Abstract
Purpose of Review
In this review, we discuss the current state of scalable manufacturing of a reproducible and potent allogeneic MSC product.
Recent Findings
Progress in the manufacturing of MSCs is focused on automated systems such as hollow-fiber and microcarrier-based bioreactor designs as viable paths towards commercial scales. Insights highlighted from scaled-down bioprocess screenings that have helped bridge the transition to scale-up manufacturing are discussed. The quality of MSCs, specifically potency assay development, is considered to systematically drive bioprocess decision making during scale-up. These potency assays include MSC activation or T cell suppression assays to understand the immunomodulatory properties of MSCs as referenced to surrogate biomarkers of inflammatory cytokines that activate MSCs and their biological functions in vitro. Reverse engineering potency based on clinical data is emphasized to develop accurate assays that predict in vivo potency.
Summary
Ultimately, these considerations will help new and existing developers better standardize operating procedures that will influence the scalable production of a potent MSC therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human mesenchymal stem/stromal cells (MSCs) have had a long history of evaluation as a cell immunotherapy. The wide and accelerated clinical use of MSCs has, in large part, been driven by pragmatic reasons: MSCs are easy to isolate, can expand substantially in cell culture, can be frozen without significant compromise to their viability upon thaw, and have purported low immunogenicity to cross transplant barriers as an allogeneic product, thus enabling an “off-the-shelf” inventory of drug substance. Their mechanism of action in immune-mediated diseases has been largely ascribed with release of secreted factors for broad-spectrum immunomodulation. Depending on the type of clinical indication, different methods of clinical cell delivery can be chosen. Systemic infusion is the most common route for MSC therapies in clinical trial registries. Therefore, this review focuses on systemic infusion [1, 2]. MSC infusion has been actively investigated as an infusion product in patients ranging from graft-versus-host-disease (GVHD) [3, 4], diabetes [5], liver failure [6], and multiple sclerosis [7]. Alternate approaches using ex vivo MSC therapy [8, 109••, ] and MSC-derived exosomes [8] are also in early clinical evaluation. Though no products have received FDA approval in adults, an estimate of one MSC therapeutic product approval for a highly prevalent indication would require a staggering 3 × 1013 MSCs to meet clinical demand per year [11•]. In order to meet this demand, sufficient investment should be focused on how these therapeutics can be manufactured, processed, and validated in closed systems under cGMP conditions in a robust manner.
Creating a Target Product Profile
For a cell therapy developer to design an appropriate clinical- or commercial-scale manufacturing process for their therapeutic indications of interest, a target product profile (TPP) is worth establishment at the earliest stages. A TPP captures critical attributes of a product before development begins including the desired indication and dosage regimen among other product criteria. One implication of a well-crafted TPP is an estimation of lot size projections for each indication, which can drive a manufacturing strategy [11•]. Although different therapeutic indications for MSCs would require different size of manufacturing lots, in this review, we focus on conventional intravenous administration of MSCs at 2 × 106 cells/kg to estimate a practical lot size of 10, 25, 100 and 500 billion MSCs for phase I trial, phase II, phase III, and commercial phase, respectively [11•]. Once a target lot size is determined, a required scale of manufacturing process can be designed to select and evaluate appropriate materials and equipment required for the entire process ideally following a quality-by-design paradigm. A typical manufacturing process for MSCs, which will be covered in more detail herein, involves a series of unit operations including tissue acquisition, upstream (cell culture) and downstream (harvest, volume reduction, wash, fill/finish and cryopreservation) processes, and testing and release (Fig. 1). Realizing a robust cell-manufacturing platform at the desired scale would then involve optimizing and scaling up each of the unit operations. To note, this manuscript discusses up to the point of MSC cryopreservation. There have been conflicting discoveries about MSC functionality and viability after cryopreservation, with reports that cryo-banked MSCs showed reduced immunomodulatory and blood regulatory properties and in vitro functionalities directly after thawing [12, 13]. However, conflicting discoveries have also been reported that 24 h of cell culture post-thaw led to a full restoration of the functionalities (including immune suppressor activity, IFN-g responsiveness and induction of IDO) [12]. Further, Moll et al. demonstrated that use of modified cryopreservation methods they had developed retained high viability and in vitro and in vivo functionalities [13]. Together, the final efficacy of cryopreserved cells could be enhanced by optimizing cryopreservation methods and/or by further developing a “therapeutic regime” at the point of care—e.g., a regime to involve a certain period (24 h or longer) of cell culture post-thaw prior to administration to a patient.
Master Cell Bank Creation
MSC manufacturing begins at the initial donor collection and ends at the final product infusion with several major processes in between [14]. Allogeneic MSCs are isolated from donor tissue samples, typically bone-marrow aspirates, by differential adhesion to create a master cell bank (MCB). Other sources include adipose tissue (e.g. SVF) or perinatal tissue sources (e.g., umbilical cord placenta), each of which is used equally as MSC sources in clinical trials today [2]. Studies have shown that age and gender of a donor can influence MSC expansion and potency [15, 16]. The true influence of donor age, gender, and comorbidities is still controversially discussed and strongly depends on the chosen assay readout and the target product profile [17]. A MCB is typically enriched in fibroblastic precursors at early-stage processing. This may depend on the starting material and isolation process, with most contaminants gone at passages 2–3. Different process parameters such as primary and secondary seeding densities, media changes, etc. can influence this as well.
MSCs can have heterogeneous populations of MSCs and even trace numbers of hematological precursors at this early expansion stage [18, 19]. In a comparative study of two typical isolation protocols, it was reported that Ficoll–Paque density gradient centrifugation was the more effective method for bone-marrow derived MSC isolation [20], providing higher cell yields, increased proliferation rates, and shorter primary culture. Closed, automated systems for density separation such as a Sepax system can be effective uses of technology to standardize isolation procedures [21]. The expansion of MSCs for human use should minimize (ideally eliminate) use of antibiotics and animal-derived products in serum and/or supplements to reduce risk to patient exposure. Several advances in xeno-free culture media demonstrate increased yields [22, 23], reduced cost of goods, and preservation of MSC characteristics [24]. These media formulations are worthy of testing and optimizing prior to technology transfer into clean-room facilities to define quality criteria that can be more accurately reproduced under cGMP engineering runs.
Intermediate Cell Banking in Two-Dimensions and Hollow-Fiber Systems
MCBs can be further expanded into intermediate banks to create larger inventory and seeding stocks for 3D bioreactor expansion and more reproducible batch production from a single donor. This is especially important for large-scale manufacturing in large clinical trials. However, potency and diminishing returns of exhausting growth potential and having stable inventory after certain population doubling thresholds [16] should be considered before defining a cell banking strategy. Intermediate banks of MSCs are typically grown in two-dimensional flasks or multi-layer factories, such as CellSTACK or HYPERFlasks, that have the potential to generate between 10 and 50 × 109 cells using scale-out methods [25]. Yet, two-dimensional culture is cost and labor intensive, limited in scale-out, and more susceptible to contamination due to manual manipulations.
To address these problems, a transition to 3D suspension culture is the most viable path forward for commercial-scale production of allogenic MSC therapeutic products. 3D culture provides a higher culture surface, though can impact MSC phenotype [26]. Differences in culture topography (2D vs 3D cell culture), pore size, substrate stiffness and cell attachment ligands impact therapeutically relevant cell properties through integrin signaling and can make a difference not only for the efficiency of the culture system but also for the potency of the resulting product [26, 27].
One such option is hollow-fiber bioreactors, which can expand MSCs on bundles of thin porous fibers where MSCs can attach. MSCs are seeded on a membrane that separates them from a perfusate stream of recirculating media. Selecting membrane materials, attachment factors, and fluid flow configurations are important process development studies to define a robust unit operation. The fiber membrane is semi-permeable for the passage of nutrients while protecting the cells from shear forces [28]. This system, in one design, has efficiently expanded cells with one bioreactor capable of housing up to almost 5 × 108 cells [29, 30] with expansion ratios over 16.5 × [ 29–32]. Packed and fibrous bioreactor designs have also been implemented for the expansion of MSCs. These designs use spherical particles tightly packed together or porous scaffold structures to provide a high surface area to volume ratio and administer media through either circulating the media in a closed vessel (CelliGen®) or use a wave-motion generator to perfuse media in and out of the vessel (CelCradle™) [33]. In this design, similar to packed bed bioreactors, a variety of carrier types can be packed into the bioreactor for MSC adherence.
These cell expansion paradigms are well-suited to expand MCBs to intermediate banks with an understanding of cell bank stability and demands of a specific target product profile. However, the yields attained even under scale-out conditions do not lend themselves toward the economies of scale needed for final product manufacture and may not be commercially viable for MSC indications with large projected demand.
Final MSC Expansion in Suspension Culture for Commercial Scale Manufacturing
The biologics industry has had success in commercial scale expansion of suspension cells for production of proteins, monoclonal antibodies, and vaccines. A suspension format enables the use of automated stirred-tank expansion systems with continuous monitoring, a mainstay in the biopharmaceutical sector. Adherent cells, such as MSCs, pose a different challenge to commercial cell expansion due their need for a growth surface. The adaptation of adherent cells into a suspension cell line has been used in a variety of bioproduction cell types such as HEK, Vero, BHK, and CHO cells, though has not been demonstrated in MSCs. Certainly, the process of altering cell phenotype to a suspension phenotype could negatively impact the potency and differentiation potential of MSCs, so comparability studies between adherent and suspension-adapted MSCs would be crucial for future adoption.
A hybrid solution for 3D MSC culture has been the use of biomaterial substrates, including collagen, fibronectin [34], or adhesive peptides [3536••] that can act as a suspension surface [36••, 37, 38]. Compared to monolayer culture, these suspension materials provide a larger surface area to volume ratio capable of supporting denser cultures [39]. Microencapsulation is one technique, whereby cells are physically encapsulated within hydrogels intended to mimic native extracellular matrices. This approach has been evaluated for MSCs with limited success as these biomaterials typically do not provide enough attachment motifs, which can affect cell growth and inter-cell interactions [26, 40]. This approach has been evaluated for MSCs with limited success. MSCs have shown long-term viability and differentiation potential in microencapsulated forms using hydrogels with various properties [41]. However, the need for a complimentary high-throughput production in microencapsulated MSCs under cGMP conditions, large scale yield data, and further characterization of CQAs and impurities from capsular material are all warranted for further consideration of this technique.
Microcarriers, in contrast, are spherical particles (typically 100–300 μm in diameter) that function as substrates for adherent cell types to grow on the surface while in the cell-particle complex can be cultured in suspension. Process development studies should consider the different types of commercially available microcarriers that have specific porosities, size, chemically functionalized or extracellular matrix coatings, and 3D surface topology, which is important for adherent MSC growth in suspension. Table 1 highlights examples of estimated yields from microcarrier expansion of MSCs at different scales. Scaled-down process development studies involving bioreactor operation and optimization of microcarrier based MSC expansion have identified several important process parameters for consideration in larger conditions [34, 42, 43]. Behie and colleagues provided additional review articles on bioreactor-mediated process development for MSCs [44, 45]. A few public reports have shown that expansion of MSCs in a 50-L stir tank bioreactor is feasible. One example of MSC microcarrier culture at this scale yielded 1 × 1010 cells over 11 days using collagen-coated microcarriers (43-fold expansion) with a viability of 96.9% [36••]. Of note, these studies included microcarriers with animal derived biological coatings which stands in contrast to growing trends away from xenogenic processes [46, 47].
The flow conditions of impeller-based bioreactors can pose biophysical forces that may harm MSCs at > 50 L scales, thus spawning newer fluid mixing designs such as vertical-wheel bioreactors commercialized by PBS Biotech. [35]. Vertical-wheel bioreactors have shown to provide more homogenous distribution of microcarriers compared to horizontal impeller systems found in stir-tank bioreactors [48] and have shown to provide a low shear environment in vessels up to 500 L [49]. Such designs have estimated yields of ~ 100 × 109 cells [25], though have not been publicly reported at full scale. Early reports at pilot and small production scale have demonstrated the feasibility of scaling MSC expansion using vertical-wheel bioreactor platforms [50]. MSCs expanded in xeno-free conditions using Synthemax II microcarriers in 3 L, 15 L, and 50 L vertical-wheel bioreactors, achieved yields up to 500,000 cells/mL within 4–5 days of culture among different donors [51]. Total cell number yields of 1.5 × 109, 1 × 1010, and 3.1 × 1010 MSCs were reported at each volumetric scale, respectively. In comparison to 2D monolayer controls, MSCs expanded in the 50L vertical-wheel bioreactor maintained pre-defined CQAs. Despite this success, parameters for downstream processing at the 50L production scale highlight the need for continued optimization, as reported by a near 15% reduction in post-harvest recovery [51].
Scalable Technologies for Cell Washing and Concentration Fill and Finishing
Several technologies for downstream processing have been proposed to meet minimal product requirements for allogeneic cell therapeutic manufacturing [52]. Few, however, provide the scalability in a closed-system format capable of processing multi-liter cell suspensions, while also ensuring product purity and high concentrating factors. Because the cells are the therapeutic product, it is critical to concentrate them in yields with > 85% viability, < 1 ppm impurities, and maintenance of critical quality attributes [53]. One option that meets such criteria at commercial scale production is the counter-flow centrifugation system.
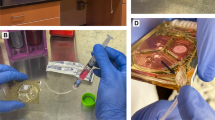
The most frequently used technology, Ksep™ commercialized by Sartorius, is a closed counterflow centrifugation system designed to concentrate cells with > 97% recovery. Its largest model, the Ksep 6000S, is capable of processing 1.2 × 1012 cells per cycle up to volumes of 2000 L (720 L/h). Despite these promising aspects of the Ksep system, there is limited information available regarding the system’s optimization/efficiency in washing and concentrating cells expanded in microcarrier based platforms. In a recent study, human pluripotent stem cells (hPSC) were expanded using microcarriers in a stir-tank bioreactor and subsequently concentrated using the Ksep 400 system [54]. Across five separate runs, hPSCs were concentrated at an optimized flow rate of 120 mL/min. Achieved cell recovery was > 90% with loss in viability reported to be < 1.3%. Readers can be directed to [54] for additional information regarding Ksep performance optimization.
Advancements in acoustic wave separation is another emerging scalable technology capable of washing and concentrating cells prior to final formulation and fill. Separators like the Ekko™ (FloDesign Sonics®) utilize macroscale acoustofluidic principles to separate particles of different sizes and density. In this system ultrasonic standing waves are generated by a piezo-electric transducer, capable of eliciting multidimensional standing waves. Cells subjected to these multidimensional waves are trapped at the standing wave nodes until they sediment out of suspension into a collection port. The Ekko has been reported to accommodate flow rates between 5 and 50 mL/min depending on the cell manipulation to be performed. Although promising in microcarrier/cell separation [55], further system optimization of scaling strategies are required if it is to accommodate allogeneic expansion platforms > 100 L.
Quality Control: MSC Potency Assays
Due to variability in MSC sourcing and different manufacturing processes, it is essential that MSCs are evaluated for quality control (QC) purposes throughout bioprocessing and scale-up. These QC assays are critical during technology transfer of processes from one manufacturing center to another when considering large distribution programs. The International Society for Cellular Therapy (ISCT) has set minimal critical quality attributes (CQAs) to define cells as MSCs [56], though there can be batch-to-batch variation in phenotype and function among different donors. Similar inter-donor variation was validated over successive population doublings by Heathman et al., which highlights the potential implications such variations could have for scaled-out manufacturing processes [16]. To avoid such variation, manufacturers should screen multiple CQAs characteristic of a desired TPP. Additional to the minimal criteria set by the ISCT, researchers have set CQAs that evaluate colony-forming unit fibroblast efficiency (CFU-F), multiplex analysis of cytokine production, transcript profiling, expanded immunophenotype analysis, short tandem repeat analysis, and immune modulation analysis [16, 19, 22, 57]. These advanced analytical techniques, however, come with considerable variance in testing methods and, though insightful for continued product characterization, may not be useful for product release.
The most critical, and elusive, for MSC therapy has been to quantitatively assess their therapeutic potency in vitro as a predictor of in vivo efficacy. Investigators have measured the regenerative effects of MSC-derived molecules including Sfrp-2 [58], SDF-1 [59, 60], IGF-1, VEGF [61], and many others in the protection of epithelial cells. Anti-apoptotic effects due to paracrine MSC factors have also been observed in injury models of the liver, kidney, and brain due to BDNF, NGF [62], and others. Yet, immune profiling offers a more direct way to assess cause-and-effect by blood measurements that aligns with MSCs known action to suppress lymphocyte and immune cell proliferation, warranting their use for immunotherapy applications [63, 64]. Immune bioassays for MSCs have been researched extensively by de Wolf et al. [65]. A recent review highlights the importance of in vivo biomarkers to correlate with MSC properties [66]. In vitro multiple-assays-matrix for in-depth MSC characterization should be correlated with changes in biomarkers in patients upon MSC use in vivo to establish value and homogeneity between batches or differences in efficacy between products. Many mechanisms have been proposed for MSCs’ mechanisms of action, ranging from short term incorporation [67], to release of microvesicles [68,69,70] or other soluble factor effects [71,72,73]. MSC immunomodulation has, in many references, been a function of secreting bioactive factors that influence the immune response. Potency assays, thus, must strive to discover such secreted factors that are mechanistically causing in vivo efficacy. This may be a multi-factorial set of measurements and include the evaluation of MSC activation which is known to alter secreted factors, including exosomes.
In vitro studies provide a model system to characterize MSC potency in terms of surrogate biomarkers of MSC immunomodulation and secreted factors that may be responsible for such effects. A few examples are reviewed to highlight important biomarkers of interest. Christy et al. evaluated various potency assays for evaluation of human MSCs, finding potency differences in the MSCs based on assay and source of MSC [74]. Using an MSC activation assay, the authors further measured IDO production in response to IFNγ and TNFα, finding that IDO is upregulated after exposure to these cytokines. Indeed, MSCs synthesize many factors such as TSG-6, nitric oxide, prostaglandins, and kyneurine through reaction with blood-borne inflammatory substrates, which are indispensable to MSC therapy [75,76,77,78]. Li et al. studied various properties of a “compartment” where MSCs can modulate T cells and determined the importance of MSC concentration, reaction time, reaction volume, and cellular factors that were dose-dependent [79•]. Chinnadurai et al. cocultured MSCs with PBMCs at different ratios and analyzed PBMC proliferation level as well as cytokine levels [80]. Their findings suggest that PBMC suppression correlated with downregulation of TNFα, IFNγ, IL-13, IL-5, and the upregulation of VEGF, IFNα, IL-7. Similarly, after MSC licensing with proinflammatory factors, researchers found an upregulation of IDO, CXCL9, CXCL10, and CXCL11. Boyt et al. similarly performed an IFNγ-licensed MSC and PBMC coculture and analyzed resulting IDO expression, finding that IDO protein levels are dictated by the dose and duration of the IFNγ licensing. They then pre-licensed the MSCs with IFNγ at various durations and discovered this slightly increases IDO production with longer durations, and that this IDO elevation persisted even once they were removed from the cytokine environment. Finally, they showed that pre-licensed MSCs suppressed PBMCs the strongest, and overall pre-licensing showed the highest form of suppression [81]. Licensing can have a potentially immune-switching phenotype in MSCs as Boland et al. prelicensed MSCs with both IFNγ and TNFα, finding that this reversed the pro-inflammatory effect of MSCs when they are in palmitate [82].
As the field continues to move towards acceptance of the primary role of MSCs as being one of paracrine function rather than direct, long-term engraftment [83] the importance of the secretome, particularly stable fractions such as extracellular vesicles, has gained traction. Increasing importance is falling onto the role of extracellular vesicles, including microvesicles such as exosomes, on MSC function in vivo [84, 85]. Thus, determining the in vivo potency of MSCs would benefit from characterization of the populations’ extracellular vesicles—contents, size, and quantity—rather than looking at the cells themselves. While studying exosome potency in vitro is still solely in vitro and not in vivo, potency assays have been investigated for a broad array of clinical application [86, 87]. Pachler et al. and others have reported differences in the capacities of MSC-derived extracellular vesicles in completing various functions: these exosomes inhibit mitogen induced T-cell proliferation but not antigen-driven mixed lymphocyte reaction in vitro, and these capacities were altered based on cell growth conditions and extracellular vesicle dose [86, 88]. Guo et al. examined MSC-secreted extracellular vesicles as modulators of immune function. MSC-EVs were injected in vivo into a mouse model, and changes in T cell population in the peripheral blood were tested. It was found that proinflammatory IFNγ and TNFα were decreased, and anti-inflammatory IL-10 was increased after MSC-EV treatment. Additionally, following PBMC coculture with varying degrees of MSC-EVs, higher doses of the vesicles led to Tc1 and Th1 immune cell suppression as well as dose-dependent decreases in IFNγ and TNFα and an increase in IL-10, indicating that the MSC-EVs exhibit a significant immunomodulatory effect in vivo [89]. While this is still a leap from measuring potency in vivo, the growing importance of exosomes in MSC mechanism of action suggests that these may be a stronger prediction agent of MSC potency in vivo. Thus, exosome characterization may serve as a broad potency predictor. But specific markers within the exosome characterization would further be needed to best identify the optimal exosomes (e.g., size, contents, rate of release) for a given application.
Reverse Engineering an In Vivo MSC Potency Assay
The outcome of administered MSCs is poorly understood and has hindered the rational development of MSC therapeutics based on an in vivo verified mechanism of action. Several issues muddle a clear understanding of in vivo MSC potency that can be predicted by surrogate biomarkers. Following administration of human MSCs in murine models, there can be rapid clearance of administered cells [67, 78, 90] and potential clot induction [91,92,93,94,95] by intravascular MSC infusion. The variability in clotting outcomes might be due to the lack of standard methods to culture the MSCs. Cells used for human trials can therefore be handled differently by clinical companies. For example, the intensity of IBMIR-triggering differs between stromal cell products from different sources and is influenced by several manufacturing parameters, such as their degree of in vitro expansion and cryopreservation. Cell products may contain remaining procoagulant cell products, lack of anticoagulation and other safety measures, and pre-activated patient status, which can actually lead to thromboembolic accidents [2, 96]. However, in well-controlled clinical studies employing optimized cell application and transfusion protocols, there was no major infusion-related toxicity reported, indicating a good safety profile if typical safety precautions are met. This may be due to highly optimized MSC application procedures in clinical trials [97]. Nevertheless, the issue of clotting must be addressed before full implementation in human studies. While most in vivo MSC research has been conducted with human MSCs in murine models, Galipeau notes a disconnect between “mouse and human clinical outcomes,” likely due to “ immune compatibility, dosing, and fitness of culture adapted MSCs” [98]. Furthermore, the rejection of these cells in allogeneic settings over time has been observed which will further decrease drug bioavailability [78, 99, 100]. Thus, a consistent biomarker signature in human patients has yet to be reported leaving uncertainty with how to manage a potency-driven manufacturing and clinical program.
An alternate approach would be to conduct dose-escalating studies (or analyze existing samples collected from retrospective trials) to identify a clear pharmacokinetic-pharmacodynamic relationship for the field. These studies would be designed with pharmacological endpoints in mind with the goal of exposing MSCs to patients in order to generate a physiological, quantifiable response that varies with dose. A pharmacodynamic response could then inspire an in vitro bioassay to be developed based on an observed alteration in a given target cell type or pathway. Such a “reverse engineering” approach would ensure a potency assay would be based on an observed in vivo effect in humans, leading to more predictable potency assays that would predict efficacy of the treatment.
Conclusion
Technologies are nearing the crossing of a rubicon for the production of MSCs at commercial scale. A linchpin for success may be a potency-guided strategy to connect clinical quality to manufacturing targets.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
Caplan H, et al. Mesenchymal stromal cell therapeutic delivery: translational challenges to clinical application. Front Immunol. 2019;10:1645.
Moll G, et al. Intravascular mesenchymal stromal/stem cell therapy product diversification: time for new clinical guidelines. Trends Mol Med. 2019;25(2):149–63.
Zhao K, et al. Immunomodulation effects of mesenchymal stromal cells on acute graft-versus-host disease after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21(1):97–104.
Kurtzberg J, et al. Allogeneic human mesenchymal stem cell therapy (remestemcel-L, Prochymal) as a rescue agent for severe refractory acute graft-versus-host disease in pediatric patients. Biol Blood Marrow Transplant. 2014;20(2):229–35.
Moon K-C, et al. Potential of allogeneic adipose-derived stem cell-hydrogel complex for treating diabetic foot ulcers. Diabetes (New York, N.Y.). 2019;68(4):837–846
Lin Bl, et al. Allogeneic bone marrow–derived mesenchymal stromal cells for hepatitis B virus–related acute‐on‐chronic liver failure: A randomized controlled trial. Hepatology (Baltimore, Md.). 2017;66(1):209–219.
Petrou P, et al. Beneficial effects of autologous mesenchymal stem cell transplantation in active progressive multiple sclerosis. Brain (London, England : 1878). 2020;143(12):3574–3588.
Allen A, et al. Mesenchymal Stromal Cell Bioreactor for Ex Vivo Reprogramming of Human Immune Cells. Sci Rep. 2020;10(1):10142.
•• Swaminathan M, et al. Pharmacological effects of ex vivo mesenchymal stem cell immunotherapy in patients with acute kidney injury and underlying systemic inflammation. Stem Cells Transl Med. 2021. This study reports a pharmacokinetic/pharmacodynamic response in human patients with systemic inflammatory diseases that are treated by ex vivo MSC therapy.
van Poll D, et al. Mesenchymal stem cell-derived molecules directly modulate hepatocellular death and regeneration in vitro and in vivo. Hepatology. 2008;47(5):1634–43.
• Olsen TR, et al. Peak MSC-Are we there yet? Front Med. 2018;5:178–178. This review captures critical process development goals under a target product profile for commercial, allogeneic MSC products.
François M, et al. Human MSC suppression correlates with cytokine induction of indoleamine 2,3-dioxygenase and bystander M2 macrophage differentiation. Mol Ther. 2012;20(1):187–95.
Moll G, et al. Do cryopreserved mesenchymal stromal cells display impaired immunomodulatory and therapeutic properties? Stem Cells. 2014;32(9):2430–42.
Smith D, et al. Towards automated manufacturing for cell therapies. Curr Hematol Malig Rep. 2019;14(4):278–85.
Siegel G, et al. Phenotype, donor age and gender affect function of human bone marrow-derived mesenchymal stromal cells. BMC Med. 2013;11(1):146–146.
Heathman TRJ, et al. Characterization of human mesenchymal stem cells from multiple donors and the implications for large scale bioprocess development. Biochem Eng J. 2016;108:14–23.
Andrzejewska A, et al. Multi-parameter analysis of biobanked human bone marrow stromal cells shows little influence for donor age and mild comorbidities on phenotypic and functional properties. Front Immunol. 2019;10:2474.
Ikebe C, Suzuki K. Mesenchymal stem cells for regenerative therapy: optimization of cell preparation protocols. Biomed Res Int. 2014;2014:951512–611.
Yin JQ, Zhu J, Ankrum JA. Manufacturing of primed mesenchymal stromal cells for therapy. Nature biomedical engineering. 2019;3(2):90–104.
Drela K, et al. Bone marrow-derived from the human femoral shaft as a new source of mesenchymal stem/stromal cells: an alternative cell material for banking and clinical transplantation. Stem Cell Res Ther. 2020;11(1):1–262.
Lechanteur C, et al. Clinical-scale expansion of mesenchymal stromal cells: a large banking experience. J Transl Med. 2016;14(1):145.
Heathman TRJ, et al. Serum-free process development: improving the yield and consistency of human mesenchymal stromal cell production. Cytotherapy (Oxford, England). 2015;17(11):1524–35.
Capelli C, et al. Human platelet lysate allows expansion and clinical grade production of mesenchymal stromal cells from small samples of bone marrow aspirates or marrow filter washouts. Bone marrow transplantation (Basingstoke). 2007;40(8):785–91.
Bhat S, et al. Expansion and characterization of bone marrow derived human mesenchymal stromal cells in serum-free conditions. Sci Rep. 2021;11(1):3403–3403.
Rowley J, Abraham E, Campbell A, Brandwein H, Oh S. Meeting lot-size challenges of manufacturing adherent cells for therapy. BioProcess International. 2012;10(3):16–22.
Drzeniek NM, et al. Bio-instructive hydrogel expands the paracrine potency of mesenchymal stem cells. Biofabrication. 2021;13(4).
Matsiko A, Gleeson JP, O’Brien FJ. Scaffold mean pore size influences mesenchymal stem cell chondrogenic differentiation and matrix deposition. Tissue Eng Part A. 2015;21(3–4):486–97.
de Almeida Fuzeta M, et al. Addressing the manufacturing challenges of cell-based therapies. Current Applications of Pharmaceutical Biotechnology. 2019;171:225–78.
Vymetalova L, et al. Large-scale automated hollow-fiber bioreactor expansion of umbilical cord-derived human mesenchymal stromal cells for neurological disorders. Neurochem Res. 2020;45(1):204–14.
Lambrechts T, et al. Large-scale progenitor cell expansion for multiple donors in a monitored hollow fibre bioreactor. Cytotherapy (Oxford, England). 2016;18(9):1219–33.
Mizukami A, et al. A fully-closed and automated hollow fiber bioreactor for clinical-grade manufacturing of human mesenchymal stem/stromal cells. Stem cell reviews and reports. 2018;14(1):141–3.
Haack-Sørensen M, et al. Culture expansion of adipose derived stromal cells. A closed automated Quantum Cell Expansion System compared with manual flask-based culture. J translational med. 2016;14(1):319–319.
Odeleye AOO, et al. An additive manufacturing approach to bioreactor design for mesenchymal stem cell culture. Biochem Eng J. 2020;156.
Jossen V, et al. Manufacturing human mesenchymal stem cells at clinical scale: process and regulatory challenges. Appl Microbiol Biotechnol. 2018;102(9):3981–94.
Lembong J, et al. Bioreactor parameters for microcarrier-based human MSC expansion under xeno-free conditions in a vertical-wheel system. Bioengineering (Basel). 2020;7(3):73.
•• Lawson T, et al. Process development for expansion of human mesenchymal stromal cells in a 50L single-use stirred tank bioreactor. Biochem Eng J. 2017;120:49–62. This study first reports important process development studies in the production of human MSCs at a 50L scale using microcarrier culture.
Rafiq QA, et al. Culture of human mesenchymal stem cells on microcarriers in a 5 l stirred-tank bioreactor. Biotech Lett. 2013;35(8):1233–45.
Jing D, et al. Growth kinetics of human mesenchymal stem cells in a 3-L single-use, stirred-tank bioreactor. Biopharm international. 2013;26(4):28.
Schnitzler AC, et al. Bioprocessing of human mesenchymal stem/stromal cells for therapeutic use: Current technologies and challenges. Biochem Eng J. 2016;108:3–13.
Qazi TH, et al. Biomaterials that promote cell-cell interactions enhance the paracrine function of MSCs. Biomaterials. 2017;140:103–14.
Khayambashi P, et al. Hydrogel encapsulation of mesenchymal stem cells and their derived exosomes for tissue engineering. Int J Molecular Sci. 2021;22(2).
Rafiq QA, et al. Systematic microcarrier screening and agitated culture conditions improves human mesenchymal stem cell yield in bioreactors. Biotechnol J. 2016;11(4):473–86.
Leber J, et al. Microcarrier choice and bead-to-bead transfer for human mesenchymal stem cells in serum-containing and chemically defined media. Process Biochem. 1991;2017(59):255–65.
Jung S, et al. Large-scale production of human mesenchymal stem cells for clinical applications. Special Issue: Stem Cells and Regenerative Medicine. 2012;59(2):106–20.
Jung S, et al. Quality manufacturing of mesenchymal stem/stromal cells using scalable and controllable bioreactor platforms, in Bioreactors for Stem Cell Expansion and Differentiation. Boca Raton. 2018.
Shahdadfar A, et al. In vitro expansion of human mesenchymal stem cells: choice of serum is a determinant of cell proliferation, differentiation, gene expression, and transcriptome stability. Stem cells (Dayton, Ohio). 2005;23(9):1357–66.
Wang Y, et al. Safety of mesenchymal stem cells for clinical application. Stem cells international. 2012;2012:652034–44.
Croughan MGD, Fang D, Lee B. Novel single-use bioreactors for scale-up of anchorage-dependent cell manufacturing for cell therapies. Stem Cell Manuf. 2016;105–139.
Lee B, et al. New Scalable Manufacturing Platform for Shear-Sensitive Cell Therapy Products. Cytotherapy (Oxford, England). 2016;18(6):S140–S140.
Sousa MF, et al. Production of oncolytic adenovirus and human mesenchymal stem cells in a single-use, Vertical-Wheel bioreactor system: Impact of bioreactor design on performance of microcarrier-based cell culture processes. Biotechnol Prog. 2015;31(6):1600–12.
Kirian RD, et al. Scaling a xeno-free fed-batch microcarrier suspension bioreactor system from development to production scale for manufacturing XF hMSCs. Cytotherapy. 2019;21(5).
Li A, et al. Advances in automated cell washing and concentration. Cytotherapy (Oxford, England), 2021.
Pattasseril J, Varadaraju H, Lock L, Rowley JA. Downstream technology landscape for large-scale therapeutic cell processing. Bioprocess Int. 2013;11(3):38–47.
Pandey PR, et al. End-to-end platform for human pluripotent stem cell manufacturing. Int J Mol Sci. 2019;21(1):89.
Rozembersky JJ, et al. A novel scaleable acoustic cell processing platform for cell concentration and washing. Cytotherapy (Oxford, England). 2017;19(5):e17–e17.
Dominici M, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy (Oxford, England). 2006;8(4):315–317.
Wiese DM, Braid LR. Transcriptome profiles acquired during cell expansion and licensing validate mesenchymal stromal cell lineage genes. Stem Cell Res Ther. 2020;11(1):1–357.
Mirotsou M, et al. Secreted frizzled related protein 2 (Sfrp2) is the key Akt-mesenchymal stem cell-released paracrine factor mediating myocardial survival and repair. Proc Natl Acad Sci U S A. 2007;104(5):1643–8.
Zhang M, et al. SDF-1 expression by mesenchymal stem cells results in trophic support of cardiac myocytes after myocardial infarction. Faseb J. 2007;21(12):3197–207.
Tang YL, et al. Paracrine action enhances the effects of autologous mesenchymal stem cell transplantation on vascular regeneration in rat model of myocardial infarction. Ann Thorac Surg. 2005;80(1):229–36; discussion 236–7.
Sadat S, et al. The cardioprotective effect of mesenchymal stem cells is mediated by IGF-I and VEGF. Biochem Biophys Res Commun. 2007;363(3):674–9.
Kurozumi K, et al. Mesenchymal stem cells that produce neurotrophic factors reduce ischemic damage in the rat middle cerebral artery occlusion model. Mol Ther. 2005;11(1):96–104.
Galipeau J, et al. International Society for Cellular Therapy perspective on immune functional assays for mesenchymal stromal cells as potency release criterion for advanced phase clinical trials. Cytotherapy. 2016;18(2):151–9.
Galipeau J, et al. Mesenchymal stromal cell variables influencing clinical potency: the impact of viability, fitness, route of administration and host predisposition. Cytotherapy. 2021;1–5.
Wolf CD, Bovenkamp MD, Hoefnagel M. Regulatory perspective on in vitro potency assays for human mesenchymal stromal cells used in immunotherapy. Cytotherapy. 2017;19(7):784–797.
Krampera M, Le Blanc K. Mesenchymal stromal cells: Putative microenvironmental modulators become cell therapy. Cell Stem Cell. 2021;28(10):1708–25.
Rbia N, et al. In vivo survival of mesenchymal stromal cell-enhanced decellularized nerve grafts for segmental peripheral nerve reconstruction. J Hand Surg Am. 2019;44(6): 514 e1–514 e11.
Sandiford OA, et al. Mesenchymal stem cell-secreted extracellular vesicles instruct stepwise dedifferentiation of breast cancer cells into dormancy at the bone marrow perivascular region. Cancer Res. 2021;81(6):1567–82.
Cone AS, et al. Mesenchymal stem cell-derived extracellular vesicles ameliorate Alzheimer’s disease-like phenotypes in a preclinical mouse model. Theranostics. 2021;11(17):8129–42.
Kirkham AM, et al. MSC-derived extracellular vesicles in preclinical animal models of bone injury: a systematic review and meta-analysis. Stem Cell Rev Rep. 2021.
Mahendru D, et al. Neuroprotective effect of bone marrow derived mesenchymal stem cell secretome in 6-OHDA-induced Parkinson's disease. Regen Med. 2021.
Tan HL, et al. Human amniotic mesenchymal stem cells-conditioned medium protects mice from high-fat diet-induced obesity. Stem Cell Res Ther. 2021;12(1):364.
Kucharzewski M, et al. Novel trends in application of stem cells in skin wound healing. Eur J Pharmacol. 2019;843:307–15.
Christy BA, et al. Use of multiple potency assays to evaluate human mesenchymal stromal cells. The Journal of Trauma and Acute Care Surgery. 2020;89(2):S109–17.
Meisel R, et al. Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood. 2004;103(12):4619–21.
Ren G, et al. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell. 2008;2(2):141–50.
Nemeth K, et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15(1):42–9.
Lee RH, et al. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell. 2009;5(1):54–63.
• Li M, et al. Therapeutic delivery specifications identified through compartmental analysis of a mesenchymal stromal cell-immune reaction. Scientific Reps. 2018;8(6816). This study develops a compartment model to define criteria for effective MSC immunomodulation of T cells using an in vitro Transwell culture system.
Chinnadurai R, et al. Potency analysis of mesenchymal stromal cells using a combinatorial assay matrix approach. Cell Rep. 2018;22(9):2504–17.
Boyt DT, et al. Dose and duration of interferon γ prelicensing interact with donor characteristics to influence the expression and function of indoleamine-2,3-dioxygenase in mesenchymal stromal cells. J Royal Soc Interf. 2020;17(167).
Boland LK, et al. IFN-γ and TNF-α pre-licensing protects mesenchymal stromal cells from the pro-inflammatory effects of palmitate. Mol Ther. 2018;26(3):860–73.
Spees JL, Lee RH, Gregory CA. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res Ther. 2016;7(1):125.
Yin K, Wang S, Zhao RC. Exosomes from mesenchymal stem/stromal cells: a new therapeutic paradigm. Biomark Res. 2019;7:8.
Nikfarjam S, et al. Mesenchymal stem cell derived-exosomes: a modern approach in translational medicine. J Transl Med. 2020;18(1):449.
Pachler K, et al. An in vitro potency assay for monitoring the immunomodulatory potential of stromal cell-derived extracellular vesicles. Int J Mol Sci. 2017;18(7).
Han Y, et al. Exosomes from hypoxia-treated human adipose-derived mesenchymal stem cells enhance angiogenesis through VEGF/VEGF-R. Int J Biochem Cell Biol. 2019;109:59–68.
Willis GR, Kourembanas S, Mitsialis SA. Toward exosome-based therapeutics: isolation, heterogeneity, and fit-for-purpose potency. Front Cardiovasc Med. 2017;4:63.
Guo L, et al. Extracellular vesicles from mesenchymal stem cells prevent contact hypersensitivity through the suppression of Tc1 and Th1 cells and expansionof regulatory T cells. Int Immunopharmacol. 2019;74.
von Bahr L, et al. Analysis of tissues following mesenchymal stromal cell therapy in humans indicates limited long-term engraftment and no ectopic tissue formation. Stem Cells. 2012;30(7):1575–8.
O’Rourke B, et al. Mesenchymal stromal cell delivery via an ex vivo bioreactor preclinical test system attenuates clot formation for intravascular application. Stem Cells Transl Med. 2021;10(6):883–94.
Coppin L, Sokal E, Stephenne X. Thrombogenic Risk Induced by Intravascular Mesenchymal Stem Cell Therapy: Current Status and Future Perspectives. Cells. 2019;8(10).
Silachev DN, et al. Effect of MSCs and MSC-derived extracellular vesicles on human blood coagulation. Cells. 2019;8(3).
Jung JW, et al. Familial occurrence of pulmonary embolism after intravenous, adipose tissue-derived stem cell therapy. Yonsei Med J. 2013;54(5):1293–6.
Moll G, et al. Are therapeutic human mesenchymal stromal cells compatible with human blood? Stem Cells. 2012;30(7):1565–74.
Moll G, et al. MSC therapies for COVID-19: importance of patient coagulopathy, thromboprophylaxis, cell product quality and mode of delivery for treatment safety and efficacy. Front Immunol. 2020;11:1091.
Hermiller JB, et al. Clonidine in congestive heart failure: a vasodilator with negative inotropic effects. Am J Cardiol. 1983;51(5):791–5.
Galipeau J, Luc SB. Mesenchymal stromal cells: clinical challenges and therapeutic opportunities. Cell Stem Cell. 2018;22(6):824–833.
Gao J, et al. The dynamic in vivo distribution of bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs. 2001;169:12–20.
Schrepfer S, et al. Stem cell transplantation: the lung barrier. Transpl Proc. 2007;39:573–6.
Jossen V, et al. Microcarrier-based expansion of human mesenchymal stem cells in the BIOSTAT STR® 50L, Z.U.o.A. Sciences, Editor. 2017, Sartorius Stedim Biotech GmbH.
Chen S, et al. Facile bead-to-bead cell-transfer method for serial subculture and large-scale expansion of human mesenchymal stem cells in bioreactors. Stem Cells Transl Med. 2021;10(9):1329–42.
Biotech P. Growth of human mesenchymal stem/stromal cells on collagen microcarriers in the Allegro™ STR 50 L Bioreactor. 2020: Port Washington, NY, USA.
Funding
This research was conducted with grant support under Grant No. R01EB012521 awarded by the National Institutes of Health and Department of Defense, BioFab USA (T0067).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
BP has equity shareholdings in Sentien Biotechnologies, Inc. related to MSC therapeutics for commercialization. SJ is an employee of PBS Biotech. The remaining authors have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Stem Cells: Policies from the Bench to the Clinic
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Teryek, M., Doshi, A., Sherman, L.S. et al. Clinical Manufacturing of Human Mesenchymal Stromal Cells using a Potency-Driven Paradigm. Curr Stem Cell Rep 8, 61–71 (2022). https://doi.org/10.1007/s40778-022-00208-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40778-022-00208-x