Abstract
The global role of action of family health promotion in all aspects of family health behavior, family health capacity, and family health status has received inadequate empirical examination relative to its potential significance, notably within a causal model pathway. The purposes of the study were to determine whether family health capacity and family health status maintain internal and external dimensions that influence family health behavior/family health status and analyze the predictive factor influence on major variables in the theoretical model of family health promotion. Analyses were conducted on data derived from 86 families that were affected by Duchenne muscular dystrophy (DMD) or spinal muscular atrophy (SMA). The participants (113; mean age, 42.68 years) including parents, siblings, patients, and caregivers completed self-reported questionnaires. Family support and family hardiness were the mediators on family general health, family general function, and family health behavior. Family support produced a mediator effect on general family function through the power to propose ideas/plans. However, general family health produced a mediator effect on general family function through geography, family support, and family hardiness, as well as a mediator effect on family health behavior through family support and family hardiness, and represented by family monthly income. Families were important sources of interpersonal influence that could increase or decrease commitment, challenge, or control to health promotion behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Duchenne muscular dystrophy (DMD) and spinal muscular atrophy (SMA) are progressive neuromuscular diseases with genetic factors characterized by muscle weakness (Billard et al. 1992; Chen, Wang, and Chang 2006; Kostova et al. 2007). There is currently no effective treatment for both diseases. Eventually, those diseases caused repeated respiratory infection, pneumonia, and highly dependent in daily activity. The incidence increased with age and negatively influenced quality of life (Chen and Jong 2006). The former disease was an X-linked-inherited recessive disorder in locus Xp21, caused by a dystrophin deficiency or mutation (Kliegman et al. 2007). The latter disease, on the other hand, was an autosomal recessive inheritance caused by the motor neuron decline of spinal cord anterior horn, lacking exon 7 on the SMN1 gene (Kostova et al. 2007; Wang et al. 2007).
Both children with DMD and SMA experienced progressive muscle weakness, comorbid conditions including neurological symptoms and cardiopulmonary function progressive failure (Biggar 2006). These symptoms reduced family function, and it was difficult to maintain family health promotion lifestyle (FHPL). Family health behaviors and families’ transition among family stress, resources, and adaptation would help to improve family health function (Chen et al. 2013a). Providing health promotion to families of children with chronic disease was one of the strategies that the International Family Nursing Association (IFNA) in an attempt to contend with increase members of family affected by DMD and SMA.
Some reports presented that family transition of children with muscular dystrophy impacted action of FHPL and threatened family health, exactly induced severe family distress including depression, isolation, helplessness, infertility, or inadequacy (Chen and Jong 2006; Chen et al. 2013b). Assessing relative factors of family health promotion model would help family of children with muscular dystrophy to play healthy role and to support family coherence through supporting group in seeking social welfare for limited time and resource. As well as providing sick children in good learning and caring environment increasingly cooperate to facilitate healthy lifestyle and extend to lifelong learning program (Martin et al. 2013).
The majority of researchers have focused on FHPL and family behaviors that were associated with family structure, family cohesion, family beliefs and values, family development stage, and place of residence (Ford-Gilboe 1997, 2002; Soubhi et al. 2004). Family will encounter system interactions that may influence the domains of family hardiness, support, and function according to the prognosis of the DMD child’s disability. Therefore, the process of promoting and protecting families’ health through the courses of their lives involves supporting mental and social health in their homes, as well as reducing the incidence of, and suffering from, primary diseases and injuries (WHO Regional Office for Europe 1999). This lack of clarity can result in healthcare needs that include health crisis assessment, prevention of health risk, and nutrition needs.
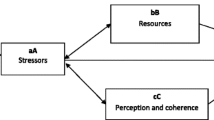
The “concept and its relationship of family health promotion model” (Chen 2008; Chen et al. 2013c; Chen and Clark 2007, 2010; Chen and Jong 2006; Chen et al. 2017) consists of four dynamical interacting components that environment factors may affect (1) family health capacity: including family hardiness (similar to family resilience) (Kuo 1994; McCubbin et al. 2001) and family support (Smilkstein 1978; Smilkstein et al. 1982); (2) family health behavior (family health promotion lifestyle); (3) family health status: including the FAD-GF (general family health) (Epstein et al. 1983) and general health (Duke Health Profile) (Parkerson 2002); (4) health needs, including health crisis assessment, health risk, and nutrition needs. Figure 1 briefly summarizes each of these components (Chen et al. 2017).
Concept and its relationship on family health promotion model retrieved from Chen et al. (2017)
Family health capacity variables were derived from the family stress, resources, and adaptation model test (Chen and Clark 2010). The family of a child with DMD/SMA can share the burdens of the child’s stressful situations, endure changes in the illness process, and find personal significance or meaning. The researchers evaluated family hardiness and utilized the results to help to, along with family support, promote family function (Chen and Clark 2007) and family health (Chen and Clark 2010). If the family could not obtain resources to assist them to cope with stress, they might have already depleted their energy and resources, by the time the chronic condition has deteriorated the child’s health.
Family health behavior plays an important role in maintaining personal health promotion lifestyle patterns to foster self-protective actions for preventing disease, reducing behaviors that increase health risk, facilitating effective adaptation to and coping with illness, and focusing on the potential and strength for growth within families of children with disability (Chen et al. 2017). Health promotion life pattern with dimensions of health behaviors includes nutrition, exercise, health responsibility, stress management, social support, and life appreciation (Chen et al. 2006), also includes in family health promotion lifestyles. Healthy behaviors and unhealthy behaviors are related to health status that may be affected by health needs such as maintaining normal BMI or body weight control that focuses on nutrition and exercise (Barnes et al. 2004; Chen et al. 2006).
Family health status combines the outcome of general family function and general health. Family functioning is a reliable predictor of parent adjustment, which has been found to solve problems, present affection, and meet the families’ needs to promote and achieve the balance of family health status (Chen and Clark 2010; Chen et al. 2014b). General health refers to families’ ability to maintain perceived, physical, mental, and social health and to maintain emotional balance to reduce anxiety, depression, pain, and disability. The Duke measures these factors, which includes positive health (physical, mental, social health, perceived health, self-esteem) and negative health (disability, pain, depression, anxiety, and depression-anxiety) (Parkerson 2002).
The researchers conducted the model derived from family stress, resources, and adaptation model to determine which major factors were influenced by family health promotion, and to elucidate its relationship with family health promotion model (Chen et al. 2013a; Chen and Clark 2007). The study further aims to (1) determine whether family health capacity and family health status maintain internal and external dimensions that influence family health behavior/family health status (2) analyze predictive factors’ influence on the major variables (family health needs, health potential capacities, family health lifestyle patterns, and family health status) in the theoretical model for family of children with muscular dystrophy. The research questions were (1)What relationships exist among the major variables within the family health promotion model? (2)Which model specifies the utilizing two main sets of equations in measurement equations and structural equations? (3)Which pathways exist between the major variables in the model? (4) Which model is a good fit for causal effect?
The following hypotheses were developed to lead the research which focused on family health behaviors. Hypothesis 1: Significant relationships exist between family support, family hardiness, general health, general family function, and family health behavior; and there are significant contributing effects on general family function and family health behavior. Hypothesis 2: Family support and family hardiness act as mediators of participants’ family health behavior through family hardiness, general health, and general family function. Hypothesis 3: Family support and family hardiness act as mediators of participants’ family health function through family support, general health, and family health behavior. Hypothesis 4: Confounding factors exist, such as geography, income, and power to propose an idea/plan to influence general family function and family health behavior through family support, family hardiness, and general health.
Method
Participants
The criteria for inclusion were as follow: (1) the family had children with DMD/SMA; and (2) the parents, patients, siblings, or major primary caregivers in the family agreed to participate and could literate in, or could communicate with, Mandarin or Taiwanese. Families were excluded from the study if the members suffered from a medical condition, were under 20 years old, or refused to participate in the study. The participants counted total was 113, consisting of 42 families of children with DMD (n = 55, mean age = 42.07, SD = 1.42) and 44 families of children with SMA (n = 58, mean age = 43.33, SD = 1.30). Both 86 families were from parents (n = 83, mean age = 45.89, SD = 7.27), siblings (n = 4, mean age = 23, SD = 3.56), patients (n = 21, mean age = 32, SD = 9.70), and caregivers (n = 5, mean age = 50, SD = 4.43).
Procedure
The study procedures were approved by the university hospital institute review board. The muscular association staffs recruited participants, who gave permission for their family’s participation via a telephone call. The researchers asked potential families to invite every family member who was over the age of 20 years to participate. After the families agreed to participate in the study, the researcher collected data by mailing a packet containing information, informed consents, questionnaires, and stamped envelopes. The researchers contacted each family if they did not response within 2 weeks or until researchers received their responses.
Measures
The researchers measured family health behaviors through health-promoting lifestyle pattern (Chen et al. 2006; Loveland-Cherry and Bomar 2004) and health status via the Duke Health Profile-17 item scale and the FAD-GF 12-item scale. The Health Promotion Life Pattern (HPLP) utilizes 40 items on a 5-point Likert scale ranging from 1 (not at all) to 5 (always), with a range score of 40–200 (Chen et al. 2006; Loveland-Cherry and Bomar 2004). In all, six subscales include nutrition, exercise, health responsibility, stress management, social support, and life appreciation that higher scores indicate an enhanced lifestyle pattern (Brolin and Shiraishi 2011). The internal consistency reliabilities of the HPLP scale and its subscales in the study range from .75 to .95, and their item-total correlations range from .35 to .69.
To assess family health capacities by the Family Hardiness Index (FHI) and the Family APGAR (FAPGAR), the FHI utilizes 20 items containing three subscales each to survey the commitment, challenge, and control through self-reporting on a 4-point Likert scale including 0 (false), 1 (most false), 2 (most true), and 3 (true), with a higher score indicating a higher level of family hardiness (Kuo 1994; McCubbin et al. 2001). The internal consistency reliabilities of the FHI scale is adequate (alpha = .82) with subscales ranging from 0.50 to 0.79 with a score range of 0–60, construct validity range from 0.70–0.86, and their item total correlation range of 0.69–0.80. The FAPGAR utilizes five items to measure adaptability, partnership, growth, affection, and resolve on a three-point scale, including 0 (hardly ever), 1 (some of the time), and 2 (almost always), with higher scores indicating higher satisfaction with family support (Smilkstein 1978; Smilkstein et al. 1982). The internal consistency reliabilities of the FAPGAR scale were good (alpha = .90), with a score range of 0–10. The construct validity and AVE of the scale were 0.90 and 0.65, respectively.
To measure family function status by the Family Assessment Device–General Function (FAD-GF) and the Duke Health Profile (DHP), the FAD-GF 12 items were presented on a four-point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree), where lower score indicated healthier families (Epstein et al. 1983). The items consisted of healthy function and unhealthy function, including six items in each dimension. The internal consistency reliability of the FAD-GF scale was good (alpha = .89). The construct validity and AVE of the scale were 0.99 and 0.92, respectively.
Additionally, the DHP-17 items presented on a Likert scale (0–2) which consisted of positive functional health (physical, social, mental, perceived health, and self-esteem) and negative functional health (anxiety, depression, combined anxiety-depression, pain, and disability) (Parkerson 2002). Participants chose one of three options to indicate the extent to which a specific statement describes them, i.e., 0 = “no, does not describe me at all,” 1 = “describes me somewhat,” or 2 = “yes, describes me exactly.” Others items addressed rating the extent of difficulty experienced in an area, where “2 = none, 1 = some, or 0 = a lot”, or rating in terms of frequency during a week “0 = none, 1 = sometimes, 2 = a lot or 0 = 5–7 days, 1 = 1–4 days, 2 = none” (Parkerson, Broadhead, and Tse 1990). The internal consistency reliabilities of the DHF scale were adequate (alpha = .77), and its subscales ranged from 0.41 to 0.66, with a score range of 0–100 (all item scores were transformed of the raw score from 0, 1, and 2 into 0, 50, and 100). The construct validity of the scale was good (.83).
The Health Needs Assessment (HNS) included a personal health risk factors assessment (Chan and Perry 2012) that examined body structure (height/wrist ratio; small-male, > 10.4; female, > 11; medium-male, 9.6–10.4; female, 0.1–11; large-male, < 9.6; female, < 10.1), body mass index (BMI: weight in kg/(height in m)2, and lumbar/waist ratio. The nutritional assessment (Chen et al. 2017) included, on the other hand, evaluation of BMI condition (BMI ranges are starvation: under 18.5, malnutrition: under 19, healthy body weight: between 19 and 25, over body weight: between 26 and 27, health problem crisis increased: body weight between 28 and 30, illness obesity: body weight over 30), health risk problem (will increase if waist circumference equals or over 35 in. for female, equals or over 40 in. for male; or decrease if waist circumference: under 35 in. for female, under 40 in. for male), body weight assessments (compared with ideal body weight are obese: over 20%, overweight: over 10–20%, normal: under or over 10%, underweight: under 10–20%, emaciate: under 20%), nutrition condition (body weight/ideal body weight ratio: severe malnutrition < 70%, moderate malnutrition = 70–79%, mild malnutrition = 80–89%, normal = 90–109%, overweight = 110–120%, and obese > 120%), health risk (lumbar/waist ratio, high health risk: male > .95, female > .85; moderate health risk: male = .90–.95, female = .80–.85; low health risk: male < .90, female < .80).
The Family Structure Analysis (FSA) examined family types, family development stages, family power structure, residence location, employment, monthly incomes, education levels, and amount of time spent watching television. Potential family types included nuclear, extended, single, reorganization, cohabitation, or living with others. The family development stages included families with members who are children attending preschool or school, adolescents, adults, or retired family members. The family power structures were denoted by: (1) decision-making by parents or others; (2) problem-solving by parents or others; and (3) maintaining the power to propose ideas/plans directly, indirectly, directly/indirectly, or via silence. The residence location options included rural, suburban/town, and urban. The employment options included professional, government/administrator, and technique/labor/none. The monthly income options included less than NT$30,000; NT $30,000–50,000; or more than NT$50,000. Education options included less than/equal to 9 years or more than 12 years. The amount of time spent watching television included options of 0 h, 1–3 h, or more than 3 h.
Data Analyses
The researchers of the current study analyzed data via an IBM SPSS Version 22 and Amos 19. Ratings for scales that differed by two muscular dystrophy groups and five different cluster of family members were analyzed with a t test or an ANOVA test for means. The researchers compared the baseline characteristics of the two groups utilizing an independent-sample t test for continuous data and Pearson chi-square for categorical variables, to detect a moderate effect size for t test (d = 0.53) and a large effect size for f test (d = 0.40) utilizing a two-tailed significant test with a power of .8 and a α level of .05 (Faul et al. 2009; Faul et al. 2007). The variable identified potential correlates of family function by a family member on the basis of bivariate analyses. The researchers analyzed predictors of contribution via hierarchical multiple regression. Then, the researchers assessed model assumptions and level of fit via a graphical check with AMOS, in addition to check causal path analysis among the variables.
Results
Of this participants, 83 (74%) were parent, 94 (83%) spoke or communicated in Taiwanese, 73 (65%) maintained a nuclear family, 65 (58%) were female, 61 (54%) were in an adolescent family development stage, and 80 (71%) held direct power to propose an idea or plan. The majority of the participants (75%) reported having at least 12-year education background and a monthly income of over NT$ 30,000. Participants classified themselves as professionals (4.4%), technique (8.8%), government office workers (15%), trade workers/administrators (15%) or labor/housewives/none (57%), and married (69%).
Before testing the model, the authors analyzed the basic data first to answer question one. The analysis revealed no significant differences in demographic characteristics of parental age, case age, sibling age (t = 0.79 ~ 1.41, p = 0.16 ~ 0.51); or in gender, marital status, education, employment, monthly income, television-watching time, residence location, family structure, decision-making, and holding the power to propose an idea or plan between DMD and SMA groups (χ2 = 2.72 ~ 7.39, p = .12 ~ .44). Primarily, parents and those in adolescent family development stage maintained a higher significant difference in DMD than SMA group (χ2 = 10.71, 14.48; p = 0.00, 0.01). Additionally, Taiwanese speakers, those with a nuclear family, and problem-solving parents maintained a higher significant difference in SMA than DMD group (χ2 = 10.71 ~ 19.86, p = 0.00 ~ 0.03).
The researchers utilized chi-square tests to compare categorical variables (Table 1). The results indicated no significant differences in family nutrition assessment of the two disease groups, including BMI condition, health risk problem (body fat), body weight assessment, health risk (lumbar/waist ratio), and body structure (χ2 = .52 ~ 5.16, p = 0.08 ~ 0.67). The researchers utilized t tests to compare means of continuous variables, which similarly presented no differences in variables of height/wrist ratio, BMI, and body weight minus ideal body weight between two disease groups (t = − .89 ~ .64, p = .34 ~ .41) except lumbar/waist ratio (t = 2.25, p = .03).
The means and standard deviations for each of the study variables between DMD and SMA groups revealed no significant differences in the family health promotion assessment, consisting of the FHPL, Duke Health Profile, FHI, FAPGAR, and FAD-GF scale scores, including their subscales (t test = − 0.43 ~ 1.37, p = 0.17 ~ 0.75) between the DMD and SMA groups (Table 2). According to comparisons of the means on the five scales, including their subscales with means for participants’ classification (fathers, mothers, patients, siblings, and caregivers), no significant differences exist between DMD and SMA groups for all variables, as the p values of the f value test ranged between 0.17 ~ 0.8.
Second, correlation test for all variables in total sample among demographics, FHPL, Duke Health Profile, FHI, FAPGAR, and FAD-GF showed that social-demographic characteristics were associated with the score of the HPLP presenting a positive relationship with family monthly income (r = .20, p < .05), education (r = .26, p < .01), and power to propose an idea/plan (r = .26, p < .01). FAPGAR scores were positively correlated with geography in Taiwan and between gender (r = 0.21, p < 0.05), and power to propose an idea/plan (r = 0.47, p < 0.01). The level of Duke Health Profile was correlated with family monthly income (r = 0.22, p < 0.05), education (r = 0.23, p < 0.05), and watching TV time (r = 0.34, p < 0.01). The score of the FAD-GF expressed a positive relationship with family monthly income (r = 0.20, p < 0.05) and power to propose an idea/plan (r = 0.46, p < 0.01). The inconsistency in the results was related to the level of the FHI of family structure. For the other focus, family power structures, only family members could directly offer an idea/suggestion (power to propose an idea/plan, r = 0.19, p < 0.05) which associated with the five scales (r = 0.20 ~ 0.47, p < 0.05 ~ 0.01). In addition, participants’ nutritional assessments (assessment of family health needs), including body structure (height/wrist ratio), BMI, and body weight judgment (body weight-ideal body weight) maintain no association with level of five scales (r = 0.001 ~ 1.68, p = 0.17 ~ 0.99) except health risk (lumbar/waist ratio, r = − 0.24, p = 0.02) correlated with the HPLP score.
Third, the researchers utilized hierarchical linear regression to determine the relative contribution of general family function. In step 1, the researchers added 10 independent variables of participants’ characteristics were added. In step 2, the researchers added family hardiness and family support to step 1. In step 3, general health was added, and finally, in step 4, the researchers added family health behavior to step 3. The final regression statistic for the full model produced significant predictors of geography, monthly income, power to propose an idea/plan, family support, and family hardiness on general family function (F = 19.64, p = 0.00, R = 0.86, bête = 0.12, − 0.14, − 0.23, − 0.25, and − 0.54, respectively; t = 2.19, − 2.10, − 3.63, − 3.11, and − 7.94, respectively; p = 0.03, 0.04, 0.01, 0.01, and 0.01, respectively).
Following the previous analysis, the researchers found that the relative contribution of general family function aligned with hierarchical linear regression in terms of determining the relative contribution of family health behavior. The final regression statistic for the full model was a significant predictors of family hardiness and general health on family health behaviors (F = 6.59, p = 0.00, R = 0.70, bête = 0.31, and 0.26; t = 2.65 and 2.56; p = 0.01 and 0.01).
Subsequently, the researchers selected latent variables as independent variables that significantly affect each other and placed them into a model test to determine the level of fit of the hypothesis. Utilizing several models facilitated a comparison of the predictors of multiple variables on family health behavior and general family function. Figure 2 illustrates the degree of fit of the final full model, including all paths from family support through family hardiness that maintain direct or indirect effect on general family function and on general family health (chi-square = 57.19, df = 58, p = 0.51, NFI = 0.93, RFI = 0.90, CFI = 1.00, GFI = 1.0, RMSEA = 0.01). The probability rate of the ideal model of family health capacity influenced on family health status model is 96% (BCC p = .96), and the probability rate of the accurate model of family health capacity’s influence on the family health status model is 99% (BIC p = .99).
Predictors on FAD-General function from family characteristics by family hardiness, family support, and family support (χ2 = 57.19 df = 58, p = .51, NFI = .93, RFI = .90, CFI = 1.0, TLI = 1.0, GFI = 1.0, AGFI = .89, PGFI = .59, RMSEA = .01): standardized estimates, BCC 0 = 0, BIC 0 = 0, BCC L and BIC L = 1.0, BCC p = .99, BIC p = .96 C/df = .99
Figure 3 shows the goodness of fit of the final full model, including all paths from family support, family hardiness, general health that had direct or indirect effect of general family health, family health behavior, and general family function (χ2 = 228.3, df = 139, p = 0.00, NFI = 0.83, RFI = 0.79, CFI = 0.93, TLI = 0.91, GFI = 0.84, RMSEA = 0.075). Family hardiness was the mediator on general family function and of general health through family support, and of family health behavior through family support and general health in the model. The probability rate of the idea model of family health capacity’s influence on family health status and on family health behavior was 100% (BCC p = 1.0), and the probability rate of the accurate model of family health capacity’s influence on family health status and on family health behavior was 100% (BIC p = 1.0).
Predictors on family behavior from family characteristics by family hardiness, family support, general health, and family general function (χ2 = 228.3, df = 139, p = .00, NFI = .83, RFI = .79, CFI = .93, TLI = .91, GFI = .84, AGFI = .78, PGFI = .61, RMSEA = .075): standardized, estimates, BCC 0 = 0, BIC 0 = 0, BCC L and BIC L = 1.0, BCC p = .1.0, BIC p = 1.0 C/df = 1.64
Afterwards, the researchers selected demographic variables that significantly affected the five scales and placed them into model test to determine the degree of fit of hypothesis. Utilizing several models aided in comparing predictors of multiple variables on family health behavior and general family function. Figure 4 shows significant direct and indirect influence on family health behavior from family support through family hardiness and general family health; from geography through general health; from power to propose a plan/idea through general family health; from power to propose a plan/idea through family support, general family health, or through general family health and family hardiness that received the ideal fit model (chi-square = 17.66, df = 17, p = 0.41, NFI = 0.94, RFI = 0.90, CFI = 1.0, GFI = 0.96, RMSEA = 0.02). The strongest explained variables for general family function and general family health were family support and family hardiness, while the strongest explained variables for family health behavior were family hardiness and family support. The probability rate of the ideal model of family health promotion model was 74% (BCC p = .74), and the probability rate of the accurate model of family health promotion model was 91% (BIC p = .91) (Fig. 4).
Predictors on health promotion life style from family characteristics by family hardiness, family support, general health, and family function (chi-square = 17.66, df = 17, p = .41, NFI = .94, RFI = .90, CFI = 1.0, TLI = 1.0, GFI = .96, AGFI = .92, PGFI = .45, RMSEA = .02): standardized estimates, BCC p = .74, BIC p = .91
Discussion
Structured family health promotion model instruments have been developed to support differentiation of family capacity to promote family health status and family health behavior. Empirical and theoretical work suggests that five major scales in the present sample are validly assessed and maintain adequate reliability via self-report by participants. Internal consistency reliabilities and construct validity for these measures were good. Item total correlations were adequate to good. These scales were moderately correlated with one another. The psychometric properties of instruments that most definitely correlated with family general function, general health, and family health behavior were family support and family hardiness.
Findings suggested that no significant differences between DMD and SMA group in the five-scale scores of family health promotion assessment including their subscales and the same among participants’ classifications of fathers, mothers, cases, siblings, and caregivers. In addition, there were no significant differences in individual characteristics and family nutrition needs assessment variables, with the exception of health risk (lumbar/waist ratio) between DMD and SMA groups. However, in the study, the researchers only identified that health risk (waist/lumbar ratio) correlated with family health behavior score. Acheson et al. (2010) indicated that risk perceptions were correlated with family history of disease, and that individuals perceived that the ability to prevent chronic disease was not related to familiar risk. The researchers would like to prevent majority of chronic diseases through advocating action of family health promotion by perceiving controllable health risk (waist/lumbar ratio). In addition, the researchers aimed to allow family members to discuss family health behaviors directly with each other by providing health education to promote family health.
The study was important in that different associations focused on studying family health behavior through education, monthly family income, and power to propose an idea/plan factors. The last two factors are associated with family general function, a result supported by other researchers presenting economic conditions that significantly affected families’ adherence to diet (Aggarwal et al. 2010). One of the major gaps in the literature was association of family support, measured by the power to propose an idea/plan, geography, and gender. Given that, watching TV time and education influenced general health; and family structure affected family hardiness. Studies have presented equivocal findings in the association of demographics, including gender, marital status, educational level, monthly income, and residence location, regarding family health behavior (Hacer et al. 2012; Pirincci et al. 2008) that depended on culture and social economical level. Poverty has been found to be a common factor of greater emotional and behavioral behaviors in children of parents under financial stress (Grant et al. 2005; Mejia et al. 2012). Family economics reflected these familial relationships, which encouraged employing integrated approaches to the development and delivery of accessible health systems (Kaakinen et al. 2010; Martin et al. 2013).
Those distress with comorbid state within family of children with muscular dystrophy should be cared for by utilizing their social health, affective communication, partnership, commitment, life appreciation, and health responsibility to improve their general family function (see Fig. 2) and maintain family health behavior (see Fig. 3). Family support was the mediator on general health through family hardiness, and on family health behavior through general health and through family hardiness and general health in the model. The mediated effect of family hardiness on general family function, general health, and family health behavior through monthly income. The path model accounted for 78% of the variance in family support to general family health, 57% in family support and family hardiness to family health behavior, and 99% in family support and family hardiness to general family function.
An examination of the concepts and their relationship to the family health promotion model showed that these associations have been suggested as either causal or as part of shared model A. The mediator of family support on general family function directly or indirectly influenced general family function, as measured by the power to propose an idea/plan or family hardiness. The mediated factors of monthly income and power to propose an idea/plan effected on family support and family hardiness on general family function. In model B, the mediator of family hardiness was directly or indirectly influenced by general family function by monthly family income, family support, family support through family hardiness, and general health. In model C, the mediators of family hardiness and general family health were directly or indirectly influenced by family health behavior, as measures of family support. The mediated of monthly income and power to propose an idea/plan effected on family support and family hardiness on family health behavior. In addition, family support, family hardiness, and general health maintained their direct or indirect effect on family health behavior. The mediator of monthly family income and the power to propose an idea/plan effected on family health behavior, on general family function, and on general family health. The family health promotion model constructed accounted for 71% of the variance in general family function and 42% in family health behavior. Previous studies have not consistently proposed a shared mediator effect of family support and demographics effected on general family function and general family health (Chen et al. 2014a; Chen et al. 2015; Chen and Clark 2010).
The outcome evidences that the family health promotion model test contributed significantly to a more predicable causal description of strengths and weaknesses not identified in general family function, causing family health behavior to pass through demographics and family capacity, which then informed to explore and expand some control in their life activities. Several studies concerning intervention to enhance health promotion behavior on teenagers provided evidence of self-efficacy as the major predictor on physical activity (Srof and Velsor-Friedrich 2006). Families represented important sources of interpersonal influence that could increase or decrease commitment, challenge, or control of health promotion behavior.
This study maintains a cross-sectional design that precludes a conclusion related to causality. However, although the hypothesis model has tested direction of effects at good fit, an additional longitudinal study is needed to elucidate these effects. Although the uniqueness of the study sample was its strength, its uniqueness also limited generalizability of the results. The sample was not a random selection from a large population of those affected by muscular dystrophy and may only present families who were motivated and able to participate in the study.
References
Acheson, L. S., Wang, C., Zyzanski, S. J., Lynn, A., Ruffin, M. T., Gramling, R., et al. (2010). Family history and perceptions about risk and prevention for chronic diseases in primary care: a report from the family healthcare impact trial. Genetics in Medicine, 12(4), 212–218. https://doi.org/10.1097/GIM.0b013e3181d56ae6.
Aggarwal, B., Liao, M., Allegrante, J. P., & Mosca, L. (2010). Low social support level is associated with non-adherence to diet at 1 year in the Family Intervention Trial for Heart Health (FIT Heart). Journal of Nutrition Education and Behavior, 42(6), 380–388. https://doi.org/10.1016/j.jneb.2009.08.006.
Barnes, M., Courtney, M. D., Pratt, J., & Walsh, A. M. (2004). School-based youth health nurses: roles, responsibilities, challenges, and rewards. Public Health Nursing, 21(4), 316–318.
Biggar, W. D. (2006). Duchenne muscular dystrophy. Pediatrics in Review, 27(3), 83–88.
Billard, C., Gillet, P., Signoret, J. L., Uicaut, E., Bertrand, P., Fardeau, M., et al. (1992). Cognitive functions in Duchenne muscular dystrophy: a reappraisal and comparison with spinal muscular atrophy. Neuromuscular Disorders, 2(5–6), 371–378. https://doi.org/10.1016/S0960-8966(06)80008-8.
Brolin, C., & Shiraishi, T. (2011). Antisense mediated exon skipping therapy for Duchenne muscular dystrophy (DMD). Artifcial DNA PNA XNA, 2(1), 6–15. https://doi.org/10.4161/adna.2.1.15425.
Chan, C. W., & Perry, L. (2012). Lifestyle health promotion interventions for the nursing workforce: a systematic review. Journal of Clinical Nursing, 21(15–16), 2247–2261. https://doi.org/10.1111/j.1365-2702.2012.04213.x.
Chen, J. Y. (2008). Mediators affecting family functioning in families of children with Duchenne muscular dystrophy. Kaohsiung Journal of Medical Sciences, 24(10), 514–522.
Chen, J. Y., & Clark, M. J. (2007). Family function in families of children with Duchenne muscular dystrophy. Family and Community Health, 30(4), 296–304. https://doi.org/10.1097/01.FCH.0000290542.10458.f8.
Chen, J. Y., & Clark, M. J. (2010). Family resources and parental health in families of children with Duchenne muscular dystrophy. Journal of Nursing Research, 18(4), 239–248. https://doi.org/10.1097/JNR.0b013e3181fbe37b.
Chen, J. Y., & Jong, Y. J. (2006). A stress model for parents of children with Duchenne muscular dystrophy. The Journal of Nursing (Chinese), 53(3), 44–51.
Chen, M. Y., Wang, E. K., & Chang, C. J. (2006). Cross-validation and discriminant validity of adolescent health promotion scale among overweight and nonoverweight adolescents in Taiwan. Public Health Nursing, 23(6), 555–560. https://doi.org/10.1111/j.1525-1446.2006.00596.x.
Chen, J.Y., Chen, S.S., Jong, Y.J., Yang, Y.H., & Lue, Y.J. (2013a). Psychosocial stress and coping strategies of parents with Duchenne muscular dystrophy children during the middle stage. In C. Angelini (Ed.), Muscular dystrophy: causes and management (pp. 339–356). New York Nova.
Chen, Y. H., Lin, Y. H., Hung, C. S., Huang, C. C., Yeih, D. F., Chuang, P. Y., et al. (2013b). Clinical outcome and cost-effectiveness of a synchronous telehealth service for seniors and nonseniors with cardiovascular diseases: quasi-experimental study. Journal of Medical Internet Research, 15(4), e87. https://doi.org/10.2196/jmir.2091.
Chen, J. Y., Yen, M. H., Chen, H. S., Liu, Y. Y., Hu, S. H., Liu, M. C., et al. (2013c). Health support: health promotion for family having a child with DMD. In C. Angelini (Ed.), Muscular dystrophy: causes and management (pp. 319–337). New York: Nova.
Chen, J.Y., Chao, M.C., Yang, S.Y., Xiao, Y.H., & Lin, Y.H. (2014a). Family resources and family health perspectives of children with turner syndrome and their parents 8th ICN INP/APNN Conference: advanced nursing practice: expending access and improving healthcare outcome. Helsinki, Finland.
Chen, J. Y., Clark, M. J., Chang, Y. Y., Liu, Y. Y., & Chang, C. Y. (2014b). Factors affecting perceptions of family function in caregivers of children with attention deficit hyperactivity disorders. The Journal of Nursing Research, 22(3), 165–175. https://doi.org/10.1097/jnr.0000000000000042.
Chen, J. Y., Chen, H. S., Liu, M. C., & Chao, M. C. (2015). Relationship between families perception of health and support in the care of vulnerable children. Clinics Mother Child Health, 12(3), 1–9. https://doi.org/10.4172/2090-7214.1000189.
Chen, J. Y., Yen, M. H., Lin, Y. H., Hu, S. H., Chen, H. S., Liu, M. C., et al. (2017). Preliminary process of developing multiple programs for promoting family health with a vulnerable child. Acta Psychopathologica, 3(1:3), 1–7. https://doi.org/10.4172/2469-6676.100075.
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9, 171–180.
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
Faul, F., Erdfelder, E., Buchner, A., & Lang, A. G. (2009). Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160.
Ford-Gilboe, M. (1997). Family strengths, motivation, and resources as predictors of health promotion behavior in single-parent and two-parent families. Research in Nursing and Health, 20, 205–217.
Ford-Gilboe, M. (2002). Developing knowledge about family health promotion by testing the developmental model of health and nursing. Journal of Family Nursing Research, 8(2), 140–156.
Grant, K., McCormick, A., Poindexter, L., Simpkins, T., Janda, C., Thomas, K., et al. (2005). Exposure to violence and parenting as mediators between poverty and psychological symptoms in urban African American adolescents. Journal of Adolescence, 28(4), 507–521.
Hacer, S., Fevziye, C., & Melis, N. (2012). Healthy lifestyle promoting behavior in Turkish women aged 18-64. Asian Pacific Journal Cancer Preview, 13, 1241–1245. https://doi.org/10.7314/APJCP.2012.13.4.1241.
Kaakinen, J.R., Gedaly-Duff, V., Coehlo, D.P., & Hanson, S.M.H. (2010). Family health care nursing: theory, practice and research (4th ed.). Philadelpia: F. A. Davis.
Kliegman, R.M., Behrman, R.E., Jenson, H.B., & Stanton, B.F. (2007). Muscular dystrophies. In R.M. Kliegman, R.E. Behrman, H.B. Jenson & B.F. Stanton (Eds.), Nelson textbook of pediatrics (pp. 608). Philadelphia: Saunders Elsevier.
Kostova, F. V., Williams, V. C., Heemskerk, J., Iannaccone, S., DiDonato, C., Swoboda, K., et al. (2007). Spinal muscular atrophy: classification, diagnosis, management, pathogenesis, and future research directions. Journal of Child Neurology., 22(8), 926–945. https://doi.org/10.1177/0883073807305662.
Kuo, S. C. (1994). Change in family functioning during perinatal period in high-risk pregnancy with preterm labor pattern [Chinese]. Nursing Research (China), 2(2), 106–115.
Loveland-Cherry, C.J., & Bomar, P.J. (2004). Family health promotion and health protection. In P.J. Bomar (Ed.), Promoting health in families (3rd ed.). Philadephia: Saunders.
Martin, P., Duffy, T., Johnston, B., Banks, P., Harkess-Murphy, E., & Martin, C. R. (2013). Family health nursing: a response to the global health challenges. Journal of Family Nursing, 19(1), 99–118. https://doi.org/10.1177/1074840712471810.
McCubbin, H. I., Thompson, A. I., & McCubbin, M. A. (2001). Family measures: stress, coping, and resiliency—inventories for research and practice. Honolulu: Kamehameha Schools.
Mejia, A., Calam, R., & Sanders, M. R. (2012). A review of parenting programs in developing countries: opportunities and challenges for preventing emotional and behavioral difficulties in children. Clinical Child Family Psychological Review, 15, 163–175. https://doi.org/10.1007/s10567-012-0116-9.
Parkerson, G. R. J. (2002). User’s guide for Duke Health Measures. Durham: Department of community and family Medicine, Duke University Medical Center.
Parkerson, G. R. J., Broadhead, W. E., & Tse, C. K. (1990). The Duke health profile: a 17-item measure of health and dysfunction. Medical Care, 28, 1056–1072.
Pirincci, E., Rahman, S., Durmus, A. B., & Erdem, R. (2008). Factors affecting health-promoting behaviors in academic staff. Public Health Nursing, 122, 1261–1263. https://doi.org/10.1016/j.puhe.2008.04.006.
Smilkstein, G. (1978). The Family APGAR: a proposal for a family function test and its use by physicians. Journal of Family Practice, 6(6), 1231–1239.
Smilkstein, G., Ashworth, C., & Montano, D. (1982). Validity and reliability of the Family APGAR as a test of family function. Journal of Family Practice, 15, 303–311.
Soubhi, H., Potvin, L., & Paradis, G. (2004). Family process and parent's leisure time physical activity. American Journal of Health Behavior, 28(3), 218–230.
Srof, B. J., & Velsor-Friedrich, B. (2006). Health promotion in adolescents: a review of Pender’s health promotion model. Nurisng Science Quarterly, 19(4), 366–373. https://doi.org/10.1177/0894318406292831.
Wang, C. H., Finkel, R. S., Bertini, E. S., Schroth, M., Simonds, A., Wong, B., et al. (2007). Consensus statement for standard of care in spinal muscular atrophy. Journal of Child Neurology, 22(8), 1027–1049. https://doi.org/10.1177/0883073807305788.
WHO Regional Office for Europe. (1999). HEALTH 21: the health for all policy framework for the WHO European Region. Copenhagen, Denmark: World Health Organization.
Acknowledgements
We would like to thank the families of the children with DMD and SMA for their contribution to the completion of this research. MCL was supported by a holistic care award from Kaohsiung Medical University Hospital, and JYC was supported by Kaohsiung Medical University grant utilizing aggregate data from a three-different-type-disease-study.
Funding
The work was funded by grant KMUH- N10004 and KMU-M104024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
MCL was supported by a holistic care award from Kaohsiung Medical University Hospital and JYC was supported by Kaohsiung Medical University grant utilizing aggregate data from a three-different-type-disease-study. JYC has received a speaker’s honorarium from Kaohsiung Medical University. The authors declare no competing interest.
Ethical Approval
Details regarding the information brochure and informed consent were approved by the KMUH IRB board (KMUH-IRB-20110397). All subjects gave informed consent and patient anonymity should be preserved.
Rights and permissions
About this article
Cite this article
Chen, JY., Yen, MH., Lin, YH. et al. Testing the Family Health Promotion Model for Family Having Children with Duchenne Muscular Dystrophy/Spinal Muscular Atrophy. Adv Neurodev Disord 2, 391–401 (2018). https://doi.org/10.1007/s41252-018-0067-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-018-0067-3