Abstract
Repeated implantation failure (RIF) is a disorder in which good-quality embryos fail to implant in the endometrium following several in vitro fertilization (IVF) cycles. This study aimed to evaluate the efficiency and safety of intrauterine infusion of platelet-rich plasma (PRP) in improvement of pregnancy outcomes in RIF patients undergoing frozen embryo transfer (FET). A total of 438 women with a history of RIF undergoing FET were assessed for eligibility to enter the study. Patients were randomly assigned to the intervention (PRP) and control groups. The intervention group received an intrauterine infusion of 0.5 ml PRP 48 h before embryo transfer while the control group received standard treatment. The rates of chemical and clinical pregnancy were defined as the primary outcome values. All women were followed up until the study endpoints that included the number of neonates born and pregnancy-related complications. Three hundred and ninety-three participants accomplished the study and their data were analyzed. The chemical pregnancy, clinical pregnancy, and live birth rates were higher in the PRP group than control group (p value: <0.0001; p value: <0.0001; p value: <0.0001 respectively). However, there were no significant differences between the two groups in terms of multiple pregnancies and pregnancy complications except for spontaneous abortion. The spontaneous abortion rate was significantly higher in the control group compared to the PRP group (p value = 0.0262). These results suggest that intrauterine infusion of PRP is an effective and safe route to improve pregnancy outcomes in RIF patients undergoing FET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent implantation failure (RIF) is a situation that is only applicable to patients experiencing assisted reproductive technology (ART) [1]. The most common definition for RIF refers to a status when a couple with a woman under the age of 40 fails to attain a clinical pregnancy after transfer of at least four good-quality embryos in three or more fresh or frozen cycles [1]. Because of variations in the definition of RIF, there is limited data on its incidence and potential risk factors. The overall occurrence of RIF has been estimated to be nearly 10% in intracytoplasmic sperm injection (ICSI) cycles [2]. Uterine and embryonic factors are involved in the pathophysiology of RIF [1, 2]. However, it can be speculated that in these couples, imperfection of the endometrium may be a likely cause for implantation failure [3, 4]. Concerning the factors which influence embryo implantation, various strategies have been developed for managing the RIF patients [2, 5]. Despite these efforts, there has been no significant improvement in the pregnancy rate of these patients in the last decade.
Platelet-rich plasma (PRP) is composed of a high concentration of autologous platelets extracted from the peripheral blood [6, 7]. Platelets are anucleated blood cells with numerous secretory granules accountable for the release of anti-inflammatory and proinflammatory cytokines, chemokines, and several growth factors (GFs) such as vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), insulin-like growth factor (IGF), basic fibroblast growth factor (b-FGF), and transforming growth factor-β1 (TGF-β1), and [8]. Amable et al. measured thirty-seven GFs and cytokines from different portions acquired during PRP preparation [9]. Due to the important roles of the mentioned GFs and cytokines in the embryonic implantation process [9, 10], intrauterine infusion of PRP has been recently introduced as a probable effective therapeutic approach for improving endometrial receptivity [11, 12]. Our previous studies showed that the local administration of PRP is an effective approach in the improvement of chemical and clinical pregnancy rates in RIF patients [13, 14]. However, clinical evidence regarding the efficiency of PRP in improvement of pregnancy outcomes in women with history of RIF remains inadequate and its effect on the abortion rate and pregnancy complications has not been evaluated yet. In this regard, the present randomized controlled trial (RCT) aimed to assess the effect of PRP on pregnancy outcomes and complications in RIF patients.
Materials and Methods
Study Population
The present study was approved by the ethical committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran. Written informed consent was obtained from all the participants. The trial was registered at the Iranian Registry of Clinical Trials (IRCT2016072229027N1).
The study population included 438 RIF patients undergoing ICSI-frozen embryo transfer (FET) cycles, which was carried out at IVF center of Gandi Hospital, Tehran, Iran, between 2018 and 2020. All of the women had a history of failure to achieve pregnancy after three or more embryo transfers with high-quality embryos. Age between 18 and 38, body mass index (BMI) ≤30 kg/m2, and serum FSH level ≤10 mIU/ml on day 2 or 3 of the menstrual cycle were deemed as inclusion criteria. Patients with known etiologies of implantation failure including immunological abnormalities, inflammatory conditions, hormonal or anatomical disorders, polycystic ovary syndrome (PCOS), ovarian hyperstimulation syndrome (OHSS), endometriosis, presence of space-occupying lesions, history of miscarriage or ectopic pregnancy, myomas, polyps, adhesions, previous pelvic surgeries, failed fertilization, and less than two embryos available for transfer were all excluded. In addition, participants with severe male factor of their spouses and chromosomal abnormalities were excluded. In total, 45 patients were left out for different causes and 393 continued the study (Fig. 1).
Study Design
The study was a single-center, controlled trial with equal randomization, which was carried out in the IVF center of Gandhi Hospital, Tehran, Iran. Patients were accidentally allocated to one of two groups including PRP group or control group. Randomization was performed using computer-generated simple random tables in a 1:1 ratio. The sample size determination was done after consideration of type 1 statistical error <5% and type 2 statistical error <20%. Outcome assessors and statisticians were unaware about randomization.
Intrauterine Infusion of PRP
Forty-eight hours before blastocyst transfer, the intervention group received 0.5 ml of PRP through intrauterine infusion while the control group received only the standard treatment. PRP was infused into the uterine cavity with IUI catheter (Takwin, Iran). According to the manufacturer protocol of PRP kit (Arya Mabna Tashkhis, Iran) for preparation of PRP, 8.5 ml of autologous blood was drawn in a tube containing 1.5 ml of anticoagulant solution and centrifuged at 1200 rpm for 12 min to separate red blood cells. In second step, the harvested plasma was centrifuged at 3300 rpm for 5 min to acquire PRP, which contained platelet 4–5 times more than peripheral blood. As control for the concentration of the isolated platelets, the platelets were quantified using automated hematology analyzer.
FET Cycle
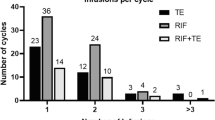
Ovarian stimulation of patients was accomplished by gonadotropin-releasing hormone (GnRH) antagonist protocol. Table 2 provides a summary of the ovarian stimulation characteristics and outcomes of the studied groups. All participants undertook FET cycle and hormone replacement therapy (HRT) was done for preparation of endometrium as a standard protocol. In brief, estradiol valerate (Aburaihan Co., Tehran, Iran) was initiated in a dose of 6 mg/d orally from the second (or third) day of the menstrual cycle and it was continued up to 8 mg if the endometrial thickness did not reach at least 7 mm. Progesterone suppository (Cyclogest; Actavis, England, UK) in a dose of 400 mg twice daily was initiated when the endometrial thickness was more than 7 mm. Blastocyst scoring was done according to the Gardner score [15, 16] as following: expansion score 0 = no cavity, score 1 = blastocoel cavity less than half volume of the embryo, score 2 = blastocoel cavity more than half volume of the embryo, score 3 = cavity completely filling the embryo, score 4 = cavity larger than the embryo and thinning zona, score 5 = hatching blastocyst; for inner cell mass (ICM), grade A = formed by many tightly packed cells, grade B = several loosely packed cells, grade C = few cells; for trophectoderm (TE), grade A = many cells forming a cohesive layer, grade B = few cells and loose layer, grade C = very few large cells. Good-quality blastocysts (expansion grades 2–3 and ICM and TE with AA classifications) on day 5 were transferred for all participants. It is important to note that the status of the chromosomes of the transferred embryos was unknown. The embryo transfers (ETs) were performed with embryo transfer catheter (Cook, USA) by an expert gynecologist with infertility fellowship under the trans-abdominal ultrasound guidance according to the American Society for Reproductive Medicine (ASRM) guidelines. According to the quality of the embryos and the condition of the females, 1–2 blastocysts were transferred in each cycle (Table 2).
Luteal Phase Support
Luteal phase support was performed by estradiol and progesterone supplementation for 2 weeks after FET. In patients with positive serum β-hCG, the luteal support was continued up to 12 weeks of pregnancy.
Outcome Assessment
Chemical pregnancy and clinical pregnancy were recognized by positive serum β-hCG after 2 weeks from the day of ET and the presence of fetal heartbeat in transvaginal ultrasound after 6 weeks from the day of ET, respectively [17]. Multiple pregnancies were determined as a conception with more than one fetus in ultrasonography. All women were followed up for the number of neonates born and pregnancy-related complications including gestation hypertension, gestational diabetes, pre-eclampsia, eclampsia, ectopic pregnancy, intrauterine growth restriction (IUGR), oligohydramnios, polyhydramnios, chorioamnionitis, peripheral edema, nausea, antepartum hemorrhage, premature rupture of the membranes (PROM), stillbirth, and spontaneous abortion.
Statistical Analysis
The results were shown as mean ± SD. GraphPad Prism (GraphPad Software, USA) was used to analyze all the obtained data. Student’s t-test, Exact test, and Chi-squared test were used for comparing the study groups. The p < 0.05 was considered as statistically significant.
Results
Baseline Characteristics
Based on the inclusion criteria, a total of 438 participants were enrolled in the study, from which 393 patients have completed the study and their data were analyzed (Fig. 1). The number of the patients, age, BMI, duration of infertility, type of infertility, number of previous ICSI or IVF-ET, hormone levels (FSH and AMH), and sperm concentration of spouse are shown in Table 1. There was no significant difference between the studied groups in these parameters. Table 2 provides ovarian stimulation characteristics and outcomes including total dose of administered gonadotropin, duration of gonadotropin administration, serum levels of luteinizing hormone (LH), estradiol (E2), and progesterone (P) on day of trigger, endometrial thickness and pattern on day of trigger, number of retrieved COCs, and number of blastocysts transferred for the studied groups. Based on the obtained data, there was no significant difference in these characteristics between the two groups.
Outcomes
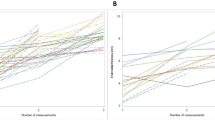
Overall comparison of pregnancy outcomes between the two study groups is presented in Table 4. The chemical pregnancy, clinical pregnancy, and live birth rates were higher in the PRP group than control group (p value: <0.0001; p value: <0.0001; p value: <0.0001 respectively). However, there were no significant differences between the two groups in term of multiple pregnancies (Table 4). Chemical pregnancy was 51.53% (101/196) for PRP group and 24.87% (49/197) for control group. Clinical pregnancy was 48.97% (96/196) for PRP group and 19.28% (38/197) for control group. Multiple pregnancy was 3.06% (6/196) for PRP group and 1.01% (2/197) for control group. Live birth was 39.28% (77/196) for PRP group and 5.58% (11/197) for control group.
There was no significant difference in occurrence of pregnancy complications including anemia, gestational hypertension, pre-eclampsia, eclampsia, gestational diabetes, ectopic pregnancy, IUGR, oligohydramnios, polyhydramnios, chorioamnionitis, peripheral edema, antepartum hemorrhage, PROM, and stillbirth (Table 3). However, the spontaneous abortion rate was significantly higher in the control group compared to the PRP group (p value = <0.0001).
Discussion
The present study showed that intrauterine infusion of PRP significantly increased the chemical pregnancy, clinical pregnancy and live birth rates in RIF patients. In addition, PRP infusion significantly decreased the spontaneous abortion rate in these patients. To the best of our knowledge, this is the first study which followed up the RIF patients who received PRP infusion prior to ET in ICSI/FET cycles until parturition. No pregnancy-related complications were observed during this study.
Successful embryo implantation depends on component embryo and receptive endometrium [18]. Indeed, implantation is a very complicated process regulated by a number of complex molecules such as hormones, cytokines, and growth factors which play together to induce endometrial receptivity for embryo at blastocyst stage [18]. Growing data show that PRP infusion is an effective approach for the improvement of pregnancy outcomes in the patients undergoing IVF/ICSI cycles, mostly in women who were not able to respond to the standard treatment [12, 19, 20]. Since various studies have demonstrated that the expression of growth factors in the endometrium of women with RIF is less than normal fertile women, local infusion of PRP which contains several growth factors and cytokines may improve endometrial receptivity and embryo implantation [18, 21].
The exact mechanism of action of PRP in enhancing pregnancy outcomes is not yet well understood. However, the regulation of immunological interactions between the embryo and the endometrium at the time of the implantation window is the most relevant theory that can explain the positive effect of PRP in cases with RIF [22, 23]. In order to prevent fetal rejection, the endometrial environment should be transformed to an anti-inflammatory state in the mid-secretory phase [22, 23]. PRP can modulate the secretion of some important inflammatory cytokines required for embryo implantation process such as interleukin (IL)-6, IL-8, and IL1-β [11]. Herein, the obtained data manifested the increase of pregnancy rate and decrease of spontaneous abortion rate in PRP group in comparison to control group. One possible explanation for these results is the immunomodulatory properties of PRP which can affect maternal-fetal communication positively beyond the early phase of implantation and throughout the pregnancy. Indubitably, more studies are needed to allow a better understanding of the exact mechanisms involved in the effect of PRP on maternal immune system.
Intrauterine PRP infusion may possibly affect the gene expression pattern of the endometrial cells. For instance, Marini et al. revealed that the expression of progesterone receptor was higher in endometrial biopsies of cows treated with PRP infusion [24]. Progesterone plays a critical role in establishment and maintenance of pregnancy [4]. Embryo growth and development require the action of progesterone through its receptor inside the endometrium, as the maternal-fetal interactions, pregnancy recognition, and uterine receptivity are all regulated by the action of progesterone [4]. Recently, Hosseinirad et al. showed that the expression of progesterone receptor is impaired in the endometrium of RIF patients [25]. Based on this available evidence, the effect of PRP on gene expression of endometrial cells can be considered as another mechanism in improving the pregnancy rate and reducing the spontaneous abortion rate and subsequently increasing the live birth rate.
To achieve successful implantation, following cyclic endometrial breakdown and shedding, endometrium completely regenerates and proliferates [26]. This multipart organization is based on migration, proliferation, and differentiation of mesenchymal cell to epithelial cell by means of several growth factors, chemokines, and proinflammatory cytokines [26]. It was found that the presence of fibrin framework over platelets supports the renewing matrix and causes rapid organization of the accurate morphological and molecular arrangements for wound healing [27, 28]. Several studies demonstrated that endometrial thickness and implantation rate were increased after intrauterine PRP infusion [6]. Similar to our previous study, Chang et al. demonstrated that PRP is able to stimulate the endometrial growth and improve pregnancy outcomes of women with thin endometrium [10, 29]. Definitely, PRP growth factors act synergistically to increase the infiltration of neutrophils and macrophages; to elevate angiogenesis, matrix deposition, and fibroplasia; and eventually induce the tissue regeneration [24, 30]. In clinical practice, the optimal endometrial thickness for embryo transfer should be > 7 mm at the end of follicular phase [26]. As the endometrial thickness was greater than 7 mm in the studied groups, the effect of PRP on pregnancy outcomes in the present study may possibly happen through other mentioned mechanisms.
The results of present study are in line with our previous studies which are published in 2016 [13] and 2019 [14] showing that PRP is an effective approach in improvement of pregnancy outcomes in RIF patients. The strengths of the present research are a large number of participants with possibly known insufficiencies of the endometrium. Furthermore, the pregnancy complications were evaluated so that no abnormal clinical symptoms were observed during the study. Most patients experienced mild complications after pregnancy commonly mild hypertension, mild anemia, mild bleeding (mostly spotting during the first trimester), mild gastrointestinal problems such as nausea, mild peripheral edema, mild antepartum hemorrhage, and controlled pre-eclampsia. Although the safety of PRP in numerous clinical practices has been shown [31,32,33], there is lack of evidence regarding the safety of intrauterine infusion of PRP and possible adverse effects of it on pregnancy-related outcomes. Based on our research, no adverse events have been reported yet during intrauterine infusion of PRP. Since PRP is prepared from autologous peripheral blood, probably there are negligible risks for pregnancy complications, immunogenic reactions, cancers, and disease transmission [10]. In addition, autologous PRP requires no culture and is characterized by ease of preparation and high safety.
In the present study, three-fold increase in the occurrence of multiple pregnancy in PRP group versus control group was not statistically significant but it is not ignorable. To increase the chance of embryo implantation, especially in RIF patients, clinics usually transfer more than one embryo to the uterus. This can lead to increased chance of multiple pregnancy and its associated adverse effects. Number, quality, and developmental stage of the transferred embryos, and the used strategies for improvement of embryo implantation rate, such as intrauterine infusion of PRP, can all have effect on the likelihood of multiple pregnancy. Based on this, single top-quality embryo transfer strategy is always recommended in case the adjuvant therapies such as PRP are going to be used [34].
Studies regarding clinical efficiency of PRP are not conclusive, possibly due to the differences in PRP preparation methods. PRP is being prepared using different protocols, sometimes without even controlling the precise concentration and the activation status of the isolated platelets [35]. Another issue that is not even mentioned in clinical reports is whether there is a correlation between the platelet concentration and its effects. Studies have already shown that low platelet concentration is inefficient and that high concentrations have an adverse effect on cell growth, but results are still contradictory [36]. Although still not deeply characterized, the leukocyte content was also shown to be an important factor, which should be avoided in PRP preparations because of their potential proinflammatory effect [36].
Several limitations should be considered in the interpretation of the obtained results in the present study. First, the control group did not receive a saline infusion as an internal control for PRP infusion. The effect of scratching during catheter insertion should be also considered. Some researchers showed the beneficial effects of endometrial scratching in RIF patients [37]; however, this result is controversial [38, 39]. Second, possible dose-response effect of PRP was not evaluated in this study. Exact platelet concentration and the content of growth factors must be defined in order to understand molecular mechanisms behind PRP.
Despite the extensive use of PRP in numerous clinical practices, its use in the field of reproductive medicine is limited [14, 40]. Therefore, further studies including clinical trials and systematic reviews are required to provide enough evidence about the efficiency and safety of PRP infusion for improvement of pregnancy outcomes in patients undergoing IVF/ICSI cycles. In addition, in vitro studies are required to unveil the molecular mechanisms involved in beneficial effects of PRP on the endometrial receptivity.
Conclusion
According to the results obtained in this study, it seems that intrauterine infusion of PRP in infertile women with RIF undergoing ICSI/FET cycles can lead to increased pregnancy and live birth rates with controllable pregnancy complications. We should clearly state that intrauterine infusion of PRP is an experimental method and further studies are needed to corroborate a therapeutic potential application of it for improving pregnancy outcomes in RIF patients.
Data Availability
The data that support the findings of this study are available from IVF center.
Code Availability
Not applicable.
References
Coughlan C, Ledger W, Wang Q, Liu F, Demirol A, Gurgan T, et al. Recurrent implantation failure: definition and management. Reprod BioMed Online. 2014;28(1):14–38. https://doi.org/10.1016/j.rbmo.2013.08.011.
Magdi Y, El-Damen A, Fathi AM, Abdelaziz AM, Youssef MA-E, Abd-Allah AA-E, et al. Revisiting the management of recurrent implantation failure through freeze-all policy. Fertil Steril. 2017;108(1):72–7.
Timeva T, Shterev A, Kyurkchiev S. Recurrent implantation failure: the role of the endometrium. J Reprod Infertil. 2014;15(4):173–83.
Hosseinirad H, Novin MG, Hosseini S, Nazarian H, Amidi F, Paktinat S, et al. Effect of 1, 25 (OH) 2-vitamin D3 on expression and phosphorylation of progesterone receptor in cultured endometrial stromal cells of patients with repeated implantation failure. Acta Histochem. 2020;122(2):151489.
Bashiri A, Halper KI, Orvieto R. Recurrent Implantation failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol. 2018;16(1):121. https://doi.org/10.1186/s12958-018-0414-2.
Semsarzadeh N, Khetarpal S. Platelet-rich plasma and stem cells for hair growth: a review of the literature. Aesthet Surg J. 2020;40(4):NP177–NP88.
Alves R, Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord. 2018;4(1):18–24. https://doi.org/10.1159/000477353.
Cavalcante MB, Cavalcante CTMB, Sarno M, Barini R. Intrauterine perfusion immunotherapies in recurrent implantation failures: systematic review. Am J Reprod Immunol. 2020;83(6):e13242.
Amable PR, Carias RBV, Teixeira MVT, da Cruz Pacheco I, Corrêa do Amaral RJF, Granjeiro JM, et al. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther. 2013;4(3):67. https://doi.org/10.1186/scrt218.
Chang Y, Li J, Chen Y, Wei L, Yang X, Shi Y, et al. Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med. 2015;8(1):1286–90.
Maleki-Hajiagha A, Razavi M, Rouholamin S, Rezaeinejad M, Maroufizadeh S, Sepidarkish M. Intrauterine infusion of autologous platelet-rich plasma in women undergoing assisted reproduction: a systematic review and meta-analysis. J Reprod Immunol. 2020;137:103078.
Zamaniyan M, Peyvandi S, Heidaryan Gorji H, Moradi S, Jamal J, Yahya Poor Aghmashhadi F, Hossein Mohammadi M. Effect of platelet-rich plasma on pregnancy outcomes in infertile women with recurrent implantation failure: a randomized controlled trial. Gynaecol Endocrinol. 2021;37(2):141–5.
Nazari L, Salehpour S, Hoseini S, Zadehmodarres S, Ajori L. Effects of autologous platelet-rich plasma on implantation and pregnancy in repeated implantation failure: a pilot study. Int J Reprod BioMed. 2016;14(10):625–8.
Nazari L, Salehpour S, Hosseini MS, Hashemi Moghanjoughi P. The effects of autologous platelet-rich plasma in repeated implantation failure: a randomized controlled trial. Hum Fertil. 2020;23(3):209–13.
Wirleitner B, Schuff M, Stecher A, Murtinger M, Vanderzwalmen P. Pregnancy and birth outcomes following fresh or vitrified embryo transfer according to blastocyst morphology and expansion stage, and culturing strategy for delayed development. Hum Reprod. 2016;31(8):1685–95.
Jansen R, Mortimer D. Towards reproductive certainty: fertility and genetics beyond 1999: the plenary Proceedings of the 11th World Congress. CRC Press; 1999.
Zeadna A, Son WY, Moon JH, Dahan MH. A comparison of biochemical pregnancy rates between women who underwent IVF and fertile controls who conceived spontaneously†. Hum Reprod. 2015;30(4):783–8. https://doi.org/10.1093/humrep/dev024.
Singh M, Chaudhry P, Asselin E. Bridging endometrial receptivity and implantation: network of hormones, cytokines, and growth factors. J Endocrinol. 2011;210(1):5–14. https://doi.org/10.1530/JOE-10-0461.
Allahveisi A, Seyedoshohadaei F, Rezaei M, Bazrafshan N, Rahimi K. The effect of platelet-rich plasma on the achievement of pregnancy during frozen embryo transfer in women with a history of failed implantation. Heliyon. 2020;6(3):e03577.
Rageh K, Barakat AA-A, Ahmed KG, Ahmed AM. PRP in recurrent implantation failure, hope or hype? A prospective randomized controlled study. Evid Based Women's Health J. 2020;10(1):46–53.
Rajaei S, Zamani AH, Jeddi-Tehrani M, Tavakoli M, Mohammadzadeh A, Dabbagh A, et al. Cytokine profile in the endometrium of normal fertile and women with repeated implantation failure. Iran J Immunol. 2011;8(4):201–8.
Griffith OW, Chavan AR, Protopapas S, Maziarz J, Romero R, Wagner GP. Embryo implantation evolved from an ancestral inflammatory attachment reaction. Proc Natl Acad Sci. 2017;114(32):E6566–E75.
Mor G, Cardenas I, Abrahams V, Guller S. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann N Y Acad Sci. 2011;1221(1):80–7.
Marini MG, Perrini C, Esposti P, Corradetti B, Bizzaro D, Riccaboni P, et al. Effects of platelet-rich plasma in a model of bovine endometrial inflammation in vitro. Reprod Biol Endocrinol. 2016;14(1):1–17.
Hosseinirad H, Novin MG, Hosseini S, Nazarian H, Safaei Z, Hashemi T, et al. Evaluation of expression and phosphorylation of progesterone receptor in endometrial stromal cells of patients with recurrent implantation failure compared to healthy fertile women. Reprod Sci. 2021;28(5):1457–65.
Coksuer H, Akdemir Y, Ulas BM. Improved in vitro fertilization success and pregnancy outcome with autologous platelet-rich plasma treatment in unexplained infertility patients that had repeated implantation failure history. Gynecol Endocrinol. 2019;35(9):815–8.
Samy A, Abbas AM, Elmoursi A, Elsayed M, Hussein RS. Effect of autologous platelet-rich plasma transfusion in the treatment of infertile women with thin endometrium and its implications in IVF cycles: a literature review. Middle East Fertil Soc J. 2020;25(1):5.
Sundman EA, Cole BJ, Karas V, Della Valle C, Tetreault MW, Mohammed HO, et al. The anti-inflammatory and matrix restorative mechanisms of platelet-rich plasma in osteoarthritis. Am J Sports Med. 2014;42(1):35–41.
Nazari L, Salehpour S, Hoseini S, Zadehmodarres S, Azargashb E. Effects of autologous platelet-rich plasma on endometrial expansion in patients undergoing frozen-thawed embryo transfer: a double-blind RCT. Int J Reprod Biomed. 2019;17(6):443–8. https://doi.org/10.18502/ijrm.v17i6.4816.
Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91(01):4–15.
Elnehrawy NY, Ibrahim ZA, Eltoukhy AM, Nagy HM. Assessment of the efficacy and safety of single platelet-rich plasma injection on different types and grades of facial wrinkles. J Cosmet Dermatol. 2017;16(1):103–11.
Fukawa T, Yamaguchi S, Akatsu Y, Yamamoto Y, Akagi R, Sasho T. Safety and efficacy of intra-articular injection of platelet-rich plasma in patients with ankle osteoarthritis. Foot Ankle Int. 2017;38(6):596–604.
Raeissadat SA, Karimzadeh A, Hashemi M, Bagherzadeh L. Safety and efficacy of platelet-rich plasma in treatment of carpal tunnel syndrome; a randomized controlled trial. BMC Musculoskelet Disord. 2018;19(1):1–6.
Monteleone PA, Peregrino PF, Baracat EC, Serafini PC. Transfer of 2 embryos using a double-embryo transfer protocol versus 2 sequential single-embryo transfers: the impact on multiple pregnancy. Reprod Sci. 2018;25(10):1501–8.
Fadadu PP, Mazzola AJ, Hunter CW, Davis TT. Review of concentration yields in commercially available platelet-rich plasma (PRP) systems: a call for PRP standardization. Reg Anesth Pain Med. 2019;44(6):652–9.
Amable PR, Carias RBV, Teixeira MVT, da Cruz PÍ. do Amaral RJFC, Granjeiro JM, et al. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther. 2013;4(3):1–13.
Van Hoogenhuijze N, Kasius J, Broekmans F, Bosteels J, Torrance H. Endometrial scratching prior to IVF; does it help and for whom? A systematic review and meta-analysis. Hum Reprod Open. 2019;2019(1):hoy025.
Lensen S, Venetis C, Ng EH, Young SL, Vitagliano A, Macklon NS, et al. Should we stop offering endometrial scratching prior to in vitro fertilization? Fertil Steril. 2019;111(6):1094–101.
Wadhwa L, Mishra M. Therapeutic efficacy of endometrial scratching in repeated controlled ovarian stimulation (COS) failure cycles. J Hum Reprod Sci. 2018;11(1):59–71.
Madhavan A, Naidu P, Rani KK, Kaur J, Mahajan N. Intrauterine autologous platelet-rich plasma therapy to improve implantation rates in patients undergoing frozen embryo transfer: a pilot study. Onco Fertil J. 2018;1(2):81.
Acknowledgements
We acknowledge all staffs who worked in IVF center at Gandi Hospital, Tehran, Iran, with especial thanks to Ms. Nahid Zadehnajaf, Ms. Mahnam Malakouti, and Ms. Marjan Nasirzadeh for their great help in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The present study was approved by the ethical committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran. The trial was registered at the Iranian Registry of Clinical Trials (IRCT2016072229027N1).
Consent to Participate
Written informed consent was obtained from all the participants.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nazari, L., Salehpour, S., Hosseini, S. et al. The Effects of Autologous Platelet-Rich Plasma on Pregnancy Outcomes in Repeated Implantation Failure Patients Undergoing Frozen Embryo Transfer: A Randomized Controlled Trial. Reprod. Sci. 29, 993–1000 (2022). https://doi.org/10.1007/s43032-021-00669-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00669-1