Abstract
Background
The present study examines impulsivity and posttraumatic stress disorder (PTSD) symptoms as factors that may help understand the relationship between adverse childhood experiences (ACEs) and adolescent binge drinking.
Methods
Data were drawn from a subset of adolescents (N = 285) ages 12–22 from the National Consortium on Alcohol & Neurodevelopment in Adolescence (NCANDA). Impulsivity and PTSD symptoms were each predicted to moderate the relationship between ACEs and binge drinking.
Results
The positive relationship between PTSD symptoms and binge drinking was stronger when impulsivity was included. The positive relationship between ACEs and binge drinking was also strengthened when accounting for PTSD symptoms.
Conclusion
Our results provide evidence that impulsivity and PTSD symptoms may increase the risk for binge drinking during adolescence, including following ACEs. Interventions targeting PTSD symptoms and impulsivity could be valuable tools in preventing adolescent binge drinking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adverse childhood experiences (ACEs) refer to traumatic or potentially traumatic events, ranging from childhood abuse and neglect to family dysfunction (i.e., domestic violence, parental risky substance use, severe parental mental illness) (Felitti et al., 1998). These experiences are prevalent, with about 46% of adolescents in the USA reporting at least one ACE (Bethell et al., 2017). While this statistic represents nearly half of all teens, it is still likely an undercount of the actual number of adolescents who have experienced ACEs (Centers for Disease Control and Prevention, 2015). For example, several factors have been identified that may contribute to the under-reporting of ACEs, including avoiding emotional pain associated with the event, feeling embarrassed or ashamed, and having a poorer ability to recall an adverse event (McKinney et al., 2009). ACEs are also associated with poorer behavioral, cognitive, social, and physiological outcomes (e.g., Andersen & Teicher, 2009; Bick & Nelson, 2016; Dube et al., 2003; Felitti et al., 1998; Glaser, 2000; Strine, 2012). Given the prevalence of ACEs and their potential for short- and long-term damaging consequences, identifying factors that may impact the relationship between ACEs and poorer outcomes is still needed. The present study focuses on factors that may impact the relations between ACEs and binge drinking in adolescents and young adults.
Several longitudinal studies examining ACEs and alcohol use in adults (e.g., Dube et al., 2002) and adolescents (e.g., Shin et al., 2009) have found that ACEs are linked to negative alcohol use behaviors. The Kaiser-Centers for Disease Control (CDC) ACEs study found that adults who retrospectively reported more ACEs had earlier initiation of alcohol use and higher rates of alcohol use disorder and binge drinking (Dube et al., 2002, 2005). In addition, among women, specific ACEs, such as child maltreatment, may lead to a shorter transition from the first use of alcohol to the meeting criteria for alcohol use disorder (i.e., a process sometimes referred to as telescoping; Oberleitner et al., 2015). These findings in adults were also supported by prospective research with adolescents in the National Longitudinal Study of Adolescent Health (AddHealth), which found an increased likelihood of binge drinking in adolescents following ACEs (Shin et al., 2009, 2013). While this research links ACEs to problematic adolescent and adult alcohol use, including binge drinking and alcohol use disorder, the factors that may interact with ACEs to lead to binge drinking during adolescence are still largely unknown.
Binge drinking is a prevalent form of high-risk alcohol use with a wide range of negative consequences, including drinking and driving, alcohol poisoning, sexual and physical assault, serious accidents or injuries, memory blackouts, and long-term alcohol addiction (Chung et al., 2018). In adults, binge drinking is typically defined as a blood-alcohol level of 0.08 or higher, which often corresponds to five or more alcoholic drinks in men and four or more alcoholic beverages for women within one occasion (NIAAA, 2004). The current study utilizes the 5/4 + guideline to measure binge drinking behaviors, and while it is commonly used, it is not without limitations. It can underestimate the prevalence of adolescent binge drinking behavior due to some adolescents’ smaller body sizes, making them likelier to reach the blood-alcohol level of 0.08 with fewer drinks than adults (Chung et al., 2018). In the present study, 85% of adolescents and young adults were at adult body size and advanced puberty status at the time of measurement, supporting the overall acceptability of the use of the 5/4 + guideline for binge drinking. Furthermore, measuring blood-alcohol levels when alcohol use behaviors occur is often not possible, making the 5/4 + guideline a practical, if imperfect, proxy to measure binge drinking.
Adolescence is a critical developmental period, leaving youth at a higher risk for additional long-term consequences of binge drinking. For example, Silveri (2012) found that adolescents that engage in binge drinking are at increased risk for long-term impairments in learning and memory. Adolescent binge drinking has also been associated with abnormal brain development, including smaller hippocampal and white matter volumes in the prefrontal cortex (Jacobus et al., 2013; Pfefferbaum et al., 2018; Squeglia & Gray, 2016). Furthermore, adolescents engaging in binge drinking are not only at an increased risk for alcohol use disorders in adulthood (Hingson et al., 2006), but binge drinking initiated during adolescence is also more likely to persist into adulthood (Degenhardt et al., 2013).
Binge drinking increases during adolescence, with an estimated 4.6% of 8th graders, 10.9% of 10th graders, and 17.2% of 12th graders reporting binge drinking (Johnston et al., 2016). Worse is that youth exposed to ACEs are at an even higher risk for binge drinking. This risk is even greater for specific ACEs. For example, adolescents in the AddHealth study who had endorsed experiencing ACEs also reported more binge drinking than those who did not endorse ACEs. The relations between ACEs and risk for binge drinking remained strong even when age, race, parental alcohol misuse, and parental supervision were controlled. Adolescents and young adults who report maltreatment-related ACEs had an increased likelihood of binge drinking patterns persisting into adulthood (Shin et al., 2013). In addition, rates of adolescent binge drinking were highest for child maltreatment relative to other ACEs, suggesting that it may carry a more substantial negative impact than other ACEs (e.g., parental divorce; Shin et al., 2009). Given the long-term impact of ACEs on binge drinking in adolescence and beyond, identifying factors that may exacerbate risk for binge drinking among youth with ACEs is needed.
In examining the nature of these relations, trauma-related sequelae may increase the risk of binge drinking. For example, hypothalamic pituitary adrenal (HPA) axis dysregulation in the body’s response to stress has been associated with a heightened risk for binge drinking (De Bellis, 2001, 2002). Moreover, posttraumatic stress disorder (PTSD) symptoms related to ACEs that can follow from HPA axis activity have also been found to increase risk for transitions to moderate/heavy drinking in adolescence (De Bellis et al., 2020). Last, neurocognitive capacities, such as impulsivity, which are also involved with the HPA axis, may predict an increased risk for binge drinking among ACE-exposed youth (Lejuez et al., 2010).
Chronic overactivation of the HPA axis in adolescence following ACEs can alter cognitive development and increase impulsivity (De Bellis, 2002). However, overactivation of the HPA axis following ACEs can also manifest as the experience of PTSD symptoms, which can have the long-term effect of increased arousal and impact adolescent cognitive development (De Bellis, 2001). Over time, PTSD symptoms may contribute to increased impulsivity during adolescence that could persist into adulthood (Twardosz & Lutzker, 2010). Related research found that PTSD symptoms predicted some dimensions of impulsivity more so than experiencing childhood trauma itself (Kim & Choi, 2020). However, this study was conducted with adults and PTSD symptoms only significantly predicted 3 out of the five dimensions of impulsivity (Kim & Choi, 2020). Therefore, in addition to examining impulsivity, PTSD symptoms will also be examined as a potential mechanism that links ACEs with binge drinking in adolescents and young adults.
PTSD symptoms among youth with ACEs may increase the risk for behaviors associated with impulsivity, including risky alcohol use (Brady et al., 2004; Jakupcak et al., 2010; Weiss et al., 2012). As previously noted, one reason youth with PTSD symptoms may be more vulnerable to engaging in risky behaviors, such as alcohol use, is the dysregulation of the HPA axis (De Bellis, 2002; Jacobsen et al., 2001; Southwick et al., 1999). Periods of impulsivity associated with PTSD-related overactivation of the HPA axis may have damaging effects (Bick & Nelson, 2016; De Bellis, 2002; Pynoos et al., 1999), including a heightened risk of problematic alcohol use (De Bellis, 2002; Twardosz & Lutzker, 2010). This prior research contributes to the present study’s hypothesis that PTSD symptoms following ACEs may exacerbate impulsivity, increasing the risk for binge drinking.
The present study operationalizes impulsivity as reacting to stimuli in a rapid, unplanned manner with limited regard for long-term consequences (Moeller et al., 2001). We adopt the biopsychosocial perspective that asserts impulsivity can arise individually or transactionally due to biological predisposition, environment (i.e., learning from peers/family, ACEs), and psychopathology (e.g., PTSD, ADHD; Moeller et al., 2001). While retrospective studies among adults have suggested that ACEs are associated with increased impulsivity (Haaris Sheikh et al., 2018; Shin et al., 2018), there are limited studies on these relations during adolescence (Danese & McEwen, 2012; Sinha, 2009).
Impulsivity may contribute to the initiation of alcohol use in adolescence (Haaris Sheikh et al., 2018; Shin et al., 2012, 2018) and increased binge drinking in adolescence and young adulthood (Clark et al., 2017; Shin et al., 2012; Tarter et al., 2003; Townshend et al., 2014). There is a significant and systematic relation between impulsivity, measured in the context of executive functioning, and binge drinking in pre-adolescent and adolescent youth (Clark et al., 2017). A similar pattern emerged in the study conducted by Townshend et al. (2014), which found that adults who engaged in more binge drinking showed more impulse control and decision-making impairments. Findings such as these highlight that impulsivity may play a role in adolescent binge drinking and could have implications for intervention and prevention efforts.
Thus, the current study aims to understand the role of impulsivity and PTSD symptoms in the relations between ACEs and binge drinking in adolescence and young adulthood. Data from the multisite National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA; Brown et al., 2015) were used to assess ACEs, impulsivity, PTSD symptoms, and binge drinking in adolescents and young adults (Brown et al., 2015). We examine the following three hypotheses from baseline to year four in the NCANDA sample.
First, we predict impulsivity in year three will moderate the relations between ACEs at baseline and binge drinking in year four; higher impulsivity will predict a stronger positive association between ACEs and binge drinking.
Second, we predict impulsivity in year three will moderate the relationship between PTSD symptoms in year two and binge drinking in year four; higher impulsivity will predict a stronger positive association between PTSD symptoms and binge drinking.
Third, we predict that PTSD symptoms in year two will moderate the relations between ACEs at baseline and binge drinking in year four; more PTSD symptoms will predict a stronger positive association between ACEs and binge drinking.
Methods
Participants and Procedures
Participants were 285 adolescents from the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) cohort (50% female; mean age = 16.1 ± 2.2 years, 12–22 years age range; (S. A. Brown et al., 2015). These data were taken from five sites, each of which had Institutional Review Board approval from their institution: Duke University, the University of Pittsburgh Medical Center (UPMC), Oregon Health & Science University (OHSU), the University of California San Diego (UCSD), and SRI International (SRI). NCANDA aims to disentangle relations between alcohol use and neurodevelopment prospectively during adolescence (Brown et al., 2015). NCANDA uses an accelerated longitudinal design, which gives a diverse age range, allowing for a more thorough examination of development across larger age ranges. To achieve the overall study aim (i.e., identifying the onset of alcohol use), NCANDA recruited participants aged 12–21 while oversampling participants between the ages of 12–15 to examine better this critical development period (Brown et al., 2015). All participants completed informed consent or assent with parent permission annually.
To study the initiation of alcohol use in the adolescent brain, most participants had to meet the criteria of no history of heavy drinking to be included in the study; however, 17% of the sample had prior alcohol use (Brown et al., 2015). Based on alcohol use history recorded at the baseline assessment, adolescents were divided into two groups: a no/low drinking group (n = 229; mean age 15.46 ± 2.3 years) and an exceeds-threshold group (n = 56; mean age 18.50 ± 1.9 years) (Pfefferbaum et al., 2016). The exceeds-threshold group was recruited to ensure a range of drinking behaviors and comprises a significantly older cohort. Previous studies have demonstrated the contrast in neurodevelopmental trajectories between the no/low drinking and exceeds-threshold groups, highlighting the importance of analyzing data from these two groups separately.
Childhood ACEs were assessed at baseline using the Childhood Trauma Questionnaire (CTQ; Bernstein et al., 2003). The CTQ is a standardized self-report inventory that consists of categories of trauma, such as physical and emotional abuse, emotional neglect, sexual abuse, and physical neglect. Each category contains five items rated on a 5-point Likert scale ranging from never true (= 1) to very often true (= 5), which gives scores of 5 to 25 for each trauma category (e.g., physical abuse). The CTQ has demonstrated high reliability and convergent and discriminant validity (Cronbach’s alpha = 0.94) (Bernstein et al., 2003). The total score from the CTQ at baseline was used in the analysis.
PTSD symptoms were assessed in year two using the Computerized Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994a; Hesselbrock et al., 1999; Norman et al., 2007b). The SSAGA is a standardized psychiatric interview for alcohol and drug abuse/dependence and other psychiatric disorders using DSM criteria. Bucholz et al. (1994b) found that the SSAGA has high reliability and validity (Cronbach’s alpha = 0.47–0.85). Participants were asked questions specific to DSM-IV diagnostic criteria for PTSD at baseline before the DSM-5 release (Norman et al., 2007a). The sum of the total number of PTSD symptoms at year two was used in the analysis.
Impulsivity was measured at year three using a computerized version of the Stanger Delayed Discounting Task, which assesses preference for smaller immediate rewards versus larger delayed rewards (Stanger et al., 2012). In this task, youth were presented with a choice between a smaller, immediate monetary reward (at least 50% of the delayed reward) versus receiving a larger amount in the future. For example, for the $100 1-day delay, youth were given a choice between at least 50% of the $100 now or receiving the full $100 1 day later. The computerized delayed discounting task, published by Stanger et al. (2012), has been validated in adolescent samples. Furthermore, these tasks have shown discriminant validity across various substance use disorders. Individuals who use drugs are more likely to choose immediate rewards than non-users, indicating more impulsive choices (MacKillop et al., 2011). A higher discount value is related to an increased preference for short-term gains over larger long-term gains, indicating more impulsive choices or “impulsivity.” Data were analyzed following Sullivan et al. (2016), where the primary outcome variable, rate of discounting, is represented by k. The task was completed for two values ($100 and $1000) at varying delays (e.g., 1 day, 7 days, 1 month, or 6 months). The current study examines the delay rate across monetary conditions and time delays. The delay rate, the natural log of k (lnk), was calculated for each of the two values ($100 and $1000) and each of the four delays (1 day, 7 days, 1 month, and 6 months), yielding eight variables.
Binge drinking was assessed in year four using the Customary Drinking and Drug Use Record (CDDR; Brown et al., 2015). The CDDR gives participants current (past 3 months) and lifetime measures of the level of involvement, withdrawal symptoms, psychological/behavioral dependence, and negative consequences of alcohol and other drugs (Brown et al., 1998). Before administering the CDDR, participants are shown the volume of one standard drink of wine, liquor, light beer, and IPA/malt liquor. This demonstration allows participants to quantify the number of standard drinks consumed more accurately. To assess for binge drinking, we assess responses to the following question while viewing the standardized drink volumes, “During the past year, how many times have you consumed four or more (females) / 5 or more (males) drinks within an occasion?” The CDDR has been shown to have high reliability and convergent validity for research and clinical purposes (Brown et al., 1998), making it a valuable assessment for measuring adolescent binge drinking. This measure utilizes the 5/4 + guideline to measure binge drinking, given that 84% of adolescents and young adults in this study were at adult body size and advanced puberty status at the time of measurement as measured by the Pubertal Development Scale (PDS; Brown et al., 2015; Petersen et al., 1988). A count of the number of days spent binge drinking in the past year was used in the present analysis.
Statistical Analysis
The current study aimed to understand how impulsivity may impact the relations between ACEs and binge drinking (hypothesis 1) and PTSD symptoms and binge drinking (hypothesis 2). We also examined how PTSD symptoms may impact the relations between ACEs and binge drinking (hypothesis 3). To evaluate these three aims, we employed moderation analyses recommended when studying interaction effects (Baron & Kenny, 1986). To probe significant moderation, simple slopes analyses were conducted using Kristopher Preacher’s interaction utility (Preacher et al., 2006).
For hypothesis one (impulsivity in ACEs and binge drinking), negative binomial regressions were conducted separately for the no/low and the exceeds-threshold drinking group. The CTQ total score at baseline (ACEs) was the independent variable and the CDDR variable (binge drinking) at year four as the outcome, with the delayed discounting variable (impulsivity) at year three as the moderator (run for each value/delay). CDDR data were positively skewed, which was expected given the nature of these data (i.e., many adolescents do not binge drink; Chung et al., 2018). Negative binomial regressions were used for the analyses recommended for “overdispersed” data (i.e., when the outcome variable’s variance exceeds the mean; Long, 1997). This hypothesis was a priori and specific; however, to account for possible type I error with four negative binomial regression analyses for each delayed discounting value ($100 vs. $1000), a Bonferroni corrected alpha level of 0.0125 was employed (Armstrong, 2014).
For hypothesis two, negative binomial regression was conducted separately for the no/low and the exceeds-threshold drinking group with PTSD symptoms in year two as the independent variable, the CDDR variable in year four as the outcome, and the delayed discounting variable in year three as the moderator. A Bonferroni corrected alpha level of 0.0125 was also used for hypothesis two, which had four negative binomial regression analyses.
For hypothesis three, negative binomial regression was conducted separately for the no/low and the exceeds-threshold drinking group, with the CTQ total score at baseline as the independent variable, the CDDR variable at year four as the outcome, and PTSD symptoms at year two as the moderator. An alpha level of 0.05 was employed as there was only one negative binomial regression.
Results
The descriptive statistics for age, sex, race, and ethnicity are presented in Table 1 for the no/low drinking and exceeds-threshold drinking groups, which were set at baseline. The means and standard deviations of the independent and outcome variables for the no/low drinking and exceeds-threshold drinking group are presented in Table 2. It is worthwhile noting that there was a significant difference in the mean number of days spent binge drinking between the no/low drinking and exceeds-threshold groups. Specifically, the exceeds-threshold group had higher average days spent binge drinking than individuals in the no/low drinking group.
-
Hypothesis 1: We predicted impulsivity would moderate the relationship between ACEs and binge drinking among adolescents in the no/low drinking and exceeds-threshold groups.
Results are summarized in Table 3. For both the exceeds-threshold and no/low drinking groups, the relationship between ACEs and adolescent binge drinking was not impacted by impulsivity. Therefore, the moderation was not probed (all p’s > 0.01).
-
Hypothesis 2: We predicted impulsivity would moderate the relationship between PTSD symptoms and binge drinking among adolescents in the no/low drinking and exceeds-threshold groups.
Results for hypothesis two are summarized in Table 3 and Table 4.
Exceeds-Threshold Group
The relationship between PTSD symptoms and adolescent binge drinking was not impacted by impulsivity. Therefore, the moderation was not probed (all p’s > 0.01).
No/Low Drinking Group
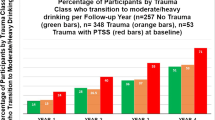
The relationship between PTSD symptoms and binge drinking increased as a function of impulsivity across five of the eight delayed discounting conditions (i.e., except for the $100 1-day and 6-month delays, and $1000 6-month delay). To probe moderation, simple slopes analyses were conducted for the significant five delayed discounting conditions (i.e., $100 7 days and 1 month; $1000 1-day, 7-day, and 1-month delay), and are presented in Fig. 1A–E and Table 4. Figure 1 depicts simple slope plots for binge drinking regressed onto PTSD symptoms at low (1 SD below the mean), moderate (at the mean), and high (1 SD above the mean) values of delayed discounting. High values (i.e., 1 SD above the mean) of delayed discounting suggest higher levels of impulsivity (i.e., preference for a smaller, immediate reward versus a larger, delayed reward). The following are the no/low group results in the five significant delayed discounting conditions.
-
$100 7-day delay: In the no/low drinking group, the simple slopes analyses revealed that PTSD symptoms were positively associated with binge drinking for low, moderate, and high levels of impulsivity (all p’s < 0.01). Results are presented in Fig. 1A.
-
$100 1-month delay: In the no/low drinking group, the simple slopes analyses revealed that PTSD symptoms were more positively associated with binge drinking for low and moderate levels of impulsivity (p < 0.01) than for higher levels (p > 0.01). Results are presented in Fig. 1B.
-
$1000 1-day delay: In the no/low drinking group, the simple slopes analyses revealed that PTSD symptoms were positively associated with binge drinking for low, moderate, and high levels of impulsivity (all p’s < 0.01). Results are presented in Fig. 1C.
-
$1000 7-day delay: In the no/low drinking group, the simple slopes analyses revealed that the relationship between PTSD symptoms, impulsivity, and binge drinking did not significantly differ based on level of impulsivity (all p’s > 0.01). Results are presented in Fig. 1D.
-
$1000 1-month delay: In the no/low drinking group, the simple slopes analyses revealed that PTSD symptoms were more positively associated with binge drinking for moderate and high levels of impulsivity (p < 0.01) than for low levels (p > 0.01). Results are presented in Fig. 1E.
-
Hypothesis 3: We predicted that PTSD symptoms would moderate the relationship between ACEs and binge drinking among adolescents in the no/low drinking and exceeds-threshold groups.
Days spent binge drinking in the past year regressed onto PTSD symptoms at low (1 SD below the mean in green), moderate (at the mean in red), and high (1 SD above the mean in black) values of delayed discounting (impulsivity) in the no/low drinking group. Panels A through E represent interactions that are referred to in the text and are the $100 7 days (A), 1 month (B), and $1000 1 day (C), 7 days (D), 1 month (E) delayed discounting conditions. The values on the X and Y axes are Z-scores
Exceeds-Threshold Group
The interaction between PTSD symptoms and ACEs did not significantly predict adolescent binge drinking. Therefore, the moderation was not probed (n = 56; β = − 0.024, p > 0.05, 95% CI [− 0.140, 0.092]).
No/Low Drinking Group
The interaction between the ACEs and PTSD symptoms was significant (n = 229; β = 0.051, p < 0.01, 95% CI [0.015, 0.088]). The simple slope analysis indicated that ACEs were more positively associated with binge drinking for low levels of PTSD symptoms (− 1 SD; b = 6.548, t = − 3.240, p < 0.01) than for moderate (mean; b = 3.842, t = − 2.288, p > 0.01) and higher levels (+ 1 SD; b = 1.136, t = 1.841, p > 0.01).
Discussion
The current study examined how impulsivity and PTSD symptoms may influence the relations between ACEs and binge drinking in the NCANDA sample. While links have been reported between ACEs and high-risk alcohol use (e.g., Dube et al., 2002; Felitti et al., 1998), much of this research has been retrospective (e.g., Felitti et al., 1998) or cross-sectional with adult participants (e.g., Fang & McNeil, 2017). The present prospective study found that for adolescents and young adults who were in the no/low drinking group (determined by baseline level of alcohol use), PTSD symptoms were related to higher rates of binge drinking. There was also some evidence that for youth in the no/low drinking group, impulsivity moderated the relationship between PTSD symptoms and binge drinking. These findings were not observed in the exceeds-threshold drinking group. Given that most of the sample was in the no/low drinking group, understanding the role of impulsivity for youth in this group could help with binge drinking prevention efforts. The implications of these results should also be understood in the context of the three study hypotheses.
We first tested the hypothesis that impulsivity strengthens the relationship between ACEs and binge drinking. The present study’s results did not find significant interactions between impulsivity as a moderator in the relationship between ACEs and adolescent binge drinking in either group (i.e., no/low and exceeds-threshold drinking groups). Adult studies examining ACEs, impulsivity, and binge drinking are mixed (Kirsch et al., 2020). Some report that impulsivity moderates the relationship between ACEs and binge drinking (Shin et al., 2015, 2018). Others have results similar to the present adolescent and young adult study (Skeer et al., 2009). Given the variation among current and prior research, how impulsivity is measured may be important to consider in future studies.
Different facets of impulsivity (i.e., premeditation, sensation seeking, negative urgency, and positive urgency) may contribute to varying results for impulsivity, ACEs, and binge drinking. For example, some studies have indicated that negative urgency (i.e., impulsive actions functioning to relieve negative emotions) may be a predictor of alcohol problems (Bø et al., 2016; Coskunpinar et al., 2013), especially among youth with ACEs (Shin et al., 2018; Wardell et al., 2016). It has also been posited that delayed discounting, as measured in the present study, may also be an indicator of negative urgency (Steward et al., 2017), while others suggest premeditation (Secades-Villa et al., 2016) or reward processing (Madden et al., 2010). Future studies may benefit from determining the facets of impulsivity involved in delayed discounting and examining these facets with binge drinking behavior.
In examining our second and third hypotheses, we found support for the role of impulsivity symptoms in understanding binge drinking in adolescents. In hypothesis two, we found that the relationship between PTSD symptoms and binge drinking differed according to impulsivity in three of the eight delayed discounting conditions (i.e., all except the $100 1-day and $1000 6-month conditions). These findings suggest impulsivity could be a worthwhile target in binge drinking prevention, particularly for teens with PTSD symptoms.
In hypothesis three, PTSD symptoms were examined as a moderator between ACEs and binge drinking. We found that PTSD symptoms significantly strengthened the relationship between ACEs and binge drinking for the no/low drinking group but not for the exceeds-threshold group. The simple slopes analyses for the no/low drinking group found that only the low levels of PTSD symptoms (i.e., not moderate or high) significantly strengthen the positive relationship between ACEs and binge drinking. While not statistically significant, the slopes for the moderate and high levels of PTSD symptoms were also in the positive direction. Given the overall pattern of results, moderate or high levels of PTSD may still play a role in the relations between ACEs and binge drinking that was not captured in the present analyses. At moderate to higher levels of PTSD symptoms, a complete PTSD diagnosis or other trauma-related disorder (e.g., mood or anxiety disorders) may be more strongly related to ACEs than binge drinking. Overall, the findings from hypotheses 2 and 3 align with research suggesting that PTSD symptoms are more likely to confer vulnerability to ACE-related consequences (i.e., SUDs, depression, anxiety, executive function deficits) than the ACEs themselves (e.g., Cole et al., 2019; De Bellis, 2001; De Bellis et al., 2020; Jaycox et al., 2004; Kirsch et al., 2020).
Moreover, the results presented here support prior findings regarding the relations between impulsivity and binge drinking. Previous research has noted that impulsivity alone is a salient risk factor for adolescent binge drinking (Lejuez et al., 2010; Shin et al., 2012; Townshend et al., 2014). Retrospective reports of higher impulsivity in childhood were associated with more co-occurring PTSD symptoms and binge drinking behaviors in adulthood (Walker et al., 2018). The present results add to prior research by presenting data collected over a four-year timespan. Youth in the no/low drinking group at baseline were more likely to transition to binge drinking at year 4 if they had experienced PTSD symptoms at year 2. Furthermore, our results suggested that PTSD symptoms increase the risk for later binge drinking even when the symptoms are not high.
While the study has many strengths, including a prospective adolescent and young adult sample, it also has limitations that should be discussed. One limitation is the relatively small sample in the exceeds-threshold drinking group. A major focus of NCANDA is examining the onset of alcohol use in adolescence. Most NCANDA participants had to meet the criteria of no to low drinking habits to be enrolled in the study. This design is a strength of NCANDA because it facilitates measuring the onset of drinking. However, having a comparatively small exceeds-threshold drinking group was a limitation for the comparisons in the present study. Previous studies have demonstrated the contrast in developmental trajectories between the no/low drinking and exceeds-threshold groups, highlighting the importance of analyzing data from these two groups separately. Specifically, previous studies have demonstrated that participants in the exceeds-threshold group had significantly smaller total, frontal, and temporal cortical volumes and thinner total, frontal, temporal, and cingulate cortices than those in the no/low drinking group (Pfefferbaum et al., 2016).
In addition, it is worth noting that the CTQ was only given to participants once (at baseline), and a new measure of ACEs was added in the second wave. This latter measure was not available for the present study. As a result, there is a possibility that participants under the age of 18 experienced additional ACEs that were unaccounted for in the present study. Last, participants in the exceeds-threshold drinking group were older than those in the no/low drinking group. While the analyses were conducted separately for the no/low and exceeds-threshold drinking groups, it would be helpful to continue to consider age further in future work.
Our results suggest that PTSD symptoms may impact binge drinking through neurocognitive pathways such as impulsivity measured via delayed discounting. More specifically, the risk exists across a spectrum. This risk includes youth with lower PTSD symptoms and impulsivity, who may still be at risk for increased binge drinking relative to youth with no PTSD symptoms and minimal impulsivity. Adolescence and young adulthood represent a critical period in development whereby the effects of binge drinking may have lifelong negative consequences, such as the development of alcohol use disorder. Understanding these relations can inform targeted binge drinking prevention and intervention strategies for adolescents and young adults, including the full spectrum of PTSD and impulsive symptoms.
Data Availability
The data that support the findings of this study are available from the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) and National Institute on Alcohol Abuse and Alcoholism (NIAAA). Restrictions apply to the availability of these data, which were used under a data distribution agreement for this study.
References
Andersen, S. L., & Teicher, M. H. (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience & Biobehavioral Reviews, 33(4), 516–524. https://doi.org/10.1016/j.neubiorev.2008.09.009
Armstrong, R. A. (2014). When to use the Bonferroni correction. Ophthalmic and Physiological Optics, 34(5), 502–508. https://doi.org/10.1111/opo.12131
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., Stokes, J., Handelsman, L., Medrano, M., Desmond, D., & Zule, W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. https://doi.org/10.1016/S0145-2134(02)00541-0
Bethell, C., Davis, M., Gombojav, N., Stumbo, S., & Powers, K. (2017). Issue Brief: Adverse childhood experiences among US children, child and adolescent health measurement initiative, Johns Hopkins Bloomberg School of Public Health, October 2017. http://www.cahmi.org/projects/adverse-childhood-experiences-aces/
Bick, J., & Nelson, C. A. (2016). Early adverse experiences and the developing brain. Neuropsychopharmacology, 41(1), 177–196. https://doi.org/10.1038/npp.2015.252
Bø, R., Billieux, J., & Landrø, N. I. (2016). Which facets of impulsivity predict binge drinking? Addictive Behaviors Reports, 3, 43–47. https://doi.org/10.1016/j.abrep.2016.03.001
Brady, K. T., Back, S. E., & Coffey, S. F. (2004). Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science, 13(5), 206–209. https://doi.org/10.1111/j.0963-7214.2004.00309.x
Brown, T. A., Chorpita, B. F., & Barlow, D. H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107(2), 179–192. https://doi.org/10.1037/0021-843X.107.2.179
Brown, S. A., Brumback, T., Tomlinson, K., Cummins, K., Thompson, W. K., Nagel, B. J., De Bellis, M. D., Hooper, S. R., Clark, D. B., Chung, T., Hasler, B. P., Colrain, I. M., Baker, F. C., Prouty, D., Pfefferbaum, A., Sullivan, E. V., Pohl, K. M., Rohlfing, T., Nichols, B. N., … Tapert, S. F. (2015). The National Consortium on Alcohol and NeuroDevelopment in Adolescence (NCANDA): A multisite study of adolescent development and substance use. Journal of Studies on Alcohol and Drugs, 76(6), 895–908. https://doi.org/10.15288/jsad.2015.76.895
Bucholz, K. K., Cadoret, R., Cloninger, C. R., Dinwiddie, S. H., Hesselbrock, V. M., Nurnberger, J. I., Reich, T., Schmidt, I., & Schuckit, M. A. (1994a). A new, semi-structured psychiatric interview for use in genetic linkage studies. Journal of Studies on Alcohol, 55, 149–158.
Bucholz, K. K., Cadoret, R., Cloninger, C. R., Dinwiddie, S. H., Hesselbrock, V. M., Nurnberger, J. I., Reich, T., Schmidt, I., & Schuckit, M. A. (1999b). A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of the SSAGA. Journal of Studies on Alcohol, 55(2), 149–158. https://doi.org/10.15288/jsa.1994b.55.149
Centers for Disease Control and Prevention. (2015). US department of health, and human services. (2013). REPORT—Antibiotic Resistance Threats in the United States, 1–114.
Chung, T., Creswell, K. G., Bachrach, R., Clark, D. B., & Martin, C. S. (2018). Adolescent binge drinking. Alcohol Research: Current Reviews, 39(1), 5–15.
Clark, D. B., Chung, T., Martin, C. S., Hasler, B. P., Fitzgerald, D. H., Luna, B., Brown, S. A., Tapert, S. F., Brumback, T., Cummins, K., Pfefferbaum, A., Sullivan, E. V., Pohl, K. M., Colrain, I. M., Baker, F. C., De Bellis, M. D., Nooner, K. B., & Nagel, B. J. (2017). Adolescent executive dysfunction in daily life: Relationships to risks, brain structure and substance use. Frontiers in Behavioral Neuroscience, 11, 223. https://doi.org/10.3389/fnbeh.2017.00223
Cole, J., Sprang, G., & Silman, M. (2019). Interpersonal trauma exposure, trauma symptoms, and severity of substance use disorder among youth entering outpatient substance abuse treatment. Journal of Child & Adolescent Trauma, 12(3), 341–349. https://doi.org/10.1007/s40653-018-0239-3
Coskunpinar, A., Dir, A. L., & Cyders, M. A. (2013). Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research, 37(9), 1441–1450. https://doi.org/10.1111/acer.12131
Danese, A., & McEwen, B. S. (2012). Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior, 106(1), 29–39. https://doi.org/10.1016/j.physbeh.2011.08.019
De Bellis, M. D. (2001). Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology, 13(3), 539–564. https://doi.org/10.1017/S0954579401003078
De Bellis, M. D. (2002). Developmental traumatology: A contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology, 27(1–2), 155–170.
De Bellis, M. D., Nooner, K. B., Brumback, T., Clark, D. B., Tapert, S. F., & Brown, S. A. (2020). Posttraumatic stress symptoms predict transition to future adolescent and young adult moderate to heavy drinking in the NCANDA sample. Current Addiction Reports, 7(2), 99–107. https://doi.org/10.1007/s40429-020-00303-1
Degenhardt, L., O’Loughlin, C., Swift, W., Romaniuk, H., Carlin, J., Coffey, C., Hall, W., & Patton, G. (2013). The persistence of adolescent binge drinking into adulthood: Findings from a 15-year prospective cohort study. British Medical Journal Open, 3(8), e003015. https://doi.org/10.1136/bmjopen-2013-003015
Dube, S. R., Anda, R. F., Felitti, V. J., Edwards, V. J., & Croft, J. B. (2002). Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors, 27(5), 713–725.
Dube, S. R., Felitti, V. J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, household dysfunction and the risk of illicit drug use: The adverse childhood experiences Study. Pediatrics, 111(3), 564–572.
Dube, S. R., Anda, R. F., Whitfield, C. L., Brown, D. W., Felitti, V. J., Dong, M., & Giles, W. H. (2005). Long-term consequences of childhood sexual abuse by gender of victim. American Journal of Preventive Medicine, 28(5), 430–438. https://doi.org/10.1016/j.amepre.2005.01.015
Fang, L., & McNeil, S. (2017). Is there a relationship between adverse childhood experiences and problem drinking behaviors? Findings from a population-based sample. Public Health, 150, 34–42. https://doi.org/10.1016/j.puhe.2017.05.005
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8
Glaser, D. (2000). Child abuse and neglect and the brain—A review. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 41(1), 97–116.
Haaris Sheikh, M., Naveed, S., Waqas, A., & Tahir Jaura, I. (2018). Association of adverse childhood experiences with functional identity and impulsivity among adults: A cross-sectional study. Research, 6, 1978. https://doi.org/10.12688/f1000research.13007.2
Hesselbrock, M., Easton, C., Bucholz, K. K., Schuckit, M., & Hesselbrock, V. (1999). A validity study of the SSAGA–A comparison with the SCAN. Addiction, 94(9), 1361–1370. https://doi.org/10.1046/j.1360-0443.1999.94913618.x
Hingson, R. W., Heeren, T., & Winter, M. R. (2006). Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatrics & Adolescent Medicine, 160(7), 739. https://doi.org/10.1001/archpedi.160.7.739
Jacobsen, L. K., Southwick, S. M., & Kosten, T. R. (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry, 158(8), 1184–1190. https://doi.org/10.1176/appi.ajp.158.8.1184
Jacobus, J., Thayer, R. E., Trim, R. S., Bava, S., Frank, L. R., & Tapert, S. F. (2013). White matter integrity, substance use, and risk taking in adolescence. Psychology of Addictive Behaviors, 27(2), 431–442. https://doi.org/10.1037/a0028235
Jakupcak, M., Tull, M. T., McDermott, M. J., Kaysen, D., Hunt, S., & Simpson, T. (2010). PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors, 35(9), 840–843. https://doi.org/10.1016/j.addbeh.2010.03.023
Jaycox, L. H., Ebener, P., Damesek, L., & Becker, K. (2004). Trauma exposure and retention in adolescent substance abuse treatment. Journal of Traumatic Stress, 17(2), 113–121. https://doi.org/10.1023/B:JOTS.0000022617.41299.39
Johnston, L. D., O’Malley, P. M., Miech, R. A., Bachman, J. G., & Schulenberg, J. E. (2016). Monitoring the future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. The University of Michigan.
Kim, J. H., & Choi, J. Y. (2020). Influence of childhood trauma and posttraumatic stress symptoms on impulsivity: Focusing on differences according to the dimensions of impulsivity. European Journal of Psychotraumatology, 11(1), 1796276. https://doi.org/10.1080/20008198.2020.1796276
Kirsch, D., Nemeroff, C. M., & Lippard, E. T. C. (2020). Early life stress and substance use disorders: Underlying neurobiology and pathways to adverse outcomes. Adversity and Resilience Science, 1(1), 29–47. https://doi.org/10.1007/s42844-020-00005-7
Lejuez, C. W., Magidson, J. F., Mitchell, S. H., Sinha, R., Stevens, M. C., & De Wit, H. (2010). Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders: IMPULSIVITY AND AUDS. Alcoholism: Clinical and Experimental Research, no-no. https://doi.org/10.1111/j.1530-0277.2010.01217.x
Long, J. S. (1997). Regression models for categorical and limited dependent variables. Sage Publications.
MacKillop, J., Amlung, M. T., Few, L. R., Ray, L. A., Sweet, L. H., & Munafò, M. R. (2011). Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology (berl), 216(3), 305–321. https://doi.org/10.1007/s00213-011-2229-0
Madden, G. J., & Bickel, W. K. (Eds.). (2010). Impulsivity: The behavioral and neurological science of discounting. American Psychological Association. https://doi.org/10.1037/12069-000
McKinney, C. M., Harris, T. R., & Caetano, R. (2009). Reliability of self-reported childhood physical abuse by adults and factors predictive of inconsistent reporting. Violence and Victims, 24(5), 653–668. https://doi.org/10.1891/0886-6708.24.5.653
Moeller, F. G., Barratt, E. S., Dougherty, D. M., Schmitz, J. M., & Swann, A. C. (2001). Psychiatric aspects of impulsivity. American Journal of Psychiatry, 158(11), 1783–1793. https://doi.org/10.1176/appi.ajp.158.11.1783
National Institute of Alcohol Abuse and Alcoholism. (2004). NIAAA council approves definition of binge drinking. NIAAA Newsletter.
Norman, S. B., Stein, M. B., & Davidson, J. R. T. (2007a). Profiling posttraumatic functional impairment. The Journal of Nervous and Mental Disease, 195(1), 48–53. https://doi.org/10.1097/01.nmd.0000252135.25114.02
Norman, S. B., Tate, S. R., Anderson, K. G., & Brown, S. A. (2007b). Do trauma history and PTSD symptoms influence addiction relapse context? Drug and Alcohol Dependence, 90(1), 89–96. https://doi.org/10.1016/j.drugalcdep.2007.03.002
Oberleitner, L. M. S., Smith, P. H., Weinberger, A. H., Mazure, C. M., & McKee, S. A. (2015). Impact of exposure to childhood maltreatment on transitions to alcohol dependence in women and men. Child Maltreatment, 20(4), 301–308. https://doi.org/10.1177/1077559515591270
Petersen, A. C., Crockett, L., Richards, M., & Boxer, A. (1988). A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence, 17(2), 117–133.
Pfefferbaum, A., Kwon, D., Brumback, T., Thomson, W. K., Cummins, K., Tapert, S. F., Brown, S. A., Thompson, W., Colrain, I., Baker, F., Prouty, D., De Bellis, M. D., Clark, D. B., Nagel, B., Chu, W., Park, S. H., Pohl, K. M., & Sullivan, E. V. (2018). Altered brain developmental FC, trajectories in adolescents after initiating drinking. American Journal of Psychiatry, 175(4), 370–380.
Pfefferbaum, A., Rohlfing, T., Pohl, K. M., Lane, B., Chu, W., Kwon, D., Nolan Nichols, B., Brown, S. A., Tapert, S. F., Cummins, K., Thompson, W. K., Brumback, T., Meloy, M. J., Jernigan, T. L., Dale, A., Colrain, I. M., Baker, F. C., Prouty, D., De Bellis, M. D., … Sullivan, E. V. (2016). Adolescent development of cortical and white matter structure in the NCANDA sample: role of sex, ethnicity, puberty, and alcohol drinking. Cerebral Cortex, 26(10), 4101–4121.https://doi.org/10.1093/cercor/bhv205
Preacher, K. J., Curran, P. J., & Bauer, D. J. (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31(4), 437–448. https://doi.org/10.3102/10769986031004437
Pynoos, R. S., Steinberg, A. M., & Piacentini, J. C. (1999). A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological Psychiatry, 46(11), 1542–1554. https://doi.org/10.1016/S0006-3223(99)00262-0
Secades-Villa, R., Martínez-Loredo, V., Grande-Gosende, A., & Fernández-Hermida, J. R. (2016). The relationship between impulsivity and problem gambling in adolescence. Frontiers in Psychology, 7.https://doi.org/10.3389/fpsyg.2016.01931
Shin, S. H., Edwards, E. M., & Heeren, T. (2009). Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of Adolescent Health (AddHealth) Study. Addictive Behaviors, 34(3), 277–280. https://doi.org/10.1016/j.addbeh.2008.10.023
Shin, S. H., Hong, H. G., & Jeon, S.-M. (2012). Personality and alcohol use: The role of impulsivity. Addictive Behaviors, 37(1), 102–107. https://doi.org/10.1016/j.addbeh.2011.09.006
Shin, S. H., Miller, D. P., & Teicher, M. H. (2013). Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug and Alcohol Dependence, 127(1–3), 31–38. https://doi.org/10.1016/j.drugalcdep.2012.06.005
Shin, S. H., Lee, S., Jeon, S.-M., & Wills, T. A. (2015). Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse & Neglect, 50, 94–103. https://doi.org/10.1016/j.chiabu.2015.02.010
Shin, S. H., McDonald, S. E., & Conley, D. (2018). Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addictive Behaviors, 78, 187–192. https://doi.org/10.1016/j.addbeh.2017.11.020
Silveri, M. M. (2012). Adolescent brain development and underage drinking in the United States: Identifying risks of alcohol use in college populations. Harvard Review of Psychiatry, 20(4), 189–200. https://doi.org/10.3109/10673229.2012.714642
Sinha, R. (2009). Stress and addiction: A dynamic interplay of genes, environment, and drug intake. Biological Psychiatry, 66(2), 100–101. https://doi.org/10.1016/j.biopsych.2009.05.003
Skeer, M., McCormick, M. C., Normand, S.-L.T., Buka, S. L., & Gilman, S. E. (2009). A prospective study of familial conflict, psychological stress, and the development of substance use disorders in adolescence. Drug and Alcohol Dependence, 104(1–2), 65–72. https://doi.org/10.1016/j.drugalcdep.2009.03.017
Southwick, S. M., Bremner, J. D., Rasmusson, A., Morgan, C. A., Arnsten, A., & Charney, D. S. (1999). Role of norepinephrine in the pathophysiology and treatment of posttraumatic stress disorder. Biological Psychiatry, 46(9), 1192–1204. https://doi.org/10.1016/S0006-3223(99)00219-X
Squeglia, L. M., & Gray, K. M. (2016). Alcohol and drug use and the developing brain. Current Psychiatry Reports, 18(5), 46. https://doi.org/10.1007/s11920-016-0689-y
Stanger, C., Ryan, S. R., Fu, H., Landes, R. D., Jones, B. A., Bickel, W. K., & Budney, A. J. (2012). Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology, 20(3), 205–212. https://doi.org/10.1037/a0026543
Steward, T., Mestre-Bach, G., Fernández-Aranda, F., Granero, R., Perales, J. C., Navas, J. F., Soriano-Mas, C., Baño, M., Fernández-Formoso, J. A., Martín-Romera, V., Menchón, J. M., & Jiménez-Murcia, S. (2017). Delay discounting and impulsivity traits in young and older gambling disorder patients. Addictive Behaviors, 71, 96–103. https://doi.org/10.1016/j.addbeh.2017.03.001
Strine, T. (2012). Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. American Journal of Health Behavior, 36(3). https://doi.org/10.5993/AJHB.36.3.11
Sullivan, E. V., Brumback, T., Tapert, S. F., Fama, R., Prouty, D., Brown, S. A., Cummins, K., Thompson, W. K., Colrain, I. M., Baker, F. C., De Bellis, M. D., Hooper, S. R., Clark, D. B., Chung, T., Nagel, B. J., Nichols, B. N., Rohlfing, T., Chu, W., Pohl, K. M., & Pfefferbaum, A. (2016). Cognitive, emotion control, and motor performance of adolescents in the NCANDA study: Contributions from alcohol consumption, age, sex, ethnicity, and family history of addiction. Neuropsychology, 30(4), 449–473. https://doi.org/10.1037/neu0000259
Tarter, R. E., Kirisci, L., Mezzich, A., Cornelius, J. R., Pajer, K., Vanyukov, M., Gardner, W., Blackson, T., & Clark, D. (2003). Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry, 160(6), 1078–1085. https://doi.org/10.1176/appi.ajp.160.6.1078
Townshend, J. M., Kambouropoulos, N., Griffin, A., Hunt, F. J., & Milani, R. M. (2014). Binge drinking, reflection impulsivity, and unplanned sexual behavior: Impaired decision-making in young social drinkers. Alcoholism: Clinical and Experimental Research, 38(4), 1143–1150. https://doi.org/10.1111/acer.12333
Twardosz, S., & Lutzker, J. R. (2010). Child maltreatment and the developing brain: A review of neuroscience perspectives. Aggression and Violent Behavior, 15(1), 59–68. https://doi.org/10.1016/j.avb.2009.08.003
Walker, J., Bountress, K. E., Calhoun, C. D., Metzger, I. W., Adams, Z., Amstadter, A., Thomas, S., & Danielson, C. K. (2018). Impulsivity and comorbid PTSD and binge drinking. Journal of Dual Diagnosis, 14(2), 89–95. https://doi.org/10.1080/15504263.2018.1439212
Wardell, J. D., Strang, N. M., & Hendershot, C. S. (2016). Negative urgency mediates the relationship between childhood maltreatment and problems with alcohol and cannabis in late adolescence. Addictive Behaviors, 56, 1–7. https://doi.org/10.1016/j.addbeh.2016.01.003
Weiss, N. H., Tull, M. T., Viana, A. G., Anestis, M. D., & Gratz, K. L. (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. https://doi.org/10.1016/j.janxdis.2012.01.007
Funding
This work was made possible with support by NIH Grants AA021697, AA021695, AA021692, AA021696, AA021681, AA021690, and AA021691. Data used here are from the data release NCANDA_PUBLIC_4Y_REDCAP_V02 (https://dx.doi.org/10.7303/syn24226662) distributed to the public according to the NCANDA Data Distribution agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arwood, Z., Nooner, K.B. Adverse Childhood Experiences and Binge Drinking in Adolescence: the Role of Impulsivity and PTSD Symptoms. J Pediatr Neuropsychol 9, 30–41 (2023). https://doi.org/10.1007/s40817-022-00135-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40817-022-00135-z