Abstract
Background
Many reconstruction methods have evolved to offer limb salvage surgery (LSS) to patients with musculoskeletal sarcomas. It can be achieved using endoprosthesis or biological reconstruction methods like allograft or autograft or a combination of both. In carefully selected patients, resected bone can be recycled and reimplanted after sterilisation using methods like irradiation, autoclaving, pasteurisation or liquid nitrogen.
Methods
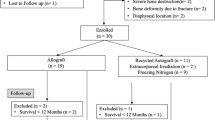
From 2010 to 2016, 10 patients with primary musculoskeletal sarcoma underwent limb salvage surgery (LSS) by wide resection of the tumour and reconstruction using recycled autograft treated with liquid nitrogen. Intercalary resection was carried out in six patients and intra-articular in four. The resected bone was dipped in liquid nitrogen for 25 min, thawed at room temperature for 15 min followed by dipping in vancomycin-mixed saline for 10 min. The recycled bone was re-implanted into its original site and stabilised with internal fixation.
Results
At a mean follow-up period of 39.6 months (range 6–97 months), all patients had a good function (mean functional score of 80%) with no evidence of local recurrence in the re-implanted bone or otherwise. Union was achieved at 15 of the 16 osteotomy sites with a mean union time of 5.2 months (range 4–7 months) without any additional surgical interventions. In none of the patient, augmentation with vascularised/non-vascularised fibula was done. No complication like fracture of the autograft, implant failure or deep/superficial infection was reported in any patient.
Conclusion
Recycled tumour-bearing autograft after treatment with liquid nitrogen is an anatomical, cost-effective, relatively simpler and reliable technique for reconstruction of bone defect after resection in selective primary musculoskeletal sarcoma patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Limb salvage, wherever possible, has become the modality of choice for surgical treatment of primary malignant bone sarcomas. Advances in imaging, neo-adjuvant chemotherapy, improved surgical resection and reconstruction techniques have contributed to our understanding and management of sarcomas more effectively resulting in not only an improved survival rate but also a good functional limb. Limb salvage surgery involves two main steps, i.e., resection and reconstruction [1]. Reconstruction can be achieved with the use of non-biological endoprosthesis or biological methods such as allograft, vascularised fibula, recycled autograft or by making use of a combination of allograft/autograft and endoprosthesis.
Endoprosthetic replacement after resection of tumour is the most commonly used technique for reconstruction of the bone and joint loss in sarcoma patients due to its easy availability for almost all anatomical locations and modularity to fit any bony defect. Excellent survival rates and long-term good results have been reported for this method of reconstruction [1, 2]. However, there are concerns regarding long-term durability of endoprosthesis on account of complications like loosening, fracture, failure of locking mechanism and infection which often requires revision [3,4,5,6,7]. Another significant factor is cost of primary endoprosthetic replacement which further increases when revision surgery is required.
Biological reconstruction has, therefore, been used to overcome the problems with non-biological materials for musculoskeletal sarcomas. Biological reconstruction makes use of allograft or autograft such as fibula or recycled autologous bone. Allograft is not readily available due to lack of bone banking facilities at many hospitals. Also, concerns regarding potential complications like immune-mediated rejections, transmission of communicable diseases, high incidence of infection, fracture and non-union have still not been adequately resolved [8,9,10,11].
Fibular autograft is another option for reconstruction of segmental bone defects after tumour resection. However, a defect size of 12 cm or more reconstructed with non-vascularised or vascularised fibula has been shown to be a statistically significant risk factor for suffering mechanical complications like fatigue fractures and non-union requiring surgical revision besides complications like donor site morbidity including ankle joint instability in children and subclinical gait alteration as observed by gait analyses [12,13,14,15]. In addition, in vascularised fibula, there may be technique-related failure of anastomosis reported to be varying from 4 to 17% [16].
Utilisation of sterilised recycled autograft is a useful alternative for reconstruction of tumour bone defects in selective patients. Recycled autograft has the unique advantage of providing an anatomically size-matched graft, while restoring the bone stock with sufficient biomechanical strength [17]. It is an inexpensive modality and does not require the services of a bone bank. However, use of this modality is possible only in cases of bone tumours with minimal bone destruction or in tumours where restoration of bone has taken place due to good response to chemotherapy. Thus, in carefully selected cases, recycled autograft seems to be an excellent option.
Several methods have been developed to sterilise the resected bone such as extra-corporeal radiotherapy (ECRT), autoclaving and pasteurisation [18,19,20,21]. ECRT although has shown good results but requires a radiation oncology facility in the hospital and also involves transporting the resected bone outside the operation theatre (OT) with proper aseptic precautions [18, 19]. Pasteurisation has shown good early results; whereas, autoclaving degrades the biological and mechanical properties of the bone [22].
In 2005, Tsuchiya et al. described a method of reconstruction using tumour-bearing autograft treated by liquid nitrogen in 28 patients [23]. This method of cryosterilization has shown excellent results with the added advantage of not requiring a special set-up as it was performed within the OT itself. There is no denaturation of bone collagen ensuring better biomechanical and osteoconductive properties as compared to other methods of sterilisation of tumour-bearing bone [17]. Based on these encouraging results and simplicity of technique, we undertook a similar procedure for recycling the tumour-bearing autograft for reconstruction in carefully selected patients of musculoskeletal sarcomas.
Materials and Methods
From 2010 to 2016, 10 patients (4 females, 6 males) underwent limb salvage surgery (LSS) by wide resection of the tumour and reconstruction with recycled tumour-bearing autograft sterilised using liquid nitrogen. The mean age of the group was 16 years (range 8–35 years). Ewing’s sarcoma was diagnosed in seven patients and two patients had osteosarcoma. One patient had liposarcoma which was wrapped around fibula. Sites involved were the proximal humerus (Fig. 2), shaft femur (Fig. 3), distal femur (Fig. 1) and distal fibula in two cases each. Proximal femur and shaft fibula were the sites affected in one patient each.
a Post neo-adjuvant chemotherapy MRI in a13 yrs female with osteosarcoma involving distal femur but sparing of epiphysis. b Check X-ray after 6 months of intercalary resection (distal osteotomy was trans-epiphyseal) and reimplantation after treatment with liquid nitrogen showing union at both osteotomy sites. c Check X-ray after 96 months of surgery. d Full range of movements at knee joint
a X-ray of humerus in a 18 years male with osteosarcoma involving proximal humerus. b MRI showing large soft tissue component. c Post neo-adjuvant chemotherapy MRI showing significant decrease in soft tissue component, d resected bone after treatment with liquid nitrogen. e Check X-ray after 6 months of reimplantation showing union at osteotomy site
After confirmation of histopathological diagnosis and appropriate staging investigations, all patients with Ewing’s sarcoma and osteosarcoma underwent appropriate neo-adjuvant chemotherapy as per institutional protocol. Response to chemotherapy was assessed pre-operatively clinically as well as by radiographs and magnetic resonance imaging (MRI) of the affected part. The resection length was planned pre-operatively based on the MRI imaging showing the maximum extent of the tumour. Intercalary resection was carried out in six patients and intra-articular in four. The four patients who underwent intra-articular resection were with tumours in proximal humerus (n = 2) and distal fibula (n = 2). The average length of resection was 20.5 cm (range 14–27 cm). Length of resection also included safe surgical margin(s). Bone marrow biopsy was taken from end(s) of resected bone as well as residual bony stump(s). In seven patients, it was possible to achieve wide surgical margins including margin of ≥ 2 cms in the bone. In three patients where bony resection margins were close to the tumour, the barrier concept elucidated by Kawaguchi et al. was taken into consideration [24]. In two patients, tumour extended up to but did not involve epiphyseal plate. In one patient with Ewing’s sarcoma of proximal femur, the involved segment along with epiphyseal plate was separated from capital femoral epiphysis; whereas in the other patient with osteosarcoma involving distal femur, trans-epiphyseal osteotomy close to epiphyseal plate was done (Fig. 3). In third patient with Ewing’s sarcoma involving shaft of femur, on pre-chemotherapy MRI, tumour extended up to lesser trochanter proximally. However due to good response to chemotherapy, there was significant reduction in the intramedullary and soft tissue extent. The proximal resection margin in this patient was 1 cm away from intramedullary extent as determined on pre-chemotherapy MRI but was > 2 cm away as determined on post-chemotherapy MRI (Fig. 2). In these three patients, intraoperative frozen sections of marrow/bone samples from osteotomy sites were taken to establish whether osteotomy sites were tumour free or not. All were reported as tumour free. Resected bone was stripped of soft tissues including periosteum. Intramedullary reaming as well as curettage of any surface tumour tissue on the resected bone was carried out. Liquid nitrogen was poured into a stainless steel cylindrical container. The resected bone was dipped in liquid nitrogen for 25 min, and then thawed at room temperature for 15 min, followed finally by dipping in vancomycin-mixed saline for 10 min. The recycled excised bone was re-implanted at original site and stabilised by appropriate internal fixation using plating, nailing or a combination of both. Patients were given planned cycles of adjuvant chemotherapy after 3 weeks of surgery. Patients were regularly followed up at monthly intervals with X-rays to assess the status of bone union at osteotomy site(s). Gradually increasing weight bearing was allowed based on the radiological evidence of progress of union. Radiological union of the re-implanted segment both proximally and distally was assessed according to the method followed by Hsu et al. [25] Graft union was defined as uninterrupted external bony borders between the graft and the recipient bone in addition to obscured or absent osteotomy lines at both junctions. Once the osteotomy site(s) united, a three monthly follow-up was maintained for the first 2 years and thereafter a 6 monthly follow-up to evaluate for any local recurrence or distant metastases.
a Pre-chemotherapy MRI of femur in a 16 years male with Ewing's sarcoma involving shaft of femur. b Post neo-adjuvant chemotherapy MRI showing significant decrease in both soft tissue component as well as intramedullary extent, c resected bone. d Clinical photograph after reimplantaion and fixation of liquid nitrogen treated resected bone. e, f Check X-rays after 24 months of reimplantation showing union at both osteotomy sites
Results
The mean follow-up period till the filing of the study was 39.6 months (range 6–97 months). At the latest follow-up, six patients continue to remain disease free. Three patients had died due to metastatic disease. One patient died at 6 months of follow-up due to chemotherapy-related complications. No local recurrence in the surgical site region or recycled autograft has been seen in any patient. Union was achieved at 15 out of the 16 osteotomy sites in 10 patients with a mean union time of 5.2 months (range 4–7 months). Non-union was seen only in one patient (case 10) at the proximal femoral osteotomy site (Fig. 4). This patient who had Ewing’s sarcoma of femoral diaphysis and was given additional local radiotherapy at a regional centre where he was receiving chemotherapy after 3 weeks of surgery which might have contributed to non-union at proximal osteotomy site. In this patient, additional autologous bone grafting was done after 11 months of initial surgery when the patient had completed his chemotherapy. Union was achieved at the end of 23 months. Patient is full weight bearing on this limb and is pain free.
The functional evaluation was performed using the modified system of the Musculoskeletal Tumour Society based on parameters including pain, functional activities, emotional acceptance, the use of external support, walking ability and gait [26]. For the upper extremity reconstructions parameters such as hand positioning, manual dexterity and lifting ability were taken into consideration instead of external support, walking ability and gait which are more relevant for the lower limb. The mean functional score for the study group was 80.2% (range 75–85%).
No complication such as fracture of the autograft, implant failure or deep/superficial infection was reported in any of our cases. One patient, where reimplantation of distal fibula was done, complained of irritation due to screw heads. In this patient, implant removal was carried out after 3 years of initial surgery. No evidence of joint cartilage damage and resultant arthritis as assessed by absence of joint surface irregularity or pain in cases that have undergone intra-articular resection has been reported till the last follow-up. Limb shortening by 1.5 cm was seen in one patient (case 1) of distal femur osteosarcoma who underwent a transphyseal distal femoral osteotomy as part of the resection process. The patient has an excellent knee function and does not complain of a limp as a result of the shortening; thus, no further intervention has been advised. Details of results are in Table 1.
Discussion
Reimplantation of resected bone treated with liquid nitrogen has been used in the domain of oral surgery since long. In 1966, Gage et al. researched the effects of liquid nitrogen on bone and in 1976, Marciani et al. reported good remodelling capacity after reimplantation of liquid nitrogen-treated resected mandibular bone [27, 28]. In 1969, Marcove and Miller used liquid nitrogen for palliative treatment in bone metastasis with good pain control [29]. In 1984, Marcove et al. described the use of the liquid nitrogen for management of the primary lesion in osteosarcoma adopting liquid nitrogen as an adjuvant to curettage and cement for reconstruction [30]. Subsequently, it was Tsuchiya et al. in 2005 who described the reconstruction method using a tumour-bearing autograft treated with liquid nitrogen and accordingly divided the technique into three types (IA/IB, II, and III). The surgical technique comprised free-freezing and pedicle-freezing methods that were used according to the tumour location. Limb functional results were graded as excellent in 71.4% of the patients [23].
The mechanism of action of liquid nitrogen on tumour cells is mainly by inducing ice crystal formation and dehydration. This selectively leads to cell death of the tumour cells as they are more sensitive to low temperatures than normal cells [31, 32]. Another possible cause of cell death during cryosurgery is ischemic infarction due to thrombosis of the microcirculation [33]. It is actually the process of alternate freezing (− 196°) for 20 min, then thawing first at room temperature for 15 min and then in physiological saline or distilled water for another 15 min which is considered fatal to the tumour cells. It has been shown that number of cycles whether one or two with liquid nitrogen treatment had a similar effect on reduction of tumour volume [17]. We followed a single cycle of liquid nitrogen treatment for 25–30 min, thawing at normal operation room temperature for 15 min and then in vancomycin-mixed normal saline for 10 min.
Proper patient selection is vital for successful use of recycled autograft. Tumours causing gross destruction of the bone are unsuitable for reconstruction with recycled autograft. Thus, a careful pre-operative assessment of bone quality is critical. The unparalleled advantage with autograft is the anatomical and symmetrical fit with ease of fixation. This makes autograft an attractive option especially in geographical locations where procuring custom-made prostheses or allograft is still a problem [34].
The osteoinductive and osteoconductive properties of frozen autograft treated with liquid nitrogen also remain intact. Studies on histological examination of frozen autograft treated by liquid nitrogen removed after implantation from patients have proved the presence of osteocytes and osteoblasts. Also, connections between bony trabeculae have been found at the host–graft junction [35]. Preservation of bone morphogenetic protein and neovascularisation has also been found [32]. Tsuchiya et al. in their group of 28 patients reported bony union at a mean of 6.7 months after surgery in 26 patients (92.8%). Non-union was seen only in two patients, one of whom had died before bony union and in the other the autograft was removed because of infection before union [23]. In our study, union was achieved at 15 of the 16 osteotomy sites (93.75%). A good functional outcome was seen in all our patients with a good range of motion at the joints near the reconstruction. Bio-integration of soft tissues and muscles into the autograft is another unique advantage seen only with autograft and allograft, not possible with artificial endoprosthesis. Reattachment of muscles on the natural graft allows better muscle control leading to a better gait [36].
Since long, complications like significant injury to the adjacent bone and soft tissue, skin necrosis and nerve injury have been associated with the use of liquid nitrogen with in vivo or by pedicle freezing method [37]. However, in all our patients, treatment with liquid nitrogen was done in vitro or by free-freezing method. Complications such as fracture and infection of the autograft, although a rare possibility, have been reported [23, 38]. Tsuchiya et al. reported complications of deep infection in three and fractures in two patients in their group of 28 patients, but all were successfully managed [23]. No such complication was reported in our study. Use of vancomycin-mixed normal saline during the recycling process could have possibly contributed to no infection in our cases, but this needs further evaluation.
Various studies have recommended the augmentation of allograft with vascularised/non-vascularised fibula [39, 40]. Similar reconstruction methods have been recommended when using recycled autograft. The augmentation of allograft with vascularised fibulae is associated with a lower failure rate as the combined reconstruction is considered to be structurally strong with improved vascular and osteogenic potential, lower rates of infection, fracture, and nonunion [39, 40]. There are no comparative studies examining the outcome of augmentation with fibula in autograft vis-à-vis allograft. However, biomechanical tests have revealed that there was no significant difference in compression strength between the intact bone and the bone treated with one-cycle liquid nitrogen process [17]. Fracture, thus, remains a remote possibility and none was reported in our study. None of the reconstruction in this series was augmented with free/vascularised fibular autograft.
Liquid nitrogen-treated autograft retains the tissue micro-architecture and certain tumour antigens not seen with irradiated or heat-treated graft which usually destroy the tissue proteins [22]. Concerns are often expressed about the ability of various sterilisation methods to completely kill the tumour cells and possibility of local recurrence within the re-implanted recycled autograft. This concern is unfounded. Rather, there is a possibility that tissue proteins from recycled tumour bone have certain antigenic properties which initiate an immune response directed against the tumour, a concept known as cryoimmunology [41]. This could possibly be responsible for low local recurrence rates. There have been reports that metastatic tumours have regressed after freezing of the primary tumour but this needs to be further substantiated [42, 43]. Tsuchiya et al. reported a 7.1% local recurrence (2 patients) in their group of 28 patients, none of which was in the recycled autograft [23]. So far, there has been no local recurrence in our group till the latest follow-up. There are also concerns about graft resorption. In the current study, there was one instance of thinning of distal fibular graft after 3 years of re-implantation. In rest of the patients, there was no such occurrence.
A potential limitation associated with recycled autograft is the non-availability of the entire resected specimen for the pathologist to do histological analysis to determine adequacy of resection margins. Also documentation to quantify response to chemotherapy to tailor subsequent chemotherapy change if any could be a problem since the entire specimen is not available. However, proper marking of the far-margins and evaluation of the soft tissue stripped off the resected bone, bone marrow biopsies both from the resected bone and residual bony stump help the pathologist in conclusively commenting on the tumour free margins and evaluating the response to chemotherapy.
Conclusions
Use of recycled autograft in carefully selected patients seems to be a viable and cost-effective option over endoprosthesis. The use of cryotherapy in the form of liquid nitrogen for sterilising tumour-bearing autograft circumvents the need for elaborate equipment, bone banking and radiation oncology facilities. Concerns regarding local recurrence within the re-implanted recycled autograft seem unsubstantiated. Indeed, the biggest advantage of a biological method which surpasses all other methods is that it is an anatomical and permanent form of reconstruction once incorporated. Careful patient selection is a pre-requisite as it is possible to use this technique only in selective patients with good bone stock. Short to medium term follow-up has established the safety, efficacy and low incidence of complications like non-union or stress fracture when liquid nitrogen is used as a method of sterilisation of tumour bearing autograft.
References
Rougraff, B. T., Simon, M. A., Kneisl, J. S., Greenberg, D. B., & Mankin, H. J. (1994). Limb salvage compared with amputation for osteosarcoma of the distal end of the femur A long-term oncological, functional, and quality-of-life study. The Journal of Bone and Joint Surgery,76(5), 649–656.
Kawai, A., Muschler, G. F., Lane, J. M., Otis, J. C., & Healy, J. H. (1998). Prosthetic knee replacement after resection of a malignant tumour of the distal part of the femur: medium to long term results. The Journal of Bone and Joint Surgery,80, 636–647.
Kumar, D., Grimer, R. J., Abudu, A., Carter, S. R., & Tillman, R. M. (2003). Endoprosthetic replacement of the proximal humerus: long-term results. The Journal of Bone and Joint Surgery,85, 717–722.
Kinkel, S., Lehner, B., Kleinhans, J. A., Jakubowitz, E., Ewerbeck, V., & Heisel, C. (2010). Medium to long-term results after reconstruction of bone defects at the knee with tumour endoprosthesis. Journal of Surgical Oncology,101, 166–169.
Renard, A. J., Veth, R. P., Schreuder, H. W., Van Loon, C. J., Koops, H. S., & Van Horn, J. R. (2000). Function and complications after ablative and limb-salvage therapy in lower extremity sarcoma of bone. Journal of Surgical Oncology,73(4), 198–205.
Grimer, R. J., Carter, S. R., Tillman, R. M., Sneath, R. S., Walker, P. S., Unwin, P. S., et al. (1999). Endoprosthetic replacement of the proximal tibia. The Journal of Bone and Joint Surgery,81, 488–494.
Natarajan, M. V., Annamalai, K., Williams, S., Selvaraj, R., & Rajagopal, T. S. (2000). Limb salvage in distal tibial osteosarcoma using a custom megaprosthesis. International Orthopaedics,24, 282–284.
Aponte-Tinao, L., Ayerza, M. A., Muscolo, D. L., & Farfalli, G. L. (2015). Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clinical Orthopaedics and Related Research,473, 1789–1796.
Matejovsky, Z., Jr., & Kofranek, I. (2006). Massive allografts in tumour surgery. International Orthopaedics,30, 478–483.
Mnaymneh, W., Malinin, T. I., Makley, J. T., & Dick, H. M. (1985). Massive osteoarticular allografts in the reconstruction of extremities following resection of tumors not requiring chemotherapy and radiation. Clinical Orthopaedics and Related Research,197, 76–87.
Tomford, W. W. (1995). Transmission of disease through transplantation of musculoskeletal allografts. The Journal of Bone and Joint Surgery,77, 1742–1754.
Lenze, U., Kasal, S., Hefti, F., & Krieg, A. H. (2017). Non-vascularised fibula grafts for reconstruction of segmental and hemicortical bone defects following meta-/diaphyseal tumour resection at the extremities. BMC Musculoskeletal Disorders,18(1), 289.
El-Gammal, T. A., El-Sayed, A., & Kotb, M. M. (2003). Reconstruction of lower limb bone defects after sarcoma resection in children and adolescents using free vascularized fibular transfer. Journal of Pediatric Orthopedics. Part B,12(4), 233–243.
Nathan, S. S., Hung-Yi, L., Disa, J. J., Athanasian, E., Boland, P., Cordeiro, P. G., et al. (2005). Ankle instability after vascularized fibular harvest for tumor reconstruction. Annals of Surgical Oncology,12(1), 57–64.
Bodde, E. W., de Visser, E., Duysens, J. E., & Hartman, E. H. (2003). Donor-site morbidity after free vascularized autogenous fibular transfer: subjective and quantitative analyses. Plastic and Reconstructive Surgery,111(7), 2237–2242.
Arai, K., Toh, S., Tsubo, K., Nishikawa, S., Narita, S., & Miura, H. (2002). Complications of vascularized fibula graft for reconstruction of long bones. Plastic and Reconstructive Surgery,109(7), 2301–2306.
Yamamoto, N., Tsuchiya, H., & Tomita, K. (2003). Effects of liquid nitrogen treatment on the proliferation of osteosarcoma and the biomechanical properties of normal bone. Journal of Orthopaedic Science,8(3), 374–380.
Kim, J. D., Lee, G. W., & Chung, S. H. (2011). A reconstruction with extracorporeal irradiated autograft in osteosarcoma around the knee. Journal of Surgical Oncology,104(2), 187–191.
Puri, A., Gulia, A., Jambhekar, N., & Laskar, S. (2012). The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and re-implantation of the host bone. The Journal of Bone and Joint Surgery,94(7), 982–988.
Khattak, M. J., Umer, M., & Haroon-ur-Rasheed, U. M. (2006). Autoclaved tumor bone for reconstruction: an alternative in developing countries. Clinical Orthopaedics and Related Research,447, 138–144.
Jeon, D. G., Kim, M. S., Cho, W. H., Song, W. S., & Lee, S. Y. (2007). Pasteurized autograft for intercalary reconstruction: an alternative to allograft. Clinical Orthopaedics and Related Research,456, 203–210.
Takata, M., Sugimoto, N., Yamamoto, N., Shirai, T., Hayashi, K., Nishida, H., et al. (2011). Activity of bone morphogenetic protein-7 after treatment at various temperatures: freezing vs. pasteurization vs. allograft. Cryobiology,63, 235–239.
Tsuchiya, H., Wan, S. L., Sakayama, K., Yamamoto, N., Nishida, H., & Tomita, K. (2005). Reconstruction using an autograft containing tumour treated by liquid nitrogen. The Journal of Bone and Joint Surgery,87, 218–225.
Kawaguchi, N., Matsumoto, S., & Manabe, J. (1995). New method of evaluating the surgical margin and safety margin for musculoskeletal sarcoma, analysed on the basis of 457 surgical cases. Journal of Cancer Research and Clinical Oncology,121, 555–563.
Hsu, R. W., Wood, M. B., Sim, F. H., & Chao, E. Y. (1997). Free vascularised fibular grafting for reconstruction after tumour resection. The Journal of Bone and Joint Surgery,79(1), 36–42.
Enneking, W. F., Dunham, W., Gebhardt, M. C., Malawar, M., & Pritchard, D. J. (1993). A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clinical Orthopaedics and Related Research,286, 241–246.
Gage, A. A., Greene, G. W., Jr., Neiders, M. E., & Emmings, F. G. (1966). Freezing bone without excision. An experimental study of bone-cell destruction and manner of regrowth in dogs. JAMA,196, 770–774.
Marciani, R. D., Giansanti, J. S., & Massey, G. B. (1976). Reimplantation of freeze-treated and saline-treated mandibular bone. Journal of Oral Surgery,34, 314–319.
Marcove, R. C., & Miller, T. R. (1969). Treatment of primary and metastatic bone tumors by cryosurgery. JAMA,207, 1890–1894.
Marcove, R. C., Zahr, K. A., Huvos, A. G., & Ogihara, W. (1984). Cryosurgery in osteogenic sarcoma: report of three cases. Comprehensive Therapy,10, 52–60.
Kimura, T., Kojima, Y., & Nakagawara, G. (1996). Current status of cryopreservation of pancreatic islets. Low Temp Med,22, 1–6. (in Japanese).
Uedaira, H. (1977). Dynamic states of water in biological systems under low temperature. Low Temp Med,3, 87–89. (in Japanese).
Goldstein, R. S., & Hess, P. W. (1977). Cryosurgical treatment of cancer. Veterinary Clinics of North America,7, 51–64.
Tsuchiya, H., Abdel-Wanis, M. E., & Tomita, K. (2006). Biological reconstruction after excision of juxta-articular osteosarcoma around the knee: a new classification system. Anticancer Research,26, 447–453.
Tanzawa, Y., Tsuchiya, H., Shirai, T., Hayashi, K., Yo, Z., & Tomita, K. (2009). Histological examination of frozen autograft treated by liquid nitrogen removed after implantation. Journal of Orthopaedic Science,14(6), 761–768.
Benedetti, M. G., Bonatti, E., Malfitano, C., & Donati, D. (2013). Comparison of allograft-prosthetic composite reconstruction and modular prosthetic replacement in proximal femur bone tumors: functional assessment by gait analysis in 20 patients. Acta Orthopaedica,84(2), 218–223.
Marcove, R. C., Weis, L. D., Vaghaiwalla, M. R., Pearson, R., & Huvos, A. G. (1978). Cryosurgery in the treatment of giant cell tumors of bone. A report of 52 consecutive cases. Cancer,41, 957–969.
Rahman, M. A., Bassiony, A., & Shalaby, H. (2009). Reimplantation of the resected tumour-bearing segment after recycling using liquid nitrogen for osteosarcoma. International Orthopaedics,33(5), 1365–1370.
Capanna, R., Campanacci, D. A., Belot, N., Beltrami, G., Manfrini, M., Innocenti, M., et al. (2007). A new reconstructive technique for intercalary defects of long bones: the association of massive allograft with vascularized fibular autograft. Long-term results and comparison with alternative techniques. Orthopedic Clinics of North America,38(1), 51–60.
Houdek, M. T., Wagner, E. R., Stans, A. A., Shin, A. Y., Bishop, A. T., Sim, F. H., et al. (2016). What is the outcome of allograft and intramedullary free fibula (Capanna technique) in pediatric and adolescent patients with bone tumors? Clinical Orthopaedics and Related Research,474, 660–668.
Drylie, D. M., Jordan, W. P., & Robbins, J. B. (1968). Immunologic consequences of cryosurgery. Investigative Urology,5, 619–626.
Joosten, J. J., Muijen, G. N., Wobbes, T., & Ruers, T. J. (2001). In vivo destruction of tumor tissue by cryoblation can induce inhibition of secondary tumor growth: an experimental study. Cryobiology,42, 49–58.
Joosten, J. J., Muijen, G. N., Wobbes, T., & Ruers, T. J. (2003). Cryosurgery of tumor tissue causes endotoxin tolerance through an inflammatory response. Anticancer Research,23, 427–432.
Funding
None.
Author information
Authors and Affiliations
Contributions
SKG: designed the study, chief surgeon in all the cases, contributed in editing and proof reading the manuscript; PA: radiologist in all cases and carried out imaging studies. Contributed in writing the manuscript; JV: contributed in data collection, literature review and drafting of manuscript; RPSP: pathologist in all cases. Contributed in editing and proof reading the manuscript; KD: oncologist in all cases. Contributed in editing and proof reading the manuscript; RJ: contributed in editing and proof reading the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
There are no financial or other relationships that might lead to a conflict of interest.
Informed Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garg, S.K., Aggarwal, P., Virk, J. et al. Limb Salvage Using Liquid Nitrogen-Treated Tumour-Bearing Autograft: A Single Institutional Experience of 10 Patients. JOIO 54, 200–207 (2020). https://doi.org/10.1007/s43465-019-00001-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-019-00001-9