Abstract
While malnutrition remains an important public health concern in poor countries, particularly among the rural and urban poor, overweight and obesity are emerging as important public health concerns for urban individuals. Globalization of the fast food industry and shifts in physical activity patterns in urban areas can result in different risks for overweight and obesity by socioeconomic status and sex for urban and rural residents. We examined Indian National Family Health Survey data, focusing on the association between urban residence and gains in body mass index among women (ages 15–49) in two survey rounds. We constructed multivariate models to assess the individual-level variation in BMI and the likelihood of becoming overweight or obese, finding that urban living is strongly associated with gains in BMI among women in India. Large cities have the highest proportions of overweight and obese women while spatial regression results suggest spatial clustering of higher BMIs in urbanized areas districts. Urban clustering of overweight and obesity may predict the future burden of chronic diseases for India but will benefit from further evaluation based on finer resolution data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Malnutrition remains a significant public health problem in many lower income countries but increasing rates of overweight and obesity are emerging priorities, especially among wealthier, urban groups (Jones-Smith et al. 2012; Swinburn et al. 2011; WHO 2006). The World Health Organization (WHO) defines overweight among as having a body mass index (BMI) of 25 kg/m2 or higher and obesity as having a BMI of 30 kg/m2 or higher (WHO 2014). Obesity is associated with higher mortality from chronic conditions such as diabetes, hypertension, cancer, and cardiovascular disease (Bhaskaran et al. 2014; Campbell 2014; Subramanian et al. 2011). Economic growth and urbanization can lead to dietary and lifestyle changes that result in a “double burden” of health risk: undernutrition among the rural and urban poor and unhealthy weight gain among the rural and urban rich (Rundle et al. 2007; WHO 2006). By 2030, the combined influence of the wider availability of fast food products, higher caloric intake from refined and processed foods, and sedentary work and life conditions associated with urban living, could contribute to a 75 % increase in the worldwide prevalence of overweight and obesity among adults ages 20 years and older (Kelly and Melnyk 2008). Past studies of overweight and obesity in developing countries have shown a strong positive association between socioeconomic status (SES) and BMI (Subramanian et al. 2011). However, changes in the urban built environment, such as sprawl and suburbanization, increase reliance on vehicular transport in lieu of walking or biking and can increase risk of being overweight or obese (Frumkin 2002; Rundle et al. 2007).
While India has much lower levels of chronic conditions, in large part due to the lower levels of obesity, an increase in overweight or obesity in urban areas will exacerbate chronic conditions that are on the rise from population aging alone (Danaei et al. 2011). This study assesses the association between urban residence and BMI among women in India. We used the Indian National Family and Health Survey (NFHS) data for 1998–1999 (NFHS-2) and 2005–2006 (NFHS-3) to determine whether urban women ages 15–49 had a higher likelihood of becoming overweight or obese than rural women. Further, we tested for spatial dependence, both the autocorrelation of error terms and spatial lag, to determine whether urbanization and proportions of overweight or obese women were spatially patterned. Men were excluded from the bulk of the analysis as there were no BMI data collected on men in the earlier survey round. Men’s BMI data from NFHS-3 (ages 15–49 years) were included for bivariate analysis.
1.1 Urbanization and Weight Gain Worldwide
Urbanization and economic growth have been linked to a global increase in the prevalence of overweight and obesity among adults and children in all regions of the world (Ivanova et al. 2008; Mathe and Brodie 2010; McLaren 2007; Olatunbosun et al. 2011). In lower income countries, increases in rates of overweight or obesity are first seen among wealthier, urban groups although over time poorer, less educated groups exhibit similar increases, indicating a potential spread from rich to poor enclaves or from urban to rural areas (Jones-Smith et al. 2012). Food and built environments in cities can interact to produce ‘obesogenic’ environments that can spatially pattern higher prevalences of overweight and obesity (Hill and Peters 1998). In major cities across Ghana, Zimbabwe, Bulgaria, and Nigeria, urban residents have been shown to be more vulnerable to unhealthy weight gain, in part due to macro-level economic trends that promote consumption of energy-dense processed foods and sedentary working conditions (Agyei-Mensah and Aikins 2010; Ivanova et al. 2008; Mathe and Brodie 2010; Olatunbosun et al. 2011).
Urban form matters: sprawl results in low residential and employment density as well as poor connectivity across cities, with increased automobile use (Frumkin 2002). In New York City, BMI was found to be negatively associated with features that are indicative of greater walkability such as higher density of public transit stops and land use mix of residential and commercial properties (Rundle et al. 2007). Similarly, greater access to local supermarkets versus neighborhood convenience stores was associated with lower BMI in American urban adolescents, especially among those with higher SES (Powell et al. 2007). In one study in urban Brazil, slum residents had higher rates of physical activity than non-slum dwellers, but also higher intakes of low-cost, high saturated fat foods (Alves et al. 2011). Combined with food consumption patterns, slum dwellers could be vulnerable to unhealthy weight gain as they age.
1.2 Urbanization and Weight Gain in India
India experienced significant economic growth starting in the early 1990s, which led to widespread changes in the urban environment as well as continued urban growth and emergence of new metropolitan areas. Since 1990, the country’s urban population has increased from 26 % to 31 % and the pace of annual urban growth far surpasses annual rural growth (World Bank 2012). By 2025, over 37 % of the Indian population will be urban (UN DESA 2013). While these urban fractions are seemingly low, India already has more large cities than any other country except China: in 2010, India had 43 cities of more than 1 million persons, three of which had close to 15 million or more persons (UN DESA 2012). Most future economic growth for the country is projected to result from moving the labor force from farming to non-farming activities (Sanyal et al. 2009). However, the population and economic growth has come at the cost of increasing income inequality; urban sprawl resulting in long work commutes, lack of quality outdoor spaces, poor safety for pedestrians and cyclists; growth of large informal settlements and slums; and greater consumption of sugars and fat (Azam 2012; Nilekani 2008; Vepa 2004).
Rising trends in overweight and obesity have also been observed in the recent past, mostly in urban areas and among adults. The prevalence of overweight and obesity has been documented to be 28 % in urban Delhi, and was higher among females than males (Gopinath et al. 1994). Higher income adults also had higher rates of overweight and obesity (32 % among males, 50 % among females) than the middle classes (16 % males, 30 % females), lower socio-economic groups (7 % males, 28 % females), followed by those living in urban slums (1 % males, 4 % females) (Gopalan 1998). Subramanian and colleagues found similar associations of pre-overweight, overweight, and obese categories with more than a twofold socioeconomic gradient across standard-of-living index quintiles for pre-overweight women and sevenfold gradient for obese women (Subramanian et al. 2007). At least one study from India also found four times higher rates of obesity among urban school children in private versus public schools, and significantly higher rates of overweight in metropolitan versus non-metropolitan areas (Misra et al. 2011). The lowest wealth and education groups in urban areas may also experience faster overweight prevalence growth rates (Jones-Smith et al. 2012). A study of rural to urban migrants in India found that urban male and female migrants reported an increase in fat intake and reduced physical activity compared to their rural siblings, corresponding to higher levels of obesity and diabetes (Ebrahim et al. 2010). Given the potential pathways between urban environments and obesity, we would need to determine whether overweight or obesity rates are spatially clustered among urban groups in India.
1.3 Spatial Patterns in Overweight and Obesity
It has been suggested that spatial clustering in non-communicable diseases (NCDs) such as diabetes and cardiovascular disease (CVD) may result from spatial clustering in risk factors such as overweight and obesity (Gallos et al. 2012). Excessive weight gain, for example, may be collectively determined by social behavior or global economic growth that impact food consumption and availability rather than by individual dietary choices (Swinburn et al. 2011). The level of physical activity may be similarly determined by environmental factors such as transportation and sedentary work environments (Hill and Peters 1998). However, without objective, geocoded measures of the urban environment, it is difficult to establish any spatial patterning of associations between the urban environment and risk of overweight or obesity. At best, data may be available by urban–rural dichotomy or for larger cities only, while fuller models allowing for multilevel analysis of risk factors with spatial correlations are still limited. This is especially true in poorer countries where geocoded surveys, particularly on urban areas, are limited.
Studies of spatial patterns of overweight and obesity have shown varying spatial patterns of area-level characteristics and BMI, with limited examination of urban factors. A study examining the association between moderate physical activity as an indirect measure of the built environment and BMI in eight neighborhoods in suburban Vancouver found no evidence of clustering of obesity with physical activity and only sporadic local clustering of obesity (Schuurman et al. 2009). The authors were also able to incorporate neighborhood level measures of residential density and median income from complementary surveys but these data are generally absent in poor countries. Others examined access to walking destinations and community design as measures of neighborhood built environment and standardized BMI z-scores among adolescents, finding no spatial association (Duncan et al. 2012).
Another study examined neighborhood composition and resource variables with smoothed BMI rates at the zip-code level in a US state (Drewnowski et al. 2007). The authors found that after adjusting for spatial dependence, median household income, and percent Hispanic, median house value was a significant predictor of obesity prevalence at the zip-code level. In Taiwan, researchers found evidence of broader obesogenic environments where risk factors that affected risk of obesity in one township likely also affected that risk in neighboring townships (Chen and Wen 2010a). Using a hierarchical spatial lag regression model, the authors found that after adjusting for individual-level SES, the risk of high BMI had shifted from well-to-do clusters in 2001 to the most deprived clusters in 2005. Multilevel analysis of the same data showed that individual characteristics of residents may interact with neighborhood conditions; women for example felt more insecure about neighborhood safety and had elevated risk for being obese (Chen and Wen 2010b).
The Indian NFHS data have been used to estimate prevalences of overweight and obesity among women by education and SES (Subramanian et al. 2007). However, the association between urban residence and overweight and obesity over the reproductive life span of women in India is not known. Further, spatial patterns of overweight and obesity by urban residence have not been examined. We explore the role of urban residence in BMI gains and the spatial patterns of overweight and obesity among women across urban and rural areas in India. In the sections that follow, we first describe our methods, including the data and sampling frame and a description of BMI outcomes among Indian women. We then present the results of our bivariate and multivariate analyses of urban residence on BMI gains.
2 Methods
2.1 Data and Sample
The dataset included two repeated cross-sections of the Indian NFHS, a representative survey of women aged 15–49 years. NFHS-2 (1998–1999), covered all 26 states and interviewed 90,303 women while NFHS-3 (2005–2006) covered all 29 states (including three new states) and interviewed 124,385 women. In each state, the rural sample was selected in two stages involving the selection of primary sampling units (PSUs) or villages with probability proportional to population size (PPS) in the first stage and random selection of households within each selected PSU in the second stage. In urban areas, the sample was selected in three stages: the first stage was PPS selection of wards arranged by geographic region and female literacy, followed by random selection of one census enumeration block (CEB) from each selected ward, and the random selection of households from each CEB. In NFHS-3, CEB-wise data were also acquired for eight selected cities of which four were India’s well-known mega-cities and four were emerging urban areas. This round also oversampled urban households in states with very small urban populations as well as slum and non-slum households in the eight selected cities to yield a sample large enough to calculate stable estimates (International Institute for Population Sciences (IIPS) and Macro International 2007).
District code names for NFHS-2 districts were supplied by the data provider, ICF International. District names were used to identify the eight cities in NFHS-2 that are sampled in NFHS-3. We assumed that NFHS-2 districts with the same name as the eight NFHS-3 cities were fully urban. District names were also used to map the distribution of overweight and obesity across the NFHS-2 sample and to test for spatial autocorrelation at the district level. We restricted our sample to women who were not pregnant and who were not missing data for the outcome. As opposed to prior studies, we did not exclude women who were smoking or breastfeeding as we wanted to adjust for these variables during analysis. This yielded a final sample of 77,613 women in NFHS-2 and 113,075 women in NFHS-3. NFHS-3 also sampled slum dwellers in the eight selected cities. Households meeting the interviewer/team-designated or census-based slum definition criteria were included (and classified as such, where appropriate). There were 10,982 slum dwelling and 8,741 non-slum dwelling women in the selected cities sample. NFHS-3 BMI data on 69,834 men ages 15–49 were included in the bivariate analysis for comparison only.
2.2 Dependent Variable
Our outcome of interest was BMI, calculated as weight in kilograms divided by height in meters squared (kg/m2). Both weight and height were measured by the interviewer. The following cut-offs were used for bivariate analysis with BMI as a categorical outcome: <16 (severely thin), 16–18.49 (moderately to mildly thin), 18.5–22.9 (normal), 23–24.9 (Indian overweight), 25–29.9 (global overweight), and ≥30 (obese). A BMI cutoff of 23 kg/m2 was used for Indian overweight based on recommendations to use lower cut-offs for Asian Indians who might be at higher risk of type 2 diabetes and cardiovascular disease at lower BMIs than the existing WHO cut-off point of 25 kg/m2 for overweight (WHO Expert Consultation 2004). BMI was used as a continuous variable for the ordinary least squares (OLS) and spatial regression models and as a three-category variable (underweight: <18.5, normal: 18.5–22.9, or overweight/obese: ≥23) for multinomial logistic regression.
2.3 Independent Variables
Independent variables for both surveys were measured similarly, except for wealth score which was available for NFHS-3 only (International Institute for Population Sciences (IIPS) and Macro International 2007; International Institute for Population Sciences (IIPS) and ORC Macro 2000). The independent variable definitions were:
-
Age: Age of the woman at the time of the interview was recorded by the interviewer. Age was used as a categorical variable (5-years groups) for bivariate analysis and as a continuous variable for linear and logistic regression.
-
Education: Education was measured as highest education level completed (categorical) and education in single years (continuous). Education level was used for bivariate analysis and education in years for linear and logistic regression.
-
Urban: Residence in urban areas (yes/no) was based on the 1991 census definition (similar for both NFHS-2 and NFHS-3). Urban was defined as: (a) all statutory places with a municipality, corporation, cantonment board or notified town area committee etc. and (b) a place satisfying the following three criteria simultaneously: (1) a minimum population of 5000; (2) at least 75 % of male working population engaged in non-agricultural pursuits; and (3) a density of population of at least 400 per km2 (1000 per sq. mile) (International Institute for Population Sciences (IIPS) and ORC Macro 2000; National Sample Survey Organization and Government of India 2001).
-
Occupation: Women’s current occupation was recorded for currently working women and those who had worked in the 12 months prior to the survey. Variable categories were combined to produce three dichotomous variables: professional/clerical, laborer, or agricultural.
-
Smoking, Breastfeeding: Smoking and breastfeeding status were recorded as currently smoking/breastfeeding or not and used as dichotomous variables.
-
Parity: Parity was recorded as the number of live births before the current pregnancy (if pregnant at the time of the survey). It was used as a continuous variable for all analysis.
-
Standard of Living Index (SLI): In the absence of reliable income data, the standard of living index was created to measure household SES (Ayad et al. 1997). It was based on rankings of household access to basic amenities and ownership of selected consumer goods. Households were classified into five categories based on their scores. The variable was included to allow comparison of SES across the two survey rounds. Variable categories were combined to produce three dichotomous variables: low SLI, medium SLI, and high SLI.
-
Wealth: The DHS wealth index was introduced in 2004 as an improvement upon SLI and is included in NFHS-3 only. It is a composite measure of a household’s cumulative living standard based on ownership of selected assets, such as televisions and bicycles; materials used for housing construction; and types of water access and sanitation facilities (Rutstein and Johnson 2004). It is a continuous scale of relative wealth and was used as a continuous variable for NFHS-3 analysis.
3 Results
3.1 Sample Characteristics (Table 1)
Not surprisingly, urban women in both surveys were more likely to have completed higher education levels than rural women. Both rural and urban women were also better educated in the third than the second round; 49.6 % of urban and 31.9 % of rural women had completed secondary education in NFHS-3 compared to 34.7 % of urban and only 17.7 % of rural women in NFHS-2. The proportion of rural women with a secondary education doubled between the two surveys and a similar, though smaller, increase was seen among urban women as well. Age distributions across the two surveys were similar except for teenagers, who formed a higher proportion of the sample in the third round. A majority of the women were non-smokers with rural women having somewhat higher proportions of smoking. Urban women also had fewer children on average and were less likely to be breastfeeding at the time of the survey. Parity decreased for both urban and rural women from the second to the third round. As expected, a larger proportion of urban women in each round also had a higher standard of living than rural women.
3.2 Bivariate Analysis
We looked at the proportion of women in each BMI category by simple residence (i.e. urban vs. rural), size of the city (town, small city, large/capital city), and eight selected cities (Fig. 1). Rural women were much more likely to be severely or moderately thin than urban women in NFHS-2 (38 vs. 21 %) and NFHS-3 (36 vs. 23 %). In contrast, urban women were nearly three times more likely to be overweight at BMI ≥ 23 kg/m3 in NFHS-2 (25 vs. 12 %) and twice as likely in NFHS-3 (30 vs. 15 %) than rural women. Obesity was much higher among urban than rural women: 6 % versus 1 % in NFHS-2 and 6 % versus 2 % in NFHS-3. In selected cities, which include some of India’s largest, the proportions of obese women were even higher: 8 % in both rounds. However, these cities also had their share of severely and moderately thin women: 16 % in NFHS-2 and 21 % in NFHS-3. Comparing the two rounds, it was notable that there were higher proportions of malnourished women in urban areas and obese women in rural women in the more recent survey, although the increases were small. Proportions of overweight women increased in both urban and rural areas.
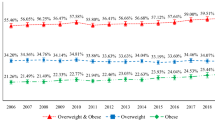
There is an unambiguous urban gradient in the share of overweight and obese women by city size. Figure 2 shows that the largest proportion of women in these categories are to be found in large cities, followed by small cities and towns, and finally rural areas. In NFHS-3, 32 % of the women in capital or large cities were overweight at BMI ≥ 23 kg/m3, compared to 30 % in small cities, 28 % in towns, and 15 % in rural areas. Obesity was prevalent in 8 % of women in large cities, followed by 6 % in small cities, 4 % in towns, and 2 % in rural areas. These comparisons were even starker if the Indian overweight benchmark was used instead of the global cut-off, 40 % of women in large cities were overweight or obese while more than a third of women in smaller cities and towns were also overweight or obese; the proportions of rural women in this category were about half as much. Data from NFHS-2 are not presented here due to the absence of city size definitions.
Women in slums were not as obese as women in non-slum urban areas but they did show some evidence of the ‘double burden’ of underweight and overweight (Fig. 3). In slums, 22 % of the women were severely or moderately thin while 32 % were overweight or 8 % obese. Among non-slum women, there were only slightly greater proportions of overweight (36 %) and obese (9 %) women but fewer thin women (18 %). In other words, and noteworthy, slum dwelling women were more likely than other urban women to be underweight (and presumably malnourished), but living in a slum did not prevent women from becoming overweight or obese.
The last bivariate description we consider before a multivariate analysis is age structure. Stratifying on place of residence for BMI outcome by age showed that BMI increased with age much more so in urban areas and especially in the four mega-cities of Chennai, Delhi, Kolkota, and Mumbai (Fig. 4). In each survey, younger, urban women had lower BMI than their rural counterparts but by age 20, urban women had much higher BMI gains than rural women. On average women living in the four mega-cities were overweight by age 30 while women in all urban areas reached overweight by age 38 in NFHS-2 and by age 35 in NFHS-3. At all post-adolescence ages and in all settings, mean BMI was higher in the more recent survey round. These two pieces of evidence suggest that this issue may be a fast evolving one for women in urban India.
Bivariate analysis comparing men and women suggested that increase in weight gain was much more pronounced among women than men (Fig. 5). Therefore, men were not included in the multivariate analysis.
3.3 Multivariate Analysis
To further explore our bivariate findings for BMI and place, we modeled several known confounders of weight gain among women, including: age, education, parity, breastfeeding, smoking, occupation, SLI, and wealth score. We estimated weighted, multivariate, linear regression models to assess the correlation between place of residence and BMI and whether the magnitude of this association changed after age as well as urban residence and wealth. We also estimated a multinomial logistic regression for Indian overweight or obese (BMI ≥ 23) and underweight (BMI < 18.5) outcomes compared to normal weight with regard to residence and urban–age interaction. All models accounted for clustering at the PSU level.Footnote 1
3.3.1 Ordinary Least Squares
In both surveys, predicted mean BMI was positively correlated with age, education, not smoking, and a high standard of living/wealth (Table 2). The interaction between wealth and urban residence was not statistically significant suggesting that while wealth increases BMI, its affect is equal in urban and rural areas (result not shown). The interaction between urban residence and age was positively associated with BMI, in fact urban residence doubled the effect of age on BMI. All else being equal, urban women added approximately 0.10 points to their BMI per year compared to rural women in each survey. This was in addition to a similar gain due to aging alone. In contrast, BMI was negatively associated with higher parity, breastfeeding, low standard of living, and working in agriculture or manual labor, conforming to a priori expectations. Having a high standard of living or greater wealth and urban-age interaction were highly, positively correlated with BMI. The magnitude of the urban interaction with wealth was quite small. Further, the relative importance of urban residence and age among urban women was clearly identified by the standardized regression coefficients (see Table 4 in “Appendix”).
3.3.2 Multinomial Logistic Regression
Multinomial predicted probabilities for BMI category support the interaction between age and urban residence for increased BMI (Fig. 6a, b). Women in urban areas had a higher probability of being overweight than underweight at age 26 in both survey rounds. In NFHS-3, women in rural areas also experienced this crossover but only at age 45. In urban areas, place clearly accelerated the association between aging and BMI by putting women at risk of being overweight at younger ages. Multinomial logistic regression results confirm the above finding; for every year of age, the odds of being overweight or obese were 1 % higher in urban than rural areas (Table 3), all else equal. Quantile regression, a method commonly used in studies of BMI was also implemented in order to segment those below and above normal weight and yielded similar results, showing a greater association between the urban–age interaction and wealth with increasing BMI percentiles (Table 5 in “Appendix”).
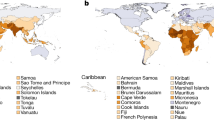
3.3.3 Exploratory Spatial Data Analysis (ESDA)
Since we do not have direct measures of district level characteristics in NFHS data, we use an ESDA approach to better capture the spatial regimes associated with urbanization. Urban areas, owing to their comparably small geographic land area, are hard to visualize on a map. However it is important to note that the proportions of overweight and obesity are spatially clustered among women. The maps in Fig. 7a, b show the proportion of women whose BMI is ≥23 kg/m2 and the proportion of the population that was urban in 2001, by district. While NFHS-2 data are not representative at the district level, the map illustrates clustering of districts with higher proportions of overweight or obese women (25 % or more), as well as clustering of more urban districts. Global Moran’s I for percent overweight or obese was 0.35 (p = 0.001 for 999 permutations), indicating a high degree of spatial autocorrelation of neighboring districts. Although we already have demonstrated a strong positive association between urban residence and individual-level BMI in the multivariable analysis above, a simple Pearson’s correlation coefficient between district-level percent OW/OB and percent urban supported our claim.
Simple Lagrange Multiplier tests for spatial errors and spatial lag using maximum likelihood estimations for percent overweight or obese by district further suggested significant spatial dependence of the dependent variable. In other words, overweight and obesity were spatially clustered. In the robust test, the lag term became less significant suggesting that when a lagged dependent variable was present, the error dependence became less significant. Both spatial error and spatial lag models improved upon the OLS model and controlling for spatial dependence improved model performance. It is plausible that while the errors were spatially correlated, the proportion of overweight or obese women in one district was influenced by values of independent variables in neighboring districts, owing to a shared built-environment overweight and obese women with a higher share of urban and high SLI households. These results were robust, even after correcting for spatial dependence, suggesting very strong urban spatial regimes. Spatial regression results are shown in Table 6 in “Appendix”.
4 Discussion
We looked at the association between urban residence and overweight or obesity for Indian women ages 15–49 years across two rounds of the Indian NFHS spanning 8 years. Urban residence was correlated with BMI across both surveys: women who lived in urban areas were more likely to be overweight or obese than women who lived in rural areas, holding equal individual level factors such as education, parity, age, and socioeconomic status. On a linear scale, urban residence doubled the association between aging and BMI, while rural residence had no additional impact on raising BMI beyond what was expected from aging alone, i.e. women become overweight in later reproductive years. In NFHS-3, women in urban areas also had a higher probability of being overweight than underweight nearly 20 years earlier than women in rural areas. This suggests that urban residence is an important modifier of the association between aging and BMI gain that is evolving over time.
Indian women’s increase in overweight and obesity has been associated with higher socioeconomic status at every age (Subramanian et al. 2009). According to the socioeconomic indicators available in the NFHS data, urban women were wealthier than rural women and controlling for place of residence may mask the association between age, place, and BMI. Our finding that living in urban areas led to more weight gain at much earlier ages than living in rural areas went beyond the expected association with education or socioeconomic status alone, both of which are higher in urban areas. Unmeasured factors regarding changes in lifestyle due to the changing urban environment may increase BMI among urban residents when compared to rural residents.
Further, it is notable that there were still considerable proportions of underweight women in urban areas in both surveys, with an increase between NFHS-2 and NFHS-3. This is alarming because it suggests that cities in India may experience a double burden of malnutrition (both under- and over-nutrition). Without a direct indication of diet or physical activity, it becomes more difficult to interpret the total effect of the urban environment, as income or socioeconomic status can be related to food consumption (both in quantity and quality) or it may reflect physical activity. We attempted to proxy this through occupation and found results in the expected direction—that more laborious work led to decreases in BMI at every age. However, given that a majority of the sample reported being a homemaker, it is not possible to generalize these findings. We assume that wealthier women are not physically active but there may be an income threshold beyond which women choose to and can afford to engage in regular exercise.
There could be additional neighborhood-level inequities if poor people live alongside the wealthier classes in mixed neighborhoods as has been suggested in other DHS survey reviews (Mark and Paul 2005). Richer women in mixed neighborhoods may be at risk from the availability of higher-fat, western style fast foods combined with a lack of outdoor space for exercise while poor women could be at greater risk of malnutrition from low wages and poor availability of healthy food. Neighborhood factors clearly go beyond socioeconomic status. Slums sampled in NFHS-3 had comparable proportions of overweight women to non-slum areas although they also had higher proportions of underweight women. Women in slums could be poor but still have urban exposures such as greater availability of high fat foods and reduced physical activity, same as their non-slum counterparts. Built-environment factors such as women's access to safe public spaces could further inhibit movement and physical activity (Phadke et al. 2011). Therefore, any study of nutrition in India has to consider inclusion of aggregate characteristics of city life, including an in-depth look at non-slum and slum-residence to determine if the increased likelihoods of overweight and obesity are driven by the same underlying mechanisms for all urban women.
The strengths of our study are that we look at large datasets across two national surveys with reliable measures of BMI that span a period of extensive economic growth and urban change in India. Therefore, we are able to capture an urban effect that had not yet extended into rural areas of the country at the time of the surveys. Our study identifies a strong association of BMI increase with a simple risk factor, age, among urban women. This finding could be useful to help focus public health policy in India. However, the persistent problem of undernutrition in urban areas needs to be addressed by municipal public health systems.
A limitation of this study is that we are not able to consider any specific urban factors that may affect BMI outcome due to de-identification of data beyond the urban–rural distinction. Although DHS datasets include a variable for city size, these general definitions are based on population size and do not convey information about the specific features of their urban environments, including those relating to food and built environments. A lack of comparable definitions of urban and rural as well as the differences in urban environment has been noted as a common limitation across similar studies (Allender et al. 2011). We also did not establish length of stay in the place of residence, which could be useful in establishing stronger associations between place and BMI. This information is available in the surveys and could be extracted for further analysis.
This study does not present information on the spatial aspect of urban growth and its potential impact on BMI outcome and is limited by holding the physical and social environment as a static condition. Specific urban and geographic factors were not available in the dataset or from other sources for either of the two datasets. However, we did find spatial clustering of overweight and obesity as has been suggested in other settings as well (Gallos et al. 2012; Michimi and Wimberly 2010). The spatial process of urbanization, especially outward spatial growth (or sprawl) of cities, could be an impediment to adequate coverage of urban public health services (Campbell and Campbell 2007). Finer resolution data would be necessary to further explore spatial patterns to identify potential environmental factors and to assess the effect of proximity to large metropolitan areas. We could not spatially distinguish between the urban and rural populations within districts. While a map at this scale is not a precise tool for policy, it allows for preliminary identification of regions with disproportionately high risk. Further research is warranted on the effect of economic, environmental, and social drivers of obesity that restrict healthy behavior among individuals (Sturm 2008). Datasets with geocoded urban locations and anthropometry measures would be much more ideal for identifying intra-urban differences in BMI by specific features of the local environment.
Research is also needed to determine the replicability of these results among men in the same setting (though with data sets that have more complete coverage of men), as well as across the urban–rural gradient in other developing countries to inform the implications for urban health planning. Research into the framing of obesity as a public health concern by municipal public health officials is also needed in light of the profusion of obesity-related myths and presumptions (Casazza et al. 2013). The policy environment can shape individual and environmental factors in shaping values and beliefs about obesity and deciding which prevention programs are implemented (Dean and Elliott 2012). This paper serves as a guide for better understanding community- and individual-level patterns of overweight and obesity and could be used in concert with multilevel modeling if direct measures of community exposures would become available.
References
Agyei-Mensah, S., & de-G Aikins, A. (2010). Epidemiological transition and the double burden of disease in Accra, Ghana. Journal of Urban Health, 87(5), 879–897. doi:10.1007/s11524-010-9492-y.
Allender, S., Wickramasinghe, K., Goldacre, M., Matthews, D., & Katulanda, P. (2011). Quantifying urbanization as a risk factor for noncommunicable disease. Journal of Urban Health, 88, 906–918. doi:10.1007/s11524-011-9586-1.
Alves, J. G. B., Figueiroa, J. N., & Alves, L. V. (2011). Prevalence and predictors of physical inactivity in a slum in Brazil. Journal of Urban Health, 88(1), 168–175. doi:10.1007/s11524-010-9531-8.
Anselin, L., Syabri, I., & Kho, Y. (2006). GeoDa: An introduction to spatial data analysis. Geographical Analysis, 38(1), 5–22.
Ayad, M., Barrere, B., & Otto, J. (1997). Demographic and socioeconomic characterisits of households. Calverton, MD: Macro International Inc.
Azam, M. (2012). Changes in wage structure in urban India, 1983–2004: A quantile regression decomposition. World Development, 40(6), 1135–1150. doi:10.1016/j.worlddev.2012.02.002.
Bhaskaran, K., Douglas, I., Forbes, H., dos-Santos-Silva, I., Leon, D. A., & Smeeth, L. (2014). Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5.24 million UK adults. The Lancet, 384(9945), 755–765. doi:10.1016/S0140-6736(14)60892-8.
Campbell, P. (2014). Obesity: A certain and avoidable cause of cancer. The Lancet, 384(9945), 727–728. doi:10.1016/S0140-6736(14)61172-7.
Campbell, T., & Campbell, A. (2007). Emerging disease burdens and the poor in cities of the developing world. Journal of Urban Health, 84(1), 54–64. doi:10.1007/s11524-007-9181-7.
Casazza, K., Fontaine, K. R., Astrup, A., Birch, L. L., Brown, A. W., Bohan Brown, M. M., et al. (2013). Myths, presumptions, and facts about obesity. New England Journal of Medicine, 368(5), 446–454. doi:10.1056/NEJMsa1208051.
Chen, D.-R., & Wen, T.-H. (2010a). Elucidating the changing socio-spatial dynamics of neighborhood effects on adult obesity risk in Taiwan from 2001 to 2005. Health and Place, 16(6), 1248–1258. doi:10.1016/j.healthplace.2010.08.013.
Chen, D.-R., & Wen, T.-H. (2010b). Socio-spatial patterns of neighborhood effects on adult obesity in Taiwan: A multi-level model. Social Science and Medicine, 70(6), 823–833. doi:10.1016/j.socscimed.2009.11.030.
Danaei, G., Finucane, M. M., Lu, Y., Singh, G. M., Cowan, M. J., Paciorek, C. J., et al. (2011). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. The Lancet, 378(9785), 31–40. doi:10.1016/S0140-6736(11)60679-X.
Dean, J. A., & Elliott, S. J. (2012). Prioritizing obesity in the city. Journal of Urban Health, 89(1), 196–213. doi:10.1007/s11524-011-9620-3.
Drewnowski, A., Rehm, C. D., & Solet, D. (2007). Disparities in obesity rates: Analysis by ZIP code area. Social Science and Medicine, 65(12), 2458–2463. doi:10.1016/j.socscimed.2007.07.001.
Duncan, D. T., Castro, M. C., Gortmaker, S. L., Aldstadt, J., Melly, S. J., & Bennett, G. G. (2012). Racial differences in the built environment—body mass index relationship? A geospatial analysis of adolescents in urban neighborhoods. International Journal of Health Geographics, 11(1), 11. doi:10.1186/1476-072X-11-11.
Ebrahim, S., Kinra, S., Bowen, L., Andersen, E., Ben-Shlomo, Y., Lyngdoh, T., et al. (2010). The effect of rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS Medicine, 7(4), e1000268. doi:10.1371/journal.pmed.1000268.
ESRI. (2012). ArcMap 10.1. Redlands, CA: Redlands.
Frumkin, H. (2002). Urban sprawl and public health. Public Health Reports, 117(3), 201–217.
Gallos, L. K., Barttfeld, P., Havlin, S., Sigman, M., & Makse, H. A. (2012). Collective behavior in the spatial spreading of obesity. Scientific Reports. doi:10.1038/srep00454.
Gopalan, C. (1998). Obesity in the Indian middle class. NFI Bulletin, 19(1), 1–4.
Gopinath, N., Chadha, S. L., Jain, P., Shekhawat, S., & Tandon, R. (1994). An epidemiological study of obesity in adults in the urban population of Delhi. The Journal of the Association of Physicians of India, 42(3), 212–215.
Hill, J. O., & Peters, J. C. (1998). Environmental contributions to the obesity epidemic. Science (New York, NY), 280(5368), 1371–1374.
International Institute for Population Sciences (IIPS), & Macro International. (2007). National Family Health Survey (NFHS-3), 2005–06: India. Mumbai: IIPS.
International Institute for Population Sciences (IIPS), & ORC Macro. (2000). National Family Health Survey (NFHS-2). Mumbai: IIPS.
Ivanova, L., Dimitrov, P., Dellava, J., & Hoffman, D. (2008). Prevalence of obesity and overweight among urban adults in Bulgaria. Public Health Nutrition, 11(12), 1407–1410. doi:10.1017/S1368980008002061.
Jones-Smith, J. C., Gordon-Larsen, P., Siddiqi, A., & Popkin, B. M. (2012). Is the burden of overweight shifting to the poor across the globe? Time trends among women in 39 low- and middle-income countries (1991–2008). International Journal of Obesity (2005), 36(8), 1114–1120. doi:10.1038/ijo.2011.179.
Kelly, S. A., & Melnyk, B. M. (2008). Systematic review of multicomponent interventions with overweight middle adolescents: Implications for clinical practice and research. Worldviews on Evidence-Based Nursing, 5(3), 113–135. doi:10.1111/j.1741-6787.2008.00131.x.
Mark, M., & Paul, C. H. (2005). Urban poverty and health in developing countries: Household and neighborhood effects. Demography, 42, 397–425.
Mathe, N., & Brodie, D. A. (2010). Overweight and obesity in urban and rural Zimbabweans. Proceedings of the Nutrition Society,. doi:10.1017/S0029665110003046.
McLaren, L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29(1), 29–48. doi:10.1093/epirev/mxm001.
Michimi, A., & Wimberly, M. C. (2010). Spatial patterns of obesity and associated risk factors in the conterminous US. American Journal of Preventive Medicine, 39(2), e1–e12. doi:10.1016/j.amepre.2010.04.008.
Misra, A., Shah, P., Goel, K., Hazra, D. K., Gupta, R., Seth, P., et al. (2011). The high burden of obesity and abdominal obesity in urban indian schoolchildren: A multicentric study of 38,296 children. Annals of Nutrition and Metabolism, 58(3), 203–211. doi:10.1159/000329431.
National Sample Survey Organization, & Government of India. (2001). Concepts and definitions used in NSS. India: New Delhi.
Nilekani, N. (2008). Imagining India: Ideas for the new century. India: Penguin.
Olatunbosun, S. T., Kaufman, J. S., & Bella, A. F. (2011). Prevalence of obesity and overweight in urban adult Nigerians. Obesity Reviews, 12(4), 233–241. doi:10.1111/j.1467-789X.2010.00801.x.
Phadke, S., Khan, S., & Ranade, S. (2011). Why loiter? women and risk on Mumbai streets. Gurgaon: Penguin.
Powell, L. M., Auld, M. C., Chaloupka, F. J., O’Malley, P. M., & Johnston, L. D. (2007). Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine, 33(4, Suppl), S301–S307. doi:10.1016/j.amepre.2007.07.007.
Rundle, A., Diez Roux, A. V., Freeman, L. M., Miller, D., Neckerman, K. M., & Weiss, C. C. (2007). The urban built environment and obesity in New York City: A multilevel analysis. American Journal of Health Promotion, 21(4s), 326–334. doi:10.4278/0890-1171-21.4s.326.
Rutstein, S., & Johnson, K. (2004). The DHS wealth index. Calverton, MD: ORC Macro.
Sanyal, S., Nagrath, S., & Singla, G. (2009). Urbanization and sustainability in India: An independent agenda. India: World Wildlife Fund.
Schuurman, N., Peters, P. A., & Oliver, L. N. (2009). Are obesity and physical activity clustered? A spatial analysis linked to residential density. Obesity (Silver Spring, MD), 17(12), 2202–2209. doi:10.1038/oby.2009.119.
StataCorp. (2013). Stata statistical software: Release 13. College Station, TX: StataCorp LP.
Sturm, R. (2008). Stemming the global obesity epidemic: What can we learn from data about social and economic trends? Public Health, 122(8), 739–746. doi:10.1016/j.puhe.2008.01.004.
Subramanian, S., Kawachi, I., & Smith, G. D. (2007). Income inequality and the double burden of under- and overnutrition in India. Journal of Epidemiology and Community Health, 61(9), 802–809. doi:10.1136/jech.2006.053801.
Subramanian, S., Perkins, J., & Khan, K. (2009). Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? American Journal of Clinical Nutrition, 90(2), 369–376. doi:10.3945/ajcn.2009.27487.
Subramanian, S., Perkins, J. M., Özaltin, E., & Smith, G. (2011). Weight of nations: A socioeconomic analysis of women in low- to middle-income countries. The American Journal of Clinical Nutrition, 93(2), 413–421. doi:10.3945/ajcn.110.004820.
Swinburn, B. A., Sacks, G., Hall, K. D., McPherson, K., Finegood, D. T., Moodie, M. L., & Gortmaker, S. L. (2011). The global obesity pandemic: Shaped by global drivers and local environments. The Lancet, 378(9793), 804–814. doi:10.1016/S0140-6736(11)60813-1.
UN DESA. (2012). File 12: Population of Urban Agglomerations with 750,000 Inhabitants or More in 2011, by Country, 1950–2025 (thousands). Retrieved October 30, 2013, from http://esa.un.org/unup/CD-ROM/Urban-Agglomerations.htm.
UN DESA. (2013). India: Demographic profile (1950–2025). Retrieved June 4, 2013, from http://esa.un.org/unup/unup/p2k0data.asp.
Vepa, S. (2004). Impact of globalization on food consumption of urban India. Rome, Italy: FAO.
WHO. (2006). Double burden of malnutrition in developing countries. Rome, Italy: Food and Agricultural Association of the United Nations. Retrieved from ftp://ftp.fao.org/docrep/fao/009/a0442e/a0442e01.pdf.
WHO. (2014). Obesity. Retrieved August 28, 2014, from http://www.who.int/topics/obesity/en/.
WHO Expert Consultation. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet, 363(9403), 157–163. doi:10.1016/S0140-6736(03)15268-3.
World Bank. (2012). Urban Population (% total): India. Retrieved September 24, 2013, from http://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Dev, A., Balk, D. Women and Weight Gain in Urban India: Evidence from the National Family Health Surveys (1998–2006). Spat Demogr 3, 1–25 (2015). https://doi.org/10.1007/s40980-015-0001-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40980-015-0001-5