Abstract
Polycystic ovary syndrome (PCOS) is a gynecological endocrine disorder and the leading cause of anovulatory female infertility. This study aimed to systematically review the effects of curcumin or turmeric on PCOS-related parameters. PubMed, Scopus, Embase, and Web of Knowledge databases and Google Scholar were searched up to August 2021 using relevant keywords. All original articles evaluating the effects of turmeric/curcumin on PCOS were eligible. Out of 107 documents, eight animal studies and five randomized placebo-controlled clinical trials (RCTs) assessing the impact of curcumin on PCOS met our inclusion criteria. The reviewed animal studies indicated the beneficial effects of curcumin on the management of hormonal and metabolic disturbances in the PCOS condition. These effects also were confirmed in some, but not all, included RCTs. Therefore, despite promising animal results, the present literature is limited to conclude the beneficial effects of curcumin on the clinical management of PSCO symptoms. The impact of bioavailability-improved formulations of curcumin on PCOS should be assessed in further well-designed RCTs with longer duration and higher doses of curcumin. Besides, mechanistic investigations on the effects of curcumin on PCOS are also recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycystic ovary syndrome (PCOS) as a gynecological-endocrine disorder is the leading cause of anovulatory female infertility. It also is related to miscarriage and pregnancy-induced complications [1, 2]. According to the Rotterdam consensus, the presence of two out of three parameters of chronic oligo- or anovulation, clinical and/or biochemical signs of hyperandrogenism, and polycystic ovarian morphology defines as PCOS. PCOS is affecting 6–21% of women of reproductive age worldwide, based on the Rotterdam criteria [3, 4]. In addition, PCOS is associated with metabolic aberrations, including insulin resistance, dyslipidemia, adiposity, hypertension, type 2 diabetes mellitus, non-alcoholic fatty liver disease, coronary heart disease, and vascular endothelial dysfunction [1, 5].
The etiology of PCOS is still unclear. However, according to a “2-hit” hypothesis, a congenital predisposition (gene variants, congenital virilization, and disturbed fetal nutrition, as “first hit”) can manifest as PCOS after exposure to an environmental risk factor (exposure to androgens, postnatal obesity, insulin-resistant hyperinsulinemia, and hyperpuberty, as the “second hit”) [6]. Moreover, oxidative stress and inflammation have undeniable roles in the pathophysiology of the disease [7, 8]. Therapeutic management of PCOS is usually limited to improve clinical manifestations, in which dietary modification, weight loss, and increased exercise are in the first-line of interventions [9]. Moreover, herbal medicine use by women with PCOS has been increased during the past years [10].
Curcuma longa L. (turmeric) is a common dietary spice and pigment with a very long history of medicinal use to treat eye infections, skin diseases, respiratory ailments, dental diseases, and digestive disorders [11]. Besides, modern science supports the effects of turmeric on such diseases [12, 13]. Curcumin (diferuloylmethane) is the main bioactive component of turmeric [14]. Recent meta-analysis studies confirm the beneficial effects of curcumin on obesity [15], diabetes [16], hypertension [17], hyperlipidemia [16, 18], oxidative stress, and inflammation [19]. Besides, some animal and human investigations have assessed the effects of curcumin on the management of hormonal and metabolic disturbances and complications of PCOS [20,21,22,23,24]. However, to the best of our knowledge, no review study has summarized the effects of turmeric/curcumin on PCOS so far. Therefore, the current systematic review aimed to comprehensively assess all published studies regarding the effects of curcumin/turmeric supplementation on the parameters of PCOS.
Materials and Methods
Research Strategy
The present systematic review was conducted according to the PRISMA (preferred reporting items for systematic reviews and meta-analysis) guideline [25] by focusing on the effects of turmeric or curcumin on PCOS. Therefore, a systematic search was performed for the relevant in vitro, animal, and human articles published until August 2021, on the PubMed, Embase, Scopus, and Thomson Reuters Web of Knowledge, using the MeSH terms and other related keywords (PubMed search strategy is shown in Supplementary Box 1). Moreover, the Google Scholar search and the forward and backward citation tracking were conducted, separately. The protocol of the present study has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the identification number CRD42020214985.
Eligibility Criteria and Screening Methods
After searching in electronic databases, duplicate studies were removed using the EndNote software, version X8.0. Then, two independent investigators initially screened titles and abstracts of the studies based on the inclusion and exclusion criteria, followed by reviewing the full text of some selected articles. Discrepancies between two reviewers were resolved by discussion or the third reviewer. Study inclusion and exclusion criteria and research questions were structured using the PICOS (population, intervention, comparison, outcome, and study design) criteria. Peer-reviewed in vitro, animal, and human studies published in the English language that examined the effect of turmeric or curcumin (natural or synthetic forms) on PCOS compared to placebo or no treatment were included. The exclusion criteria were literature reviews, newspapers, magazines, conference abstracts, book chapters, notes, short surveys, letters, editorials, case report studies, clinical trial registration, and thesis. Moreover, investigations on the combination of turmeric/curcumin with other agents or medications and other diseases were ineligible.
Data Extraction
Data extraction sheets were developed according to the study types and in line with recommendations from PRISMA [25]. After pilot-testing on one article of each study type, refinement of sheets was performed. Then, two investigators independently extracted data from all selected studies. The data extraction sheets are summarized in Tables 1 and 2.
Risk of Bias Assessment
The risk of bias assessment of the included animal studies and randomized placebo-controlled clinical trials (RCTs) was performed by two independent authors, according to the Office of Health Assessment and Translation (OHAT) [26] and Cochrane [27] handbooks, respectively. Discrepancies between the two reviewers were resolved by discussion or the third reviewer. The response options for each risk of bias question of the OHAT tool are “ − − ” (definitely high risk of bias), “ − ” (probably high risk of bias), “ + ” (probably low risk of bias), or “ + + ” (definitely low risk of bias). After answering questions for each included animal study, using the OHAT recommendations, we gave numerical values from − 2 to + 2 to each question and tiered studies according to the calculated averages (three tiers of the low, moderate, and high risk of bias) [28]. Besides, the Cochrane collaboration’s tool has six bias domains with three response options of “low,” “unclear,” and “high” risk of bias [29]. Based on the discussion among the reviewers, selection bias, performance bias, and detection bias were selected as the key domains for judgment of the overall risk of bias. Each of the included studies was considered to have “low risk of bias” when it had the low risk of bias for all the three key domains, “unclear risk of bias” if it had the unclear risk of bias for ≥ 1 key domain, and “high risk of bias” when it had a high risk of bias for ≥ 1 key domain [29,30,31].
Results
Study Selection
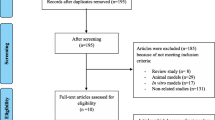
The process of study selection has been depicted in Fig. 1. A total of 92 citations were identified from the electronic databases (PubMed, Embase, Scopus, and Web of Knowledge), and 15 studies were obtained from Google Scholar search. After removing duplicates (n = 70), title and abstract screening were conducted for the other 37 articles among them, and 22 articles were selected for full-text screening based on the inclusion and exclusion criteria. Following the selection process, 13 articles (eight animal studies and five RCTs) [20,21,22,23,24, 32,33,34,35,36,37,38,39], published until August 2021, were included in the systematic review. No additional articles were found through forwarding and backward citation tracking of eligible studies.
Study Characteristics
The main characteristics of the included studies are summarized in Tables 1 and 2. All studies assessed the efficacy of curcumin on PCOS features. Except for four studies [24, 32, 38, 39], others were conducted in Iran [20,21,22,23, 33,34,35,36,37]. Of the eight animal studies, seven examinations were on rats (Wistar [24, 32,33,34,35, 39] and Sprague Dawley [36] rats), and one was on BALB/c mice [20]. A total of 91 animals were included in this review. PCOS was induced in the animals with letrozole [24, 32, 39], dehydroepiandrosterone (DHEA) [20, 36], or estradiol valerate (E2V) [33,34,35] administration. Curcumin [24, 33,34,35,36, 39] or its nanoparticles [20, 32] was administered to animals by gavage [24, 32, 36] or injection [20, 33,34,35, 39], in concentrations varied from 54 mg/kg [20] to 600 mg/kg [35]. The curcumin treatment duration also ranged from 14 [33,34,35, 39] to 30 [36] days after PCOS induction.
The five included RCTs were extracted from four independent investigations, and PCOS was diagnosed according to the Rotterdam criteria in overweight or obese patients of reproductive age in all studies [21,22,23, 37, 38]. A total of 265 women were included in this review. The mean age and body mass index (BMI) of women ranged from 27.6 to 30.97 years and 27.4 to 29.8 kg/m2, respectively. The participants of the intervention groups received 500 [23], 93.34 [38], 1000 [37], or 1500 [21, 22] mg/day of curcumin. The curcumin or placebo administration duration was 6 [37], 8 [38], or 12 [21,22,23] weeks. The number of participants in the intervention groups ranged from 15 [38] to 34 [21, 22] between studies. The data was analyzed according to the intention to treat analysis only in one of the included RCTs [22].
Risk of Bias Assessment
The risk of bias assessment and tier classifications of animal studies is presented in Table 3. Out of the eight selected animal studies, only three studies [20, 35, 36] used randomization for the allocation of animals in different groups. None of the animal studies reported the blindness of outcome assessors to the experimental groups, and only one of the included studies provided sample size calculations [32]. Moreover, in one investigation, the duration of the examination was not similar between the control and intervention groups [24]. Selective reporting bias was also detected in two of the included studies [34, 35]. Finally, two animal studies of the total were classified as tier 1 [20, 36] and six as tier 2 [24, 32,33,34,35, 39], according to the OHAT’s tier system.
Details of the risk of bias assessment of RCTs are demonstrated in Table 4. Of five included RCTs, one trial had an overall unclear risk of bias due to selection bias [23], one had a high risk of bias because of performance bias (single-blinded) [38], and the others had a low risk of bias [21, 22, 37]. In one of the included RCTs, the data related to body weight changes during the follow-up period, as a secondary pre-specified outcome, was not stated [22]. Moreover, in two other studies, reported data on the macronutrient and micronutrient intakes were incomplete [23, 37].
Outcomes
Morphology and Histopathology
Polycystic ovarian, theca cells hyperplasia and hypertrophy, apoptosis of granulosa cells, and decreased corpus luteum are common morphological and histopathological features of PCOS [6]. The included animal studies indicated beneficial effects of curcumin on alleviating ovarian weight [34], volume [20], cysts [34,35,36, 39], and theca layer [34, 35] and also increasing granulosa cells [24, 32, 35] and corpus luteum [24, 34, 36]. Moreover, oocytes were appeared in the ovaries of animals after curcumin administration, in a dose-dependent manner [24, 32]. Fatemi Abhari et al. reported a reduction in the total number of primordial, primary, secondary, and antral follicles in the animals treated with curcumin nanoparticles [20], but the other two studies reported contradictory results [24, 34, 35] (Table 1).
Apoptosis
Apoptosis was assessed only in one of the included studies. Fatemi Abhari et al. demonstrated downregulation of the expression of Bax (B-cell lymphoma 2 (Bcl2)-associated X protein) and caspase3 apoptosis-inducing factors, and also augmentation of anti-apoptotic factor Bcl2 in the ovary tissue of animals with PCOS after treatment with curcumin-loaded super-paramagnetic iron oxide (Fe3O4) nanoparticles. So, the apoptotic death of granulosa cells and interstitial tissue was diminished after curcumin therapy [20] (Table 1).
Sex Hormones
An increment of the levels of luteinizing hormone (LH) and insulin can increase androgen production and lead to impairment of ovarian follicle development and PCOS. Elevation of the serum LH/follicle-stimulating hormone (FSH) ratio is also the main characteristic of PCOS women [38]. Five of the included animal studies analyzed the effects of curcumin on the serum sex hormone levels of animals with PCOS. These studies reported the attenuation of LH [34, 35, 38] and testosterone [24, 32, 35] and augmentation of FSH [34, 35, 38], estradiol [24, 32], and progesterone [24, 32, 34, 35] levels after curcumin therapy. Shahmoradi et al. also demonstrated a dose-dependently effect of curcumin on the increment of the uterine estrogen receptor α (ERα) gene expression in the animals with PCOS [36] (Table 1).
Two RCTs assessed the effects of curcumin on sex hormone levels in PCOS patients and reported no influence of this phytochemical on the LH and FSH levels [22, 38]. Asan et al. also detected no significant change in the DHEAS, sex hormone-binding globulin, and testosterone levels with 93.34 mg/day curcumin supplementation for 8 weeks [38]. Although, Heshmati et al. indicated the reduction of DHEA levels in the PCOS patients treated with 1500 mg/day curcumin for 12 weeks, after adjustment for basic value of the variable, treatment type, age, and BMI [22] (Table 2).
Glycemic Control
The effects of curcumin intake on the glycemic control of animals with PCOS were examined in four included studies [24, 32, 33, 36], and the reduction of fasting plasma glucose (FPG) [24, 32, 36], fasting insulin levels (FIL) [32, 33, 36], hemoglobin A1C (HbA1c) [24], or insulin resistance [32, 33, 36] were reported. Insulin resistance was assessed by calculation of homeostatic model assessment of insulin resistance (HOMA-IR) using the equation of [FPG (mg/dL) × FIL (µU/mL)]/405. Administration of curcumin at dose of 300 mg/kg also increased the quantitative insulin sensitivity check index (QUICKI), which was calculated by 1/(log(FIL µunit/mL) + log(FPG mg/dL)) formula [33]. Besides, Abuelezz et al. reported the increment of β cell functionality (HOMA-β%) with 50, 100, and 200 mg/kg of nanocurcumin, and also an improvement of the insulin sensitivity by the high doses (100 and 200 mg/kg). They also demonstrated dose-dependently augmentation of the pancreatic tissue integrity, islets area, and count of β-cells by the administration of nanocurcumin [32]. In the other study by Shahmoradi et al., an augmentation of the gene expression of glucose transporter 4 (GLUT4) was also reported after curcumin therapy of animals with PCOS [36] (Table 1).
In four included RCT investigations, the effects of curcumin supplementation on glycemic parameters were assessed in PCOS patients [22, 23, 37, 38]. Among them, three studies indicated the reduction of FPG [22, 23, 38], and two reported a decrease in FIL and HOMA-IR levels [23, 38] following curcumin administration compared to the placebo. Three studies [22, 23, 37] also evaluated QUICKI levels in PCOS women, which only one RCT reported increased QUICKI in women receiving 500 mg/day curcumin for 12 weeks [23]. Although, the GLUT-1 gene expression levels were not affected by 500 mg/day curcumin administration for 12 weeks, according to the study by Jamilian et al. [23] (Table 2).
Lipid Profile
Despite the heterogeneity in the methods of the included studies, all three investigations assessing the effects of curcumin on the lipid profile of animals with PCOS reported a significant decline in the serum triglyceride (TG), total cholesterol (TC), and low-density lipoprotein cholesterol (LDL-C) and also an increase in the high-density lipoprotein cholesterol (HDL-C) levels [24, 32, 35] (Table 1).
Three of the included RCTs examined the impact of curcumin supplementation on lipid profile in PCOS women [23, 37, 38]. Reduction of TC, LDL-C, and TC/HDL-C ratio and HDL-C increment were only demonstrated in one RCT in which supplementation with 500 mg/day curcumin was applied. The attenuation of LDL receptor (LDLR) gene expression after curcumin administration was also reported in this study [23] (Table 2).
Anthropometric Parameters
Three investigations have examined the effects of curcumin on body weight in the animal models of PCOS [34,35,36]. Among them, two studies reported a dose-dependently reduction of the PCOS-induced overweight with 100–400 mg/kg of curcumin administration [34, 36]. Although, there was no effect of 600 mg/kg curcumin injection on body weight in the other study [35] (Table 1).
All included RCTs evaluated the impact of curcumin on the anthropometric parameters in PCOS subjects [22, 23, 37, 38]. Of the four RCTs, two demonstrated the effects of curcumin at the dose of 93.34 or 500 mg/day and duration of 8 or 12 weeks, respectively, on body weight reduction [23, 38]. Although, BMI attenuation was reported only by 500-mg/day curcumin supplementation [23]. Moreover, from two articles assessing the effects of curcumin on waist circumference [22, 38] and body fat mass [37, 38], only one study reported beneficial effects [38] (Table 2).
Inflammation and Oxidative Stress
The anti-inflammatory and antioxidant potential effects of curcumin on the animal models of PCOS are assessed in four investigations [24, 32,33,34]. In these studies, curcumin dose-dependently suppressed inflammation by attenuating the levels of inflammatory biomarkers such as interleukin-6 (IL-6), C-reactive protein (CRP), and tumor necrosis factor-α (TNF-α) [32,33,34]. Moreover, an increment of the levels of antioxidant enzymes (superoxide dismutase (SOD), glutathione (GSH), and catalase), and a reduction of the lipid peroxidation marker malondialdehyde (MDA) were also reported after curcumin administration [24, 32] (Table 1).
The effects of curcumin on serum glutathione peroxidase (GPx) and SOD enzyme activities in PCOS women were assessed by only Heshmati et al. In this study, 1500-mg/day curcumin supplementation for 12 weeks increased serum activity of GPx [21]. Furthermore, high-sensitivity CRP (hs-CRP) and CRP were evaluated in two studies [37, 38], and only a significant reduction in CRP levels was detected in PCOS women following 93.34-mg/day curcumin supplementation for 8 weeks [38] (Table 2).
Other Outcomes
The downregulation of phosphoinositide 3-kinase (PI3K)/protein kinase B (AkT)/mammalian target of rapamycin (mTOR) pathway in the animal model of letrozole-induced PCOS was reported by Abuelezz et al. In this study, nanocurcumin administration increased the protein expression of the main players of the PI3K/AKT/mTOR pathway [32] (Table 1). Moreover, in two of the included RCTs, curcumin also upregulated the expression levels of peroxisome proliferator-activated receptor-γ (PPAR-γ) and PPAR-γ coactivator 1-α (PGC1-α) in the peripheral blood mononuclear cells of PCOS women [21, 23] (Table 2).
Discussion
In the present study, the available evidence concerning the influence of turmeric/curcumin supplementation on PCOS was reviewed. The included animal studies revealed the favorable effects of curcumin on PCOS. Furthermore, some of the included RCTs indicated improvement of hormonal disturbances, glycemic control, lipid profile, and anthropometric features in PCOS women. However, these beneficial effects were not supported in all reviewed RCTs.
Curcumin may improve hormonal profiles in PCOS condition by reducing oxidative stress, inflammation, ovarian androgen receptor proteins, and also targeting nuclear factor-erythroid 2 related factor 2 (Nrf2)/ heme oxygenase-1 (HO-1) and PI3K/Akt signaling pathways to attenuate apoptosis in granulosa cells [40,41,42]. Upregulation of PPAR-γ is another mechanism underlying the positive effects of curcumin on PCOS. PPAR-γ is a ligand-activated transcription factor playing crucial roles in the regulation of insulin sensitivity, energy metabolism, adipocyte differentiation, inflammation, and lipid metabolism [43]. Activation of PPAR-γ also contributes to the control of the synthesis of steroid hormones in the granulosa cells, follicle growth, and oocyte maturation [44]. Although, there are not sufficient clinical data regarding the effectiveness of curcumin on improvement of hormonal disturbances in PCOS women.
Raising the levels of free testosterone by lowering the liver synthesis of sex hormone-binding globulin levels [45, 46] and decreasing ovulation, conception, and pregnancy [47] occurs in the hyperinsulinemic condition. On the other hand, androgens may also contribute to insulin resistance in PCOS. Some studies are supporting the amelioration of the clinical and biochemical parameters of PCOS by improvement of insulin resistance [48]. The reviewed animal investigations in the present study suggested the insulin-sensitizing effects of curcumin in the animal models of PCOS [24, 32, 36]. Evidence suggests that these effects of curcumin are partly mediated by inhibition of hepatic glycogenolysis and gluconeogenesis and also increment of hepatic and peripheral glucose uptake. Stimulation of hepatic glucokinase, PPAR-γ, PGC1-α, AMP-activated protein kinase (AMPK), incretin secretion, lipid metabolism, and GLUT4 are some proposed mechanisms of curcumin in this regard [16, 23, 32, 36, 49, 50]. PGC1-α is a transcriptional coactivator involved in mitochondrial biogenesis, brown adipose tissue differentiation, glucose metabolism, thermogenesis, fatty acid oxidation, antioxidant defense, and insulin sensitivity [21, 51]. Most of the included RCTs also supported the beneficial effects of curcumin on reducing FPG in PCOS women. Although, data regarding insulin sensitivity was inconsistent and should be further investigated.
Dyslipidemia may promote the development of insulin resistance, oxidative stress, hyperandrogenism, and infertility. Besides, hyperandrogenism can also lead to lipid abnormalities [52]. Lipid profile improvement after curcumin therapy is reported in animals with PCOS [24, 32, 35]. In this line, a recent meta-analysis of RCTs reported that curcumin reduces blood lipid levels in patients suffering from different disorders, including metabolic syndromes, type 2 diabetes, non-alcoholic fatty liver disease, chronic kidney disease, and obesity. The lipid-lowering impact of curcumin could be mediated by its inhibitory effects on cholesterol esterification, cholesterol uptake in the intestine, cholesterol biosynthesis, and TG deposition in the liver [53]. Nevertheless, most of the currently available RCTs did not support the influence of curcumin on lipid profile in PCOS women, and more studies in this field are necessary.
There is a bi-directional relationship between obesity and PCOS. Hyperandrogenism may cause visceral adiposity in PCOS women. Meanwhile, reproductive and metabolic disturbances such as insulin resistance, hyperandrogenism, and anovulation are more common in obese women, even independent of PCOS diagnosis [54, 55]. Curcumin supplementation is supposed to ameliorate fat mass and obesity by increasing energy expenditure, lipolysis, and AMPK and PGC1-α expression. Inhibition of the inflammatory and oxidant pathways, adipocyte differentiation, Janus kinase, and 11β-hydroxysteroid dehydrogenase type 1 enzyme are also other proposed mechanisms for the anti-obesity effects of curcumin [15, 56]. Nonetheless, the included animal studies and RCTs revealed inconsistent results regarding the effects of curcumin on anthropometric features in PCOS that should be more investigated in future examinations.
Amelioration of inflammation and oxidative stress can improve the complications of PCOS, especially insulin resistance [8, 57]. In this study, curcumin showed its robust anti-inflammatory and antioxidant effects in the animal models of PCOS by lowering IL-6, CRP, TNF-α, and MDA and also increasing SOD, GSH, and catalase [24, 32, 34]. However, only GPX and CRP, but not SOD and hs-CRP, were affected by curcumin in the included RCTs [21, 37, 38]. Upregulation of PPAR-γ, PGC1-α, and Nrf2/HO-1 pathway and down-regulation of nuclear factor kappa B, activator protein-1, and signal transducer and activator of transcription (STAT) proteins are some suggested mechanisms for anti-inflammatory and antioxidant properties of curcumin [21, 23, 40, 58,59,60].
The most important limitation of this systematic review was the small number of trials that prohibited performing a meta-analysis. Second, although all reviewed RCTs were conducted on obese/overweight PCOS patients, there was considerable heterogeneity regarding curcumin dose, duration of investigations, sample sizes, and age of patients. Third, most of the included studies were conducted in Iran, and therefore, the findings are not generalizable to other populations and may cause possible bias.
Conclusion
Animal studies underlined the potential effects of curcumin on the management of hormonal and metabolic disturbances related to PCOS. Reducing oxidative stress, inflammation, and Nrf2/HO-1 and PI3K/Akt signaling pathways and stimulation of hepatic glucokinase, PPAR-γ, PGC1-α, AMPK, and incretin secretion are some proposed mechanisms related to the observed effects. Although present clinical literature is limited to conclude the beneficial effects of curcumin on the management of PCOS symptoms. Further well-designed RCTs with longer duration and higher doses of curcumin, especially bioavailability-improved formulations, are warranted to be performed on PCOS women. Besides, mechanistic examinations on the effects of curcumin on this syndrome are also suggested.
Availability of Data and Materials
Not applicable.
Code availability
Not applicable.
Abbreviations
- AMPK:
-
AMP-activated protein kinase
- AkT:
-
Protein kinase B
- BMI:
-
Body mass index
- Bax:
-
B-cell lymphoma 2 (Bcl2)-associated X protein
- CRP:
-
C-reactive protein
- CI:
-
Confidence intervals
- ERα:
-
Estrogen receptor α
- FSH:
-
Follicle-stimulating hormone
- FPG:
-
Fasting plasma glucose
- FIL:
-
Fasting insulin levels
- GLUT:
-
Glucose transporter
- GPX:
-
Glutathione peroxidase
- GSH:
-
Glutathione
- HbA1c:
-
Hemoglobin A1C
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- HDL-C:
-
High-density lipoprotein cholesterol
- hs-CRP:
-
High-sensitivity CRP
- HO-1:
-
Heme oxygenase-1
- IL-6:
-
Interleukin-6
- LH:
-
Luteinizing hormone
- LDL-C:
-
Low-density lipoprotein cholesterol
- LDLR:
-
LDL receptor
- MD:
-
Mean difference
- MDA:
-
Malondialdehyde
- mTOR:
-
Mammalian target of rapamycin
- Nrf2:
-
Nuclear factor-erythroid 2-related factor 2
- PCOS:
-
Polycystic ovary syndrome
- PI3K:
-
Phosphoinositide 3-kinase
- PPAR-γ:
-
Peroxisome proliferator-activated receptor-γ
- PGC1-α:
-
PPAR-γ coactivator 1-α
- QUICKI:
-
Quantitative insulin sensitivity check index
- RCTs:
-
Randomized placebo-controlled clinical trials
- SOD:
-
Superoxide dismutase
- STAT:
-
Signal transducer and activator of transcription
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- TNF-α:
-
Tumor necrosis factor-α
References
Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020;35:100937.
Boomsma CM, Fauser BC, Macklon NS, editors. Pregnancy complications in women with polycystic ovary syndrome. Semin Reprod Med. 2008: © Thieme Medical Publishers.
Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016;106(1):6–15.
ESHRE TR, Group A-SPCW. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Amiri M, Tehrani FR, Behboudi-Gandevani S, Bidhendi-Yarandi R, Carmina E. Risk of hypertension in women with polycystic ovary syndrome: a systematic review, meta-analysis and meta-regression. Reprod Biol Endocrinol. 2020;18(1):1–15.
Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37(5):467–520.
Mohammadi M. Oxidative stress and polycystic ovary syndrome: a brief review. Int J Prev Med. 2019;10.
González F. Inflammation in polycystic ovary syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids. 2012;77(4):300–5.
Liao Y-N, Hu W-L, Hung Y-C. Complementary therapy with traditional Chinese medicine for polycystic ovarian syndrome. Debatable Topics in PCOS Patients: IntechOpen; 2017.
Arentz S, Abbott JA, Smith CA, Bensoussan A. Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings. BMC Complement Altern Med. 2014;14(1):511.
Hatcher H, Planalp R, Cho J, Torti F, Torti S. Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci. 2008;65(11):1631–52.
Prasad S, Aggarwal BB. Turmeric, the golden spice: from traditional medicine to modern medicine. chapter; 2011.
Araujo C, Leon L. Biological activities of Curcuma longa L. Mem Inst Oswaldo Cruz. 2001;96(5):723–8.
Hewlings SJ, Kalman DS. Curcumin: a review of its’ effects on human health. Foods. 2017;6(10):92.
Mousavi SM, Milajerdi A, Varkaneh HK, Gorjipour MM, Esmaillzadeh A. The effects of curcumin supplementation on body weight, body mass index and waist circumference: a systematic review and dose-response meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2020;60(1):171–80.
Poolsup N, Suksomboon N, Kurnianta PDM, Deawjaroen K. Effects of curcumin on glycemic control and lipid profile in prediabetes and type 2 diabetes mellitus: a systematic review and meta-analysis. PloS one. 2019;14(4):e0215840.
Hadi A, Pourmasoumi M, Ghaedi E, Sahebkar A. The effect of Curcumin/Turmeric on blood pressure modulation: a systematic review and meta-analysis. Pharmacol Res. 2019;150:104505.
Qin S, Huang L, Gong J, Shen S, Huang J, Ren H, et al. Efficacy and safety of turmeric and curcumin in lowering blood lipid levels in patients with cardiovascular risk factors: a meta-analysis of randomized controlled trials. Nutr J. 2017;16(1):68.
Tabrizi R, Vakili S, Akbari M, Mirhosseini N, Lankarani KB, Rahimi M, et al. The effects of curcumin-containing supplements on biomarkers of inflammation and oxidative stress: a systematic review and meta-analysis of randomized controlled trials. Phytother Res. 2019;33(2):253–62.
Abhari SMF, Khanbabaei R, Roodbari NH, Parivar K, Yaghmaei P. Curcumin-loaded super-paramagnetic iron oxide nanoparticle affects on apoptotic factors expression and histological changes in a prepubertal mouse model of polycystic ovary syndrome-induced by dehydroepiandrosterone-a molecular and stereological study. Life Sci. 2020:117515.
Heshmati J, Golab F, Morvaridzadeh M, Potter E, Akbari-Fakhrabadi M, Farsi F, et al. The effects of curcumin supplementation on oxidative stress, sirtuin-1 and peroxisome proliferator activated receptor γ coactivator 1α gene expression in polycystic ovarian syndrome (PCOS) patients: a randomized placebo-controlled clinical trial. Diabetes Metab Syndr. 2020;14(2):77–82.
Heshmati J, Moini A, Sepidarkish M, Morvaridzadeh M, Salehi M, Palmowski A, et al. Effects of curcumin supplementation on blood glucose, insulin resistance and androgens in patients with polycystic ovary syndrome: a randomized double-blind placebo-controlled clinical trial. Phytomedicine. 2020:153395.
Jamilian M, Foroozanfard F, Kavossian E, Aghadavod E, Shafabakhsh R, Hoseini A, et al. Effects of curcumin on body weight, glycemic control and serum lipids in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Clin Nutr ESPEN. 2020.
Reddy PS, Begum N, Mutha S, Bakshi V. Beneficial effect of Curcumin in Letrozole induced polycystic ovary syndrome. Asian Pac J Reprod. 2016;5(2):116–22.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
Program NT. Handbook for conducting a literature-based health assessment using OHAT approach for systematic review and evidence integration. Office of Health Assessment and Translation (OHAT), Division of the National Toxicology Program, National Institute of Environmental Health Sciences. 2015. https://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookjan2015_508.pdf.
Tarsilla M. Cochrane handbook for systematic reviews of interventions. J Multidiscip Eval. 2010;6(14):142–8.
Suh M, Wikoff D, Lipworth L, Goodman M, Fitch S, Mittal L, et al. Hexavalent chromium and stomach cancer: a systematic review and meta-analysis. Crit Rev Toxicol. 2019;49(2):140–59.
Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration. www cochrane-handbook org. 2011.
White CM, Pasupuleti V, Roman YM, Li Y, Hernandez AV. Oral turmeric/curcumin effects on inflammatory markers in chronic inflammatory diseases: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2019;146:104280.
Vaghef-Mehrabany E, Maleki V, Behrooz M, Ranjbar F, Ebrahimi-Mameghani M. Can psychobiotics “mood” ify gut? An update systematic review of randomized controlled trials in healthy and clinical subjects, on anti-depressant effects of probiotics, prebiotics, and synbiotics. Clin Nutr. 2020;39(5):1395–410.
Abuelezz NZ, Shabana ME, Abdel-Mageed HM, Rashed L, Morcos GN. Nanocurcumin alleviates insulin resistance and pancreatic deficits in polycystic ovary syndrome rats: Insights on PI3K/AkT/mTOR and TNF-α modulations. Life Sci. 2020;256:118003.
Mohammadi S, Bardei LK, Hojati V, Ghorbani A, Nabiuni M. Anti-inflammatory effects of curcumin on insulin resistance index, levels of interleukin-6, C-reactive protein, and liver histology in polycystic ovary syndrome-induced rats. Cell J (Yakhteh). 2017;19(3):425.
Mohammadi S, Kayedpoor P, Karimzadeh-Bardei L, Nabiuni M. The effect of curcumin on TNF-α, IL-6 and CRP expression in a model of polycystic ovary syndrome as an inflammation state. J Reprod Infertil. 2017;18(4):352.
Raoofi A, Amini A, Farahani RM. The synergistic effect of curcumin and ziziphora extract due to their anti-inflammatory and antioxidant properties on ovarian tissue follicles. J Pharm Res Int. 2018:1–11.
Shahmoradi MK, Askaripour M, Rajabi S, Dzigandzli G. Beneficial effects of curcumin on rats with polycystic ovary syndrome: evaluation of the gene expression of GLUT4, Erα and insulin resistance. GMJ Med. 2018;2(1):80–7.
Sohaei S, Amani R, Tarrahi MJ, Ghasemi-Tehrani H. The effects of curcumin supplementation on glycemic status, lipid profile and hs-CRP levels in overweight/obese women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled clinical trial. Complement Ther Med. 2019;47:102201.
Asan SA, Bas M, Eren B, Karaca E. The effects of curcumin supplementation added to diet on anthropometric and biochemical status in women with polycystic ovary syndrome: a randomized, placebo-controlled trial. Prog Nutr. 2020;22(4).
Alibraheemi NA, Bustani GS, Al-Dhaliny AM. Effect of curcumin on LH and FSH hormones of polycystic syndrome induced by letrozole in female rats. Lat Am J Pharm. 2021;179–183.
Yan Z, Dai Y, Fu H, Zheng Y, Bao D, Yin Y, et al. Curcumin exerts a protective effect against premature ovarian failure in mice. J Mol Endocrinol. 2018;60(3):261–71.
Choi H, Lim J, Hong J. Curcumin interrupts the interaction between the androgen receptor and Wnt/β-catenin signaling pathway in LNCaP prostate cancer cells. Prostate Cancer Prostatic Dis. 2010;13(4):343–9.
Shi Q, Shih C-Y, Lee K. Novel anti-prostate cancer curcumin analogues that enhance androgen receptor degradation activity. Anti-Cancer Agents in Medicinal Chemistry (Formerly Current Medicinal Chemistry-Anti-Cancer Agents). 2009;9(8):904–12.
Janani C, Kumari BR. PPAR gamma gene–a review. Diabetes Metab Syndr. 2015;9(1):46–50.
Vitti M, Di Emidio G, Di Carlo M, Carta G, Antonosante A, Artini PG, et al. Peroxisome proliferator-activated receptors in female reproduction and fertility. PPAR research. 2016;2016.
Polak K, Czyzyk A, Simoncini T, Meczekalski B. New markers of insulin resistance in polycystic ovary syndrome. J Endocrinol Invest. 2017;40(1):1–8.
Fica S, Albu A, Constantin M, Dobri GA. Insulin resistance and fertility in polycystic ovary syndrome. J Med Life. 2008;1(4):415.
Zhang D, Yang X, Li J, Yu J, Wu X. Effect of hyperinsulinaemia and insulin resistance on endocrine, metabolic and fertility outcomes in women with polycystic ovary syndrome undergoing ovulation induction. Clin Endocrinol. 2019;91(3):440–8.
Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012;33(6):981–1030.
Kato M, Nishikawa S, Ikehata A, Dochi K, Tani T, Takahashi T, et al. Curcumin improves glucose tolerance via stimulation of glucagon-like peptide-1 secretion. Mol Nutr Food Res. 2017;61(3):1600471.
Pan Y, Zhao D, Yu N, An T, Miao J, Mo F, et al. Curcumin improves glycolipid metabolism through regulating peroxisome proliferator activated receptor γ signalling pathway in high-fat diet-induced obese mice and 3T3-L1 adipocytes. R Soc Open Sci. 2017;4(11):170917.
Cheng C-F, Ku H-C, Lin H. PGC-1α as a pivotal factor in lipid and metabolic regulation. Int J Mol Sci. 2018;19(11):3447.
Liu Q, Xie Y-J, Qu L-H, Zhang M-X, Mo Z-C. Dyslipidemia involvement in the development of polycystic ovary syndrome. Taiwan J Obstet Gynecol. 2019;58(4):447–53.
Saeedi F, Farkhondeh T, Roshanravan B, Amirabadizadeh A, Ashrafizadeh M, Samarghandian S. Curcumin and blood lipid levels: an updated systematic review and meta-analysis of randomised clinical trials. Arch Physiol Biochem. 2020:1–0.
Sam S. Obesity and polycystic ovary syndrome. Obes Manag. 2007;3(2):69–73.
Beatriz MA. The role of obesity in the development of polycystic ovary syndrome. Curr Pharm Des. 2012;18(17):2482–91.
Bradford PG. Curcumin and obesity. BioFactors. 2013;39(1):78–87.
Amini L, Tehranian N, Movahedin M, Tehrani FR, Ziaee S. Antioxidants and management of polycystic ovary syndrome in Iran: a systematic review of clinical trials. Iran J Reprod Med. 2015;13(1):1.
Sahebkar A, Cicero AF, Simental-Mendía LE, Aggarwal BB, Gupta SC. Curcumin downregulates human tumor necrosis factor-α levels: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016;107:234–42.
Loboda A, Damulewicz M, Pyza E, Jozkowicz A, Dulak J. Role of Nrf2/HO-1 system in development, oxidative stress response and diseases: an evolutionarily conserved mechanism. Cell Mol Life Sci. 2016;73(17):3221–47.
Heming M, Gran S, Jauch S-L, Fischer-Riepe L, Russo A, Klotz L, et al. Peroxisome proliferator-activated receptor-γ modulates the response of macrophages to lipopolysaccharide and glucocorticoids. Front Immunol. 2018;9:893.
Acknowledgements
We thank the Nutrition Research Center of Tabriz University of Medical Sciences, Tabriz, Iran (Grant number: 66590).
Funding
This work was approved and supported by the vice-chancellor and the Nutrition Research Center of Tabriz University of Medical Sciences (Grant Number: 66590).
Author information
Authors and Affiliations
Contributions
All authors conceived the original idea of this review and contributed to the development of the search strategy, inclusion and exclusion criteria, and data extraction form. Dr. S.S.Z. and R.M.G. determined the eligibility of papers and evaluated the risk of bias, and Dr. M.R. was the third reviewer. Dr. S.S.Z and R.M.G. wrote the manuscript, and Dr. S.S.Z. extracted data. Dr. M.R. supervised the project and helped to revise and proofread the manuscript. All authors have approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shojaei-Zarghani, S., Molani-Gol, R. & Rafraf, M. Curcumin and Polycystic Ovary Syndrome: a Systematic Review. Reprod. Sci. 29, 2105–2118 (2022). https://doi.org/10.1007/s43032-021-00826-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00826-6