Abstract
There is emerging evidence that cognitive impairment could be a diabetes mellitus-related complication. It has been suggested that diabetic people are at increased risk of cognitive decline, since the metabolic and vascular disturbances of the disease affect brain function. Additionally, prolonged exposure to olther potential detrimental factors leads to irreversible cognitive decrements over time due to the aging process. Neurocognitive impairment signifies decreased performance in cognitive domains such as verbal and nonverbal memory, both immediate and delayed memory, executive function, attention, visuospatial and psychomotor performance, information processing speed, semantic knowledge, and language abilities. The aim of the present article is to review the existing literature on the issue of the neurocognitive decline in type 2 diabetes. A literature search of databases was performed, using as keywords “diabetes” and “cognitive impairment,” and the reference list of papers so identified were examined, with only English language papers being used. Understanding and preventing diabetes-associated cognitive deficits remains a key priority for future research. It is important to ascertain whether interventions to delay diabetes onset or better control of established disease could prevent some of its adverse effects on cognitive skills.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 DM (T2DM) represents a metabolic disorder with hyperglycemia and glucose intolerance as its main manifestations. There are two underlying mechanisms leading to its gradual clinical development, namely insulin resistance combined with relative deficiency of insulin secretion due to pancreatic beta-cell dysfunction. Both insulin resistance and impairment in beta-cell function have a strong genetic component. As a result, a state of impaired glucose tolerance and/or impaired fasting glucose appears long before leading to overt diabetes. It has been proposed that T2DM onset may occur 9–12 years prior to its clinical diagnosis [1].
The incidence and prevalence of diabetes are expected to rise in the coming decades due to obesity co-existing with other risk factors, such as a sedentary lifestyle and physical inactivity. Obesity, especially in the form of central adiposity, appears to be an important causative factor, as it leads to a chronic, low-grade inflammatory state, linked to insulin resistance. Proinflammatory cytokines are believed to trigger insulin resistance [2]. Both adiposity and hyperinsulinemia have also been associated with impaired glucose tolerance.
Concerning the chronic complications of diabetes, apart from microangiopathy and macroangiopathy, research has recently focused on another possible implication of T2DM, that is, cognitive impairment tentatively linked to the disease since insulin was discovered [3]. It has been proposed that diabetic patients are at increased risk of developing cognitive deficits with a number of additive or synergistic factors affecting brain structure and function. Main focus has been on a variety of metabolic and vascular brain disturbances, namely cerebrovascular and neurodegenerative changes.
Studies evaluating the impact of T2DM on cognitive skills report an accelerated decline over a period of 5 years [4]. These studies compare non-demented diabetic populations to healthy controls in relation to the rate of cognitive decline. Cognitive decrements concern several cognitive domains including verbal memory, executive function, and attention and information processing speed abilities. These reductions seem to be related to a number of factors such as a longer duration of diabetes, poor glycemic control, the presence of microvascular complications, and comorbidities. Taken together, these data are in favor of decreased cognitive abilities in people with T2DM [5].
Moreover, diabetes has been associated with impaired neurocognitive function in the form of dementia. The most commonly found forms of dementia are Alzheimer’s disease (AD) and vascular dementia (VaD), whereas mild cognitive impairment (MCI) is a less severe form of dementia but a considerable risk factor for the development of AD [6]. An increased risk of dementia in diabetic populations has been demonstrated in several studies and meta-analyses with a combined overall relative risk (RR) of 1.51, while more than one fifth of subjects with dementia have T2DM [7].
There has been a growing body of literature on the metabolic contribution of T2DM to the AD neurodegenerative process referring to this with the term “type 3 diabetes” (T3DM) [8]. It has been proposed that AD could represent a brain-specific form of diabetes based on their pathophysiological similarities. These include impaired insulin sensitivity and signaling in CNS, cerebral amyloid beta (Aβ) aggregation and tau hyperphosphorylation, brain vasculopathy, mitochondrial dysfunction, oxidative stress, and activation of the inflammatory response. These processes impair neuronal function and provoke neurodegenerative events, thus leading to a deterioration of cognitive capacities. Although T2DM has been recognized as a risk factor for AD-like dementia, further analysis of their shared pathophysiological pathways is beyond the scope of this article.
Mechanisms of diabetes-associated cognitive dysfunction are today coming under greater scrutiny as the prevalence of diabetes steadily increases because of aging populations, and older age relates to neurocognitive decline. Most research is conducted in populations > 65 years, with only a few studies investigating diabetes starting in midlife. It has been hypothesized that the impact diabetes exerts on cognition increases from midlife onwards, cognitive impairment being greatest between 65 and 75 years and declining thereafter [9].
According to the classification of neuropsychological assessment proposed by van den Berg et al. [10], cognitive domains to be evaluated include general intelligence, memory, processing speed, attention, cognitive flexibility, perception/visual construction, and language. In an attempt to evaluate cognitive status in diabetes, Pasquier [11] provides indications on how to assess cognition in clinical practice by reporting on a few bedside tests together with functional and behavioral scales. He concludes that the most common, diabetes-related cognitive profile involves slowing in motor control, difficulty in retrieving learned material, and impairment in attention and problem solving processes.
Potential agents of cognitive deficits in T2DM
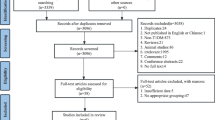
Regarding the T2DM-related neurocognitive dysfunction, several putative causative factors are shown in Fig. 1.
Hyperglycemia
Hyperglycemia, the hallmark of T2DM, has received considerable attention regarding its role in cognitive decline. Increased levels of glucose may have a toxic impact on neurons through the formation of advanced glycation end products (AGEs), which accumulate rapidly in diabetes due to accelerated oxidation of glycated proteins. When coupled with free radicals, AGEs aggravate the oxidative damage to neurons by up-regulating reactive oxygen species [ROS] [12]. Hyperglycemia leads to high intracellular glucose levels, since insulin is not necessary for neuronal glucose uptake. When intracellular glucose is transformed into sorbitol, the cofactor nicotinamide adenine dinucleotide phosphate (NADPH) is consumed by aldose reductase. NADPH is also important for regenerating glutathione, a critical intracellular antioxidant. When glutathione is reduced, an aggravation of oxidative stress results. A cascade of reduced antioxidants along with increased lipid peroxidation products leads to the oxidative stress observed in diabetes, as exemplified in a recent review on this issue [13].
Extensive evidence suggests that mitochondria have a pivotal role in neurodegenerative diseases. They are the central coordinators of energy metabolism, and in neurons, they are vital for the maintenance of synaptic function and transmission. Oxidative stress, insulin resistance, and hyperglycemia are considered major causative factors impairing brain mitochondrial homeostasis. Alterations in their structure (DNA mutations and DNA copy number depletion) together with their impaired function lead to reduced ATP production, decreased mitochondrial biogenesis, and production of reactive oxygen species (ROS). As it has been demonstrated in neurons of streptozocin-induced diabetic mice, these events are related to diabetic neuronal loss and synaptic pathology, thus exerting a negative impact on cognitive performance [14].
In addition, AGEs activate microglia in the central nervous system (CNS), which can become detrimental to neurons when overactivated. In cerebral vessels, AGEs interact with AGE surface receptors (RAGEs), thus interrupting the structural and functional activity of lipids and proteins, which, in turn, leads to a cascade of inflammatory processes. Evidence demonstrates that AGEs and their surface receptors aggravate brain injury, leading to white matter and myelin destruction. Overexpression of RAGEs in neurons and glia cells of cognitive-impaired diabetic mice has been reported [15].
Glucoregulatory control seems to be a key factor for cognitive decrements in diabetics. In a study, cognitive skills of patients were evaluated before and after antidiabetic treatment [16]. Comparing treated with untreated T2DM patients and controls, the researchers found significant differences at baseline. Improvements in verbal memory tasks were attributed to effective glycemic control in diabetic participants. So far, research has indicated that T2DM-related cognitive impairments are partially reversible by means of better glycemic control of the disease.
Experimental studies demonstrate that higher levels of HbA1c negatively correlate with cognitive performance. In a longitudinal panel study, researchers compared adults with and without diabetes. A higher HbA1c level was associated with greater memory decline. Meanwhile, diabetes patients displaying elevated HbA1c exhibited greater deterioration in memory skills [17]. Nevertheless, another study assessing HbA1c and cognitive skills in a middle-aged population concluded that HbA1c was not a significant independent predictor of cognitive impairment. Hyperglycemia, assessed by HbA1c, did not seem to add predictive value beyond the diabetes status itself [18].
Moreover, HbA1c cannot reflect the temporal variations and daily fluctuations of glucose levels. Glycemic fluctuations, especially in poorly controlled patients, could be related to cognitive deficits as well. A cross-sectional study, The Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS), compared diabetic and prediabetic subjects in relation to MRI-demonstrated vascular pathology and volumetrics. It was proposed that the risk of accelerated cognitive decline depends on two parameters, namely severity and duration of hyperglycemia. According to these authors, the two previously mentioned factors significantly aggravate decrements in cognitive skills [19].
Impaired glucose tolerance
The same cognitive domains affected in DM have also been found to be impaired in prediabetic situations, though to a smaller degree. Body tissues gradually develop insulin resistance in the context of prediabetes. Insulin resistance results in a neurodegenerative cascade in the CNS, by increasing AGEs, oxidative stress, mitochondrial dysfunction, and Aβ deposition. These factors negatively affect neuronal functions and promote gliosis, reducing thus the cognitive reserve [20].
According to a systematic review, impaired glucose tolerance (IGT) taking place prior to the development of diabetes is a causative factor of neurocognitive deficits. Since IGT in prediabetic situations is more likely to remain untreated, this can result in a state of longer exposure to increased glucose levels [21]. In the AusDiab study investigating the association of cognitive performance with IGT, an increased risk of decrements in cognitive tasks was attributed to higher glucose levels in non-diabetics [22]. Moreover, a study of ostensibly healthy middle-aged females concluded that cognitive function, namely memory, psychomotor and executive function, is negatively influenced by abnormalities in glucose tolerance prior to the development of diabetes [23].
Hypoglycemia
There is no dispute that a severe, long-lasting episode of hypoglycemia can provoke brain damage, since the brain uses glucose as its main energy source. Impairment of endothelial function can be the result of leucocyte transport and increased platelet activation during hypoglycemic episodes. The hippocampus, basal ganglia, and cortex are mainly affected in terms of neuronal necrosis and gliosis. Hippocampal vulnerability to an acute hypoglycemic state may also account for cognitive deficits. Hypoglycemic neuronal damage and death may be induced by a subtype of the excitatory neurotransmitter N-methyl-d-aspartate (NMDA) receptor that is overactivated. Interestingly, it was observed that hypoglycemia-induced neuronal necrosis could be prevented with the use of an NMDA receptor antagonist. In this review, the authors make the point that NMDA receptor antagonists seem to contribute to neuronal cell survival [24].
It has also been noted that cognitive skills like memory and learning are impaired during acute hypoglycemic episodes with glucose levels < 54 mg/dL [25]. Restoration of glucose levels appears to improve cognitive ability. Moreover, the earlier diabetes begins, the more frequent and severe the hypoglycemic episodes patients experience. Recurrent hypoglycemia together with defective glucose counterregulation and lowering of glycemic threshold leads to a state of “hypoglycemia unawareness,” especially in diabetes of longer duration.
Long-term effects of hypoglycemia have been associated mostly with insulin treatment. A recent systematic review and meta-analysis reached the conclusion that patients on insulin therapy are at greater risk of impaired cognition. Insulin therapy was associated with a 21% increased risk of dementia. More advanced diabetes in terms of duration and severity, treated with insulin, increases the likelihood of severe hypoglycemia. A complex, bidirectional relationship has been proposed between hypoglycemia and cognitive dysfunction. Severe hypoglycemic episodes provoke neuronal dysfunction, thus leading to impaired cognition. At the same time, diabetics with cognitive deficits may exhibit poor disease management, which increases the possibility of experiencing hypoglycemic episodes. However, newer insulin analogs by replicating the endogenous secretion of insulin seem to be promising as they are related to a decreased level of hypoglycemia. Incretins could also be beneficial in reducing the hypoglycemic risk and its associated cognitive deficits [26].
Another literature review on diabetes and cognitive impairment [27], identified three studies demonstrating a significant relationship between hypoglycemia and increased risk of cognitive decline. One of these, a longitudinal study, compared T2DM patients with or without prior hypoglycemic episodes. Investigating the risk of developing cognitive deficits, it was found that patients with prior hypoglycemia had an almost threefold increased risk during the 7-year follow-up compared to those without pre-existing hypoglycemic episodes [28]. Future studies considering duration and severity of diabetes and comorbidities in relation to adverse cognitive outcomes would enable deeper understanding of metabolic-neurocognitive interactions.
The findings on neurocognitive impairment are inconsistent when standard is compared with intensive glycemic control. Hypoglycemia seems to be a side effect of intensive glucose control treatment but not of standard glycoregulation. In a meta-analysis [29] of intensive glycemic control, the author suggested that while it does not decrease the rate of cognitive decline, it increases the hypoglycemic risk. ACCORDION MIND, the observational extension study of The Action to Control Cardiovascular Risk in Diabetes-Memory in Diabetes (ACCORD-MIND) randomized trial, concluded that intensive glycoregulation does not have long-term beneficial effects. When compared to standard management of hyperglycemia, the intensive one did not result in cognitive improvements in diabetic participants [30]. Nevertheless, others [31] are in favor of intensive control, since it may prevent microvascular brain damage and its associated neurocognitive dysfunction. Meanwhile, better glycemic control is a key factor in reducing mortality rate in T2DM. In light of this conflicting evidence, it has been proposed that individualized glycemic targets should be applied, taking into consideration diabetes duration and severity, its long-term complications as well as its comorbidities.
Insulin resistance
Insulin resistance, a factor contributing to the onset of diabetes, seems to play a role in cognitive dysfunction, given the role of insulin action in the brain. Insulin promotes neuronal survival and synaptic plasticity, while it inhibits apoptosis and neuroinflammation. The supply of insulin to the brain is mainly via pancreatic beta-cells, and it crosses the blood–brain barrier (BBB) by means of a saturable transporter mechanism. Dysfunction of the BBB, in terms of decreased permeability to insulin, leads to a smaller quantity of insulin reaching the brain. This has been associated with reduced facilitation of neuronal activation in diabetes. Moreover, a dysfunctional BBB allows potentially toxic substances and metabolites to be transferred to the brain, exerting a negative impact on the CNS and, consequently, on higher cognitive processes. Neuronal insulin resistance also contributes to Aβ accumulation, as it reduces its clearance and degradation by the insulin-degrading enzyme (IDE). In addition to being a metalloprotease that catabolizes insulin, IDE possesses anti-amyloidogenic properties and is highly expressed in the brain. Thus, neurons and mitochondria become more susceptible to Aβ toxicity. These insulin resistance-linked mechanisms lead to a vicious cycle of neuroinflammation and neurodegeneration in the setting of T2DM [32]. Additionally, reduced cerebral glucose metabolism due to insulin resistance leads to neuronal dysfunction. The impaired glucose uptake and utilization in the brain are associated with synaptic dysfunction; thus, neuronal cells become more susceptible to oxidizing insults.
However, there is a debate as to whether there is de novo insulin synthesis in the brain. Evidence supports the notion that insulin is strongly expressed in GABAergic neurogliaform cells of the cerebral cortex [33] and that insulin receptors (IRs) are abundant in the brain. They have been identified in the cortex and hippocampus, regions supporting cognitive function. Insulin regulates mitochondrial function and facilitates long-term potentiation (LTP) in the hippocampus, thus strengthening neuronal synapses which are necessary for memory and learning processes. A human study demonstrated better cognitive performance on selective attention and word recall tasks achieved when exogenous insulin was administered to younger, healthy males [34]. This further corroborates the pivotal role of insulin in human brain function and cognitive performance.
The insulin signaling pathway is thought to be decreased in the diabetic brain due to insulin resistance and deficiency. Aβ affects insulin signaling, since its accumulation inhibits auto-phosphorylation of IR, leading to the inability of IR to bind insulin and phosphorylate insulin receptor substrate (IRS). The interactions of phosphorylated receptors with IRS have a pivotal role in the transmission of neuronal signals in terms of stimulating survival and plasticity and inhibiting apoptosis of neuronal cells [35]. There is evidence of inhibited IRS hippocampal expression in obese rats following a long-term high-fat diet. Deficits in spatial learning and memory along with global cognitive deterioration was linked to insulin hypometabolism in the brain [36]. Defective insulin signaling also exerts a negative impact on the phosphorylation of insulin-like growth factor receptors (IGFRs). Inhibition of the uptake of insulin-like growth factors IGF-1 and IGF-2 in the brain has dire effects on cognition, since they regulate neuronal function via the activation of intrinsic receptor tyrosine kinases [35].
Furthermore, elevated pro-inflammatory cytokines have a negative effect on insulin signaling, as they lead to a state of chronic inflammation that promotes neurodegeneration. Inflammatory mediators also contribute to increased amyloid production, which further promotes oxidative stress, impaired brain insulin signaling, and neurodegenerative cognitive procedures [37].
A rapidly increasing body of literature is describing the neurotrophic effects that insulin exerts on the CNS. After the use of intranasal insulin, an improvement of memory skills has been reported, and insulin administration attenuates cognitive decline through inhibition of neuronal apoptosis and Aβ clearance. It improves cerebral glucose metabolism and preserves brain volume. The intranasal passage enables successful transmission of insulin through the BBB and its delivery to the brain, probably involving the insulin/IR signaling pathway. However, some researchers argue that insulin systemic administration does not have therapeutic implications for cognitive impairment, since it has a lower brain penetration level and it is associated with a higher hypoglycemic risk [38].
β-Amyloid deposition
As mentioned previously, cognitive decline has been linked to accumulation of Aβ, which aggregates in senile plaques. Aβ, α metabolite of the amyloid precursor protein (APP), is derived through the amyloidogenic pathway, with the help of β- and γ-secretases [37]. In the brain, Aβ peptides can bind to RAGEs, thus accelerating oxidative stress and neuronal deficits. The overexpression of RAGEs takes place in neuronal areas associated with cognitive performance, such as the hippocampus and cortex. Recently, researchers investigated the restorative effect that the RAGE-specific inhibitor FPS-ZM1 exerts on abnormal Aβ influx and on cognition in db/db mice. After treatment with the inhibitor, Aβ flow through the BBB was decreased as well as hippocampal amyloid deposition. Neuronal plasticity in the hippocampus and spine deficits were restored, while neuronal apoptosis and cognitive impairment were alleviated [39].
Since Aβ deposition participates in the loss of neuronal surface insulin receptors (IRs), this prevents the activation of the canonical insulin signaling cascade and the release of Aβ to the extracellular compartment. The accumulation of Aβ has toxic effects on neuronal integrity. Aβ is also perceived as a crucial mediator in mitochondrial injury, since it provokes their increased fragmentation and decreased fusion. Proper mitochondrial function is necessary for ATP production, cell signaling pathways, and regulation of apoptosis. Their dysfunction is detrimental to cellular metabolism, and it enhances release of ROS, which in turn exacerbates neuroinflammation processes. Taken together, all these contribute to neuronal impairment, potentially resulting in poor cognitive performance [40].
Of interest is the observation that accumulation of Aβ occurs several years before cognitive deficits become apparent and that Aβ oligomers have also been identified in the pancreatic islet of T2DM patients. This finding further supports the possibility that they have a significant role in DM and its associated impairment in cognitive abilities. Moreover, by applying immunohistochemical techniques on autopsied brain and pancreatic tissue from diabetic patients, a notable similarity between islet and neural Aβ has been identified [41].
Acetylcholine (Ach)
It is generally aknowledged that acetylcholine (Ach) has a crucial role among neurotransmitters influencing cognitive function and memory formation. Ach-mediated neurotransmission is a key factor in the regulation of neuronal network excitability, synaptic plasticity, and proper brain circuitry [42]. The enzyme responsible for its production, Ach transferase, is regulated by insulin. In the context of T2DM, insulin resistance has been associated with down-regulation of Ach synthesis, which appears to have negative repercussions for the structural and functional integrity of neurons. This neuronal dysfunction appears to be a crucial mediator in the evolution of diabetes-related cognitive impairments.
The role of Ach in cognitive decline was exemplified in a rat model of streptozocin-induced diabetes. Ach levels were measured in serum, cerebrospinal fluid (CSF), and brain tissues. Cognitive performance was studied by using the Morris water maze (MWM) test showing that the streptozocin-treated group demonstrated decreased Ach levels compared to controls and cognitive deficits in this group were attributed to impairment of the cholinergic system [43].
Inflammation
It has been demonstrated that both diabetes and insulin resistance are accompanied by inflammation. Insulin resistance, one of the main causes of T2DM, can be the result of inflammation, but it can also lead to an inflammatory state. There is evidence that diabetes exerts its adverse effects on cognitive performance through activation of inflammatory pathways. Diabetics have impaired endothelial-dependent vasodilation mechanisms and higher expression of inflammatory cytokines in the hippocampus and cortex, compared to healthy controls. Key elements of the inflammatory response, such as tumor necrosis factor-a (TNFa), fibrinogen, and plasminogen activator inhibitor-1 (PAI-1), have been found to be elevated in diabetic patients. Hyperglycemia has been proposed as a crucial factor, leading to differentiation of inflammatory regulators, namely macrophages. These cells contribute to the diabetes-related brain inflammation as they stimulate the production of TNF-α, IL-1β, IL-6, and IL-1Ra. The hyperglycemic state of diabetes exerts an effect on gene expression up-regulating cytokine secretion and inflammatory processes[44].
The potential role of white blood cells (WBCs) in the inflammatory hypothesis of T2DM is still evolving. They are thought to worsen insulin resistance and precipitate the clinical development of T2DM via immune system activation. Due to the breakdown of the blood BBB, a large infiltration of immune cells takes place, leading to neuronal cell death [45].
Research so far has proposed a synergistic effect of inflammatory markers, especially IL-6, and apoli poprotein genotype (ApoE) predisposing T2DM patients to poor cognitive performance. ApoE-ε4 carriers demonstrate the lowest cognitive level compared to T2DM patients carrying the E2 or E3 alleles. ApoE-ε4 allele-diabetic carriers have significantly lower global cognition as well as lower scores in executive and memory skills. Neurobiological mechanisms suggest that both ApoE-ε4 allele and diabetes share common neurodegenerative and vascular mechanisms, namely Aβ deposition, which forms hippocampal and cortical neuritic plaques, aggregation of neurofibrillary tangles, as well as cerebral amyloid angiopathy and atherosclerosis [46].
It is possible that ApoE-ε4 allele modifies cognitive performance in diabetics of middle or older age. Research so far has failed to demonstrate a significant association between T2DM and ApoE-ε4 carriership at younger ages [47]. The role of ApoE-ε4 carriership in diabetic neurocognitive impairment remains to be elucidated.
HPA axis dysregulation
lIntegrity of the hypothalamic-pituitary-adrenal axis (HPA) is fundamental for a successful response to stressful stimuli so that homeostasis is restored. In humans, components of the HPA axis regulate circulating cortisol levels, which normally fluctuate in a circadian rhythm, demonstrating morning zenith and evening nadir. Compared with controls, diabetic populations appear to undergo up-regulation of the HPA axis. This leads to a state of hypercortisolemia, which, inter alia, has been shown to negatively affect CNS functions. Glucocorticoids regulate cognition by exerting an effects on brain structures. It has been proposed that glucocorticoids are implicated in cortical atrophy, volume reduction of the hippocampus, and ventricular enlargement [48].
In an attempt to clarify the modifying factors of cognitive decrements in the T2DM setting, researchers compared middle-aged T2DM subjects with controls. After dexamethasone administration, individuals with diabetes exhibited decreased cortisol suppression and impaired HPA axis feedback control. These features were associated with decrements in declarative memory skills. Diabetics demonstrate accelerated cognitive decline due to diminished HPA feedback along with functional hippocampal damage, resulting from exposure to glucocorticoids. The hippocampus appears to be the first region affected by the hyperglycemic environment. Neuronal atrophy or shrinkage of dendritic spines, all related to hippocampal-dependent learning and memory skills, was reported [49].
It has also been suggested that in metabolic conditions, such as T2DM, glucocorticoids have a precipitating role in neuroinflammation. In a genetic animal model of diabetes, db/db mice were treated with a glucocorticoid synthesis inhibitor under 2 weeks. This led to a sensitization of brain microglia to immune challenges as the treatment lowered the threshold for cytokine release. Thus, accumulation of the pro-inflammatory cytokines TNF-α and IL-1β was revealed. The association between neuronal deficits and HPA axis impairment, as well as neuroanatomical changes to the hippocampus, implies a negative impact on cognitive abilities [50].
Furthermore, there is evidence that prolonged raised serum cortisol levels, due to HPA axis persistent stimulation, have a role in the entire spectrum of the metabolic syndrome. Glucocorticoid excess stimulates elevation of plasma glucose levels, and it enhances insulin resistance. Circulating levels of triglycerides and cholesterol are increased, whereas decreased insulin-induced vasodilation causes hypertension. Obesity can derange metabolic homeostasis via adipocyte-secreted proinflammatory cytokines, which in turn impair the cortisol’s circadian rhythmicity. This leads to higher cortisol levels in the evening and early night, being detrimental to tissues on its own, since tissue sensitivity to cortisol is higher at this time [51].
Structural, functional, and metabolic brain changes
Even though the pathophysiology of the relationship between T2DM and neurocognitive impairment remains unraveled, neuroimaging studies support the notion that diabetes-related cognitive decrements can be attributed to brain structural changes. A systematic review points to global and regional brain atrophy in cortical and subcortical regions. The process of brain atrophy is potentially affected by the extent of brain infarcts, diabetes duration, glycemic control achieved, and the history of recurrent hypoglycemic episodes. Concerning regional brain atrophy, neuronal changes in the medial temporal lobe, especially the hippocampus, have been reported in T2DM populations [52].
A reduction in total brain volume accompanied by decrements in cortical and subcortical volume has been identified in diabetes. MRI data on subcortical gray matter (GM) volumes have shown a reduction in T2DM patients compared to healthy controls. Researchers suggest that this indicates that the long-lasting hyperglycemia state negatively affects brain structures and accelerates brain atrophy. Diabetics are especially at risk for deficits in the prefrontal regions, which have been associated with depressive symptoms and decrements in cognition [53]. Meanwhile, an interesting hypothesis suggests that the impact of diabetes on brain pathology is directly related to the age at which the disease starts. It has been proposed that midlife onset of diabetes relates to late-life cognitive deficits through a loss of brain volume. A cohort study investigating cognitive change over a 20-year period reported that individuals with diabetes in midlife experienced 19% greater cognitive age-related decline in comparison with those without diabetes [54].
By using diffusion kurtosis imaging, microstructural changes in white and gray matter integrity have also been detected in diabetic patients compared to controls. It has been proposed that the reduced microstructural integrity and microvascular lesions in diabetes have been attributed to poor disease regulation. Thus, stabilization in the rate of brain atrophy could be achieved by improving glycemic control of the disease [55].
Ventricular enlargement and white matter hyperintensity (WMH) with lesions have also been implicated as potential markers of worse neurocognitive performance in T2DM. Research suggests that white matter microstructural impairments and WMH severity are both linked to the magnitude of impairment in information processing speed, attention, and executive functioning. These changes in brain structural properties have been detected even before clinical diagnosis of the diabetes-related cognitive dysfunction. The severity of white matter lesions has been related to factors such as diabetes duration, HbA1c level, insulin level, hypertension, and neurodegenerative changes [56].
Even before cognitive deficits and brain structural alterations, become evident diabetic patients may exhibit changes in brain functional connectivity (FC). By using resting-state functional MRI (fMRI) in T2DM patients, it was shown that the posterior cingulate cortex (PCC), one of the default mode network (DMN) hubs. An association between decreased FC of the PCC and worse performance in several neurocognitive tests was established. Diabetics also demonstrate aberrant, reduced functional connectivity between the hippocampus and other brain regions. This impairment is related to insulin resistance along with a decreased spontaneous brain activity. A default recognition network and poor encoding, in relation to carrying out cognitive tasks, was hypothesized [57].
Furthermore, fMRI data point to disturbances of low-frequency, spontaneous fluctuations of hemodynamic activity in several brain areas in the T2DM setting. Decreased amplitude of these fluctuations was related to deficits in memory and executive performance tasks carried out by T2DM subjects in comparison to controls [58]. It is believed that these neurocognitive impairments are associated with the diabetes-induced impaired β-cell function and hyperglycemia status. Elevated glycemic parameters of the disease have been linked to impaired brain activity, contributing to cognitive deficits. Interestingly, increased task difficulty and working memory load in diabetic patients led to more severe frontal cortex dysfunction and worse cognitive performance [59].
Additionally, cerebral blood flow (CBF) in cognition regulating areas appears to be decreased in T2DM. This phenomenon is partially mediated by insulin resistance, resulting from the impaired insulin transduction pathway. Insulin resistance impairs vasodilation mechanisms and supply of the brain with glucose, oxygen, and nutritional agents. The decreased availability of nutrients to the brain contributes to the cascade of oxidative stress and inflammatory response. fMRI findings are consistent with changes of regional CBF and oxygenation, as a result of the increased Aβ load in the diabetic brain [60].
Microvascular disease
It has been suggested that T2DM patients are prone to cognitive deficits as cerebral microvascular disease (MVD) emerges. There is evidence that hyperglycemia contributes to MVD through impaired insulin-mediated glucose disposal. This leads to stiffening of small brain arteries and microvascular remodeling. Decreased neurogenesis, neuronal cell death, cerebral microbleeds, and white-matter lesions have been linked to cerebral small-vessel damage rendering the brain susceptible to deficits in a broad range of neurocognitive abilities [61].
Microvascular complications of diabetes have been identified as potential factors involved in functional brain abnormalities and cognitive decline. Microvascular disease, particularly in the retina, may reflect structural and metabolic changes taking place in the diabetic brain. It has been speculated that retinal vessels and cerebral small vessels share similar embryological sources, thus providing an explanation for their link to cognitive alterations. Interestingly, data from both the ACCORD-MIND and the ACCORD-Eye studies, including T2DM patients, support the association between diabetic retinopathy and impaired cognitive performance. It has been proposed that diabetic retinopathy constitutes an independent risk factor for cognitive deficits [62].
Cerebrovascular disease, cardiovascular disease, and other metabolic syndrome factors
Although knowledge is as yet incomplete, vascular disturbances occurring in diabetes are implicated in the pathophysiology of cognitive decline. Inadequate cerebral drainage of Aβ and up-regulation of APP both exacerbate Aβ deposition in brain parenchyma. This appears to be a potential mechanism leading to functional neuronal impairment. Insulin resistance in the brain, manifesting a breakdown of the insulin-signaling pathway, together with hyperinsulinemia, has been suggested as a pathogenic cerebral signaling pathway, linking T2DM and cerebrovascular disease [63].
Cardiovascular disease (CVD) in the form of stroke, transient ischemic attack, or coronary heart disease is the leading cause of death on a global scale. Diabetic populations are at greater risk of CVD compared to controls. The occurrence of CVD is related to major risk factors, such as obesity, high cholesterol and triglyceride levels, and high blood pressure [64]. In a meta-analysis of 102 prospective studies, it was observed that diabetic patients have an increased risk of ischemic stroke, which may further contribute to cognitive deficits along with its concomitant neurodegenerative process [65].
Apart from hyperglycemia and hyperinsulinemia, the metabolic syndrome (MetS) also encompasses hypertension and dyslipidemia, which are risk factors for atherosclerosis and cerebrovascular disease. It has been proposed that MetS contributes to neuroinflammation, since it disrupts the BBB, increasing its permeability. As a consequence, pathogens and immune cells are infiltrating the brain. There they disrupt the function of glial and neuronal cells, and ttrigger cell death. Consequently, hormonal dysregulation occurs, resulting in CNS insulin resistance. Impaired insulin signaling provokes mitochondrial dysfunction and oxidative stress, exacerbating neurodegeneration. MetS is a major contributing factor in T2DM-associated cognitive decline [66].
Considering the impact of MetS on neuronal health, crucial brain functions, including cognition, have been linked to glutamate, a key element of neurotransmission. Due to oxidative stress, a large amount of ROS is produced, leading to increased levels of glutamate. The latter triggers the secretion of pro-inflammatory cytokines, thus exacerbating the inflammatory and neurodegenerative process. In order to investigate the effect T2DM exerts on cognitive capacity, researchers replicated animal models of T2DM by exposing them to monosodium glutamate (MSG) during the neonatal period. Compared to controls, MSG-treated animals demonstrated high expression of inflammatory cytokines, Aβ deposition, and impaired neuronal synaptic plasticity in the hippocampus. Long-term potentiation (LTP) of hippocampal neurons was also inhibited. LTP, reflecting persistent strengthening of synapses and long-lasting neuronal signal transmission, is tightly correlated with hippocampal synaptic plasticity and the processes of learning and memory formation [67].
The components of MetS often occur together and interact with each other. In the population-based Framingham study [68], the lower scores of diabetic participants in tests of verbal and visual memory, auditory attention, abstract reasoning, and verbal fluency were attributed to an interaction between diabetes and hypertension. The Third National Health and Nutrition Examination Survey (NHANES III) reported that the co-existence of hypertension and diabetes exerted a negative impact on the metabolic-related cognitive performance, after adjustment for demographic and socioeconomic variables [69].
Poor control of hypertension has been related to a common T2DM complication, namely diabetic autonomic neuropathy (DAN). Even though inadequate hypertension management is a risk factor for cognitive deficits, there is as yet limited evidence suggesting a relationship between DAN and impairment of cognitive skills. The hypothesis that they share a common pathophysiological mechanism is based on the assumption that they affect brain areas (hypothalamus, brainstem, and cortex) that control both cognitive and autonomic function. There is the possibility that cognitive skills worsen because of the cerebral hypoperfusion that orthostatic hypotension provokes. However, this cognitive dysfunction may be a transient phenomenon during an orthostatic hypotension episode. Comparing T2DM patients with DAN to diabetics without DAN and controls, poorer cognitive performance on visual memory tasks but not on verbal memory performance was demonstrated in diabetics with DAN. Nevertheless, DAN co-existing with diabetes was related to a higher frequency of microangiopathy and retinopathy [70].
Adiposity, a key factor of cardiovascular and cerebrovascular disease, has been associated with cognitive impairment through the mechanism of insulin resistance. Free fatty acids produced by adipocytes lead to the overexpression of TNF-α, a well-known inflammatory cytokine, which increases Aβ production in the brain. The obesity-induced metabolic disorder seems to play a critical role in cognitive dysfunction via systemic pro-inflammation and neuroinflammation processes in the hippocampus [71].
As a metabolic disorder, T2DM attenuates changes in lipid metabolism, namely dyslipidemia. Among other factors, the hyperglycemic state promotes oxidative stress through a disturbance of lipids. The latter promote neurodegeneration and apoptosis by having an impact on neuronal activity. Mitochondrial and endothelial function is also impaired. These biochemical processes lead to cerebral damage and impairment of cognitive skills [72].
Nevertheless, other authors suggest that diabetics on statin treatment may exhibit altered brain insulin levels. It has been proposed that brain insulin signaling participates in the regulation of memory and learning processes. Statins may interfere with the pathway of insulin transfer to the brain via transporters embeded in the BBB, thus down-regulating insulin uptake in the brain and impairing learning and memory formation skills [73, 74].
Recently, a review has addressed the question whether statin therapy may increase the risk of diabetogenicity. Based on two meta-analyses of statin trials, authors report a risk of 9–12% of T2DM on individuals on statin treatment. Statins may contribute to prolonged periods of peripheral hyperinsulinemia and interfere with insulin sensitivity and secretion. The risk of developing T2DM is associated with longer duration of statin use, and it is dose-dependent and differs among statin types. Research points to simvastatin being related to increased risk of diabetes, whereas the least diabetogenic statin appears to be pravastatin. However, there is consensus that the benefits of statin treatment in reducing cardiovascular events exceed the risk of diabetes being developed [75].
Depression
Diabetic populations have an increased risk of depression compared to controls. Reports indicate that the comorbidity of depressive-like behavior in T2DM is considerable. The two diseases share common pathophysiological mechanisms, involving mainly insulin resistance and chronic cytokine-related inflammatory response. Changes in HPA axis activity, cortisol levels, and noradrenergic and serotoninergic brain neurotransmission are key factors linking the two diseases. The depressive symptomatology has been associated with hippocampal atrophy as well as deficits in memory and learning abilities [76].
Cerebral microvascular disease (MVD), manifesting as cerebral microbleeds, lacunar infarcts, and white-matter hyperintensities (WMHs) has a pivotal role in cognitive decline [77]. There is a recent review and meta-analysis of observational data in humans, stressing the contribution of MVD to late-life depression. It was conlcuded that frontal brain structures and connecting pathways regulating mood are disrupted, since cerebral microvascular integrity is impaired in diabetes. In support of this concept, microvascular dysfunction was related to a greater risk of depression and impaired cognition [78]. The interaction between depression and cognitive decrements in diabetes remains to be elucidated with further research.
Conclusion
It has been suggested [79] that cognition can be negatively affected mainly during two crucial periods: childhood when the brain is still developing and late adulthood because of neurodegenerative changes due to the aging process. Outside these two critical periods, any micro- and macrovascular complications that occur in the setting of T2DM will most likely lead to development of neurocognitive impairment. However, it is unlikely that any single factor is solely responsible for neurocognitive decline among diabetes patients: instead, they appear to act synergically, leading to deficits of cognitive skills. Thus, there is a continued need for patient education on maintaining a healthy life style through diet, exercise, and when necessary, medication. Meanwhile, the identification of novel therapeutic strategies that could prevent or even reverse the diabetes-related cognitive decrements should be further addressed in future research.
References
Harris MI, Klein R, Welborn TA, Knulman MW (1992) Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care 15(7):815–819
Dye L, Boyle NB, Champ C, Lawton C (2017) The relationship between obesity and cognitive health and decline. Proc Nutr Soc 74(4):443–444. https://doi.org/10.1017/S0029665117002014
Miles WR, Root HF (1922) Psychologic tests applied to diabetic patients. Arch Int Med 30(6):767–777
Yates KF, Sweat V, Yau PL, Turchiano MM (2012) Impact of metabolic syndrome on cognition and brain: a selected review of the literature. Arterioscler Tromb Vasc Biol 32(9):2060–2067. https://doi.org/10.1161/ATVBAHA.112.252759
Moheet A, Mangia S, Seaquist ER (2015) Impact of diabetes on cognitive function and brain structure. Ann N Y Acad Sci 1353:60–71. https://doi.org/10.1111/nyas.12807
Pal K, Mukadam N, Petersen I, Cooper C (2018) Mild cognitive impairment and progression to dementia in people with diabetes, prediabetes and metabolic syndrome: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol 53:1149–1160. https://doi.org/10.1007/s00127-018-1581-3
Moon JH (2016) Endocrine risk factors for cognitive impairment. Endocrinol Metab 31:185–192. https://doi.org/10.3803/EnM.2016.31.2.185
de la Monte SM, Wands JR (2008) Alzheimer’s disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol 2:1101–1113. https://doi.org/10.1177/193229680800200619
van den Berg E, de Craen AJM, Biessels GJ, Gussekloo J, Westendorp RGJ (2006) The impact of diabetes mellitus to cognitive decline in the oldest of the old: a prospective population-based study. Diabetologia 49:2015–2023
van den Berg E, Kloppenborg RP, Kessels RPC, Kappelle LJ, Biessels GJ (2009) Type 2 diabetes mellitus, hypertension, dyslipidemia and obesity: a systematic comparison of their impact on cognition. Biochim Biophys Acta 1792(5):470–481. https://doi.org/10.1016/j.bbadis.2008.09.004
Pasquier F (2010) Diabetes and cognitive impairment: how to evaluate the cognitive status? Diabetes Metab 36(Suppl 3):S100–S105. https://doi.org/10.1016/S1262-3636(10)70475-4
Dobi A, Bravo SB, Veeren B et al (2019) Advanced glycation end-products disrupt human endothelial cells redox homeostasis: new insights into reactive oxygen species production. Free Radic Res 1:1–20. https://doi.org/10.1080/10715762.2018.1529866
Ito F, Sono Y, Ito T (2019) Measurement and clinical significance of lipid peroxidation as a biomarker of oxidative stress: oxidative stress in diabetes, atherosclerosis, and chronic inflammation. Antioxidants (Basel) 25(3):8. https://doi.org/10.3390/antiox8030072
Solanki I, Parihar P, Shetty R, Parihar MS (2017) Synaptosomal and mitochondrial oxidative damage followed by behavioral impairments in streptozocin induced diabetes mellitus: restoration by Malvastrum tricuspidatum. Cell Mol Biol 63(7):94–101. https://doi.org/10.14715/cmb/2017.63.7.16
Cho HJ, Xie C, Cai H (2018) AGE- induced neuronal cell death is enhanced in G2019S LRRK2 mutation with increased RAGE expression. Transl Neurodegener 7:1. https://doi.org/10.1186/s40035-018-0106-z
Cooray G, Nilsson E, Wahlin A et al (2011) Effects of intensified metabolic control on CNS function in type 2 diabetes. Psychoneuroendocrinology 36(1):77–86. https://doi.org/10.1016/j.psyneuen.2010.06.009
Pappas C, Andel R, Infurna FJ, Setharaman S (2017) Glycated haemoglobin (HbA1c), diabetes and trajectories of change in episodic memory performance. J Epidemiol Community Health 71(2):115–120. https://doi.org/10.1136/jech-2016-207588
Breitling LP, Olsen H, Müller H et al (2014) Self- or physician-reported diabetes, glycemia markers, and cognitive functioning in older adults in Germany. Am J Geriatr Psychiatry 22(11):1105–1115. https://doi.org/10.1016/j.jagp.2013.06.004
Schneider ALC, Selvin E, Sharrett AR et al (2017) Diabetes, prediabetes, and brain volumes and subclinical cerebrovascular disease on MRI: the atherosclerosis risk in communities neurocognitive study (ARIC- NCS). Diabetes Care 40(11):1514–1521. https://doi.org/10.2337/dc17-1185
Bitra VR, Rapaka D, Akula A (2015) Prediabetes and Alzheimer’s disease. Indian J Pharm Sci 77(5):511–514
Ganmore I, Beeri MS (2018) The chicken or the egg? Does glycaemic control predict cognitive function or the other way around? Diabetologia 61(9):1913–1917. https://doi.org/10.1007/s00125-018-4689-9
Anstey KJ, Sargent-Cox K, Eramudugolla R, Magliano DJ, Shaw JE (2015) Association of cognitive function with glucose tolerance and trajectories of glucose tolerance over 12 years in the AusDiab study. Alzheimers Res Ther 7(1):48. https://doi.org/10.1186/s13195-015-0131-4
Lamport DJ, Chadwick HK, Dye L, Mansfield MW, Lawton CL (2014) A low glycaemic load breakfast can attenuate cognitive impairments observed in middle aged obese females with impaired glucose tolerance. Nutr Metab Cardiovasc Dis 24(10):1128–1136. https://doi.org/10.1016/j.numecd.2014.04.015
Welters A, Klüppel C, Mrugala J et al (2017) NMDAR antagonists for the treatment of diabetes mellitus- current status and future directions. Diabetes Obes Metab 19(Suppl 1):95–106. https://doi.org/10.1111/dom.13017
Bie-Olsen LG, Kjaer TW, Pedersen-Bjergaard U et al (2009) Changes of cognition and regional cerebral activity during acute hypoglycemia in normal subjects: a H2 150 positron emission tomographic study. J Neurosci Res 87(8):1922–1928. https://doi.org/10.1002/jnr.22002
McMillan JM, Mele BS, Hogan DB, Leung AA (2018) Impact of pharmacological treatment of diabetes mellitus on dementia risk: systematic review and meta-analysis. BMJ Open Diab Res Care 16(1):6. https://doi.org/10.1135/bmjdrc-2018-000563
Ojo O, Brooke J (2015) Evaluating the association between diabetes, cognitive decline and dementia. Int J Environ Res Public Health 12(7):8281–8294. https://doi.org/10.3390/ijerph120708281
Lin CH, Sheu WH (2013) Hypoglycaemic episodes and risk of dementia in diabetes mellitus: 7 year follow up study. J Intern Med 273(1):102–110. https://doi.org/10.1111/joim.12000
Tuligenga RH (2015) Intensive glycemic control and cognitive decline in patients with type 2 diabetes: a meta-analysis. Endocr Connect 4(2):R16–R24. https://doi.org/10.1530/EC-15-0004
Murray AM, Hsu FC, Williamson JD et al (2017) ACCORDION MIND: results of the observational extension of the ACCORD MIND randomized trial. Diabetologia 60(1):69–80
Kawamura T, Umemura T, Hotta N (2012) Cognitive impairment in diabetic patients: can diabetic control prevent cognitive decline? Journal of Diabetes Investigation 3(5):413–423. https://doi.org/10.1111/j.2040-1124.2012.00234.x
Umegaki H (2014) Type 2 diabetes as a risk factor for cognitive impairment: current insights. Clin Interv Aging 9:1011–1019. https://doi.org/10.2147/CIA.548926
Molnár G, Faragó N, Kocsis ÁK et al (2014) GABAergic neurogliaform cells represent local sources of insulin in the cerebral cortex. J Neurosci 34(4):1133–1137. https://doi.org/10.1523/JNEUROSCI.4082-13.2014
Kern W, Peters A, Fruehwald-Schultes B et al (2001) Improving influence of insulin on cognitive functions in humans. Neuroendocrinology 74(4):270–280
Kullmann S, Heni M, Hallschmid M et al (2016) Brain insulin resistance at the crossroads of metabolic and cognitive disorders in humans. Physiol Rev 96(4):1169–1209. https://doi.org/10.1152/physrev.00032.2015
Hu DH, Li YL, Liang ZJ et al (2018) Long-term high-fat diet inhibits hippocampal expression of insulin receptor substrates and accelerates cognitive deterioration in obese rats. Nan Fang Yi Ke Da Xue Xue Bao 38(4):460–465
de Nazareth AM (2017) Type 2 diabetes mellitus in the pathophysiology of Alzheimer’s disease. Dement Neuropsychol 11(2):105–113. https://doi.org/10.1590/1980-57642016dn11-020002
Tumminia A, Vinciquerra F, Parisi M, Frittitta L (2018) Type 2 diabetes mellitus and Alzheimer’s disease: role of insulin signalling and therapeutic implications. Int J Mol Sci 24:19 (11). https://doi.org/10.3390/ijms19113306
Wang H, Chen F, Du YF et al (2018) Targeted inhibition of RAGE reduces amyloid-β influx across the blood-brain barrier and improves cognitive deficits in db/db mice. Neuropharmacology 131:143–153. https://doi.org/10.1016/j.neuropharm.2017.12.026
Butterfield DA, Domenico FD, Barone E (2014) Elevated risk of type 2 diabetes for development of Alzheimer disease: a key role for oxidative stress in brain. Biochim Biophys Acta 1482(9):1693–1706. https://doi.org/10.1016/j.bbadis.2014.06.010
Leino M, Popova SN, Alafuzoff I (2017) Transactive DNA binding protein 43 rather than other misfolded proteins in the brain is associated with islet amyloid polypeptide in pancreas in aged subjects with diabetes mellitus. J Alzheimer Dis 59(1):43–56. https://doi.org/10.3233/JAD-170192
Rivera EJ, Goldin A, Fulmer N et al (2005) Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer’s disease: link to brain reductions in acetylcholine. J Alzheimers Dis 8(3):247–268
Zhou X, Zhu Q, Han X et al (2015) Quantitative-profiling of neurotransmitter abnormalities in the disease progression of experimental diabetic encephalopathy rat. Can J Physiol Pharmacol 93(11):1007–1013. https://doi.org/10.1139/cjpp-2015-0118
Moganti K, Li F, Schmuttermaier C et al (2017) Hyperglycemia induces mixed M1/M2 cytokine profile in primary human monocyte-derived macrophages. Immunobiology 222(10):952–959. https://doi.org/10.1016/j.imbio.2016.07.006
Zhang Y, Bai J, Wu H, Ying JY (2015) Trapping cells in paper for white blood cell count. Biosens Bioelectron 69:121–127. https://doi.org/10.1016/j.bios.2015.02.019
Zhen J, Lin T, Huang X et al (2018) Association of ApoE genetic polymorphism and type 2 diabetes with cognition in non-demented aging Chinese adults: a community based cross-sectional study. Aging Dis 9(3):346–357. https://doi.org/10.14336/AD.2017.0715
van Eersel MAE, Joosen H, Gansevoort RT et al (2013) The interaction of age and type 2 diabetes on executive function and memory in persons aged 35 years or older. PLoS One 8(12). https://doi.org/10.1371/journal.pone.0082991
Kino T, Chrousos GP (2005) Glucocorticoid effects on gene expression. In: Steckler T, Kalin NH, Reul JMHM (eds) Handbook of stress and the brain. Elsevier B.V, Amsterdam, pp 295–311
Bruehl H, Wolf OT, Sweat V et al (2009) Modifiers of cognitive function and brain structure in middle-aged and elderly individuals with type 2 diabetes mellitus. Brain Res 14(1280):186–194. https://doi.org/10.1016/j.brainres.2009.05.032
Dey A, Hao S, Erion JR et al (2014) Glucocorticoid sensitization of microglia in a genetic mouse model of obesity and diabetes. J Neuroimmuno 269(1–2):20–27. https://doi.org/10.1016/j.jneuroim.2014.01.013
Nader N, Chrousos GP, Kino T (2010) Interactions of the circadian CLOCK system and the HPA axis. Trends Endocrinol Metab 21(5):277–286. https://doi.org/10.1016/j.tem.2009.12.011
Lee JH, Choi Y, Jun C et al (2014) Neurocognitive changes and their neural correlates in patients with type 2 diabetes mellitus. Endocrinol Metab (Seoul) 29(2):112–121. https://doi.org/10.3803/EnM.2014.29.2.112
Cui D, Liu X, Liu M et al (2019) Subcortical gray matter structural alterations in prediabetes and type 2 diabetes. Neuroreport 30(6):441–445. https://doi.org/10.1097/WNR.0000000000001224
Rawlings AM, Sharrett AR, Schneider AL et al (2014) Diabetes in midlife and cognitive change over 20 years: a cohort study. Ann Intern Med 161(11):785–793. https://doi.org/10.7326/M14-0737
Xiong Y, Sui Y, Zhang S et al (2018) Brain microstructural alterations in type 2 diabetes: diffusion kurtosis imaging provides added value to diffusion tensor imaging. Eur Radiol 24(9):1997–2008. https://doi.org/10.1007/s00330-018-5746-y
Zhang Y, Cao Y, Xie Y et al (2019) Altered brain structural topological properties in type 2 diabetes mellitus patients without complications. J Diabetes 11(2):129–138. https://doi.org/10.1111/1753-0407.12826
Tan X, Liang Y, Zeng H et al (2019) Altered functional connectivity of the posterior cingulate cortex in type 2 diabetes with cognitive impairment. Brain Imaging Behav 5. https://doi.org/10.1007/s11682-018-0017-8
Liu D, Duan S, Zhou C et al (2018) Altered brain functional hubs and connectivity in type 2 diabetes mellitus patients: a resting-state fMRI study. Front Aging Neurosci 6(10):55. https://doi.org/10.3389/fnagi.2018.00055
Chen Y, Liu Z, Zhang J et al (2014) Altered brain activation patterns under different working memory loads in patients with type 2 diabetes. Diabetes Care 37(12):3157–3163. https://doi.org/10.2337/dc14-1683
Arnold SE, Arvanitakis Z, Macauley-Rambach SL et al (2018) Brain insulin resistance in type 2 diabetes and Alzheimer disease: concepts and conundrums. Nat Rev Neurol 14(3):168–181. https://doi.org/10.1038/nrneurol.2017.185
Stehouwer CDA (2018) Microvascular dysfunction and hyperglycemia: a vicious cycle with widespread consequences. Diabetes 67(9):1729–1741. https://doi.org/10.2337/dbi17-0044 Review
Hugenschmidt CE, Lovato JF, Ambrosius WT et al (2014) The cross-sectional and longitudinal associations of diabetic retinopathy with cognitive function and brain MRI findings: the action to control cardiovascular risk in diabetes (ACCORD) trial. Diabetes Care 37:3244–3252. https://doi.org/10.2337/dc14-0502
de la Monte SM, Wands JR (2005) Review of insulin, insulin-like growth factor expression, signaling, and malfunction in the central nervous system: relevance to Alzheimer’s disease. Journal of Alzheimer’s disease: JAD 7:45–61
Balakumar P, Maung-U K, Jagadeesh G (2016) Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res 113(Pt A):600–609. https://doi.org/10.1016/j.phrs.2016.09.040
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733):2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Van Dyken P, Lacoste B (2018) Impact of metabolic syndrome on neuroinflammation and the blood-brain barrier. Front Neurosci 12:930. https://doi.org/10.3389/fnins.2018.00930
Jin L, Li YP, Feng Q et al (2018) Cognitive deficits and Alzheimer-like neuropathological impairments during adolescence in a rat model of type 2 diabetes mellitus. Neural Regen Res 13(11):1995–2004. https://doi.org/10.4103/1673-5374.239448
Mahmood SS, Levy D, Vasan RS, Wang TJ (2014) The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet 383(9921):999–1008. https://doi.org/10.1016/S0140-6736(13)61752-3
Palta P, Huang ES, Kalyani RR et al (2017) Hemoglobin A1c and mortality in older adults with and without diabetes: results from the National Health and Nutrition Examination Surveys (1988-2011). Diabetes Care 40(4):453–460. https://doi.org/10.2337/dci16-0042
Zilliox LA, Chadrasekaran K, Kwan JY, Russell JW (2016) Diabetes and cognitive impairment. Curr Diab Rep 16(9):87. https://doi.org/10.1007/s11892-016-0775-x
van Gemert T, Wölwer W, Weber KS et al (2018) Cognitive function is impaired in patients with recently diagnosed type 2 diabetes, but not type 1 diabetes. J Diabetes Res 9:1470476. https://doi.org/10.1155/1470476
Rojas-Carranza CA, Bustos-Cruz RH, Pino-Pinzon CJ et al (2018) Diabetes-related neurological implications and pharmacogenomics. Curr Pharm Des 24(15):1695–1710. https://doi.org/10.2174/1381612823666170317165350
Goh DA, Dong Y, Lee WY et al (2014) A pilot study to examine the correlation between cognition and blood biomarkers in a Singapore Chinese male cohort with type 2 diabetes mellitus. PLoS One 9(5):e96874. https://doi.org/10.1371/journal.pone.0096874.eCollection
Zhao WQ, Alkon DL (2001) Role of insulin and insulin receptor in learning and memory. Mol Cell Endocrinol 177(1–2):125–134
Laakso M, Kuusisto J (2017) Diabetes secondary to treatment with statins. Curr Diab Rep 17(2):10. https://doi.org/10.1007/s11892-017-0837-8
Martinac M, Pehar D, Karlović D et al (2014) Metabolic syndrome, activity of the hypothalamic-pituitary-adrenal axis and inflammatory mediators in depressive disorder. Acta Clin Croat 53(1):55–71
Wardlaw JM, Smith EE, Biessels GJ et al (2013b) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12(8):822–838. https://doi.org/10.1016/S1474-4422(13)70124-8
Rensma SP, van Sloten TT, Launer LJ, Stehouwer CDA (2018) Cerebral small vessel disease and risk of incident stroke, dementia and depression, and all-cause mortality: a systematic review and, meta-analysis. Neurosci Biobehav Rev 90:164–173. https://doi.org/10.1016/j.neubiorev.2018.04.003
Gradman TJ, Laws A, Thompson LW, Reaven GM (1993) Verbal learning and/or memory improves with glycaemic control in older subjects with non-insulin-dependent diabetes mellitus. J Am Geriatr Soc 41(12):1305–1312
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karvani, M., Simos, P., Stavrakaki, S. et al. Neurocognitive impairment in type 2 diabetes mellitus. Hormones 18, 523–534 (2019). https://doi.org/10.1007/s42000-019-00128-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-019-00128-2