Abstract
Family factors, such as poor family functioning and trauma, have been associated with negative outcomes for homeless adolescents. Further study is needed to better understand how family factors and trauma jointly relate to mental health problems and externalizing behaviors among homeless adolescents. Structural equation modeling was used to examine the influence of trauma (encompassing traumatic events experienced prior to, and after, becoming homeless) and family factors (poor family functioning and family conflict) on mental health problems and externalizing behaviors (substance use, delinquent behaviors, and sexual risk) among 201 homeless adolescents, ages 12 to 17 years. Trauma, poor family functioning, and family conflict significantly predicted greater mental health problems, delinquent behaviors, high-risk sexual behaviors and substance use. Overall, the findings suggest that family factors appear to be key to understanding mental health problems and externalizing behaviors among homeless adolescents. Implications, limitations and future directions are addressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adolescents comprise 22.1% of the homeless population in the United States, which translates to approximately 1.7 million young people being homeless on any given night (National Alliance to End Homelessness, 2014; SAMHSA, 2010). Given this information, homeless adolescents require far greater attention in our efforts to end homelessness in the U.S. (United States Interagency Council on Homelessness, 2016). The healthy developmental trajectory of these young people into adulthood is a significant public health concern due to their increased risk for mental health problems, externalizing behaviors (e.g., substance use and delinquent behaviors), victimization, sexual abuse and exploitation, trauma, and difficulties in school (APA Presidential Task Force, 2009; Bender, Ferguson, Thompson, Komlo, & Pollio, 2010; Clark & Robertson, 1996; Kelly & Caputo, 2007; Office of Disease Prevention and Health Promotion, 2014). Previous research has found that homeless adolescents report significantly high rates of mental health problems, substance use, and trauma histories (e.g., Merscham, Van Leeuwen, & McGuire, 2009). Moreover, homeless adolescents are at great risk of becoming chronically homeless adults if their mental health and behavioral problems are not addressed and developmentally appropriate housing options (e.g., reconnections to family and returning home, supported transitional housing, etc.) are not provided to enable them to make a healthy transition into adulthood (Fowler, Toro, & Miles, 2009; Toro, Dworsky, & Fowler, 2007).
Adolescents become homeless for a number of reasons, including being jettisoned from their homes or running away from home due to family issues such as poor family functioning and/or family conflict (APA Presidential Task Force, 2009; Haber & Toro, 2004; Toro, Hobden, Durham, Oko-Riebau, & Bokszczanin, 2014), as well as traumatic events such as physical abuse within their homes or exposure to violence in their general environment (Coates & McKenzie-Mohr, 2010). In addition to these traumatic events that occur prior to leaving home, adolescent homelessness is also linked to other traumas such as victimization, violence, sexual abuse, and/or physical abuse that occur during the course of being homeless. Traumatic events experienced both prior to and after becoming homeless can derail the healthy developmental trajectories of homeless adolescents and are risk factors for the onset of mental health problems (Bender et al., 2010; Coates & McKenzie-Mohr, 2010; Edidin, Ganim, Hunter, & Karnik, 2012; Yu, North, LaVesser, Osborne, & Spitznagel, 2008; Van den Bree et al., 2009). For example, homeless adolescents disproportionately report depression and anxiety compared to their housed peers (Ginzler, Garrett, Baer, & Peterson, 2007; Van den Bree et al., 2009). Further, becoming homeless can amplify adolescents’ prior existing mental health problems (Parks, Stevens, & Spence, 2007; Whitbeck, Hoyt, & Yoder, 1999; Yu et al., 2008). These mental health problems can also lead to or co-occur with maladaptive externalizing behaviors (Salomonsen-Sautel et al., 2008) such as violence, delinquency, and substance use and abuse (Whitbeck, Hoyt, & Ackley, 1997; Whitbeck, Hoyt, Yoder, Cauce, & Paradise, 2001).
Clearly, trauma plays a major role in the lives of homeless adolescents. This research investigates the relationships among family factors, including family functioning and family conflict, trauma (encompassing traumatic events experienced prior to, and after, becoming homeless), mental health problems, and externalizing behaviors among homeless adolescents. The authors begin with a review of previous research on homeless adolescents to determine how family factors, such as poor family functioning, and trauma are related to negative outcomes for homeless adolescents (Coates & McKenzie-Mohr, 2010; Edidin et al., 2012; Gwadz, Nish, Leonard, & Strauss, 2007; Toro & Goldstein, 2000).
Family Factors and Trauma, both Prior to and after Becoming Homeless
Consistent and longstanding conflict with parents and/or caregivers is one of the primary reported reasons adolescents leave their homes (Whitbeck & Hoyt, 1999). These conflicts are often related to relationships with step-parents or their parents’/caregivers’ partners, sexual activity, sexual orientation, substance use, and school problems (Robertson & Toro, 1999; Whitbeck & Hoyt, 1999). In addition to family conflict, many homeless adolescents have experienced traumatic events in their homes prior to becoming homeless, and report high rates of abuse and/or neglect from family members (Coates & McKenzie-Mohr, 2010; Gwadz et al., 2007; Toro & Goldstein, 2000; Zerger, Strehlow, & Gundlapalli, 2008). The rate of reported conflict and trauma among homeless adolescents is higher than their housed counterparts (Toro & Goldstein, 2000; Wolfe, Toro, & McCaskill, 1999).
Many homeless adolescents not only have experienced traumatic events in their homes and families, but also have reported non-familial abuse and neglect outside of their homes prior to becoming homeless (Gwadz et al., 2007; Robertson, 1989). Gwadz et al. (2007) found that 85.9% of a sample of homeless adolescents reported experiencing at least one traumatic event in their lives outside of their homes prior to becoming homeless. These experiences varied by gender, as female homeless adolescents were more likely to report emotional abuse and sexual abuse as traumatic events, while male homeless adolescents were more likely to report physical neglect (Gwadz et al., 2007). Many of these traumatic experiences are antecedents to adolescents becoming homeless (Coates & McKenzie-Mohr, 2010; Gwadz et al., 2007; Tyler & Bersani, 2008). Bender et al. (2010) found 57% of the homeless adolescents that they surveyed reported experiencing a traumatic event prior to their first episode of homelessness, and 24% met the DSM-IV diagnostic standard for post-traumatic stress disorder (PTSD). In addition, homelessness can intensify the subsequent effects of previous traumatic experiences and lead to subsequent traumas (Thompson, 2005), which can also result in negative mental health and behavioral outcomes among these adolescents.
Although considerable attention has been given to the trauma resulting from these traumatic events that occurred prior to their becoming homeless, less attention has been focused on how the experience of being homeless can exacerbate the previous traumatic experiences of these adolescents and create new traumas (Coates & McKenzie-Mohr, 2010; Hopper, Bassuk, & Olivet, 2010; Whitbeck et al., 1999). Being homeless has repeatedly been described as a traumatic event for a young person (Coates & McKenzie-Mohr, 2010; Hopper et al., 2010; Karabanow, 2008). Homeless adolescents are exposed on a daily basis to environments and situations that could potentially lead to trauma such as repeated moves, constantly seeking shelter and food, and interacting with strangers in unfamiliar environments where victimization can occur (Bender et al., 2010).
Mental Health Problems and Externalizing Behaviors
As a result of traumatic events, such adolescents often report an array of mental health concerns and risky externalizing behaviors (Ginzler et al., 2007; Salomonsen-Sautel et al., 2008; Van den Bree et al., 2009). Mental health issues are prevalent among homeless adolescents. Previous research on the mental health of homeless adolescents has found that 19% to 53% report mental health problems (Cauce et al., 1997; Feitel, Margetson, Chamas, & Lipman, 1992; McCaskill, Toro, & Wolfe, 1998; Mundy, Robertson, Greenblatt, & Robertson, 1989; Toro, Goldstein, & Rowland, 1998). Externalizing behaviors such as substance use, high-risk sexual behaviors and delinquency are also prevalent among homeless adolescents (Lombardo & Toro, 2004; Whitbeck et al., 1997; Whitbeck et al., 2001). Many of these externalizing behaviors, including substance use and high-risk sexual behaviors, co-occur with the identified mental health conditions seen in homeless adolescents (National Health Care for the Homeless Council, 2015).
Substance use has been investigated thoroughly among homeless adolescents. Homeless adolescents are more likely to report using substances compared to their housed counterparts (e.g., Schwartz, Sorensen, Ammerman, & Bard, 2008). Alcohol use is widespread: 57% to 70% of samples of homeless adolescents report current alcohol use, 52% report consuming five or more alcoholic drinks a week, and 38% report having 15 or more drinks per week (Halcon & Lifson, 2004; Rosenthal, Mallett, Milburn, & Rotheram-Borus, 2008; Van Leeuwen et al., 2004). Nationally, as many as 75% to 95% of homeless adolescents have reported using marijuana or other drugs (e.g., Halcon & Lifson, 2004; Van Leeuwen et al., 2004). Reported rates of injection drug use among samples of homeless adolescents range from 17% to 41% (e.g., Kerr et al., 2009; Marshall, Kerr, Qi, Montaner, & Wood, 2010; Rosenthal et al., 2008). Polysubstance use is also common among homeless adolescents: 25% reported using three to five drugs within the previous three months, and 26% reported using six or more drugs in that time period (Rosenthal et al., 2008). Strong associations also have been found between delinquency and substance use among homeless adolescents (Dashora, Erdem, & Slesnick, 2010).
In addition to substance use, high-risk sexual behaviors also are prevalent among homeless adolescents. Many studies have noted that homeless youth engage in a variety of high-risk sexual behaviors, including having unprotected sex with multiple people and survival sex, which involves trading sex for subsistence needs such as food, shelter, and/or drugs (e.g., Rew, Grady, Whittaker, & Bownman, 2008; Tevendale, Lightfoot, & Slocum, 2009). Further, substance use, in and of itself, is associated with high-risk sexual behaviors. Previous research has found that compared to their housed counterparts, substance-using homeless youth had more sexual partners and used condoms less often (Solorio et al., 2008). Both substance use and high-risk sexual behaviors pose serious threats to the healthy trajectory of these adolescents into adulthood. High-risk sexual behaviors increase risk for life-impacting sexually transmitted illnesses such as human immunodeficiency virus (HIV). Homeless youth are 6 to 12 times more likely to become infected with HIV than housed youth (Ray, 2006; Rotheram-Borus, Becker, Koopman, & Kaplan, 1991). The HIV rate in this population is significantly higher than the prevalence in the general U.S. adolescent population (Centers for Disease Control, 2012).
Family factors are strongly linked to these mental health problems and externalizing behaviors among homeless adolescents (Solorio et al., 2008). For example, family abuse among homeless adolescents has been positively related to reports of depressive symptoms, lack of family support, and deviant peer affiliation (Bao, Whitbeck, & Hoyt, 2000). In addition, previous research has found that adolescents who leave home due to abuse or violence are more likely to become involved in delinquent behaviors (Stein, Milburn, Zane, & Rotheram-Borus, 2009). Specifically, poor relationships with their fathers or male guardians increased the likelihood of engaging in delinquent behaviors, while poor relationships with their mothers or female guardians increased the likelihood of engaging in survival sex behaviors (Stein et al., 2009). Lastly, parental violence has been found to also be a significant, positive predictor of alcohol problems among homeless adolescents (Haber & Toro, 2009).
Current Study
Previous research shows that family factors and trauma are related to negative outcomes for homeless adolescents (e.g., Coates & McKenzie-Mohr, 2010; Hopper et al., 2010; Whitbeck & Hoyt, 1999). It does not, however, provide a clear understanding of how family factors and trauma together can exacerbate the adolescents’ mental health problems and externalizing behaviors. The simultaneous influence of family factors and trauma on mental health problems and externalizing behaviors in the lives of homeless adolescents has not been examined in published research to date. Therefore, this study investigates the relationships among family factors, including poor family functioning and family conflict, trauma (experienced prior to and after becoming homeless), and their simultaneous influence on mental health concerns and externalizing behaviors among homeless adolescents. Understanding these linkages may lead to better intervention strategies for addressing the mental health and behavioral problems of homeless adolescents to prevent their trajectory into chronic adult homelessness, thus improving their chances of having a healthy transition into adulthood.
Structural equation models with latent variables (SEM; Bentler, 2006) were used to investigate associations among measures of trauma experienced prior to and after becoming homeless, poor family functioning, and family conflict, and in turn, assess their influence on recently identified mental health conditions and externalizing behaviors (substance use, delinquent behaviors, and high-risk sexual behaviors). Age was included as another predictor. The authors hypothesized that both poor family functioning and family conflict, as well as trauma, would be significantly associated with increased mental health issues and externalizing behaviors. The authors also hypothesized that being an older adolescent would predict mental health problems and externalizing behaviors on the basis of developmental expectations over time (i.e., high-risk sexual behaviors occur more frequently as young people age).
Methods
Participants
During the period of March 2006 through August 2008, baseline data were collected for a randomized controlled trial of a family intervention for newly homeless adolescents. Eligibility criteria for the study included being 12 to 17 years old, being away from home for less than six months, and having the potential to return home to live. Adolescents in Los Angeles and San Bernardino counties were recruited through community organizations such as shelters or schools, or through flyers and advertisements. If an adolescent expressed interest in the study, an attempt was made to obtain written informed consent from the adolescent and his/her parent/guardian. If both the adolescent and adult provided this consent, they were asked to complete baseline assessments, and those families completing both assessments were randomized into the study. The study and all consent and assent procedures were approved by the University of California Los Angeles Institutional Review Board. For several months after recruitment into the intervention was closed (through December 2008), additional adolescents were recruited solely to complete baseline assessments without attempting to engage a parent or guardian. In the intervention phase of the study, 442 adolescents indicated initial interest. Of those, 219 (50%) completed the consent process and were baselined. After removing those with missing data on analysis variables, the resultant sample contained 201 homeless adolescents. Their baseline assessments provide the data analyzed in this research.
Measures
To avoid too many indicators for the size of the sample in SEM, individual items were randomly combined into parcels to obtain mean indicators in some cases (Little, Cunningham, Shahar, & Widaman, 2002). Indicators of the latent variables are described below.
Demographic
A single-item variable represented an adolescent’s age in years.
Trauma
The UCLA Post-Traumatic Stress Disorder (PTSD) Index for DSM-IV was used to assess trauma symptoms (Rodriguez, Steinberg, & Pynoos, 1999; Steinberg, Brymer, Decker, & Pynoos, 2004). Three items were constructed to be used as latent variables in the path analyses that are described below. The first was a count of the number of stressful events reported by the adolescent, such as seeing someone beaten up, shot or killed; this variable ranged from 0 to 10. The second was an average of their endorsement of 13 items assessing their feelings of fear, confusion, and upset at the most stressful experience they reported; each item was scaled as yes = 1 or no = 0 (coefficient alpha = .87). The last was an average of their endorsement of 22 symptoms such as intrusive thoughts, arousal, re-experiencing, or avoidance. These items were on a 0 to 4 scale where none = 0 and most = 4 (coefficient alpha = .95).
Poor Family Functioning
Family functioning was assessed using six subscales of the Family Functioning measure (Bloom, 1985; Bloom & Naar, 1994): cohesion, expressiveness, disengagement, democratic family style, laissez-faire family style, and authoritarian family style. This measure was adapted from four frequently-used, established measures of family functioning: the Family Environment Scale (Moos & Moos, 1994), Family-Concept Q Sort (Van der Veen & Novak, 1971), Family Adaptability and Cohesion Evaluation Scale (Olson, Bell, & Portner, 1982), and the Family Assessment Measure (Skinner, Steinhauer, & Santa-Barbara, 1983; Skinner, Steinhauer, & Sitarenios, 2000). The Family Functioning measure has demonstrated good internal reliability consistency (Loveland-Cherry, Youngblut, & Leidy, 1989; Roosa & Beals, 1990) and discriminant validity (Nash, Hulsey, Sexton, Harralson, & Lambert, 1993; Stark, Humphrey, Crook, & Lewis, 1990).
Three parcels were created randomly from the means of the items as indicators of a family function latent variable (coefficient alpha for the 35 items = .85). Items ranged from 1 to 4 from “very untrue for my family” to “very true for my family” and items were reverse-coded as necessary to make higher scores indicate poor family functioning.
Family Conflict
Family conflict was ascertained from the Conflict subscale of the Family Functioning measure. Ten items were scaled in the negative direction; item values ranged from rarely (1) to all of the time (4). Examples include: “You insulted or swore at him” and “You sulked and refused to talk about it.” The coefficient alpha was high (.86) and items were combined at random to create three parcels indicating the factor.
Mental Health Problems
Mental health problems were ascertained through the 53-item Brief Symptom Inventory (BSI) (Derogatis, 1975, 1993), a shortened version of the SCL-90 (Derogatis, 1992) that is designed to assess symptoms of mental health problems. The Global Symptom Inventory (GSI), the mean score across all items of the BSI, was used for simplicity; high coefficient alpha scores have been obtained using this measure with an analogous population (.96; Yuan, Bentler, & Kano, 1997) with ratings ranging from 1 (not at all) to 5 (extremely). Higher scores indicated increased symptoms of mental health conditions. Adolescents were asked whether the symptom (e.g., “nervousness or shakiness inside”, “thoughts of ending your life”) had bothered them during the past week including today.
Delinquent Behaviors
Delinquent behaviors, defined using the DSM-IV-TR (American Psychiatric Association, 2000) diagnostic criteria for conduct disorder, were measured by a count of conduct problems exhibited during the prior three months (Rotheram-Borus, Rosario, Van Rossem, Reid, & Gillis, 1995). Thirteen items queried whether an adolescent had ever participated in various actions such as physical cruelty that caused pain, starting a physical fight, using a weapon, stealing, or setting fires. Items were scaled as no (0) and yes (1). The items were randomly combined to create three mean indicators (coefficient alpha = .74).
High-Risk Sexual Behaviors
High-risk sexual behaviors were assessed with 4 items: 1) the square root of the number of sex partners they had in the past three months; 2) whether they had ever had sex while drinking or taking drugs (yes = 1, no = 0); 3) whether they drank alcohol or used drugs before having sexual intercourse the last time; and 4) a sum of 12 various high-risk sexual behaviors such as vaginal, anal, or oral sex with anyone who injected drugs, anyone whose sexual history they did not know very well, or anyone with HIV or AIDS (coefficient alpha = .73).
Substance use
A substance use latent variable was indicated with 3 items: 1) the average score on the 27-item Drug Abuse Screening Test (DAST) (Skinner, 1982), scored dichotomously (yes = 1, no =0; coefficient alpha = .93); 2) the average score on the 24-item Michigan Alcoholism Screening Test (MAST; Selzer, 1971), scored dichotomously (yes = 1, no = 0; coefficient alpha = .88); and 3) based on lifetime use of fifteen substances, such as marijuana, cocaine or crack, or amphetamines (coefficient alpha = .82). This variable ranged from 0 to 13 with a modal response of 3 and a mean of 2.95.
Analysis
Latent variable analyses were performed using the EQS structural equations program (Bentler, 2006). Goodness-of-fit was assessed with the maximum-likelihood χ2 statistic (ML χ2), the Comparative Fit Index (CFI), the Satorra-Bentler χ2 (S-B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA) (Bentler, 2006; Hu & Bentler, 1999). An initial confirmatory factor analysis (CFA) assessed the adequacy of the hypothesized measurement model and provided the associations among the latent variables as well as the demographic variable of age. The authors then tested a predictive path model that positioned the variables of age, trauma, poor family functioning, and family conflict as predictors of mental health problems and externalizing behaviors. Relationships that were significant among the predictor variables also were retained in this model, as correlations and significant correlations among the error residuals of the outcome variables were also allowed. Non-significant paths and correlations in this model were trimmed gradually following the recommended model-evaluation procedure of MacCallum (1986). Suggestions from the LaGrange Multiplier test, which reports supplementary modifications to the original model that will improve the fit, were evaluated and were allowed only if deemed appropriate theoretically and logically (LM test; Chou & Bentler, 1990).
Results
Sample
The average age of the adolescents was 15 years old (range = 12 to 18 years). Nearly two-thirds (64%) were male. Sixty-three percent of the sample was Hispanic/Latino, 12% was White, 19% was African-American, 1% was Asian/Pacific Islander, and 5% reported themselves as mixed race/ethnicity.
Confirmatory Factor Analysis
The initial CFA had an excellent fit Table 1
All hypothesized factor loadings were significant (p ≤ .001). Table 1 presents the factor loadings, means, and standard deviations of the measured variables. Table 2 reports the correlations among age and all of the latent variables in the CFA. Only 1 supplementary association was added to the measurement model, a covariance between error residuals of mental distress and delinquent behaviors (standardized r = .39).
As hypothesized, being older was associated with more high-risk sexual behaviors and drug and alcohol use
Trauma was modestly associated with being a younger homeless adolescent. The three delinquent behaviors variables were highly intercorrelated and summed as a single delinquent-behaviors variable for easier viewing in Table 2. Mental health problems were correlated with trauma and the family factors variables. Poor family functioning was significantly associated with family conflict, as well as with the externalizing behaviors.
Path Analysis
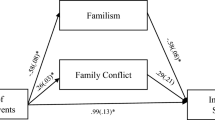
Figure 1 presents the final trimmed path model in which age, trauma, poor family functioning, and family conflict predicted mental health problems, delinquent behaviors, high-risk sexual behaviors and substance use. This model has excellent fit statistics. The model explained 21% of the variance in mental health problems, 17% of the variance in delinquent behaviors, 22% of the variance in high-risk sexual behaviors, and 19% of the variance in substance use.
Path model testing influence of demographics, trauma, and family factors on mental health problems and externalizing behaviors among homeless adolescents (N = 201). Latent constructs are in circles, single items are in rectangles; 1-headed arrows depict standardized regression paths, 2-headed arrows represent correlations (standardized covariances; * = p ≤ .05, ** = p ≤ .01, *** = p ≤ .001). Fit statistics: ML χ2 = 249.29, 173 df, CFI = .95, RMSEA = .047); S-B χ2 = 217.65, 173 df; RCFI = .96, RMSEA = .036
Mental health problems and delinquent behaviors both were predicted by greater trauma as well as by the family conflict and poor family functioning variables. High-risk sexual behaviors were predicted by being older, poor family functioning, and greater family conflict. Substance use was predicted by being older and greater family conflict. As was seen in the bivariate correlations, being a younger adolescent was associated with higher trauma scores and poor family functioning was significantly associated with greater family conflict. Trauma, family conflict, and poor family functioning variables were not significantly associated with each other. The error residuals of the externalizing behaviors were all intercorrelated and the error residual of mental health problems was only significantly associated with the error residual of delinquent behaviors.
Discussion
Previous research on homeless adolescents has demonstrated that trauma is present in the lives of many of these young people (Bender et al., 2010; Coates & McKenzie-Mohr, 2010; Edidin et al., 2012; Van den Bree et al., 2009). Moreover, family conflict and poor family functioning are often linked to their homelessness (Coates & McKenzie-Mohr, 2010; Edidin et al., 2012; Gwadz et al., 2007; Toro & Goldstein, 2000; Whitbeck & Hoyt, 1999; Zerger et al., 2008). The purpose of this research was to examine how homeless adolescents’ experiences of family conflict, poor family functioning, and traumatic events that occurred prior to and after they became homeless were associated with mental health problems and externalizing behaviors. Traumatic events identified for consideration in this study included events such as ‘seeing someone beaten up, shot or killed’; ‘hearing about the violent death or serious injury of a loved one’; and ‘being beaten up, shot or threatened to be hurt.’ Prior studies of homeless adolescents had not examined these constructs simultaneously to assess their relative impact (Edidin et al., 2012).
In general, both trauma and family factors were found to be related to externalizing behaviors. This can be seen in both the bivariate associations and also in the path model. Trauma was significantly associated with mental health problems and delinquent behaviors but was not significantly associated with either high-risk sexual behaviors or substance use. Both poor family functioning and family conflict were significantly associated with these externalizing behaviors, as well as mental health problems and delinquent behaviors, in the bivariate analysis. In the path analysis, poor family functioning predicted more mental health problems, delinquent behaviors, and high-risk sexual behaviors, and family conflict predicted higher levels of all of the outcome variables including substance use.
These analyses also revealed an interesting association between trauma and delinquent behaviors. Clearly, the role of trauma should be considered in interventions that address delinquent behaviors among homeless adolescents. What contributes to this relationship remains to be determined in future research. One explanation for this relationship is that trauma resulting from exposure to violence (e.g., Coates & McKenzie-Mohr, 2010) may be related to delinquent behaviors. Research suggests that for homeless adolescents, distal traumatic events, such as violence in their neighborhoods of origin, may be even more salient predictors of trauma than recent events in their lives, such as homelessness experiences (Whitbeck & Hoyt, 1999; Whitbeck, Hoyt, Johnson, & Chen, 2007).
Poor family functioning was found to be associated with family conflict and all but one externalizing behavior—substance use. Although the authors examined family conflict as a possible predictor of mental health problems and externalizing behaviors, externalizing behaviors may have led to more family conflict as well. Poor family functioning appears likely to contribute to externalizing behaviors as well as mental health problems.
Whitbeck et al. (2007) found that among homeless adolescents, older adolescents had higher rates of lifetime trauma than younger adolescents. As in prior research, older homeless adolescents in this study reported more high-risk sexual behaviors and substance use than younger homeless adolescents.
One surprising finding is that there were no observed gender differences in externalizing behaviors as previously found in other research. In this sample, female and male adolescents were equally at risk as they reported engaging in similar rates of high-risk sexual behaviors and substance use. The authors also found no gender differences in rates of trauma; however, this is consistent with the findings of others (Stewart et al., 2004; Whitbeck & Hoyt, 1999). There also were substantial relationships among the externalizing behaviors and robust predictors of these behaviors. Overall rates of high-risk sexual behaviors and substance use were surprisingly low compared to some other studies. Bender et al. (2010) found that 45.7% of the homeless adolescents in their sample met criteria for drug addiction as well as for alcohol addiction. Rates were lower for those participants who had trauma. The adolescents in this sample were more recently homeless, so perhaps they had not yet become chronically homeless and part of a street culture where alcohol and drug abuse are common.
Multiple age differences were found in this sample; being an older adolescent was associated with higher rates of high-risk sexual behaviors and substance use. This finding is consistent with other research on homeless adolescents that found older homeless adolescents are more likely to report substance use and risky survival sex behaviors (e.g., trading sex for a place to stay; Stein et al., 2009). Unfortunately, high-risk sexual behaviors may lead adolescents to be further victimized on the streets either as an adolescent or later as an adult.
While this research contributes to the small body of literature on trauma among homeless youth, the authors must acknowledge several limitations. Given that this study is cross-sectional, the finding of the association between mental health problems and trauma—while exactly what one would expect from clinical experience and practice—should still be interpreted with some caution. Causality cannot be fully established as the temporal order of the variables that were assessed is not known. In particular, the timing of the traumatic events that may have led to the adolescents’ trauma symptoms is not known. Longitudinal studies of homeless adolescents are needed to more fully understand the sequela of events that may lead to the development of trauma among homeless adolescents. Without these data, we are limited in our ability to develop appropriate and effective treatment options to address the trauma experienced by these young people.
Nonetheless, in addition to the findings on the relationship of trauma to mental health problems and externalizing behaviors, these findings, overall, suggest that family factors appear to be critical to understanding mental health problems and externalizing behaviors among homeless adolescents. This research is one of the few existing studies that examines the possible impact of family factors on trauma and the mental health of homeless adolescents. Even when these family factors are in the past, this study suggests that they still need to be addressed as part of any comprehensive assessment when homeless adolescents are screened for mental health treatment and services. Expanded screening that also assesses trauma and identifies the source of the trauma and the nature of family relationships could assist clinicians and caseworkers in making more informed decisions about when and how to intervene to reunite a homeless youth with his/her family.
Family factors should also be targeted in family-based interventions for homeless adolescents, given the protective function that positive family relationships can provide (Milburn et al., 2005; Stein et al., 2009). Reconnecting homeless adolescents to caring adults is also one of the goals of the federal policy to end adolescent homelessness (United States Interagency Council on Homelessness, 2016; Office of Disease Prevention and Health Promotion, 2014). Reconnections and opportunities for positive engagement should occur when the family is capable of welcoming the adolescent back into the home. This process might include psychotherapy and other services for multiple family members rather than interventions aimed only at the adolescent. Individual, social and political efforts should focus on keeping families together and connected with each other in a healthy pro-social way.
To conclude, these findings provide support for the adaptation and development of family-centered interventions for homeless adolescents that are informed by family factors, trauma, and mental health. Such interventions may provide trauma-informed approaches for homeless adolescents and their family members to rebuild connections and improve communication to reduce mental health problems and externalizing behaviors. As an example, family-centered trauma interventions, such as those in the SAMHSA Homeless Families Programs (e.g., Trauma Adaptive Recovery Group Education and Therapy; Trauma Recovery and Empowerment, and Addiction and Trauma Recovery Integration Model) may be appropriate to address both individual and familial trauma among homeless adolescents with family conflict (SAMHSA Homeless Families Coordinating Center, 2005). There are also preventative interventions that could be adapted for homeless adolescents to deter further trauma and the development of PTSD. One example of this type of intervention is the UCLA Families OverComing Under Stress (FOCUS) model, an evidence-based, family-centered, trauma-informed, psychoeducational preventive intervention that has been widely used with military families. FOCUS is designed to promote individual and family resilience and reduce psychological distress in families (Lester et al., 2011). While supporting the development of family-centered interventions such as those mentioned here, this study also highlights further the need for services aimed at homeless youth to be trauma-informed, germane to individual mental health needs, and delinquency prevention-focused. Regardless of the program or intervention utilized to target this population, however, the results of this study indicate the need for further ongoing research into the lives and experiences of homeless adolescents and their families, in order to avoid the oft-times inevitable trajectory into adult homelessness, criminality, and/or serious mental illness.
References
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: Author.
American Psychological Association (APA). (2009). Presidential Task Force on Psychology’s contribution to end homelessness. Helping People without Homes. Washington, DC: American Psychological Association.
Bao, W. N., Whitbeck, L. B., & Hoyt, D. R. (2000). Abuse, support, and depression among homeless and runaway adolescents. Journal of Health and Social Behavior, 41, 408–420.
Bender, K., Ferguson, K., Thompson, S., Komlo, C., & Pollio, D. (2010). Factors associated with trauma and posttraumatic stress disorder among homeless youth in three U.S. cities: The importance of transience. Journal of Traumatic Stress, 23, 161–168.
Bentler, P. M. (2006). EQS 6 structural equations program manual. Encino: Multivariate Software, Inc..
Bloom, B. L. (1985). A factor analysis of self-report measures of family functioning. Family Process, 24, 225–239.
Bloom, B. L., & Naar, S. (1994). Self-report measures of family functioning: Extensions of a factorial analysis. Family Process, 33, 203–216.
Cauce, A. M., Paradise, M., Embry, L., Morgan, C., Lohr, Y., Theofelis, J., Sy, J., & Wagner, V. (1997). Homeless youth in Seattle: Youth characteristics, mental health needs, and intensive case management. Unpublished manuscript, Department of Psychology, University of Washington.
Centers for Disease Control and Prevention (CDC). (2012). HIV surveillance report 2010: Diagnoses of HIV infection and AIDS in the United States and dependent areas. Atlanta, Georgia: U.S. Department of Health and Human Services. Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/.
Chou, C. P., & Bentler, P. M. (1990). Model modification in covariance structure modeling: A comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behavioral Research, 25, 115–136.
Clark, R., & Robertson, M. J. (1996). Surviving for the moment: A report on homeless youth in San Francisco. Berkeley: Alcohol Research Group.
Coates, J., & McKenzie-Mohr, S. (2010). Out of the frying pan, into the fire: Trauma in the lives of homeless youth prior to and during homelessness. Journal of Sociology & Social Welfare, 37, 65–98.
Dashora, P., Erdem, G., & Slesnick, N. (2010). Better to bend than break: Coping strategies utilized by substance abusing homeless youth. Journal of Health Psychology, 16(1), 158–168.
Derogatis, L.R. (1975). Brief symptom inventory. Baltimore: Clinical Psychometric Research. Minneapolis.
Derogatis, L. R. (1992). SCL-90-R, administration, scoring & procedures manual-II for the revised) version and other instruments of the psychopathology rating scale series. Townson: Clinical Psychometric Research, Inc.
Derogatis, L. R. (1993). Brief symptom inventory (BSI): Administration, scoring, and procedures manual (3rd ed.). Minneapolis: National Computer Systems.
Edidin, J. P., Ganim, Z., Hunter, S. J., & Karnik, N. S. (2012). The mental and physical health of homeless youth: A literature review. Child Psychiatry and Human Development, 43(3), 354–375.
Feitel, B., Margetson, N., Chamas, R., & Lipman, C. (1992). Psychosocial background and behavioral and emotional disorders of homeless and runaway youth. Hospital & Community Psychiatry, 43(2), 155–159.
Fowler, P. J., Toro, P. A., & Miles, B. W. (2009). Pathways to and from homelessness and associated psychosocial outcomes among adolescents leaving the foster care system. nashAmerican. Journal of Public Health, 99(8), 1453–1458. doi:10.2105/AJPH.2008.142547.
Ginzler, J. A., Garrett, S. B., Baer, J. S., & Peterson, P. L. (2007). Measurement of negative consequences of substance use in street youth: An expanded use of the Rutgers alcohol problem index. Addictive Behaviors, 32(7), 1519–1525.
Gwadz, M., Nish, D., Leonard, N., & Strauss, S. (2007). Gender differences in traumatic events and rates of post-traumatic stress disorder among homeless youth. Journal of Adolescence, 30, 117–129.
Haber, M., & Toro, P. A. (2004). Homelessness among families, children and adolescents: An ecological-developmental perspective. Clinical Child and Family Psychology Review, 7, 123–164.
Haber, M., & Toro, P. A. (2009). Parent-adolescent violence and later behavioral health problems among homeless and housed youth. American Journal of Orthopsychiatry, 79, 305–318.
Halcon, L. L., & Lifson, A. R. (2004). Prevalence and predictors of sexual risks among homeless youth. Journal of Youth and Adolescence, 33(1), 71–80.
Hopper, E., Bassuk, E., & Olivet, J. (2010). Shelter from the storm: Trauma-informed care in homelessness service settings. The Open Health Services and Policy Journal, 3, 80–100.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
Karabanow, J. (2008). Getting off the street: Exploring young people’s street exits. American Behavioral Scientist, 51, 772–788.
Kelly, K., & Caputo, T. (2007). Health and street/homeless youth. Journal of Health Psychology, 12(5), 726–736.
Kerr, T., Marshall, B. D., Miller, C., Shannon, K., Zhang, R., Montaner, J. S., & Wood, E. (2009). Injection drug use among street-involved youth in a Canadian setting. BioMed Central Public Health, 9, 171–177.
Lester, P., Mogil, C., Saltzman, W., Woodward, K., Nash, W., Leskin, G., Bursh, B., Green, S., Pynoos, R., & Beardslee, W. R. (2011). FOCUS (families OverComing under stress): Implementing family centered prevention for military families facing wartime deployments and combat operational stress. Military Medicine, 176(1), 19–25.
Little, T. D., Cunningham, W. A., Shahar, G., & Widaman, K. F. (2002). To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling, 9, 151–173.
Lombardo, S., & Toro, P. A. (2004). Risky sexual behaviors and substance abuse among homeless and other at-risk adolescents. Unpublished manuscript, Department of Psychology, Wayne State University, Detroit, MI.
Loveland-Cherry, C. J., Youngblut, J. M., & Leidy, N. W. (1989). A psychometric analysis of the family environment scale. Nursing Research, 38, 262–266.
MacCallum, R. (1986). Specification searches in covariance structure modeling. Psychological Bulletin, 100, 107–120.
Marshall, B. D., Kerr, T., Qi, J., Montaner, J. S., & Wood, E. (2010). Public injecting and HIV risk behavior among street-involved youth. Drug and Alcohol Dependence, 110(3), 254–258.
McCaskill, P. A., Toro, P. A., & Wolfe, S. M. (1998). Homeless and matched housed adolescents: A Comparative study of psychopathology. Journal of Clinical Child Psychology, 27, 306–319.
Merscham, C., Van Leeuwen, J. M., & McGuire, M. (2009). Mental health and substance abuse indicators among homeless youth in Denver, Colorado. Child Welfare, 88(2), 93–110.
Milburn, N. G., Rotheram-Borus, M. J., Batterham, P., Brumback, B., Rosenthal, D., & Mallett, S. (2005). Predictors of close family relationships over one year among homeless young people. Journal of Adolescents, 28, 263–275.
Moos, R. H., & Moos, B. S. (1994). Family environment scale manual (3rd ed.). Palo Alto: Consulting Psychologists Press.
Mundy, P., Robertson, J. M., Greenblatt, M., & Robertson, M. J. (1989). Residential instability in adolescent psychiatric inpatients. Journal of the American Academy of Adolescent and Child Psychiatry, 28, 176–181.
Nash, M. R., Hulsey, T. L., Sexton, M. C., Harralson, T. L., & Lambert, W. (1993). Long-term sequelae of childhood sexual abuse: Perceived family environment, psychopathology, and dissociation. Journal of Consulting and Clinical Psychology, 61, 276–283.
National Alliance to End Homelessness (2014). An emerging framework for ending unaccompanied youth homelessness. Washington, DC.
National Health Care for the Homeless Council (2015). Behavioral health among youth experiencing homelessness: A quarterly research review of the National HCH Council, 3:4. Nashville, TN. https://www.nhchc.org/wp-content/uploads/2011/09/in-focus-behavioral-health-among-youth.pdf.
Office of Disease Prevention and Health Promotion. (2014). Healthy people 2020. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
Olson, D.H., Bell, R.Q., & Portner, J. (1982). FACES II: Family adaptability and cohesion evaluation scales. St. Paul: Family Social Science, University of St. Paul, Minnesota.
Parks, R. W., Stevens, R. J., & Spence, S. A. (2007). A systematic review of cognition in homeless children and adolescents. Journal of the Royal Society of Medicine, 100(1), 46–50.
Ray, N. (2006). Lesbian, gay, bisexual and transgender youth: An epidemic of homelessness. New York: National Gay and Lesbian Task Force Policy Institute and the National Coalition for the Homeless.
Rew, L., Grady, M., Whittaker, T. A., & Bownman, K. (2008). Interaction of duration of homelessness and gender on adolescent sexual health indicators. Journal of Nursing Scholarship, 40(2), 109–115.
Robertson, M. J. (1989). Homeless Youth in Hollywood: Patterns of Alcohol Use. A report to the National Institute on Alcohol Abuse and Alcoholism (report no. C51). Berkeley: Alcohol research group.
Robertson, M. J., & Toro, P. A. (1999). Homeless youth: Research, intervention, and policy. In L. B. Fosburg & D. L. Dennis (Eds.), Practical lessons: The 1998 National Symposium on Homelessness Research (pp. 3–1–3-32). Washington DC: U.S. Department of Housing and Urban Development and U.S. Department of Health and Human Services.
Rodriguez, N., Steinberg, A., & Pynoos, R. S. (1999). UCLA PTSD index for DSM-IV instrument information: Child version, parent version, adolescent version: Los Angeles: UCLA trauma Psychiatry services.
Roosa, M. W., & Beals, J. (1990). Measurement issues in family assessment: The case of the family environment scale. Family Process, 29, 191–198.
Rosenthal, D. A., Mallett, S., Milburn, N., & Rotheram-Borus, M. J. (2008). Drug use among homeless young people in Los Angeles and Melbourne. Society for Adolescent Medicine, 43(3), 296–305.
Rotheram-Borus, M. J., Becker, J. V., Koopman, C., & Kaplan, M. (1991). AIDS knowledge and beliefs, and sexual behavior of sexually delinquent and non-delinquent (runaway) adolescents. Journal of Adolescence, 14, 229–244.
Rotheram-Borus, M. J., Rosario, M., Van Rossem, R., Reid, H., & Gillis, J. R. (1995). Prevalence, course, and predictors of multiple problem behaviors among gay and bisexual male adolescents. Developmental Psychology, 31(1), 75–85.
Salomonsen-Sautel, S., Van Leeuwen, J. M., Gilroy, C., Boyle, S., Malberg, D., & Hopfer, C. (2008). Correlates of substance usage among homeless youth in eight cities. The American Journal of Addiction, 17, 224–234.
SAMHSA Homeless Families Coordinating Center. (2005). Trauma interventions for homeless families—Innovative features and common themes. Washington, DC: Vanderbilt University Center for Evaluation and Program Improvement.
Schwartz, M., Sorensen, H. K., Ammerman, S., & Bard, E. (2008). Exploring the relationship between homelessness and delinquency: A snapshot of a group of homeless youth in San Jose, California. Child and Adolescent Social Work Journal, 25(4), 255–269.
Selzer, M. L. (1971). The Michigan Alcoholism screening test (MAST): The quest for a new diagnostic instrument. American Journal of Psychiatry, 3, 176–181.
Skinner, H. A. (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371.
Skinner, H. A., Steinhauer, P. D., & Santa-Barbara, J. (1983). The family assessment measure. Canadian Journal of Community Mental Health, 2, 91–105.
Skinner, H. A., Steinhauer, P. D., & Sitarenios, G. (2000). Family assessment measure (FAM) and process model of family functioning. Journal of Family Therapy, 22(2), 190–210.
Solorio, R. M., Rosenthal, D., Milburn, N. G., Weiss, R. E., Batterham, P. J., Gandura, M., & Rotheram-Borus, M. (2008). Predictors of sexual risk behaviors among newly homeless youth: A longitudinal study. Journal of Adolescent Health, 42, 401–409.
Stark, K. D., Humphrey, L. L., Crook, K., & Lewis, K. (1990). Perceived family environments of depressed and anxious children: Child’s and maternal figure’s perspectives. Journal of Abnormal Child Psychology, 18, 527–547.
Stein, J. A., Milburn, N. G., Zane, J. I., & Rotheram-Borus, M. J. (2009). Paternal and maternal influences on problem behaviors among homeless and runaway youth. American Journal of Orthopsychiatry, 79(1), 39–50.
Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6, 96–100.
Stewart, A. J., Steiman, M., Cauce, A. M., Cochran, B. N., Whitbeck, L. B., & Hoyt, D. R. (2004). Victimization and posttraumatic stress disorder among homeless adolescents. Journal of the Academy of Child & Adolescent Psychiatry, 43, 325–331.
Substance Abuse and Mental Health Services Administration [SAMHSA]. (2010). Current statistics on the prevalence and characteristics of people experiencing homelessness in the United States. Rockville: Homelessness Resource Center.
Tevendale, H. D., Lightfoot, M., & Slocum, S. L. (2009). Individual and environmental protective factors for risky sexual behavior among homeless youth: An exploration of gender differences. AIDS and Behavior, 13(1), 154–164.
Thompson, S. J. (2005). Factors associated with trauma symptoms among runaway/homeless adolescents. Stress, Trauma and Crisis: An International Journal, 8, 143–156.
Toro, P.A., Dworsky, A., & Fowler, P. J. (2007). Homeless youth in the United States: Recent research findings and intervention approaches. In D. Dennis, G. Locke, & J. Khadduri (Eds.), Towards understanding homelessness: The 2007 National Symposium on Homelessness Research (pp. 6-1–6-33). Washington, DC: USDHHS.
Toro, P. A., & Goldstein, M. S. (2000). Outcomes among homeless and matched housed adolescents: A longitudinal comparison. In Presented at the 108th annual convention of the American Psychological Association. Washington: DC.
Toro, P. A., Goldstein, M. A., & Rowland, L. L. (1998). Preliminary analyses: Housing, adolescence and life outcomes (HALO) project. Wayne State University, Department of Psychology (research funded by the National Institute on Alcohol Abuse and Alcoholism).
Toro, P. A., Hobden, K. L., Durham, K. W., Oko-Riebau, M., & Bokszczanin, A. (2014). Comparing the characteristics of homeless adults in Poland and the United States. American Journal of Community Psychology, 53(1–2), 134–145.
Tyler, K. A., & Bersani, B. E. (2008). A longitudinal study of early adolescent precursors to running away. Journal of Early Adolescents, 28(2), 230–251.
United States Interagency Council on Homelessness (2016). The president’s 2016 budget: Fact sheet on homelessness assistance. Washington, D.C. United States Interagency Council on Homelessness. Retrieved from http://usich.gov/resources/uploads/asset_library/2016_Budget_Fact_Sheet_on_Homelessness_Assistance.pdf.
Van den Bree, M., Shelton, K., Bonner, A., Moss, S., Thomas, H., & Taylor, P. J. (2009). A longitudinal population-based study of factors in adolescence predicting homelessness in young adulthood. Journal of Adolescent Health, 45, 571–578.
Van der Veen, F., & Novak, A. L. (1971). Perceived parental attitudes and family concepts of disturbed adolescents, normal siblings, and normal controls. Family Process, 10, 327–343.
Van Leeuwen, J. M., Hopfer, C., Hooks, S., White, R., Petersen, J., & Pirkopf, J. (2004). A snapshot of substance abuse among homeless and runaway youth in Denver, Colorado. Journal of Community Health, 29(3), 217–229.
Whitbeck, L. B., & Hoyt, D. R. (1999). Nowhere to grow: Homeless and runaway adolescents and their families. New York: Walter de Gruyter, Inc..
Whitbeck, L. B., Hoyt, D. R., & Ackley, K. A. (1997). Abusive family backgrounds and victimization among runaway and homeless adolescents. Journal of Research on Adolescence, 7, 375–392.
Whitbeck, L. B., Hoyt, D. R., Johnson, K. D., & Chen, X. (2007). Victimization and posttraumatic stress disorder among runaway and homeless adolescents. Violence and Victims, 22, 721–734.
Whitbeck, L. B., Hoyt, D. R., & Yoder, K. A. (1999). A risk-amplification model of victimization and depressive symptoms among runaway and homeless adolescents. American Journal of Community Psychology, 27(2), 273–296.
Whitbeck, L. B., Hoyt, D. R., Yoder, K. A., Cauce, A. M., & Paradise, M. (2001). Deviant behavior and victimization among homeless and runaway adolescents. Journal of Interpersonal Violence, 16(11), 1175–1204.
Wolfe, S. M., Toro, P. A., & McCaskill, P. A. (1999). A comparison of homeless and matched housed adolescents on family environment variables. Journal of Research on Adolescence, 9, 53–66.
Yu, M., North, C., LaVesser, P., Osborne, V., & Spitznagel, E. (2008). A comparison study of psychiatric and behavior disorders and cognitive ability among homeless and housed children. Community Mental Health Journal, 44(1), 1–11.
Yuan, K.-H., Bentler, P. M., & Kano, Y. (1997). On averaging variables in a confirmatory factor analysis model. Behaviormetrika, 24, 71–83.
Zerger, S., Strehlow, A. J., & Gundlapalli, A. V. (2008). Homeless young adults and behavioral health: An overview. American Behavioral Scientist, 51, 824–841.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milburn, N.G., Stein, J.A., Lopez, S.A. et al. Trauma, Family Factors and the Mental Health of Homeless Adolescents. Journ Child Adol Trauma 12, 37–47 (2019). https://doi.org/10.1007/s40653-017-0157-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40653-017-0157-9