Key Summary Points
To identify factors influencing Discharge Directly Home (DDH) from an acute hospital following hip fracture, as opposed to Discharge to an Alternative Location (DAL).
AbstractSection FindingsYounger patients who were independently mobile pre-fracture were more likely to be DDH. Timely surgery with early post-operative mobilisation and a shorter length of stay increased the odds of DDH.
AbstractSection MessageThe Irish Hip Fracture Standards incorporate 2 out the 3 modifiable factors identified in this paper, which reinforces the importance of the IHFS in improving patient outcomes.
Abstract
Purpose
Although home continues to be the place from which the majority of patients are admitted, less than one third of patients are Discharged Directly Home (DDH) following hip fracture. Once ready for discharge, DDH as opposed to Discharge to an Alternative Location (DAL), i.e., community care, rehabilitation facility or long-term care, is a high priority for patients and clinicians alike. Not only is DDH integral to the quality of life of patients, it is also an essential driver of the socioeconomic cost of hip fracture care.
Methods
We analysed 21,819 cases in the Irish Hip Fracture Database from 2013 to 2019. Descriptive and analytical statistics were conducted.
Results
29% (n = 6476) of patients were DDH during the study period. On multivariate analysis, the odds of DDH decreased as age increased (OR 0.28, p < 0.01, 95% CI 0.24–0.34). Patients who were independently mobile prior to fracture were 47% more likely to be DDH (OR 1.47, p < 0.01, 95% CI 1.29–1.68). Those mobilised early post operatively were 24% more likely to be DDH (OR 1.24, p < 0.01, 95% CI 1.06–1.45). Patients who waited > 72 h prior to surgery were 30% less likely to be DDH (OR 0.70, p < 0.01, 95% CI 0.56–0.88).
Conclusion
The authors identified patient characteristics that increased the likelihood of DDH, i.e., younger patients independently mobile prior to fracture, who received timely surgery and early post-operative mobilisation. The Irish Hip Fracture Standards (IHFS) incorporate 2 out the 3 modifiable factors identified, which reinforces the importance of the IHFS in improving patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is a serious public health issue owing to an ageing population and increasing frailty in older adults. In Ireland, there are approximately 3700 hip fractures per annum, with 60% of cases occurring in those over 80 years [1]. Hip fractures among older adults are one of the leading causes of hospitalisation and result in considerable morbidity, mortality and healthcare usage [2]. Although there is much evidence underpinning outcome measures, such as mortality, less is known about the factors influencing discharge destination following hip fracture. Once ready for discharge, Discharge Directly Home (DDH), as opposed to Discharge to an Alternative Location (DAL), i.e., rehabilitation facility, community or long-term care, is a high priority for hip fracture patients and clinicians alike. Not only is DDH integral to the quality of life of patients, it is also a driver of the socioeconomic cost of hip fracture care.
Hip fracture patients incur three times the in-patient cost compared to age-matched non-hip fracture patients, and post-acute utilisation of healthcare is also substantial due to the need for rehabilitation after surgery [3]. From an Irish healthcare perspective, the estimated cost of one admission for hip fracture is approximately €12,687 with inpatient care being a significant component of the cost incurred [4]. The total direct and indirect cost of falls and fractures for people aged ≥ 65 years is estimated at €404 million per annum, accounting for an estimated 4.2% of all public health expenditure in Ireland [5]. Identifying factors to stratify hip fracture patients into those most likely to be DDH as opposed to DAL could help streamline the postoperative phase. In turn, this could facilitate efficient discharge planning to the most appropriate and cost effective discharge destination.
Although home continues to be the place from which the majority of Irish patients (85%) are admitted, less than one third of patients are DDH from the acute hospital [1, 6]. Prognostic factors for DDH and remaining there 12 months after hip fracture are those that reflect better health prior to fracture and better functionality at hospital discharge [7]. Salar et al. demonstrated that younger females without cognitive impairment who were independently mobile prior to fracture were most likely to be DDH from acute hospital following hip fracture [8]. A US based study of > 33,000 hip fracture patients showed that increasing age and American Society of Anaesthesiologists (ASA) Grade II or greater predicted discharge to a destination other than home [9].
The rising incidence of hip fractures coupled with increasing frailty and potential for dependency post fracture has implications for service delivery, discharge planning and healthcare costs. Premature discharge or discharge to an unsuitable environment can result in the need for subsequent healthcare utilisation, such as visits to the emergency department or re-hospitalisation [10]. Furthermore, discharging patients to a location other than home frequently delays discharge, while the necessary logistical arrangements are made [11]. Identifying subgroups most likely to be DDH on admission could make the discharge process more efficient [12].
Discharged directly home—international landscape
There is considerable variation from country to country in terms of the proportion of hip fracture patients DDH following hip fracture. For instance, in England, Wales and Northern Ireland (NHFD) 52% of patients are DDH, which is the highest of the hip fracture registries [13]. In comparison, Italy has the lowest proportion of patients DDH at 11% [14]. Ireland sits midway amongst international counterparts with 22% of patients DDH in 2018 (Fig. 1) [15]. It is important to note that characteristics of the patient population and healthcare systems vary considerably from country to country, which renders direct comparisons challenging [16].
International overview of discharge directly home from acute hospital [15]
Discharged directly home—national landscape
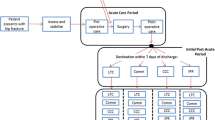
In 2017, the IHFD launched a quality improvement initiative with a specific focus on getting patients home following hip fracture. The theme of the campaign ‘From Broken Bone to Walking Home’ focused on ensuring hip fracture patients received the right care at the right time to enable them to be discharged home directly. There was considerable engagement with the quality improvement initiative across all 16 trauma sites and a 4% improvement in DDH was seen the following year. The distribution of patients discharged to the each discharge location is depicted in Fig. 2.
Aim
This paper aims to identify factors influencing DDH from an acute hospital following hip fracture as opposed to DAL.
Methods
Irish hip fracture database
The Irish Hip Fracture Database (IHFD) was established in 2012 with a clear focus on driving improvements in patient care and data quality. It is a clinically led, web-based system, where data are collected though the Hospital In-Patient Enquiry (HIPE) portal, in association with the Healthcare Pricing Office (HPO). The audit is clinically supported by the Irish Institute of Trauma and Orthopaedic Surgery (IITOS) and the Irish Gerontological Society (IGS). Operational management is provided by the National Office for Clinical Audit (NOCA). The Irish Hip Fracture Standards (IHFS) are the standards against which the Irish healthcare services are benchmarked. The IHFS are in alignment with the Best Practice Tariff (BPT) for hip fractures, which focuses on 8 core parameters; 6 clinical and 2 for data quality and governance (Fig. 3).
All sixteen trauma units in the Republic of Ireland voluntarily submit data on all patients over age 18 that are discharged following hip fracture. Data are reported on patients over the age of 60 in the National report. Data are collected for each hip fracture episode from admission to 30 day post discharge. Data are entered locally via IHFD audit coordinators, with support from the local IHFD clinical lead and NOCA. A specific data entry form is used to record details of an extensive number of variables ranging from the patients’ pre-operative functional status to the type of surgery and clinical outcomes. These variables are measured against the IHFS and are linked to the BPT. The IHFD data set with full description of the variables collected are described in the most recent IHFD annual report [1]. The IHFD is a timely and accurate database with 99% coverage.
Within the IHFD, low energy trauma is the most common cause of hip fracture with almost a quarter of patients recorded as having previously sustained a fracture. The most common type of surgical repair is cemented hemi-arthroplasty [36% (n = 1282)] followed by internal fixation with a short IM nail [16% (n = 558)] [1]. Three quarters of surgical repairs are conducted under spinal anesthesia, either alone [53% (n = 1,886)] or in combination with a nerve block [21% (n = 757)] [1]. There has been an increase in the degree of comorbidity of patients, i.e., ASA Grade III (severe systemic disease) admissions increased from 39% (n = 767) in 2013 to 53% (n = 1799) in 2019 [1]. A full description of the trends in hip fracture care in the Republic of Ireland from 2013 to 2018 has been published elsewhere [17].
Statistical analysis
We retrospectively analysed 21,819 cases in the IHFD from 2013 to 2019. Data were exported from Microsoft Excel into Stata® (version 16) for analysis. Descriptive statistics were used to describe the patient characteristics, care pathway and outcomes. Continuous variables such as time spent in the Emergency Department (ED) and time to surgery were divided into categories in keeping with the IHFS. A one way analysis of variance (ANOVA) was used to measure variation between individual hospitals in relation to discharge practices. Univariate logistic regression was undertaken to assess the impact of variables routinely collected by the IHFD on the likelihood of DDH following hip fracture. A multivariate logistic regression model was constructed using the statistically significant variables from univariate analysis. Model fit for the final multivariate model was satisfactory (Pseudo R2 0.11). Missing data was minimal and treated as missing at random. An adjustment for outliers was not required for this data set. A value of p < 0.05 indicated statistical significance.
Results
Patient characteristics
Data pertaining to discharge destination was available for 100% (n = 21,819) of cases from 2013 to 2019, with 29% (n = 6476) of patients DDH from acute hospital. There were inherent differences between patients DDH compared to those DAL. These differences ranged from general health and functionality pre-fracture to the care pathway during admission (Table 1).
Distribution of DDH from individual hospitals
The proportion of patients DDH varied according to each individual hospital (Fig. 4). ‘Hospital O’ had the largest proportion of patients DDH [58.9% (n = 880)], whereas ‘Hospital I’ had the lowest [13.9% (n = 142)]. The difference in discharge practices between hospitals was statistically significant (p < 0.00). However, it is important to note that each hospital varies in terms of case mix, staffing levels, presence of an ortho-geriatrician etc., which may affect discharge practices. The IHFD strives to minimise variation between individual units and promotes a standardised approach to hip fracture care.
Univariate logistic regression
On univariate analysis, younger patients were more likely to be DDH than older patients (OR 0.26, p < 0.01, 95% CI 0.24–0.29) (Table 2). Those with a high functional mobility pre-fracture [as defined by New Mobility Score (NMS) > 6] were more than twice as likely to be DDH compared to those with poor pre-fracture mobility (OR 2.72, p < 0.01, 95% CI 2.48–2.97). During the in-patient journey, the likelihood of DDH decreased as time to surgery increased by each 24 h increment (p < 0.01). Patients who were not mobilised on the day of or after surgery were 33% less likely to be DDH (OR 0.67, p < 0.01, 95% CI 0.62–0.73). In relation to length of stay, patients admitted for greater than 15 days were less likely to be DDH (OR 0.85, p < 0.01, 95% CI 0.77–0.93). Sex was not a statistically significant predictor of discharge destination.
Multivariate logistic regression
A multivariate logistic regression model was constructed using the statistically significant variables from univariate analysis (Table 3). On multivariate analysis the odds of being DDH decreased as age increased (OR 0.28, p < 0.01, 95% CI 0.24–0.34). Patients who were independently mobile prior to fracture were 47% more likely to be DDH compared to those with low functional mobility pre-fracture (OR 1.47, p < 0.01, 95% CI 1.29–1.68). In terms of source of admission, patients admitted from a nursing home or long stay facility had little chance of being DDH.
During the course of hospital admission, patients who waited > 72 h prior to surgery were 30% less likely to be DDH (OR 0.70, p < 0.01, 95% CI 0.56–0.88). Length of hospital stay was also a significant variable as patients admitted for less than 15 days had a greater chance of being DDH (OR 1.18 p < 0.03, 95% CI 1.01–1.38). Patients who were mobilised early post operatively were 24% more likely to be DDH (OR 1.24, p < 0.01, 95% CI 1.06–1.45).
Discussion
This is the first time that factors influencing discharge destination for Irish hip fracture patients have been investigated on a national scale and the findings have implications for clinical practice. For many patients, hip fracture can mean a change in living accommodation after discharge from acute hospital. Although the vast majority (82%) of patients are admitted from home, less than one third of patients are DDH. For those admitted from locations other than home, discharge to the residence from which they were admitted is central to minimising disruption to the patients social circumstances and quality of life post fracture. The findings of this paper illustrate the inherent differences between patients DDH compared to those DAL, both in terms of pre-fracture functionality and care pathway. Some of these differences are modifiable, whereas others are not. Multivariate analysis showed that younger patients who were independently mobile pre-fracture were 47% more likely to be DDH (OR 1.47, p < 0.01, 95% CI 1.29–1.68). The literature investigating post-acute pathways in hip fracture care supports the intuitive finding that patients in better health pre-fracture are more likely to be DDH. Other studies have found increasing age, presence of comorbidities, cogitative impairment and functional dependence to be significant predictors of discharge to a nursing home or long-term care facility [8, 18, 19].
Three modifiable factors within the care pathway were identified. Timely surgical intervention with early post-operative mobilisation and shorter length of stay were statistically significant predictors of DDH. Patients who waited > 72 h for surgical repair were 30% less likely to be DDH (OR 0.70, p < 0.01, 95% CI 0.56–0.88). This finding is similar to other studies which showed that early operative treatment was associated with an improved ability to return to independent living and a shorter hospital stay. Al-Ani et al. demonstrated that patients who were operated on > 36 h (OR 0.44) or > 48 h (OR 0.33) after admission were less likely to return to independent living after 4 months (p < 0.05) [20]. Nanjayan et al. also demonstrated that patients who waited > 36 h to surgery for medical reasons were more likely to be discharged to a location other than from where they were admitted (OR 4.35, p < 0.01, 95% CI 1.21–15–79) [21].
In relation to length of stay, patients admitted for less than 15 days had a greater chance of being DDH (OR 1.18, p < 0.03, 95% CI 1.01–1.38). However, the association between increased length of stay and DAL could be due to logistical issues. A recent study by Salonga-Reyes et al. showed that a lack of available rehabilitation facilities, residential care or supported care beds was the most common reason for discharge delay, followed by administrative delays in obtaining decisions on funding for home care packages [22]. Family refusal was also a factor in a small portion of cases. Proactively identifying patients with a high probability of returning home at an early stage in the care pathway could allow for suitable support services to be set up for those returning home, while allowing a timely search for rehabilitation, community or long-term care facilities for those with a low probability of being discharged home directly. The analysis in this paper has identified patient characteristics that increase the likelihood of DDH, i.e., younger patients independently mobile prior to fracture, who receive timely surgery with early post-operative mobilisation.
There is a wide variation in length of stay across the hip fracture registries worldwide, most likely due to different patient demographics, case mix, care pathways and healthcare systems. For instance, the mean (median) length of stay in Spain is 11 (9.4) days, UK 15.6 (12) days, Ireland 20 (13) days, Australia 9.2 (7.7) days and a mean of 8 days for both Sweden and Denmark [12]. Length of stay is a multi-faceted variable that involves a complex interplay between patient, process and organisational factors. Each region has a different proportion of patients operated on early, mobilised early, reviewed by a Geriatrician etc. all of which could affect the length of hospital admission. It is also important to note that length of stay can be somewhat an artificial metric as patients may be discharged early from an acute hospital to another healthcare facility for a short period of time and subsequently discharged home. Currently, the IHFD is unable to capture secondary discharge location as it utilises HIPE data, which records the primary discharge destination only. Notwithstanding, there is an opportunity to optimise each step of the patient journey, as encompassed by the IHFS so that patients have every chance of returning home post fracture.
Most strikingly, patients who were mobilised early post operatively were 24% more likely to be DDH (OR 1.24, p < 0.01, 95% CI 1.06–1.45). This is not the first time that early mobilisation has been identified as a key factor in hip fracture care. Sheehan et al. demonstrated that early mobilisation was associated with a twofold increase in the adjusted odds of being discharged within 30 days of surgery [23]. Similarly, Ferris et al. investigated the impact of early mobilisation on in-hospital mortality and showed that older males who were not mobilised on the day of or after surgery had the highest risk of in-hospital mortality (p < 0.01) [24]. Following on from this, one new standard for early mobilisation on the day of or after surgery was added to the IHFS. The ability to be mobilised early post operatively is a good composite measure of both patient and organisational factors in orthogeriatric care.
The discharge of an older person from an acute hospital to the most appropriate setting following hip fracture surgery is complex. The findings presented in this paper further reinforce the importance of the IHFS in improving patient outcomes. More specifically, the IHFS incorporate 2 of the 3 modifiable process measures highlighted above, i.e., surgical repair of the fracture within 48 h (IHFS 2) and early post-operative mobilisation by a physiotherapist (IHFS 7). These are also quality standards of other international audits. The modifiable factors identified should be optimised so that patients can return home post hip fracture and regain their pre-fracture functionality.
Limitations
The IHFD is a large data set of over 21,000 hip fracture patients with excellent data coverage and data completeness. All 16 trauma centres in the Republic of Ireland are included; therefore, it is representative of the Irish population and there is no selection bias. It is important to note that a certain proportion of patients DAL may get home eventually after rehabilitation etc. However, the authors were not able to account for this as HIPE captures the initial discharge destination only and does not record follow-up data on mid-to-long-term outcomes. Second, the authors were not able to address whether DDH or DAL was appropriate for the patient in the context of other variables not recorded by the IHFD. Moving forward, qualitative research capturing the patients’ perspective on other variables that may influence discharge destination such as social support or home environment would be useful. Further analysis looking at the variability in discharge practices between hospitals is warranted.
Conclusion
Although the vast majority of patients are admitted from home, less than one third of patients are DDH. This paper identified inherent differences between those DDH as opposed to DAL, both in terms of patient characteristics and care pathway. Younger patients who were independently mobile pre-fracture were more likely to be DDH. Timely surgery with early post-operative mobilisation and a shorter length of stay increased the odds of DDH. The IHFS incorporate 2 of the 3 modifiable process measures identified, which reinforces the importance of the IHFS in improving patient outcomes.
References
National Office of Clinical Audit (2020). Irish Hip Fracture Database National Report 2019. Dublin: National Office of Clinical Audit. ISSN 2565–5388. https://www.noca.ie/audits/irish-hip-fracture-database. (Accessed 21 Nov 2020)
Pitzul KB, Wodchis WP, Carter MW et al (2016) Post-acute pathways among hip fracture patients: a system-level analysis. BMC Health Serv Res 16:275. https://doi.org/10.1186/s12913-016-1524-1
Stukel TA, Fisher ES, Alter DA et al (2012) Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. J Am Med Assoc 10:1037–1045
Kelly MA, McGowan B, McKenna MJ, Bennett K, Carey JJ, Whelan B, Silke C (2018) Emerging trends in hospitalisation for fragility fractures in Ireland. Ir J Med Sci 187:601–608
Gannon B, O’Shea E, Hudson E (2008) Economic consequences of falls and fractures among older people. Ir Med J 101(6):170–173 (PMID: 18700509)
Baker PN, Salar O, Ollivere BJ et al (2014) Evolution of the hip fracture population: time to consider the future? A retrospective observational analysis. BMJ Open 4:e004405. https://doi.org/10.1136/bmjopen-2013-004405
Gamboa-Arango A, Duaso E, Malafarina V et al (2020) Prognostic factors for discharge to home and residing at home 12 months after hip fracture: an Anoia hip study. Aging Clin Exp Res 32(5):925–933. https://doi.org/10.1007/s40520-019-01273-9 (Epub 2019 Aug 3 PMID: 31377999)
Salar O, Baker PN, Forward DP, Ollivere BJ, Weerasuriya N, Moppett IK, Moran CG (2017) Predictors of direct home discharge following fractured neck of femur. Ann R Coll Surg Engl 99(6):444–451. https://doi.org/10.1308/rcsann.2017.0021 (PMID:28660828;PMCID:PMC5696970)
Sivasundaram L, Tanenbaum JE, Mengers SR, Trivedi NN, Su CA, Salata MJ, Ochenjele G, Voos JE, Wetzel RJ (2020) Identifying a clinical decision tool to predict discharge disposition following operative treatment of hip fractures in the United States. Injury 51(4):1015–1020. https://doi.org/10.1016/j.injury.2020.02.108 (Epub 2020 Feb 21 PMID: 32122627)
Barberi S, Mielli L (2018) Rehabilitation and discharge. In: Hertz K, Santy-Tomlinson J (eds) Fragility fracture nursing perspectives in nursing management and care for older adults. Springer
Deakin DE, Wenn RT, Moran CG (2008) Factors influencing discharge location following hip fracture. Injury 39(2):213–218. https://doi.org/10.1016/j.injury.2007.07.012 (Epub 2007 Dec 11 PMID: 18062969)
Pitzul KB, Wodchis WP, Kreder HJ, Carter MW, Jaglal SB (2017) Discharge destination following hip fracture: comparative effectiveness and cost analyses. Arch Osteoporos 12(1):87. https://doi.org/10.1007/s11657-017-0382-8 (PMID: 28965297)
The Royal College of Physicians (2017) National hip fracture database annual report 2018. eISBN 978–1–86016–736–2. https://nhfd.co.uk/20/hipfractureR.nsf/docs/2018Report. (Accessed 20 Oct 2020)
Zurlo A, Bellelli G (2018) Orthogeriatrics in Italy: the gruppo Italiano Di Ortogeriatria (GIOG) audit on hip fractures in the elderly. Geriatric Care 4(2):33–35
Ojeda-Thies C, Sáez-López P, Currie CT et al (2019) Spanish national hip fracture registry (RNFC): analysis of its first annual report and international comparison with other established registries. Osteoporos Int 30(6):1243–1254. https://doi.org/10.1007/s00198-019-04939-2 (Epub 2019 Mar 23 PMID: 30904929)
Leigheb F, Vanhaecht K, Sermeus W et al (2012) The effect of care pathways for hip fractures: a systematic review. Calcif Tissue Int 91:1–14
Walsh M, Ferris H, Coughlan T et al (2020) Trends in hip fracture care in the Republic of Ireland from 2013 to 2018: results from the Irish Hip Fracture Database. Osteoporos Int. https://doi.org/10.1007/s00198-020-05636-1
Aharanoff G, Barsky A, Hieber R, Zuckerman J, Koval K (2004) Predictors of discharge to a skilled nursing facility following hip fracture surgery in New York State. Gerontology 50:298–302
Maciejewski ML, Radcliff TA, Henderson WG, Cowper Ripley D, Vogel WB, Regan E, Hutt E (2013) Determinants of postsurgical discharge setting for male hip fracture patients. J Rehabil Res Dev 50(9):1267–1276. https://doi.org/10.1682/JRRD.2013.02.0041 (PMID: 24458966)
Al-Ani AN, Samuelsson B, Tidermark J, Norling A, Ekström W, Cederholm T, Hedström M (2008) Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Joint Surg Am 90(7):1436–1442. https://doi.org/10.2106/JBJS.G.00890 (PMID: 18594090)
Nanjayan SK, John J, Swamy G, Mitsiou K, Tambe A, Abuzakuk T (2014) Predictors of change in “discharge destination” following treatment for fracture neck of femur. Injury 45(7):1080–1084. https://doi.org/10.1016/j.injury.2014.02.005 (Epub 2014 Feb 15 PMID: 24613613)
Salonga- Reyes A, Scott IA (2017) Stranded: cause and effects of discharge delays involving non acute in patients requiring maintaineance care in a tertiary referral hospital general medicine service. Aust Health Rev 41(1):54–62. https://doi.org/10.1071/AH15204 (PMID: 27028335)
Sheehan KJ, Goubar A, Almilaji O, Martin FC, Potter C, Jones GD, Sackley C, Ayis S (2021) Discharge after hip fracture surgery by mobilisation timing: secondary analysis of the UK National Hip Fracture Database. Age Ageing 50(2):415–422. https://doi.org/10.1093/ageing/afaa204 (PMID:33098414;PMCID:PMC7936027)
Ferris H, Brent L, Coughlan T (2020) Early mobilisation reduces the risk of in-hospital mortality following hip fracture. Eur Geriatr Med 11(4):527–533. https://doi.org/10.1007/s41999-020-00317-y (Epub 2020 Apr 9 PMID: 32297275)
Funding
No funding, grants or financial support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethical approval
Research ethics approval was obtained from the St James Hospital/ Tallaght University Hospital Research Ethics Committee, in accordance with the European Communities (Clinical Trials on Medicinal Products for Human Use) Regulations 2004 & ICH GCP Guidelines.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferris, H., Brent, L., Sorensen, J. et al. Discharge destination after hip fracture: findings from the Irish hip fracture database. Eur Geriatr Med 13, 415–424 (2022). https://doi.org/10.1007/s41999-021-00556-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00556-7