Abstract
Tuberculosis is a public health problem globally and as well in Sri Lanka. By calling for the health-related quality of life assessments, attention is focused on the problems experienced by the patients. The objective of this study was to assess how tuberculosis patients have reported health-related quality of life in Sri Lanka. This cross-sectional study enrolled 552 new pulmonary tuberculosis patients. Each participant completed the EQ-5D-3L in a face-to-face interview at the initiation, at the end of 2 months and at 6 months of medication completion. Data derived from EQ-5D-3L reported problems at three levels in each dimension and the EQ-Visual Analogue Scale (EQ-VAS) described the quality of life as a single index score. Utility values were calculated using the Sri Lankan EQ-5D-3L value set and quality-adjusted life years (QALYs) were calculated by multiplying the medication period with the utility value difference between the initiation of medication and the medication completion at 6 months. Problems related to all dimensions of health-related quality of life were decreased during the medication. The mean EQ-VAS score at initiation was 59.64 (SD = 21.6) and increased up to 78.0 (SD = 16.1) and 83.4 (SD = 16.5) at end of 2 months and at end of 6 months, respectively, which was significant at each phase of medication (Wilks’ Lambda = 0.55, F = 187.33, P < 0.001). The mean QALYs gained during the medication was 0.05 (SD = 0.07). Health-related quality of life improved significantly among tuberculosis patients with medication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is an infectious disease and it can affect any organ in humans. Most often, it affects the lungs and when it affects the lungs, it is known as pulmonary tuberculosis (PTB) [1]. Tuberculosis is a curable disease, and despite the availability of effective medicine [2, 3], it is still a major health issue globally [4]. Sri Lanka is a middle-income country in South Asia and TB prevalence is low in the country [5], but TB is still a stigmatizing disease in Sri Lanka [6]. Tuberculosis patients undergo many psychological problems such as anxiety, fear and depression and socio-economic problems in addition to the clinical problems [7,8,9] due to societal discrimination, having to be off work or school in the initial period of treatment and a prolonged period of treatment in the management of TB for at least 6 months with multiple and potentially toxic drugs [10]. Therefore, it is important to deal with these associated psychological and social problems of this vulnerable group of patients in addition to clinical problems.
The struggle with psychological and social problems is experienced by the individual patients, and therefore, it is very important to measure the impact of these problems from the patient’s voice, and the field of research that has emerged from this aspect is termed health-related quality of life [11]. When the quality of life is combined with the quantity of life, it serves as a composite indicator QALY [12] a quantitative measure of health outcomes [13] which measures the value that patients place on their health state and is crucial in understanding the experience of their health condition. Over the past several years, a growing number of studies have assessed the impact of TB on health-related quality of life (HRQOL) of patients in many countries globally and the majority had been implemented in low-income and middle-income countries [14,15,16,17,18]. High-income countries report few studies assessing HRQOL among TB patients which include mainly the migrated population [19]. The studies have assessed the HRQOL of patients at various time points during treatment and the majority have assessed the HRQOL at the initiation of treatment, at end of 2 months and at end of 6 months of treatment completion. Results show that HRQOL was very low at the initiation of treatment and improved significantly at the completion of treatment [15, 20]. Different tools such as World Health Organization Quality of Life BREF (WHOQOL-BREF) [8], Short-Form 36 (SF-36) [21] and St. George’s Respiratory Questionnaire (SGRQ) [22] have been used to measure HRQOL. The authors have concluded that HRQOL indicators are important as patient-reported health outcomes of TB patients with other clinical and laboratory indicators to assess the complete health status of patients [8, 21, 23,24,25]. Most studies have described the HRQOL separately in psychological, social, functional and physical dimensions of the HRQOL construct [24, 26, 27]. Some studies have reported the calculation of QALYs related to TB [13, 18]. However, such studies were lacking in Sri Lanka except for one study in assessing HRQOL in TB patients during the period of treatment [16] but not a single study has been carried out in calculating QALYs of TB patients.
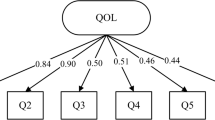
The aim of this study was to measure the HRQOL of new PTB patients registered for treatment in the largest TB clinic in Sri Lanka at three time points during the period of TB treatment of 6 months. The study also aimed to assess the QALYs gained during the treatment. To assess HRQOL and QALYs, the EuroQol five dimension-three-level (EQ-5D-3L) tool was used. The EQ-5D-3L is simple to understand and it takes only 3–5 min to answer the questionnaire. This tool is the most popular generic preference-based tool [28] that is widely used to estimate utilities and thus it has generated a greater number of country-specific value sets in many countries including Sri Lanka [29]. The utilities were used to calculate quality-adjusted life-years [12, 13]. The EQ-5D-3L measures the HRQOL in five dimensions of mobility, self-care, usual activities, pain/discomfort and anxiety/depression [28]. The thermometer-like EQ-VAS of the EQ-5D-3L was used to assess health status that can be assumed by the patient [29].
Methods
Study Setting and Study Population
We collected data from 552 newly diagnosed PTB patients [1] who have not taken treatment before and registered for treatment in the central chest clinic (CCC) of Colombo district, in Sri Lanka. These patients were with drug-sensitive PTB and include bacteriologically confirmed and clinically diagnosed patients with PTB. Bacteriologically, conformation was through sputum microscopy, sputum culture or GeneXpert test. A patient whose sputum sample is bacteriologically negative but has been diagnosed with active TB by a clinician with consultation of a consultant respiratory physician and decided to treat with a full course of TB treatment includes the clinically diagnosed patients.
A sample size calculation was carried out to determine the sample size needed to identify QALYs gain.
N = the sample size.
The minimal clinically important difference (MCID), in this case, is the minimum time trade off (TTO) increment in determining preference for EQ-5D health status. A conservative MCID of 0.05 was used as 6 months is a minimum increment in the TTO (i.e. 0.5/10) [29]. Standard deviation (SD) of 0.26 of Sri Lankan value set was used for the equation. δ values for significance (Sig) and power are to be assumed from a normal distribution table. By convention, significance was considered at p < 0.05 and power was 80% and assumed to follow a normal distribution. To compensate for the inefficiency of data that were not normally distributed, the power calculation was adjusted by 1/0.95. Sample size (N) was calculated as 445 with 80% power of detecting a difference of 6 months in TTO valuations with a 5% significance based on 0.26 SD [30]. Following anticipation was made based on past data regarding TB patients: loss to follow-up (8%), death (5%), non-participation (10%) and transfer out to other clinics (1%) by the completion of treatment. Considering these anticipations, the sample size was adjusted to 552 (445 + 107).
The consecutive sampling method was used to select study participants allowing the potential of including all the consequent eligible new PTB patients registered at the chest clinic during the study period until the required sample size was recruited. An inherent problem with this sampling technique is that the study findings could only be confined to the period in which the data were collected and there could be a limitation in generalizing the findings to the rest of the period in the year. This issue would arise if reporting of TB has any seasonal variations and no such seasonal variations have been identified in relation to TB.
The study setting selected in our study is the largest chest clinic in Sri Lanka and located in the Colombo district which is the capital city of Sri Lanka. Out of all districts in Sri Lanka, the highest number of TB patients is reported from the Colombo district and this accounts for 25% of the Sri Lankan national figure. Sri Lanka has reported between 5000 and 6000 new PTB patients annually during the past two decades [31].
The TB patients enrolled were more than 18 years and could understand Sinhala language. Those with known psychiatric illnesses, co-morbid diseases, severe illness and pregnancy were excluded.
Prior to starting data collection, the patients gave their consent in writing. They were informed about the purpose of the study and assured that refusal to participate at any point would have no impact on their medication as usual and consent was taken in writing, only if the participant agreed to participate in the research study. The participants were given a copy of the information sheet. All personal details provided were treated as strictly confidential. The ethics committee approved the consent procedure. The ethical approval was obtained from the Ethics Review Committee of the University of Colombo Faculty of Medicine Sri Lanka (EC-17-019).
Data Collection
The data were collected over 1 year in 2017–2018. Face-to-face interviews were carried out by trained pre-intern medical officers. The patients were interviewed at three encounters during the TB medication. Upon recruitment at the initiation of medication, the patients indicated their current health status to the items in the EQ-5D-3L questionnaire which was taken as the baseline status of health. Thereafter, the patients were interviewed at the end of 2 months and at the end of 6 months during the TB medication, when they visited the CCC to obtain the anti-TB drugs. The EQ-5D-3L questionnaire has been validated for Sri Lanka to be used in the Sinhala language [29]. In addition, the participants responded to the EQ-VAS, a thermometer-like indicator to record the current health status at each of the three patient encounters. The participants were requested to indicate “which level of point best match your own health condition today”. The basic socio-demographic data of the patients were obtained through a structured questionnaire.
Data Analysis
Analysis of data was carried out using SPSS version 22.0. The frequency of people reporting no problems, some problems and severe problems for each dimension of the EQ-5D-3L was calculated at the initiation of medication, at the end of 2-month medication and at the end of 6-month medication completion and presented as a descriptive profile. Data collected from the EQ-VAS was presented as mean and median values and one-way repeated-measure analysis of variance (ANOVA) was used to compare the change in EQ-VAS scores of TB patients at initiation of medication, at the end of 2 months and after completing medication at the end of 6 months.
The health status described by the EQ-5D-3L descriptive system was converted into a single summary index by applying values (also called weights) to the three levels in five dimensions of the instrument. Information obtained from this method was used to assess utilities for each respondent by using Sri Lankan population EQ-5D-3L value set. Quality-adjusted life-years were calculated by multiplying the treatment period in years (0.5) with the utility value difference between the initiation of medication and at the medication completion at the end of 6 months. The QALYs were disaggregated for gender, marital status, ethnicity, religion, employment status, education status and the household income, and significance between groups in categorical variables was assessed using one-way between-group ANOVA with post hoc tests. A two-sided P value < 0.05 was considered statistically significant throughout the analyses.
Results
Of the total of 552 patients enrolled in the study, all responded (100% response rate) to the EQ -5D-3L measure at the beginning of medication and 465 (84.2%) of them responded at the second encounter at the end of 2-month intensive phase of medication and 485 (87.8%) responded at the third encounter at the end of 6-month medication completion. The overall attrition rate of the study was 15.7% (n = 87). Reasons for attrition included failure to answer more than half of the questionnaire due to various disturbances (n = 6), loss to follow-up (n = 20), not attended the clinic as scheduled for the second and 6 months of medication period (n = 26), transferred out to other clinics (n = 20), death (n = 1), hospitalized due to severe illness (n = 12) and treatment failure (n = 2). All patients could understand and answer the questions in Sinhala, and therefore, ethnic variability was not a barrier in the enrolment of patients.
Description of the Study Participants
Table 1 describes the study population. The mean age was 49.1 years (SD = 16.2) and the majority belong to the age between 35 and 64 years (60.7%). The majority were males [n = 378 (68.5%)]. By ethnicity, the greater proportion was Sinhalese [n = 290 (52.5%)] followed by Muslims [n = 170 (30.8%)]. Patients who were married or living together included the majority [n = 382(69.2%)]. Education category from grade 6 to ordinary level (O/L) but O/L failed comprised the major proportion of the study population [n = 229 (41.5%)] and 340 (61.6%) patients were employed when they were registered for TB medication.
Description of Reported Problems in the EQ-5D-3L Dimensions
Table 2 shows reported problems faced by the TB patients in five dimensions of the EQ-5D-3L during the treatment.
A substantial proportion of patients reported some problems in mobility at the initiation of treatment [168 (30.4%)]; however, the proportion of patients with some problems in mobility reduced over the treatment period to 76 (15.7%) at the end of 2 months and 49 (10.7%) at the end of 6 months (p < 0.001). Severe problems in mobility were not reported by any patients during the treatment period.
With regard to self-care, some problems were reported by 37 (6.7%) at the initiation of treatment followed by 28 (5.8%) and 46 (9.9%) at the end of 2 months and at the end of 6 months, respectively (p = 0.039). Severe problems were not reported by any patients during the treatment period.
Concerning the ability to perform usual activities, some problems were reported by 171 (31%) at the initiation of treatment while it was 61 (12.6%) and 46 (9.9%) at the end of 2 months and at the end of 6 months, respectively (p < 0.001). None of the patients reported severe problems in usual activities during the treatment period.
Results revealed 288 (52.2%) patients reporting some problems in pain/discomfort at the initiation of treatment followed by 139 (28.7%) and 46 (9.9%) at the end of 2 months and at the end of 6 months, respectively, and 19 (3.4%) patients reported of severe problems in pain/discomfort at the initiation of treatment (p < 0.001).
Regarding anxiety/depression, some problems were reported by 153 (27.7%) patients at the initiation of treatment followed by 95 (19.6%) and 46 (9.9%) at the end of 2 months and at the end of 6 months, respectively (p < 0.001), and severe problems were reported by 36 (6.5%) and 10 (2.0%) at initiation of treatment and at end of 2 months, respectively (p < 0.001).
EQ-5D-VAS Score During the Treatment
As described in Table 3, the mean EQ-5D-VAS score increased during the medication period from 59.64 (SD = 21.6) at the initiation of medication up to 78.0 (SD = 16.1) and 83.4 (SD = 16.5) at the end of 2 months and at the end of 6-month medication period, respectively. The increase in EQ-5D-VAS score was significant from initiation of medication to end of 2-month medication and from this phase to 6-month medication completion (Wilks’ Lambda = 0.55, F = 187.33, p < 0.001).
Quality-Adjusted Life Years Gained During the TB Medication
A mean QALYs of 0.05 (SD = 0.07) have been gained during the 6-month medication period. Table 4 includes the mean QALYs gained during the 6-month medication period disaggregated by socio-demographic characteristics. The QALYs gained during the medication period was significantly different (p < 0.001) among the age groups of the study population. Post hoc tests revealed that the patients aged 31–50 years (p = 0.005) and 51–65 years (p < 0.001) gained significantly more QALYs than the older age group of > 66 years. There was no significant difference (p = 0.638) in QALYs gained between males and females during the medication period.
As shown in Table 5, QALYs gained by males during the medication period was significantly different among the age groups (p = 0.04); however, post hoc tests with Bonferroni adjustments revealed that this difference was not significant between each age groups in males. The reason behind is that the Bonferroni correction is used to limit the possibility of getting a statistically significant result when doing multiple tests and the correction lowers the area where you can reject the null hypothesis that it makes the p value smaller [32].
The QALYs gained by females was significantly different among the age groups (p < 0.001) and post hoc tests revealed that the QALYs gained in the age groups 31–50 years (p < 0.001) and in the age group 51–60 years (p < 0.001) were significantly higher than in the older age group of > 66 years. There was no significant difference in QALYs gained among groups of other categories such as education level, household income, employment status, marital status, religion, ethnicity, current alcohol consumption and current smoking status.
Discussion
It was evident from this study that TB affects the dimensions of mobility, self-care, usual activities, pain/discomfort and anxiety/depression of HRQOL in keeping with results of other studies in different countries that assessed HRQOL of TB patients using different instruments [14,15,16,17, 33]. It was also evident that HRQOL of TB patients has been improved significantly with standard anti-TB medication for 6 months which is also consistent with similar studies done in North India among new PTB patients using WHOQOL-BREF [8], another study done in India among PTB patients using SF-36 [21], in Indonesia among smear-positive PTB patients using SGRQ [22] and in Pakistan among new PTB patients using EQ-5D-3L [17]. The only study reported from Sri Lanka [16] also shows similar results of significant improvement of the HRQOL (p < 0.001) among TB patients during the medication period, as measured by the WHOQOL-BREF. The HRQOL has been assessed using many different instruments [34] which makes it difficult for direct comparison among these studies.
In our research study, at the initiation of medication, nearly one-third of patients responded as having some problems in mobility, usual activities and anxiety/depression, with nearly half of the population responded to have pain/discomfort. In Pakistan (a high TB prevalent country), nearly 50% of the patients presented with some problems in mobility, usual activities, anxiety/depression and pain/discomfort [17]. In our study, no one gave an account of severe problems in mobility and usual activates; however, 3.4% and 6.5% announced with severe problems in pain/discomfort and anxiety/depression, respectively. In Pakistan, 5% and 40% presented with severe problems in mobility and usual activities, respectively, while 20% revealed to have severe problems in pain/discomfort and anxiety/depression. Other than the physical debilitation, TB patients are psychologically affected. Therefore, these patients need psychological support to cope up with emotional deprivation. A study that has been done in Malaysia among new PTB patients also showed that 67.1% of patients were at the risk of depression at the start of TB medication [9]. However, anti-TB medication has improved psychological well-being as well [35].
We used the EQ-5D-3L instrument in this study, because, in addition to its use as a HRQOL assessment instrument, it is also the most popular generic preference-based tool to measure utility in association with any disease [28]. Moreover, a population-based country-specific EQ-5D-3L-derived value set is available for Sri Lanka [29]. This population-based value set is very important in estimating utilities. Tuberculosis medication outcome in terms of QALYs will be useful in economic evaluations in Sri Lanka in an era of the introduction of new investigation technologies, the emergence of drug resistance TB and the availability of different medication regimens.
The mean QALYs gained by the PTB patients in our study was 0.05 (SD = 0.07). According to a study done in Tarrant County, Texas [13], during 2002 in an assessment of QALYs lost due to acute illness and ambulatory medication among culture-positive PTB patients, they found that each individual PTB patient averaged a loss of 0.046 QALYs prior to clinical cure during the medication. In a study in Indonesia, the average of QALYs was 0.74 in the intensive phase, and it was 0.87 in the continuous phase (p < 0.05) [18].
Our study was a follow-up study and there was a certain amount of loss to follow-up cases due to various reasons. The overall loss to follow-up count was 87 (15.7%). The loss to follow-up is a major source of bias, and if this proportion was large in the range of 30% to 40%, this would certainly raise serious doubts about the validity of the study results [36]. A loss to follow-up rate of 25% has been documented in the study done previously to assess HRQOL in TB patients during the 6-month medication period in Sri Lanka [16]. Other international studies revealed an overall loss to follow-up rate ranging from 16 to 35% [8, 9, 37] during a 6-month medication period.
A major proportion of patients in this current study belonged to the age group of 35–64 years (60.7%) and the mean age was 49.1 years (SD = 16.2). Even though all age groups are affected by TB, people in the productive age are under a major risk of contracting TB. As evident from global reports, most TB patients globally were between the age groups of 15–55 years [38]. In Sri Lanka, national figures reveal that majority of all new TB cases were in the age group of 15–54 in 2014 [n = 5241(60.3%)], in 2015 [n = 5328(59.2%)] and in 2016 [n = 4810 (59.7%)]. There was a clear preponderance of males [n = 378 (68.5%)] in this study population. According to the Sri Lankan national figures in 2016, 65.7% (n = 5473) were males [39], and globally out of the estimated 10.4 million, 90% were adults and of which 65% were males [1].
Higher TB notification rates in men may partly reflect epidemiological differences in exposure, the risk of infection and progression from infection to disease. Community-based epidemiological studies have revealed that males have a higher prevalence of TB infection and a higher rate of progression from infection to active disease than females. Even though some say profound gender differential is due to barriers for women in seeking health care, this phenomenon affecting the Sri Lankan females is doubtful given the fact that high literacy rates among women and almost non-existent social discrimination affecting women regarding their health-seeking behaviour and decision-making power.
A strength of this research study is that the study participants were interviewed only during their usual scheduled visits to the clinic and it only took 5 to 10 min to complete the questionnaires. Availability of population value set for the EQ-5D-3L for Sri Lanka was another strength. However, due to attrition, it was not possible to assess the improvement of HRQOL in all the patients enrolled at the initiation of the study. Therefore, the improvement in HRQOL is evident only in patients who faced all three interviews. However, all possible measures were taken to minimize loss to follow-up rates such as the building of good rapport with patients. In addition, the patients were advised about the importance of attending on due clinic dates, and after obtaining prior consent, patients were informed about their scheduled clinic dates over the phone.
Conclusion
The HRQOL of PTB patients improved significantly with standard anti-TB medication. Assessment of HRQOL/QALYs is an important health outcome indicator in addition to the clinical and laboratory indicators.
References
World Health Organization. Treatment of tuberculosis guidelines. Fourth edition. The World Health Organization. Geneva, Switzerland. 2010. https://apps.who.int/iris/bitstream/handle/10665/44165/9789241547833_eng.pdf. Accessed 15 May 2019.
World Health Organization. Adherence to long term therapies- evidence for action. World Health Organization. Geneva, Switzerland. 2003. https://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf;jsessionid. Accessed 08 May 2019.
Nicolau I, Ling D, Tian L, Lienhardt C, Pai M. Research questions and priorities for tuberculosis: a survey of published systematic reviews and meta-analyses. PLoS One. 2012;7(7):e42479. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3407095/ .
World Health Organization. The END TB Strategy. Global strategy and targets for tuberculosis prevention, care and control after 2015. Geneva, Switzerland. 2014. https://www.who.int/tb/post2015_strategy/en/. Accessed 15 May 2019.
World Health Organization Tuberculosis control in the South-East Asia Region. Annual TB report 2015. World Health Organization. Regional Office for South-East Asia 2015. https://apps.who.int/iris/handle/10665/205286. Accessed 20 May 2019.
Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental, and social well-being: a field report from South India. Soc Sci Med. 2005;60(8):1845–53.
Marra CA, Marra F, Cox VC, Palepu A, Fitzgerald JM. Factors influencing quality of life in patients with active tuberculosis. Health Qual Life Outcomes. 2004 Oct 20;2:58. https://doi.org/10.1186/1477-7525-2-58.
Aggarwal AN, Gupta D, Janmeja AK, Jindal SK. Assessment of health-related quality of life in patients with pulmonary tuberculosis under programme conditions. The International Journal of Tuberculosis and Lung Disease. 2013;17(7):947–53. https://doi.org/10.5588/ijtld.12.0299.
Atif M, Syed Sulaiman SA, Shafie AA, Asif M, Sarfraz MK, Low HC, et al. Impact of tuberculosis treatment on health-related quality of life of pulmonary tuberculosis patients: a follow-up study. Health Qual Life Outcomes. 2014;12(1):1–11. https://doi.org/10.1186/1477-7525-12-19.
Louw JS, Mabaso M, Peltzer K. Change in health-related quality of life among pulmonary tuberculosis patients at primary health care settings in South Africa: a prospective cohort study. PLoSOne. 2016;11:1–13. https://doi.org/10.1371/journal.pone.0151892.
Muldoon MF, Barger SD, Flory JD, Manuck SB. What are quality of life measurements measuring? Bmj. 1998;316(7130):542–5. https://doi.org/10.1136/bmj.316.7130.542.
Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1:80. https://doi.org/10.1186/1477-7525-1-80.
Miller TL, McNabb SJN, Hilsenrath P, Pasipanodya JWS. Personal and societal health quality lost to tuberculosis. PLoS One. 2009;4(4):e5080. https://doi.org/10.1371/journal.pone.0005080.
Bauer M, Leavens A, Schwartzman K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual Life Res. 2013;22(8):2213–35. https://doi.org/10.1007/s11136-012-0329-x.
Brown J, Capocci S, Smith C, Morris S, Abubakar I, Lipman M. Health status and quality of life in tuberculosis. Int J Infect Dis. 2015;32:68–75. https://doi.org/10.1016/j.ijid.2014.12.045.
Kasthuriaratchi, SK. Direct and indirect cost of treatment, household cost and quality of life of patients with tuberculosis in the district of Colombo. MD Thesis. 2009. Post Graduate Institute of Medicine. University of Colombo, Sri Lanka.
Saleem S, Malik AA, Ghulam A, Ahmed J, Hussain H. Health-related quality of life among pulmonary tuberculosis patients in Pakistan. Qual Life Res. 2018;27:3137–43. https://doi.org/10.1007/s11136-018-1954-9.
Oktavia D, Perwitasari DA & Supadmi W. Quality-adjusted life years (QALYs) of tuberculosis patients in the intensive and continuous phase in a Private Hospital of Yogyakarta, Indonesia. Journal Pharm Biomed Sci. 2016, (January), 4–7.
Kruijshaar ME, Lipman M, Essink-Bot ML, Lozewicz S, Creer D, Dart S, et al. Health status of UK patients with active tuberculosis. International Journal of Tubeculosis and Lung Disease. 2010;14(3):296–302.
Kastien-Hilka T, Abulfathi A, Rosenkranz B, Bennett B, Schwenkglenks M, Sinanovic E. Health-related quality of life and its association with medication adherence in active pulmonary tuberculosis– a systematic review of global literature with focus on South Africa. Health Qual Life Outcomes. 2016;14(1):42. https://doi.org/10.1186/s12955-016-0442-6.
Patil SS, Rawal S, Anuraj R, Rahul S, Doddayya H. A study on assessment of patients health related quality of life during tuberculosis treatment in a tertiary care teaching hospital. Indian Journal of Pharmacy Practice. 2016;9(1):19–25. https://doi.org/10.5530/ijopp.9.1.5.
Maguire GP, Anstey NM, Ardian M, Waramori G, Tjitra E, Kenangalem E, et al. Pulmonary tuberculosis, impaired lung function, disability, and quality of life in a high-burden setting. The International Journal of Tuberculosis and Lung Disease. 2009;13(12):1500–6.
Kavitha V, Srinivas B, Shashikanth P, Muralikrishna B. Assesment of quality of life and oxidative stress in tuberculosis patients visiting directly observed treatment short course centres of Warangal. Asian Journal of Pharmaceutical and Clinical Research. 2016;9(2):200–5. https://innovareacademics.in/journals/index.php/ajpcr/article/view/10382 .
Kisaka SMB, Rutebemberwa E, Kasasa S, Ocen F, Nankya-Mutyoba J. Does health-related quality of life among adults with pulmonary tuberculosis improve across the treatment period? A hospital-based cross sectional study in Mbale Region. Eastern Uganda BMC Research Notes. 2016;9(1):467. https://doi.org/10.1186/s13104-016-2277-y.
Dhingra VK, Rajpal S. Health related quality of life scoring in tuberculosis. Indian J Tuberc. 2003;50:99–104.
Patel P, Ramanuj V, Bala D. Assessment quality of life (QoL) of TB patients registered in tuberculosis units of Ahmedabad Municipal Corporation area by using WHO Short Form-36. Scholars J Appl Med Sci. 2014;2(6F):3303–6.
FSheila Nascimento Pereira de Farias, Célia Regina da Silva Medeiros, Paz, Elisabete Pimenta Araújo, Alexandrina de Jesus Serra Lobo, & Ghelman, Liane Gack. Completeness in caring: study of quality of life in clients with tuberculosis. Escola Anna Nery. 2013, 17(4), 749–754. https://doi.org/10.5935/1414-8145.20130020
Reenen M & Oppe M. EQ-5D-3L user guide: basic information on how to use the EQ-5D-3L instrument. EuroQol Research Foundation 2015
Kularatna S, Whitty JA, Johnson NW, Jayasinghe R, Scuffham PA. EQ-5D-3L derived population norms for health-related quality of life in Sri Lanka. PLoS One. 2014;9(11):1–12. https://doi.org/10.1371/journal.pone.0108434.
Gudex CM, Hawthorne MR, Butler AG, Duffey PO. Measuring patient benefit from botulinum toxin in the treatment of dystonia. Feasibility of cost-utility analysis. Pharmacoeconomics. 1997;12(6):675–84. https://doi.org/10.2165/00019053-199712060-00007.
National Programme for Tuberculosis Control and Chest Diseases (NPTCCD). Annual Report of the National Programme for Tuberculosis Control and Chest Diseases-2017. Ministry of Health, Nutrition & Indigenous Medicine Sri Lanka. 2017.
Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Boston, MA: Pearson; 2012.
Hansel NN, Wu AW, Chang B, Diette GB. Quality of life in tuberculosis: patient and provider perspectives. Qual Life Res. 2004;13(3):639–52.
Chamla D. The assessment of patients’ health-related quality of life during tuberculosis treatment in Wuhan, China. The International Journal of Tuberculosis and Lung Disease. 2004;8(9):1100–6.
Kastien-Hilka T, Rosenkranz B, Sinanovic E, Bennett B, Schwenkglenks M. Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS One. 2017;12(4):e0174605.
Hennekens CH, Julie EB, Sherry LM. Epidemiology in medicine. First ed. USA: Little Brown and Company Boston/Toronto; 1987.
Jaber AAS, Khan AH, Sulaiman SAS, Ahmad N, Anaam MS. Evaluation of health-related quality of life among tuberculosis patients in two cities in Yemen. PLoS One. 2016;11(6):1–19. https://doi.org/10.1371/journal.pone.0156258.
World Health Organization. Global Tuberculosis Report 2017. Geneva: World Health Organization. 2017, https://www.who.int/tb/publications/global_report/gtbr2017_main_text.pdf. Accessed 15 May 2019.
National Programme for Tuberculosis Control and Chest Diseases (NPTCCD). Annual Report of the National Programme for Tuberculosis Control and Chest Diseases-2016. Ministry of Health, Nutrition & Indigenous Medicine Sri Lanka. 2016.
Acknowledgements
The authors would like to acknowledge the support provided by the EuroQol authorizers in granting permission to use the EQ-5D-3L in present study free of charge.
Funding
Financial assistance was granted by Global Fund to fight Acquired Immune Deficiency Syndrome Tuberculosis and Malaria (GFATM). The funding was for the conduct (payment for the data collectors) of the study.
Author information
Authors and Affiliations
Contributions
SS contributed to the concept, design of the study, acquisition of data, analysis and interpretation of data, drafting the article and final approval of the version to be published.
SG contributed to the concept, design of the study, interpretation of data and intellectual input for analysis of data, revising the article critically for important intellectual content and final approval of the version to be published.
SK contributed to the concept, design of the study, analysis and interpretation of data, revising the article critically for important intellectual content, and final approval of the version to be published.
NG contributed to the concept, design of the study, interpretation of data and intellectual input for analysis of data, revising the article critically for important intellectual content and final approval of the version to be published.
The manuscript has been read and approved by all the authors, and the requirements for authorship have been met.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was conducted after ethical approval from the Ethics Review Committee of the University of Colombo Faculty of Medicine Sri Lanka (EC-17-019). Ethical Review Committee of the University of Colombo Faculty of Medicine Sri Lanka is a national ethical review committees in the country. An Ethical Review Committee is not available in the chest clinic where this study was conducted, and therefore, ethical approval was obtained from one of the major national ethical review committees in the country. Thereafter, administrative clearance was taken from the Director of the National Programme for Tuberculosis Control and Chest Diseases (NPTCCD) and from the in-charge medical officer of the CCC to implement the study. The EuroQol authorizers granted permission to use the EQ-5D-3L questionnaire in this research study free of charge and the study was registered in their organization (ID: 12423).
Informed Consent
Informed written consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Seneviratne, S., Ginige, S., Kularatna, S. et al. EQ-5D-3L-Derived Health-Related Quality of Life Among Tuberculosis Patients in Sri Lanka. SN Compr. Clin. Med. 2, 2778–2786 (2020). https://doi.org/10.1007/s42399-020-00571-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00571-y