Abstract
Five to 10% of patients with stage IA, grade 1 or 2, endometrioid adenocarcinoma subsequently develop locoregional or distant recurrence. These patients have significantly reduced 5-year survival rates and salvage therapy success rates as low as 40%. The aim of this review is to highlight knowledge gaps that could further refine the risk categories of endometrial carcinoma (EC) and guide future randomized trials of adjuvant therapy for low-risk EC. A systematic search of the literature on PubMed and Medline was conducted using the following search terms: endometrial cancer, endometrial adenocarcinoma, endometrioid adenocarcinoma, low grade, early stage, stage IA, low risk, locoregional recurrence, and relapse. Relevant primary studies were extracted and included in this review. Risk factors for recurrence of low-risk EC were epidemiological (age, body mass index, ethnicity), molecular (DNA MMR, MSI, TP53 mutation and P53 defect, CTNNB1 mutation, PTEN and POLE mutation, L1CAM expression), pathological (positive peritoneal cytology, lymphovascular invasion, tumor size), and others like Ki67-percentage, micro-RNA expression, and hormonal receptor expression. CTNNB1 mutation, L1CAM expression, lymphovascular invasion, and tumor size were identified as significant risk factors for recurrence in low-risk EC. There are subsets of low-risk EC patients at high risk of recurrence and should be suspected when having the following risk factors: positive molecular markers, large tumor size, and lymphovascular invasion. A novel scoring system and randomized controlled trials should be conducted to identify these patients who will benefit most from adjuvant therapy to avoid recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Every year, around 400,000 new cases of endometrial cancer are reported worldwide. Not only is it the most common gynecological malignancy, but its incidence rates are also projected to further increase globally [1]. Endometrial cancer (EC) has traditionally been classified into two major histological subtypes since 1983 [2]. The majority of cases are classified as type I endometrioid EC which has a more favorable genetic and prognostic profile. For the purpose of management decisions, EC patients are further sub-classified by their risk of recurrence according to patient age, tumor size, FIGO staging, histological type and grade, and lymphovascular space involvement (LVSI) [3, 4].
In early-stage EC, adjuvant radiotherapy has been shown to reduce locoregional recurrence but does not improve overall survival [5], while adjuvant systemic therapy may prolong progression-free survival in patients with LVSI [6]. An ongoing phase II clinical trial is being conducted to assess the effect of adjuvant chemotherapy in early-stage node-negative EC (NCT01244789) [7]. Other studies have shown a trend towards improved survival with combination adjuvant chemoradiotherapy in early-stage EC [8, 9]. However, there is currently insufficient evidence to include adjuvant therapy in the management strategy of patients at low risk of recurrence (stage IA, grade 1 or 2, endometrioid adenocarcinoma) [10]. Despite being considered at low risk for disease relapse, 5–10% of these patients subsequently develop locoregional or distant recurrence. Unfortunately, these patients have significantly reduced 5-year survival rates and salvage therapy success rates as low as 40% [11,12,13,14]. Future risk stratification systems should be expanded to identify that particular subset of susceptible patients.
We are conducting this narrative review of the literature to identify risk factors for locoregional and/or distant recurrence after treatment of low-risk EC. The aim of this review is to highlight knowledge gaps that could further refine the risk categories of EC and guide future randomized trials of adjuvant therapy for low-risk EC.
Methods
A systematic search of the literature on PubMed and Medline was conducted using the following search terms: endometrial cancer, endometrial adenocarcinoma, endometrioid adenocarcinoma, low grade, early stage, stage IA, low risk, locoregional neoplasm recurrence, recur, and relapse. The detailed search strategy is shown in Fig. 1. A hand search of the literature and all related citations was also carried out. All relevant primary studies were retrieved, including studies that utilized fertility-sparing treatments as their primary intervention, and their data were extracted to be included in this review. Studies that did not include low-risk patients or did not perform a separate subgroup analysis were excluded from this review.
Results
All authors participated in the screening process. We identified 1171 potential studies. Twenty-three studies [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] were included in this review. Figure 2 illustrates our study selection process. These studies included the data of 451 recurrent cases of EC. Three of the studies did not report their number of recurrences. The most common site of recurrence was vaginal cuff (N = 83) and the reported median time to recurrence ranged from 13 to 80 months.
Epidemiological Factors
Age
Twelve studies [15,16,17,18,19,20,21,22,23,24,25,26] examined the role of age as a predictor for risk of recurrence after treatment of low-risk EC. Only 3 studies could establish age as a statistically significant predictor of recurrence [15, 18, 24]. Stasenko et al. conducted a case-control study that compared the median age of both the recurrence and control groups (65 vs 57.5 years); the recurrence group was found to have a statistically significant higher median age (P = 0.025). Wang et al. studied the rate of recurrence of low-risk EC in 30 young premenopausal women who received fertility-sparing treatment. The median age was significantly higher in the recurrent cohort as compared to the non-recurrent cohort (34 vs 30 years; P = 0.003). A retrospective cohort by Yoney et al. showed that age over 60 was associated with statistically significant worse disease-free survival (DFS) (P = 0.021). The remaining nine studies failed to establish a statistical significance of age as a risk predictor for recurrence in low-risk EC. However, 3 studies found that age was significantly associated with worse overall survival [16, 22, 24]. Kim et al. narrowly achieved statistical significance with a hazard ratio (HR) of 1.04 (95% CI, 1.00–1.08). The retrospective cohort by Ayhan et al. estimated a HR of 3.13 (95% CI, 1.14–8.63). Statistical significance was also achieved by Yoney et al. (P = 0.022). The details of all 12 studies are summarized in Table 1.
Body Mass Index
Seven studies [15, 18,19,20, 23, 27, 28] discussed body mass index (BMI) as a risk factor for recurrence. Two studies [20, 28] reported BMI as a statistically significant risk factor for recurrence. Both studies were retrospective cohorts of patients who received fertility-sparing treatment for low-risk EC. They both found a BMI ≥ 25 kg/m2 to be significantly more common in cases that experienced recurrence (P = 0.033). Park et al. used a multivariate analysis to determine the odds ratio (OR) for recurrence with BMI ≥ 25 kg/m2 (OR = 2.14; 95% CI, 1.06–4.31). Stasenko et al. demonstrated a different pattern where patients with recurrence had a lower median BMI than patients without recurrence (27.6 kg/m2 vs 31.2 kg/m2) [15]. This result was statistically significant (P < 0.001). No studies examined the effect of BMI on survival. The details of all 7 studies are summarized in Table 1.
Ethnicity
A single case-control study discussed ethnicity as a risk factor for recurrence after treatment of low-risk EC [15]. Out of 14 patients with recurrence, 79% were White, 14% did not specify, 7% were Hispanic, and none was African American or Asian. Patients without recurrence were 83% White, 8% Asian, 4% African American, 3% did not specify, and 0.2% Hispanic. These differences were statistically significant (P < 0.001).
Molecular Factors
DNA Mismatch Repair Status and Microsatellite Instability
Three studies [15, 16, 29] discussed DNA mismatch repair (MMR) and microsatellite instability (MSI) as a risk factor for recurrence of low-risk EC. According to Stasenko et al., 211/486 (43%) of the patients had a DNA MMR immunohistochemistry analysis performed [15]. DNA MMR deficiency was compared in both the recurrence and control groups (22% vs 11%). The difference between both groups was not statistically significant (P = 0.21). They demonstrated that 24 (45%) of MMR-deficient EC were due to MLH1 hypermethylation. Kim et al. demonstrated a statistical significance in progression-free survival for DNA MMR-deficient tumors, with a hazard ratio (HR) of 2.69 (95% CI, 1.06–6.82) [16]. However, overall survival was not statically significant with a hazard ratio (HR) of 1.23 (95% CI, 0.49–3.10). MLH1 deficiency, mainly due to hypermethylation, accounted for 78% of cases. In both previous studies, after genetic testing, Lynch syndrome was found to account for 19% and 34% of MMR-deficient tumors respectively. Moroney et al. compared frequency of MSI-H in both the recurrence and control groups (53% vs 21%), and the difference was statistically significant with odds ratio (OR) 4.4 (95% CI, 1.1–17.0) [29]. The details of these 3 studies are summarized in Table 2.
TP53 Mutation and P53 Defect
Stasenko et al. and Moroney et al. discussed TP53 mutation and P53 defect as a predictor for recurrence in low-risk EC [15, 29]. They both compared TP53 mutation in the recurrence and control groups (22% vs 11%) and (7% vs 14%), respectively. Neither study achieved statistical significance (P = 0.58) and (P = 0.65), respectively. The details of these 2 studies are summarized in Table 2.
Catenin Beta 1 (CTNNB1) Mutation
Three studies [15, 29, 30] discussed CTNNB1 mutation as a predictor for recurrence after low-risk EC. Moroney et al. compared frequency of CTNNB1 mutation in both the recurrence and control groups (60% vs 28%); the difference was statistically significant with odds ratio (OR) 3.9 (95% CI, 1.1–14.70). Similarly, Costigan et al. compared the frequency of recurrence in tumors with CTNNB1 mutations and a control group (30% vs 0%), and the difference was statistically significant (P = 0.003). On the other hand, Stasenko et al. compared frequency of CTNNB1 mutation in both the recurrence and control groups (44% vs 30%), and the difference between both groups was not statistically significant (P = 0.44). The details of these 3 studies are summarized in Table 2.
PTEN and POLE Mutation
Two studies [15, 29] reported the incidence of PTEN and POLE mutations in patients with recurrence after treatment of low-risk EC. Stasenko et al. compared the frequency of PTEN mutation in both the recurrence and control groups (100% vs 63%); the difference between both groups was statistically significant (P = 0.04). However, when comparing the frequency of POLE mutation frequency in both the recurrence and control groups (11% vs 19%), the difference was not statistically significant (P = 1.00). Moroney et al. compared the frequency of the PTEN mutation in both the recurrence and control groups (80% vs 86%); however, the difference was not statistically significant (P = 0.68). They also compared the frequency of the POLE mutation in both the recurrence and control groups (0% vs 7%); the difference was not statistically significant (P = 0.54). The details of these 2 studies are summarized in Table 2.
L1 Cell Adhesion Molecule (L1CAM) Expression
Two studies [26, 31] analyzed the value of immunohistochemical L1CAM positivity to predict clinical outcomes. Kommos et al. reported a 5-year overall survival rate of 63.8% for patients with L1CAM and 95.3% for patients without L1CAM expression. This difference was statistically significant (P < 0.0001). The 5-year disease-free period was also calculated for patients with L1CAM versus patients with no L1CAM expression (71.8% vs 100%; P <0.0001). Zeimet et al. studied 657 patients with low-grade EC. They compared frequency of L1CAM expression in both the recurrence and control groups, and the difference was statistically significant with a hazard ratio (HR) 14.65. Also, overall survival was statically significant with a hazard ratio (HR) 10.49. Both studies showed that L1CAM is a significant prognostic indicator for overall survival.
Pathological Factors
Histopathological variables have always been taken into consideration in risk stratification systems for EC. We looked at 3 of those variables to determine whether the same conclusions can be drawn for low-risk EC.
Peritoneal Cytology
Two studies analyzed positive peritoneal cytology as a risk predictor for recurrence [15, 32]. Matsuo et al., in a retrograde study of 1124 patients with low-grade EC, showed that positive peritoneal cytology is associated with decreased disease-free survival with a HR of 3.21 (95% CI 1.36–7.60; P = 0.005). They also estimated a HR for distant recurrence of 7.46 (95% CI 2.28–24.4; P < 0.001), but there was no significant association between local recurrence and positive peritoneal cytology (HR 1.74, 95% CI 0.50–6.01; P = 0.38). Stasenko et al. found that 7% of patients with recurrence had a positive peritoneal cytology compared to 4% of patients with no recurrence (P = 0.852). The details of these 2 studies are summarized in Table 3.
Lymphovascular Space Invasion
Nine studies [16, 21,22,23,24,25, 33,34,35] discussed lymphovascular space invasion (LVSI) as a risk factor for recurrence in patients with low-risk EC. Six studies [16, 21, 23, 24, 33, 34] demonstrated statistical significance for LVSI as a risk for recurrence. Kim et al., in a retrograde study of 475 patients, concluded that the HR for a worse progression-free survival (PFS) for patients with positive LVSI was 4.11 (95% CI, 1.35–12.48; P = 0.01). However, the HR for a worse overall survival (OS) with positive LVSI was 1.32 (95% CI, 0.35–4.93). Ureyen et al. reported a worse 5-year disease-free survival (DFS) in patients with positive LVSI compared to patients with negative LVSI (80.1% vs 96.8%; P < 0.001). However, their multivariate analysis revealed that the OR for recurrence was 1.209 (P = 0.879). Gitte Ortoft et al. and Güngördük et al. reported HR of 2.4 (95% CI 1.3–4.3, P < 0.05) and an OR of 5.8 (95% CI 2.0–16.9, P = 0.001) for recurrence in patients with positive LVSI, respectively. Dos Reis et al. reported HR of 3.98 for reduced recurrence-free survival (RFS) (95% CI 1.64–9.63, P = 0.002). Their HR for reduced 5-year OS was 4.78 (95% CI, 1.38–16.5). Lastly, Yoney et al. reported worse DFS in patients with positive LVSI (P = 0.011) and reduced 5-year OS (P = 0.009). On the other hand, Han et al. and Bendifallah et al. showed no statistical significance for LVSI as a risk factor for recurrence in low-risk EC patients. They reported hazard ratios of 0.960 (P = 0.961) and 1.05 (P = 0.9952) for reduced 5-year RFS in patients with positive LVSI, respectively. Ayhan et al. recorded a worse 5-year PFS in patients with positive LVSI (85.5% vs 97%, P < 0.001) on univariate analysis. The calculated HR for worse 5-year PFS on multivariate analysis was not statistically significant (HR = 0.29; 95% CI, 0.07–1.2). They also demonstrated that the HR for worse 5-year OS was 6.68 (95% CI, 1.60–27.89) for patients with positive LVSI. The details of all 9 studies are summarized in Table 3.
Tumor Size
Six studies [17, 21,22,23, 25, 36] discussed tumor size as a predictor for recurrence in low-risk EC patients. Two studies [21, 36] used a tumor size cutoff of ≥ 35 mm. Among those two studies, only Canlorbe et al. reported a statistically significant difference; tumor size ≥ 35 mm was associated with lower RFS (P = 0.005). A retrospective cohort by Sozzi et al. used a tumor size cutoff of ≥ 25 mm and accordingly estimated a HR for local recurrence of 18.7 (95% CI 2.4–140.3; P = 0.004). Out of four studies [22, 23, 25, 36] that used a tumor size cutoff of ≥ 20 mm, only Güngördük et al. could establish a statistical significance of that cutoff in their case-control study. They estimated an OR for recurrence of 6.6 (95% CI 2.7–15.8; P <0.001) for patients with tumor size ≥ 20 mm. Two studies [21, 22] conducted survival analysis using tumor size. Both did not achieve statistical significance. Ureyen et al. reported 5-year DSS for tumor size ≥ 35 mm vs < 35 mm (96.6% vs 100%; P = 0.102). Ayhan et al. reported 5-year OS for tumor size ≥ 20 mm vs < 20 mm (97.4% vs 98.7%; P = 0.723). The details of these 6 studies are summarized in Table 3.
Other Risk Predictors
Ki67 as a Marker of Cellular Proliferation
Two studies [18, 37] discussed Ki67 as a predictor for recurrence after EC. Jiang et al. deduced that the optimal predictive cutoff value for Ki67 is 38%. They compared the 3-year RFS for both the recurrence and control groups (72.6% vs 98.7%). The difference between both groups was statistically significant (P < 0.001). Wang et al. conducted a retrospective study of 30 patients with low-risk EC receiving fertility-sparing treatment. They compared the median percentage of Ki67 in both the recurrence and control groups (12.50% vs 13.75%); however, the difference was not statistically significant (P = 0.426). The details of these 2 studies are summarized in Table 4.
Micro-RNA Expression
De Foucher et al. [27] studied micro-RNA expression levels as a predictive factor for local and distant recurrence in low-risk EC. Micro-RNA-184 fold change (FC) <0.083 is responsible for telomerase maintenance and DNA replication. Micro-RNA-497 5p FC <0.45 and micro-RNA-195 5p FC <0.58 are responsible for PI3 kinase signaling pathway, cancer, and cell cycle checkpoint. Micro-RNA-196 3p FC <0.56 correlates with endometrial cancer and MAPK/cdk5. The expression of these micro-RNA was lower in recurrence compared to the control group. This difference was statistically significant: P = 0.016, P = 0.025, P = 0.025, P = 0.001, respectively.
Hormonal Receptors
Wang et al. [18] examined the expression of estrogen and progesterone receptors as a risk factor for recurrence in low-risk EC patients undergoing fertility preservation treatment. Both the recurrence and control groups were compared as regards estrogen- and progesterone-receptor expression. No statistical significance was observed (P = 0.379; P=0.472, respectively).
Discussion
Previous research has examined recurrence patterns following all stages of endometrial cancer in correlation with multiple individual- and disease-related variables [38,39,40,41,42,43,44]. However, these studies included heterogeneous populations and categorized endometrial cancer patients in varying risk groups. We utilized these studies to guide our selection of various potential risk factors, specifically, for recurrence after low-risk EC. These patients have significantly reduced 5-year survival rates and salvage therapy success rates as low as 40% [11,12,13,14].
Twelve studies [15,16,17,18,19,20,21,22,23,24,25,26] discussed age as a risk predictor for recurrence; only three studies [15, 18, 24] could achieve statistical significance. One of those studies recruited a small cohort of young patients receiving fertility-sparing treatment [18]. Similarly, only three studies [16, 22, 24] established age as a poor prognostic factor for survival. Yoney et al. [24] did not report their measure of survival. Hence, data available so far regarding age does not support the addition of age into a new risk classification system for low-risk EC. Similarly, BMI could only be established as a statistically significant risk predictor in two [20, 28] out of seven [15, 18,19,20, 23, 27, 28] studies. Both studies were performed on young patients receiving fertility-preserving treatment, and they both used a BMI cutoff of 25 kg/m2. In fact, another study by Stasenko et al. [15] contradicted the previous findings and found a higher median BMI among patients without recurrence. Larger well-designed cohort studies are needed to highlight the role of BMI as a potential risk predictor. Ethnic differences were only reported in a single case-control study [15]. Only fourteen patients had recurrences. In addition, some patients did not report their ethnicities. There is insufficient data to determine the possible role of ethnicity.
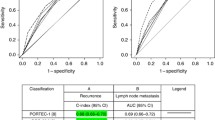
The Cancer Genome Atlas (TCGA) study has fueled intense research of molecular prognostication of EC [45]. The molecular framework devised, which originally defined 4 genomic subtypes, is continuously being modified by data from clinical trials to become more comprehensive of the most important molecular alterations in EC [46,47,48,49]. Accordingly, the choice of adjuvant therapy will take into account molecular risk profiles [50]. The ongoing PORTEC-4a trial reflects the paradigm shift in adopting molecular profiling in the development of newer risk-stratification systems [51]. Unfortunately, the role of molecular profiling in low-risk endometrial cancer is still unclear. We included 6 studies that examined the potential role of some of these molecular markers in low-risk EC [15, 16, 26, 29,30,31]. The results reported in these studies are consistent with findings from other studies that included a broader patient population with several risk groups [52,53,54,55,56].
Several genetic mutations were studied as possible markers: MMR status, TP53, CTNNB1, PTEN, POLE, and L1CAM. MMR status and MSI could be useful as a risk predicator for recurrence and survival, as Kim et al. [16] and Moroney et al. [29] have demonstrated a statistically significant difference between the recurrence and control groups. However, Stasenko et al. [15] have failed to show a statistical difference between both groups. This could be attributed to the small sample size. Out of the 14 recurrences reported by Stasenko et al., only 5 had their MMR immunohistochemistry status recorded. Further studies are needed to solidify the role of MMR and MSI as risk predictors. TP53 mutation as a risk predictor for recurrence of low-grade EC was discussed by two studies [15, 29], but neither study achieved statistical significance of TP53 mutation as a risk for recurrence or reduced survival. This might be attributed to their low sample size. Further studies should be designed to include a larger number of patients to establish a more definite role for TP53 mutation. CTTNB1 mutation could be a useful predictor of recurrence, as Moroney et al. [29] and Costigan et al. [30] have demonstrated a statistically significant difference between the recurrence and control groups. However, Stasenko et al. results failed to show a similar pattern. This, however, could be attributed to their small sample size, as only nine samples underwent molecular testing. Overall, CTTNB1 is a promising molecular marker that could be used to identify women with low-risk EC at risk for recurrence. PTEN and POLE mutations as a risk predictor for recurrence of low-risk EC were reported by two studies [15, 29]. Both studies showed that there was no statistically significant difference between the recurrence and control groups regarding POLE mutation. However, only Stasenko et al. [15] could demonstrate a statistical significant difference regarding PTEN mutation. Both studies were limited by their small sample sizes of 9 and 15. Further larger cohorts are needed to highlight the role of PTEN and POLE mutations as risk predictors.
L1CAM expression has been shown to be a statistically significant predictor of recurrence by Kommos et al. [26] and Zeimet et al. [31]. Both studies have also shown that L1CAM expression is a significant prognostic indicator for overall survival. L1CAM is a promising molecular marker for both recurrence and overall survival and might have a role in a new risk classification system.
Other markers like Ki67, micro-RNA expression, and hormone receptor expression were studied as prognostic factors for recurrence. Two studies [18, 37] assessed Ki67 percentage and risk of recurrence. Jiang et al. [37] found that there is a statistically significant reduction of 3-year RFS, whereas Wang et al. [18] showed statistically insignificant difference of Ki67 percentage between both groups, recurrent and non-recurrent cases. Wang et al. recruited 30 patients with low-grade EC who received fertility-sparing treatment. Recurrence in this study could be more attributed to the nature of fertility-sparing treatment. More well-structured studies are required to shed light on the optimal cutoff value for Ki67 percentage to predict EC. Micro-RNA expression was only reported in a single case-control study recruiting 21 patients who underwent TH-BSO [27]. They found that various micro-RNA expressions were lower in cases with recurrence compared to patients with no recurrence. However, there is insufficient data to provide evidence that micro-MRNA expression could be used as a prognostic tool for EC patients. A single study, Wang et al. [18] reported estrogen and progesterone receptors as risk factors for recurrence in 30 young women who received fertility-sparing treatment. Further research is needed to correlate hormonal receptor expression and risk of recurrence, as they found that there was no difference in hormonal receptor expression in patients with and without recurrence.
Pathological criteria like positive peritoneal cytology, lymphovascular invasion, and various cutoffs of tumor size were vastly studied and showed the most consistent interpretations. Of the two studies [15, 32] discussing the relationship of peritoneal cytology to recurrence, only Matsuo et al. [32] reported a statistically significant reduction of disease-free survival in cases with positive peritoneal cytology. They also showed a statistically significant relationship between positive peritoneal cytology and distant recurrence as opposed to local recurrence. The study’s strength lies in the large sample size. However, both studies have their limitations. Matsuo et al. failed to report the number of recurrences in their study, while Stasenko et al. reported a recurrence rate of only 2.9%. Further research is needed to further elucidate the significance of peritoneal cytology as a prognostic factor to guide adjuvant therapy. LVSI is one of the widely studied prognosticators and is promising to predict recurrence in this subset of patient with low-risk EC. Six studies [16, 21, 23, 24, 33, 34] reported LVSI as statistically significant risk factor for recurrence. The remaining 3 studies [22, 25, 35] had varying limitations. In the study by Ayhan et al. [22], patients with a positive LVSI status were more likely to receive adjuvant therapy; this may have affected the true recurrence rates of the subgroup. Furthermore, a high proportion of the patients underwent pelvic and para-aortic lymphadenectomy offsetting the effect of LVSI. Bendifallah et al. [35] attributed the lack of statistical significance regarding LVSI in their study to the low incidence of LVSI in the low-risk subgroup of patients. Six studies assessed the association between tumor size and risk of recurrence. Canlorbe et al. [36], Sozzi et al. [17], and Güngördük et al. [23] reported various cutoffs of tumor size as a statistically significant predictor of recurrence. A different tumor size cutoff was used by each of the 3 studies. Thus, further research is needed to identify the optimal tumor size cutoff indicating the strongest association between tumor size and recurrence. It is worth noting that two studies [21, 22] that reported tumor size as statistically non-significant in cases of recurrence, were based on univariate analysis. Additionally, Han et al. [25] and Ureyen et al. [21] must be interpreted in light of the fact that both studies respectively included 4.7% and 5.7% of all patients with stage IA grade 3 EC.
One main strength of the current review lies in its novelty, as it is the first review to collect all studies including this subset of low-risk EC patients who are at high risk of recurrence and reduced survival. Some limitations are also present. We included studies that included radical surgical treatment, adjuvant therapy, and conservative fertility-sparing management. There was a variation of outcomes between patients who received different types of treatment. Patients who received conservative management represent a unique subset of patients with low-risk EC. The differences may be accounted for by the younger age, different tumor biology, hormonal receptor expression, and possible differing molecular alterations [57]. In addition, a minority of studies in the current review included either G3 or stage IB as low-risk EC patients. Also, studies from different countries stratified patients according to different guidelines and there was variability in regional guidelines for interventions.
Conclusion
There are subsets of low-risk EC patients at high risk of recurrence and should be suspected when having the following risk factors: positive molecular markers, large tumor size, and lymphovascular invasion. A novel scoring system and randomized controlled trials should be conducted to identify these patients who will benefit most from adjuvant therapy to avoid recurrence.
References
Zhang S, Gong TT, Liu FH, Jiang YT, Sun H, Ma XX, et al. Global, regional, and national burden of endometrial cancer, 1990-2017: results from the Global Burden of Disease Study, 2017. Front Oncol. 2019;9:1440. Published 2019 Dec 19. https://doi.org/10.3389/fonc.2019.01440.
Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10–7.
Keys HM, Roberts JA, Brunetto VL, the Gynecologic Oncology Group, et al. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2004;92:744–51.
Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016;387(10023):1094–108. https://doi.org/10.1016/S0140-6736(15)00130-0.
Kong A, Johnson N, Kitchener HC, Lawrie TA. Adjuvant radiotherapy for stage I endometrial cancer: an updated Cochrane systematic review and meta-analysis. J Natl Cancer Inst. 2012;104(21):1625–34. https://doi.org/10.1093/jnci/djs374.
Beavis AL, Yen TT, Stone RL, Wethington SL, Carr C, Son J, et al. Adjuvant therapy for early stage, endometrial cancer with lymphovascular space invasion: is there a role for chemotherapy? Gynecol Oncol. 2020;156(3):568–74. https://doi.org/10.1016/j.ygyno.2019.12.028.
Danish Gynecological Cancer Group. Chemotherapy or observation in stage I-II intermediate or high risk endometrial cancer. ClinicalTrials.gov Identifier: NCT01244789 [Internet]. Copenhagen: Danish Gynecological Cancer Group. 2018 [cited 2021 Jan 13]. Available from: https://clinicaltrials.gov/ct2/show/NCT01244789
Hogberg T, Signorelli M, de Oliveira CF, Fossati R, Lissoni AA, Sorbe B, et al. Sequential adjuvant chemotherapy and radiotherapy in endometrial cancer--results from two randomised studies. Eur J Cancer. 2010;46(13):2422–31. https://doi.org/10.1016/j.ejca.2010.06.002.
Boothe D, Williams N, Odei B, Poppe MM, Werner TL, Suneja G, et al. The addition of adjuvant chemotherapy to radiation in early-stage high-risk endometrial cancer: survival outcomes and patterns of care. Int J Gynecol Cancer. 2017;27(5):912–22. https://doi.org/10.1097/IGC.0000000000000963.
SGO Clinical Practice Endometrial Cancer Working Group, Burke WM, Orr J, et al. Endometrial cancer: a review and current management strategies: part II. Gynecol Oncol. 2014;134(2):393–402. https://doi.org/10.1016/j.ygyno.2014.06.003.
Xu Y, Burmeister C, Hanna RK, Munkarah A, Elshaikh MA. Predictors of survival after recurrence in women with early-stage endometrial carcinoma. Int J Gynecol Cancer. 2016;26(6):1137–42. https://doi.org/10.1097/IGC.0000000000000733.
Bendifallah S, Ouldamer L, Lavoue V, Canlorbe G, Raimond E, Coutant C, et al. Patterns of recurrence and outcomes in surgically treated women with endometrial cancer according to ESMO-ESGO-ESTRO Consensus Conference risk groups: results from the FRANCOGYN study Group. Gynecol Oncol. 2017;144(1):107–12. https://doi.org/10.1016/j.ygyno.2016.10.025.
Topfedaisi Ozkan N, Meydanlı MM, Sarı ME, Demirkiran F, Kahramanoglu I, Bese T, et al. Factors associated with survival after relapse in patients with low-risk endometrial cancer treated with surgery alone. J Gynecol Oncol. 2017;28(5):e65. https://doi.org/10.3802/jgo.2017.28.e65.
Francis SR, Ager BJ, Do OA, Huang YHJ, Soisson AP, Dodson MK, et al. Recurrent early stage endometrial cancer: patterns of recurrence and results of salvage therapy. Gynecol Oncol. 2019;154(1):38–44. https://doi.org/10.1016/j.ygyno.2019.04.676.
Stasenko M, Feit N, Lee SSK, Shepherd C, Soslow RA, Cadoo KA, et al. Clinical patterns and genomic profiling of recurrent ‘ultra-low risk’ endometrial cancer. Int J Gynecol Cancer. 2020;30(6):717–23. https://doi.org/10.1136/ijgc-2020-001241.
Kim SR, Pina A, Albert A, McAlpine JN, Wolber R, Gilks B, et al. Mismatch repair deficiency and prognostic significance in patients with low-risk endometrioid endometrial cancers. Int J Gynecol Cancer. 2020;30(6):783–8. https://doi.org/10.1136/ijgc-2019-000910.
Sozzi G, Uccella S, Berretta R, Petrillo M, Fanfani F, Monterossi G, et al. Tumor size, an additional risk factor of local recurrence in low-risk endometrial cancer: a large multicentric retrospective study. Int J Gynecol Cancer. 2018;28(4):684–91. https://doi.org/10.1097/IGC.0000000000001223.
Wang CJ, Chao A, Yang LY, Hsueh S, Huang YT, Chou HH, et al. Fertility-preserving treatment in young women with endometrial adenocarcinoma: a long-term cohort study. Int J Gynecol Cancer. 2014;24(4):718–28. https://doi.org/10.1097/IGC.0000000000000098.
Park JY, Seong SJ, Kim TJ, Kim JW, Kim SM, Bae DS, et al. Pregnancy outcomes after fertility-sparing management in young women with early endometrial cancer. Obstet Gynecol. 2013;121(1):136–42. https://doi.org/10.1097/aog.0b013e31827a0643.
Park JY, Kim DY, Kim JH, Kim YM, Kim KR, Kim YT, et al. Long-term oncologic outcomes after fertility-sparing management using oral progestin for young women with endometrial cancer (KGOG 2002). Eur J Cancer. 2013;49(4):868–74. https://doi.org/10.1016/j.ejca.2012.09.017.
Ureyen I, Karalok A, Turkmen O, Kimyon G, Akdas YR, Akyol A, et al. Factors predicting recurrence in patients with stage IA endometrioid endometrial cancer: what is the importance of LVSI? Arch Gynecol Obstet. 2020;301(3):737–44. https://doi.org/10.1007/s00404-019-05418-z.
Ayhan A, Şahin H, Sari ME, Yalçin I, Haberal A, Meydanli MM. Prognostic significance of lymphovascular space invasion in low-risk endometrial cancer. Int J Gynecol Cancer. 2019;29(3):505–12. https://doi.org/10.1136/ijgc-2018-000069.
Güngördük K, Firat Cüylan Z, Kahramanoglu I, Oge T, Akbayir O, Dede M, et al. Risk factors for recurrence in low-risk endometrial cancer: a case-control study. Oncol Res Treat. 2018;41(7-8):466–70. https://doi.org/10.1159/000488112.
Yoney A, Yildirim C, Bati Y, Unsal M. Low risk stage I endometrial carcinoma: prognostic factors and outcomes. Indian J Cancer. 2011;48(2):204–10. https://doi.org/10.4103/0019-509X.82895.
Han KH, Kim HS, Lee M, Chung HH, Song YS. Prognostic factors for tumor recurrence in endometrioid endometrial cancer stages IA and IB. Medicine (Baltimore). 2017;96(21):e6976. https://doi.org/10.1097/MD.0000000000006976.
Kommoss F, Kommoss F, Grevenkamp F, Bunz AK, Taran FA, Fend F, et al. L1CAM: amending the “low-risk” category in endometrial carcinoma. J Cancer Res Clin Oncol. 2017;143(2):255–62. https://doi.org/10.1007/s00432-016-2276-3.
de Foucher T, Sbeih M, Uzan J, et al. Identification of micro-RNA expression profile related to recurrence in women with ESMO low-risk endometrial cancer. J Transl Med. 2018;16(1):131. Published 2018 May 21. https://doi.org/10.1186/s12967-018-1515-6.
Park JY, Seong SJ, Kim TJ, Kim JW, Bae DS, Nam JH. Significance of body weight change during fertility-sparing progestin therapy in young women with early endometrial cancer. Gynecol Oncol. 2017;146(1):39–43. https://doi.org/10.1016/j.ygyno.2017.05.002.
Moroney MR, Davies KD, Wilberger AC, Sheeder J, Post MD, Berning AA, et al. Molecular markers in recurrent stage I, grade 1 endometrioid endometrial cancers. Gynecol Oncol. 2019;153(3):517–20. https://doi.org/10.1016/j.ygyno.2019.03.100.
Costigan DC, Dong F, Nucci MR, Howitt BE. Clinicopathologic and immunohistochemical correlates of CTNNB1 mutated endometrial endometrioid carcinoma. Int J Gynecol Pathol. 2020;39(2):119–27. https://doi.org/10.1097/PGP.0000000000000583.
Zeimet AG, Reimer D, Huszar M, Winterhoff B, Puistola U, Abdel Azim S, et al. L1CAM in early-stage type I endometrial cancer: results of a large multicenter evaluation [published correction appears in. J Natl Cancer Inst. 2013;105(15):1142–50. https://doi.org/10.1093/jnci/djt144.
Matsuo K, Yabuno A, Hom MS, Shida M, Kakuda M, Adachi S, et al. Significance of abnormal peritoneal cytology on survival of women with stage I-II endometrioid endometrial cancer. Gynecol Oncol. 2018;149(2):301–9. https://doi.org/10.1016/j.ygyno.2018.02.012.
Ørtoft G, Lausten-Thomsen L, Høgdall C, Hansen ES, Dueholm M. Lymph-vascular space invasion (LVSI) as a strong and independent predictor for non-locoregional recurrences in endometrial cancer: a Danish Gynecological Cancer Group Study. J Gynecol Oncol. 2019;30(5):e84. https://doi.org/10.3802/jgo.2019.30.e84.
dos Reis R, Burzawa JK, Tsunoda AT, Hosaka M, Frumovitz M, Westin SN, et al. Lymphovascular space invasion portends poor prognosis in low-risk endometrial cancer. Int J Gynecol Cancer. 2015;25(7):1292–9. https://doi.org/10.1097/IGC.0000000000000490.
Bendifallah S, Canlorbe G, Raimond E, Hudry D, Coutant C, Graesslin O, et al. A clue towards improving the European Society of Medical Oncology risk group classification in apparent early stage endometrial cancer? Impact of lymphovascular space invasion. Br J Cancer. 2014;110(11):2640–6. https://doi.org/10.1038/bjc.2014.237.
Canlorbe G, Bendifallah S, Laas E, Raimond E, Graesslin O, Hudry D, et al. Tumor size, an additional prognostic factor to include in low-risk endometrial cancer: results of a French multicenter study. Ann Surg Oncol. 2016;23(1):171–7. https://doi.org/10.1245/s10434-015-4583-3.
Jiang P, Jia M, Hu J, et al. Prognostic value of Ki67 in patients with stage 1-2 endometrial cancer: validation of the cut-off value of Ki67 as a predictive factor. Onco Targets Ther. 2020;13:10841–50. Published 2020 Oct 27. https://doi.org/10.2147/OTT.S274420.
Sasada S, Yunokawa M, Takehara Y, Ishikawa M, Ikeda S, Kato T, et al. Baseline risk of recurrence in stage I-II endometrial carcinoma. J Gynecol Oncol. 2018;29(1):e9. https://doi.org/10.3802/jgo.2018.29.e9.
Bishop EA, Java JJ, Moore KN, Walker JL. Pathologic and treatment outcomes among a geriatric population of endometrial cancer patients: an NRG Oncology/Gynecologic Oncology Group Ancillary Data Analysis of LAP2. Int J Gynecol Cancer. 2017;27(4):730–7. https://doi.org/10.1097/IGC.0000000000000947.
Ouldamer L, Bendifallah S, Body G, et al. Predicting poor prognosis recurrence in women with endometrial cancer: a nomogram developed by the FRANCOGYN study group. Br J Cancer. 2016;115(11):1296–303. https://doi.org/10.1038/bjc.2016.337.
AlHilli MM, Mariani A, Bakkum-Gamez JN, et al. Risk-scoring models for individualized prediction of overall survival in low-grade and high-grade endometrial cancer. Gynecol Oncol. 2014;133(3):485–93. https://doi.org/10.1016/j.ygyno.2014.03.567.
Fujimoto T, Nanjyo H, Fukuda J, Nakamura A, Mizunuma H, Yaegashi N, et al. Endometrioid uterine cancer: histopathological risk factors of local and distant recurrence. Gynecol Oncol. 2009;112(2):342–7. https://doi.org/10.1016/j.ygyno.2008.10.019.
Bendifallah S, Canlorbe G, Huguet F, Coutant C, Hudry D, Graesslin O, et al. A risk scoring system to determine recurrence in early-stage type 1 endometrial cancer: a French multicentre study. Ann Surg Oncol. 2014;21(13):4239–45. https://doi.org/10.1245/s10434-014-3864-6.
Stelloo E, Nout RA, Osse EM, Jürgenliemk-Schulz IJ, Jobsen JJ, Lutgens LC, et al. Improved risk assessment by integrating molecular and clinicopathological factors in early-stage endometrial cancer-combined analysis of the PORTEC cohorts. Clin Cancer Res. 2016;22(16):4215–24. https://doi.org/10.1158/1078-0432.CCR-15-2878.
Cancer Genome Atlas Research Network, Kandoth C, Schultz N, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67–73. https://doi.org/10.1038/nature12113.
Kommoss S, McConechy MK, Kommoss F, et al. Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann Oncol. 2018;29(5):1180–8. https://doi.org/10.1093/annonc/mdy058.
Stelloo E, Bosse T, Nout RA, MacKay HJ, Church DN, Nijman HW, et al. Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol. 2015;28(6):836–44. https://doi.org/10.1038/modpathol.2015.43.
Britton H, Huang L, Lum A, Leung S, Shum K, Kale M, et al. Molecular classification defines outcomes and opportunities in young women with endometrial carcinoma. Gynecol Oncol. 2019;153(3):487–95. https://doi.org/10.1016/j.ygyno.2019.03.098.
León-Castillo A, de Boer SM, Powell ME, Mileshkin LR, Mackay HJ, Leary A, et al. Molecular classification of the PORTEC-3 trial for high-risk endometrial cancer: impact on prognosis and benefit from adjuvant therapy. J Clin Oncol. 2020;38(29):3388–97. https://doi.org/10.1200/JCO.20.00549.
van den Heerik ASVM, Horeweg N, de Boer SM, et al. Adjuvant therapy for endometrial cancer in the era of molecular classification: radiotherapy, chemoradiation and novel targets for therapy. International Journal of Gynecologic Cancer. 2020. https://doi.org/10.1136/ijgc-2020-001822.
van den Heerik ASVM, Horeweg N, Nout RA, Lutgens LCHW, van der Steen-Banasik EM, Westerveld GH, et al. PORTEC-4a: international randomized trial of molecular profile-based adjuvant treatment for women with high-intermediate risk endometrial cancer. Int J Gynecol Cancer. 2020;30(12):2002–7. https://doi.org/10.1136/ijgc-2020-001929.
Huvila J, Laajala TD, Edqvist PH, Mardinoglu A, Talve L, Pontén F, et al. Combined ASRGL1 and p53 immunohistochemistry as an independent predictor of survival in endometrioid endometrial carcinoma. Gynecol Oncol. 2018;149(1):173–80. https://doi.org/10.1016/j.ygyno.2018.02.016.
Obata T, Nakamura M, Mizumoto Y, et al. Dual expression of immunoreactive estrogen receptor β and p53 is a potential predictor of regional lymph node metastasis and postoperative recurrence in endometrial endometrioid carcinoma. PLoS One. 2017;12(11):e0188641. Published 2017 Nov 30. https://doi.org/10.1371/journal.pone.0188641.
Kurnit KC, Kim GN, Fellman BM, Urbauer DL, Mills GB, Zhang W, et al. CTNNB1 (beta-catenin) mutation identifies low grade, early stage endometrial cancer patients at increased risk of recurrence. Mod Pathol. 2017;30(7):1032–41. https://doi.org/10.1038/modpathol.2017.15.
Cosgrove CM, Cohn DE, Hampel H, Frankel WL, Jones D, McElroy JP, et al. Epigenetic silencing of MLH1 in endometrial cancers is associated with larger tumor volume, increased rate of lymph node positivity and reduced recurrence-free survival. Gynecol Oncol. 2017;146(3):588–95. https://doi.org/10.1016/j.ygyno.2017.07.003.
Pasanen A, Tuomi T, Isola J, Staff S, Bützow R, Loukovaara M. L1 cell adhesion molecule as a predictor of disease-specific survival and patterns of relapse in endometrial cancer. Int J Gynecol Cancer. 2016;26(8):1465–71. https://doi.org/10.1097/IGC.0000000000000801.
Baxter E, Brennan DJ, McAlpine JN, et al. Improving response to progestin treatment of low-grade endometrial cancer. Int J Gynecol Cancer. 2020;30(11):1811–23. https://doi.org/10.1136/ijgc-2020-001309.
Acknowledgements
We would like to thank Menna Kamel, MBBS, for her essential contribution to this manuscript. She assisted in designing the search strategy and participated in the screening process and study selection.
Funding
The authors are financially independent.
Availability of Data and Material
The data and material that support the findings of this study are available from the corresponding author upon request.
Code Availability
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
There is a waiver as the review does not include any study on humans and/or animals.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laban, M., El-Swaify, S.T., Ali, S.H. et al. The Prediction of Recurrence in Low-Risk Endometrial Cancer: Is It Time for a Paradigm Shift in Adjuvant Therapy?. Reprod. Sci. 29, 1068–1085 (2022). https://doi.org/10.1007/s43032-021-00565-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00565-8