (2013). One-step arthroscopic technique for the treatment of osteochondral lesions of the knee with bone-marrow-derived cells: three years results. Musculoskeletal Surgery, 97(2), 145–151.
Haleem, A., El-Singergy, A., Sabry, D., et al. (2010). The clinical use of human culture-expanded autologous bone marrow mesenchymal stem cells transplanted on platelet-rich fibrin glue in the treatment of articular cartilage defects: a pilot study and preliminary results. Cartilage, 1(4), 253–261.
Koh, Y. G., Choi, Y. J., Kwon, O. R., & Kim, Y. S. (2014). Second-look arthroscopic evaluation of cartilage lesions after mesenchymal stem cell implantation in osteoarthritic knees. American Journal of Sports Medicine, 42, 1628–1637.
Wakitani, S., Okabe, T., Horibe, S., Mitsuoka, T., Saito, M., Koyama, T., et al. (2011). Safety of autologous bone marrow-derived mesenchymal stem cell transplantation for cartilage repair in 41 patients with 45 joints followed for up to 11 years and 5 months. Journal of Tissue Engineering and Regenerative Medicine, 5, 146–150.
Awad, M. E., Hussein, K. A., Helwa, I., Abdelsamid, M. F., et al. (2019). Meta-Analysis and evidence base for the efficacy of autologous bone marrow mesenchymal stem cells in knee cartilage repair: methodological guidelines and quality assessment. Stem Cells International, 2019, 3826054.
Wang, M., Yuan, Z., Ma, N., Hao, C., et al. (2017). Advances and prospects in stem cells for cartilage regeneration. Stem Cells International, 2017, 4130607. https://doi.org/10.1155/2017/4130607.
Arshi, A., Petrigliano, F. A., Williams, R. J., & Jones, K. J. (2020). Stem cell treatment for knee articular cartilage defects and osteoarthritis. Current Reviews in Musculoskeletal Medicine, 13(1), 20–27.
Zhang, S., Chu, W. C., Lai, R. C., Lim, S. K., Hui, J. H., & Toh, W. S. (2016). Exosomes derived from human embryonic mesenchymal stem cells promote osteochondral regeneration. Osteoarthritis Cartilage, 24, 2135–2140.
Steinert, A., Noth, U., & Tuan, R. (2008). Concepts in gene therapy for cartilage repair. Injury, 39(Suppl 1), S97–113.
Cucchiarini, M., & Madry, H. (2018). Advances in gene therapy for cartilage repair. Annals of Joint, 3(97), 1–9.
Brunger, J. M., Huynh, N. P., Guenther, B. M., et al. (2014). Scaffold mediated lentiviral transduction for functional tissue engineering of cartilage. Proceedings of the National Academy of Sciences USA, 111, E798–E806.
Zhang, M., & Wang, J. (2015). Epigenetics and osteoarthritis. Genes and Diseases, 2(1), 69–75.
Ozkul, Y., & Galderisi, U. (2016). The impact of epigenetics on mesenchymal stem cell biology. Journal of Cellular Physiology, 9999, 1–9.
Funding
No grants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Debnath, U.K. Mesenchymal Stem Cell Therapy in Chondral Defects of Knee: Current Concept Review. JOIO 54 (Suppl 1), 1–9 (2020). https://doi.org/10.1007/s43465-020-00198-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00198-0