Abstract
Background
Chronic kidney disease (CKD) progression is associated with significant comorbidities and costs. In Italy, limited evidence of healthcare resource consumption and costs is available. We therefore aimed to investigate the direct healthcare costs in charge to the Lombardy Regional Health Service (RHS) for the treatment of CKD patients in the first year after starting hemodialysis and in the 2 years prior to dialysis.
Methods
Citizens resident in the Lombardy Region (Italy) who initiated dialysis in the year 2011 (Jan 1 to Dec 31) were selected and data were extracted from Lombardy Regional databases on their direct healthcare costs in the first year after starting dialysis and in the 2 years prior to it was analyzed. Drugs, hospitalizations, diagnostic procedures and outpatient costs covered by RHS were estimated. Patients treated for acute kidney injury, or who died or stopped dialysis during the observational period were excluded.
Results
From the regional population (>9,700,000 inhabitants), 1067 patients (34.3 % females) initiating dialysis were identified, of whom 82 % underwent only hemodialysis (HD), 13 % only peritoneal dialysis (PD) and the remaining 5 % both treatments. Direct healthcare costs/patient were € 5239, € 12,303 and € 38,821 (€ 40,132 for HD vs. € 30,444 for PD patients) for the periods 24–12 months pre-dialysis, 12–0 months pre-dialysis, and in the first year of dialysis, respectively.
Conclusions
This study highlights a significant economic burden related to CKD and an increase in direct healthcare costs associated with the start of dialysis, pointing to the importance of prevention programs and early diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, kidney disease is the 9th leading cause of death and affects more than 10 % of the adult population, in most cases remaining undiagnosed. In 2012, total Medicare expenditure (excluding drugs) linked to kidney failure accounted for around 6 % of the Medicare budget costs [1]. In developed countries, end-stage renal disease (ESRD), requiring renal replacement therapy (RRT) in the form of dialysis or transplantation, represents an important and growing cost driver for National Health Services (NHS) with an annual growth of dialysis programs ranging between 6 and 12 % over the past two decades [2].
Only a minority of people with chronic kidney disease (CKD) will develop kidney failure in their life, partly due to the high risk of cardiovascular mortality in these patients (8- to 10-fold higher in CKD populations) [3–5]. US data report that among patients in CKD stage 3 (almost 40 % of the entire CKD population) only 0.15–0.2 % per year over 10–25 years progress to ESRD [3, 4, 6].
A huge economic impact and loss of productivity are associated with advanced kidney disease: several developed countries spend more than 2–3 % of their annual healthcare budget in providing treatment to the 0.02–0.03 % of the total population affected by ESRD [7]. In 2001, it was estimated in Italy that 1.8 % of the total healthcare budget was spent on ESRD patients, who represented 0.083 % of the general population [8]. But in Italy, there is limited evidence available on the healthcare resource consumption and costs [9, 10], particularly in relation to a large number of patients followed over a period of several years from pre-dialysis to RRT. In recent years, due to healthcare budget restrictions, analyses of the economic dimensions of health care have become important to identify areas for potential improvement. The aim of this study was to evaluate direct healthcare costs and resource consumption in CKD patients new to dialysis in the 2 years before beginning dialysis and in the first year of dialysis. The analysis was conducted from the perspective of the Lombardy Regional Healthcare Service (RHS).
Methods
The Italian public healthcare system provides coverage in terms of healthcare services to all Italian citizens on a Regional basis. All medical services provided by the Italian National Health system (hospitalizations, diagnostic procedures and drugs) are recorded, for each citizen, in local/regional databases for administrative purposes. For this study, data were provided by the Operative Unit for Government Data, Strategies and Plans of the healthcare system of the Lombardy Region (with a population of about 9,700,000 inhabitants) to enable an analysis of the healthcare resource consumption and related costs covered by the RHS of patients who underwent dialysis in 2011 (selection period: Jan 1 to Dec 31) for CKD/ESRD. The following information included in the RHS databases was analyzed: demographic characteristics of patients, drugs reimbursed by RHS (distributed through pharmacies in the local community or by RHS structures) in terms of consumption and costs, hospital discharge records in terms of frequency, diagnosis and costs, and diagnostic procedures including outpatient procedures, laboratory tests and visits. Only direct healthcare costs covered by the RHS were estimated for the purpose of the present analysis; transport costs, pension costs, productivity losses and any other direct or indirect costs not covered by RHS were not considered. Estimations of costs were based on the costs of goods/services paid by the Lombardy Region in the reference period and tariffs charged to the RHS reported in the data warehouse; drug prices paid by RHS could in some cases be lower than published prices due to hidden discounts applicable to NHS structures. As this study was carried out using data from the Lombardy RHS databases, private healthcare expenditure was not included. Patients’ tax codes were used in order to link the different databases.
Only data on individuals resident in the Lombardy Region were selected and all data were analyzed anonymously. All patients for whom a dialysis was recorded in 2011 were screened. From this population, patients with at least one dialysis treatment during the selection period and without any dialysis treatments in the previous 24 months were selected for the study (incident patients) and analyzed in a retrospective, observational and non-interventional way. Patients who discontinued dialysis during the first year (i.e. patients incident to dialysis who were still alive at 1 year from dialysis entrance but with a dialysis period—first to last dialysis date—shorter than 365 days), patients who underwent kidney transplantation, and patients with acute kidney injury (identified through the International Classification of Diseases, 9th Revision, Clinical Modification (ICD9-CM), [11] code 584) were excluded. Patients who died during the first year of dialysis were analyzed separately.
Selected patients were analyzed separately according to the type of dialysis and dialysis techniques used, identified through ICD9-CM codes reported in Table 1. Major concomitant pathologies were also identified in order to estimate their impact on healthcare costs; the diseases considered were: diabetes, cardiovascular diseases (CVD), and malignancies. The selected pathologies were attributed to patients by the analysis of their specific healthcare resource consumption in the 24 months preceding start of dialysis. Diabetes was identified through the prescription of drugs of the anatomical therapeutic chemical (ATC) class A10 (drugs used in diabetes) [12]; malignancies were identified through hospitalizations with ICD9-CM diagnosis (at any level) from 140 to 239 (neoplasm) [11] and/or prescriptions of drugs of ATC class L01 (antineoplastic and immunomodulating agents) [12]; CVD, including particularly severe cases, was identified through hospitalizations coded ICD9-CM from 390 to 459 (diseases of the circulatory system) [11].
For incident patients, healthcare resource consumption and costs were evaluated for the 24 months preceding the start of dialysis and for the 12 months after starting dialysis. For each patient, drug costs were calculated by multiplying the number of prescriptions by the cost of each prescription; hospitalization costs were calculated by multiplying each admission by the unit cost for each regional DRG tariff; diagnostic procedure costs were calculated by multiplying each procedure by its regional tariff.
Statistical analysis
We used proportions as the descriptive statistic for categorical variables, and mean ± standard deviation (SD), or median, for continuous variable. Costs were compared with the Wilcoxon non parametric test (for two samples) or Kruskall–Wallis test (for more than two samples). We used SAS software (version 9.2) to perform data analysis.
Results
A total of 8316 CKD patients who underwent dialysis in 2011 were identified (1083 were previously excluded because they were affected by acute kidney injury). Of these, 1682 were incident to dialysis, of whom 1067 (mean age 65.2 years, 58 % aged >65 years; 65.7 % males) met the pre-specified selection criteria for analysis (Table 2). Type of dialysis, dialysis techniques and intensity of assistance are also reported in Table 2. In the whole incident population (n = 1682), the mortality rate in the first year of dialysis was 21.7 % (n = 365) with a mean time to death from start of dialysis of 111.75 ± 108.64 days, median 69 days.
Considering incident dialysis, of 1067 patients who survived at least for the first year of dialysis and who did not discontinue RRT, the vast majority of patients were treated with only hemodialysis (HD) (81 %). Almost three out of four HD patients (72.4 %) were treated by diffusive techniques as a first treatment and about 67 % of HD sessions were performed in hospital centers; patients receiving only limited-care HD accounted for only 3.6 %. Almost half of the patients who underwent only PD (49.3 %) were treated with continuous ambulatory peritoneal dialysis (CAPD).
Presence and frequency of comorbidities in the total analyzed incident population (n = 1067) is reported in Table 3. Only one-third of patients had none of the identified concomitant pathologies; 10.2 % were affected by malignancies, 29.7 % by diabetes and 56.1 % by CVD; 1.9 % of the total population had all three selected concomitant pathologies.
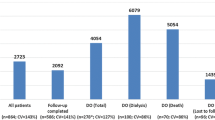
Average expenditure per patient increased from € 2317.8 ± 3399.2 in the period 24–18 months pre-dialysis, to € 8655.5 ± 8399.9 in the last 6 months before starting dialysis, further increasing to around € 19,000 in each of the two 6-months periods after starting dialysis (Fig. 1). Drugs expenditure increased slightly in the pre-dialysis period and remained substantially stable from 6 months before starting dialysis to 12 months after starting dialysis. Costs for diagnostic procedures (excluding dialysis) increased markedly from the 6 months pre-dialysis to the year following the start of dialysis. Hospitalization costs increased dramatically in the 6 months prior to dialysis and then decreased. Detailed costs by dialysis technique and type of assistance are reported in Table 4.
As expected [9, 21–23], the average yearly healthcare costs for patients treated only by HD were 32 % higher than for patients treated only by PD (€ 40,132.1 ± 13,321.8 vs. € 30,444.0 ± 9381.5, p < 0.0001, Wilcoxon test). Of patients receiving only HD, those treated only by convective techniques had a yearly cost that was 23 % higher than those treated only by diffusive techniques, although hospitalization costs in the latter group were 94 % higher than in the convective technique patients. Considering dialysis setting, patients receiving only limited-care HD had a 36 % lower yearly cost than those undergoing HD in dialysis centers (€ 30,518.4 ± 13,535.5 vs. € 41,641.1 ± 13,277.8, p < 0.0001, Wilcoxon test). Dialysis and hospitalizations represented by far the major cost drivers in all the subpopulations analyzed while, from 6 months before dialysis onward, drugs and diagnostic procedures had a limited impact on total healthcare costs.
Average yearly costs per patient saw a huge increase mainly due to hospitalization costs with the increasing number of comorbidities; in particular, the yearly cost for the hospitalization of patients with three concomitant pathologies was double that of patients without (Table 5). Healthcare costs in the last year of life of incident dialysis patients were € 35,571.9 ± 30,071.7 per patient (n = 365), the major cost component being hospitalization, representing 69.6 % of total healthcare costs (€ 24,762.6), while diagnostic procedures accounted for only 5.2 % (€ 1858.1).
Discussion
CKD is a complex disease that imposes a significant burden in terms of public health expenditure, the quality of life of affected patients, and healthcare management costs [8, 13–16]. The extremely significant burden of CKD costs was recently reported by the Global Burden of Disease Study 2013 Collaborators [17] who estimated the number of years lived with disabilities by CKD patients to be over 12 million. Some studies have shown that healthcare resources and costs associated with the treatment of CKD increase dramatically with the progression of the disease, particularly when RRT begins [9, 10, 18]. An Italian study [9] with a similar methodology to ours estimated the cost per patient covered by the NHS for 1 year preceding the start of dialysis to be € 11,123; these data are in line with our findings (€ 12,302.6). However, to our knowledge there are no published Italian or European data on incident dialysis patients covering the period from 24 months pre-dialysis to 12 months post dialysis initiation. The only data covering a similar period are contained in a study by St. Peter et al. [18], which was performed on a US population referring to the years 1995–1998; although our data are not directly comparable with theirs due to the different periods of analysis and healthcare settings, there is an evident similarity in the trend showing a steep increase in healthcare resource consumption and costs leading up to dialysis treatment. The only available studies investigating costs of patients incident to dialysis [18–20] are not Italian studies and were conducted in different healthcare settings, from a different perspective of analysis and with different methodologies, which means that comparison with our results is unfeasible.
Our findings regarding the economic advantages of treating patients with PD versus HD are expected and already reported in other studies, even if they do not focus on the incident population [9, 21–23]. The higher costs associated with the treatment of patients affected by concomitant pathologies are in line, despite the above-mentioned differences, with St. Peter et al. [18]. A very recent study published by Li et al. [24], performed on incident dialysis patients obtained linking the Hospital Episodes Statistics dataset to the UK Renal Registry data, despite the differences in the observational period (2003–2006) and healthcare setting, support some of our findings regarding the higher hospitalization costs in HD versus PD patients, the impact of comorbidities on costs and the higher hospitalization costs of patients that died during the first year of dialysis versus HD patients.
The use of administrative databases as a source information has some recognized limitations, such as the lack of clinical information, the unavailability of indirect costs, the impossibility to separate costs related to the specific disease or its comorbidities [25]. Administrative databases have, on the other hand, several advantages as they provide collected information on each individual patient who can be observed longitudinally for long periods accurately and systematically. In a real-world setting, this kind of analysis allows the estimation of treatment patterns and healthcare resource consumption and costs, thanks to the single datasets being linked using a tax code. These characteristics make administrative databases feasible tools for studies investigating real-world treatment patterns [26, 27].
This study presents complete and detailed information on a very large number of patients extracted from the administrative databases of a large Italian region, covering almost 10 million inhabitants. Moreover, the selected population was observed longitudinally over a long period of time (3 years) and in a very recent period. It could therefore accurately represent the therapeutic patterns and costs associated with patients incident to dialysis in the Lombardy Region. Finally, as far as we know, this study is the first to present detailed data on all dialysis techniques in different settings and the healthcare resource consumption and costs for patients over a prolonged pre-dialysis period.
This study highlights a dramatic increase in resource consumption and healthcare costs associated with the treatment of patients approaching RRT, underlining the possible advantages of prevention programs, as also reported by the National Kidney Foundation [28]. Our analysis of the different dialysis techniques/settings showed some already known information (higher costs associated with HD vs. PD) and some new evidence such as the differences in total amount of costs and cost composition of different dialysis techniques and different settings in HD patients. In PD patients, this study does not reveal significant differences between CAPD and APD. Finally, as expected, the presence of severe comorbidities is linked to a wide increase in resource consumption and healthcare costs mainly due to the increase in hospitalization costs.
References
Centers for Disease Control and Prevention (CDC) (2015) Chronic Kidney Disease Initiative—Protecting Kidney Health. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention. Available at http://www.cdc.gov/diabetes/projects/pdfs/ckd_summary.pdf. Accessed September, 9th 2015
Couser WG, Remuzzi G, Mendis S, Tonelli M (2011) The contribution of chronic kidney disease to the global burden of major non communicable diseases. Kidney Int 80(12):1258–1270. doi:10.1038/ki.2011.368 Epub 2011 Oct 12
Levey AS, Astor BC, Stevens LA et al (2010) Chronic kidney disease, diabetes, and hypertension: what’s in a name? Kidney Int 78:19–22
Keith DS, Nichols GA, Gullion CM et al (2004) Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med 164:659–663
Wen CP, Cheng TY, Tsai MK et al (2008) All-cause mortality attributable to chronic kidney disease: a prospective cohort study based on 462,293 adults in Taiwan. Lancet 371:2173–2182
Eriksen BO, Ingebretsen OC (2006) The progression of chronic kidney disease: a 10-year population-based study of the effects of gender and age. Kidney Int 69:375–382
Levey AS, Atkins R, Coresh J et al (2007) Chronic kidney disease as a global public health problem: approaches and initiatives—a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72:247–259
Pontoriero G, Pozzoni P, Vecchio LD et al (2007) International Study of Health Care Organization and Financing for renal replacement therapy in Italy: an evolving reality. Int J Health Care Finance Econ 7:201–215
Roggeri DP, Roggeri A, and Salomone M (2014) Chronic kidney disease: evolution of healthcare costs and resource consumption from predialysis to dialysis in Piedmont Region, Italy. Adv Nephrol 2014, Article ID 680737, 6 pages. doi:10.1155/2014/680737
Cicchetti A, Ruggeri M, Codella P, Ridolfi A (2011) I costi socio-sanitari dell’insufficienza renale cronica. Farmeconomia e Percorsi Terapeutici 12(1):21–28
International Classification of Diseases (ICD) (1978) 9th Revision, Basic Tabulation List with Alphabetic Index. World Health Organization, Geneva
World Health Organization Collaborating Centre for Drug Statistics and Methodology (2015). Available at http://www.whocc.no/atc_ddd_index/. Accessed September, 9th 2015
Zoccali C, Kramer A, Jager KJ (2010) Chronic kidney disease and end-stage renal disease—a review produced to contribute to the report ‘the status of health in the European union: towards a healthier Europe’. NDT Plus 3(213–312):224
Gorodetskaya I, Zenios S, McCulloch CE et al (2005) Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int 68:2801–2808
Kimmel PL, Patel SS (2006) Quality of life in patients with chronic kidney disease: focus on end-stage renal disease treated with hemodialysis. Semin Nephrol 26:68–79
Schieppati A, Remuzzi G (2005) Chronic renal diseases as a public health problem: epidemiology, social, and economic implications. Kidney Int 68(Supplement 98):S7–S10
Global Burden of Disease Study (2013) Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800. doi:10.1016/S0140-6736(15)60692-4
St. Peter WL, Khan SS, Ebben JP et al (2004) Chronic kidney disease: the distribution of health care dollars. Kidney Int 66:313–321
Salonen T, Reina T, Oksa H et al (2003) Cost analysis of renal replacement therapies in Finland. Am J Kidney Dis 42(6):1228–1238
Coentrão LA, Araújo CS, Ribeiro CA et al (2013) Cost analysis of hemodialysis and peritoneal dialysis access in incident dialysis patients. Perit Dial Int 33(6):662–670
Karopadi AN, Mason G, Rettore E et al (2013) Cost of peritoneal dialysis and haemodialysis across the world. Nephrol Dial Transplant 28(10):2553–2569
Liu FX, Quock TP, Burkart J et al (2013) Economic evaluations of peritoneal dialysis and hemodialysis: 2004–2012. F1000Research 2:273
Just PM, Riella MC, Tschosik EA et al (2008) Economic evaluations of dialysis treatment modalities. Health Policy 86(2–3):163–180
Li B, Cairns JA, Fotheringham J et al (2015) Understanding cost of care for patients on renal replacement therapy: looking beyond fixed tariffs. Nephrol Dial Transplant 30(10):1726–1734. doi:10.1093/ndt/gfv224
Haut ER, Pronovost PJ, Schneider EB (2012) Limitations of administrative databases. JAMA 307(24):2589–2590
Schneeweiss S, Avorn J (2005) A review of uses of healthcare utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol 58(4):323–337
Harpe SE (2009) Using secondary data sources for pharmacoepidemiology and outcomes research. Pharmacotherapy 29(2):138–153
National Kidney Foundation (2002) K/DOQI Clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 39(suppl 1):S1–S266
Acknowledgments
ReNe, Renal Lombardy Network (Centre, Director) Bergamo, Prof. G. Remuzzi; Bergamo Gavazzeni, Dr. G. Mingardi; Zingonia, Dr. M. Lorenz; Ponte San Pietro, Dr. A. Meterangelis; Treviglio, Dr. E.G. Galli; Seriate, Dr. L. Pedrini; Brescia Spedali Civili, Prof. G. Cancarini; Montichiari, Prof. F. Scolari; Desenzano, Dr. M. Brognoli; Gavardo, Dr. M. Brognoli; Manerbio, Dr. M. Brognoli; Chiari, Dr. M. Bracchi; Esine, Dr. M. G. Cattaneo; Como S. Anna, Dr. C. Minoretti; Lecco, Dr. G. Pontoriero; Crema, Dr. G. De Petri; Cremona, Dr. F. Malberti; Mantova, Dr. P.L. Botti; Bollate, Dr. U. Teatini; Cernusco S.N, Dr. O. Bracchi; Cinisello B, Dr. C. Pozzi; Desio, Dr. R. Scanziani; Legnano, Dr. C. Guastoni; Lodi, Dr. M. Farina; Magenta, Dr. C. Guastoni; Melegnano, Dr. S. Bisegna; Milano De Marchi, Dr. G.Montini; Niguarda, Dr. G. Colussi, Policilinico IRCCS Croff, Prof. P.G. Messa; S. Carlo, Dr. M. Gallieni; Milano S. Paolo, Prof. M. Cozzolino; Milano Simone Martini, Dr. D. Brancaccio; Monza, Prof. A. Stella; Vimercate, Dr. G.M. Ferrario; Casa di Cura S. Donato, Dr. M. Doria; Milano Sacco, Dr. A. Genderini; Milano H.S.R, Dr. D. Spotti; Milano FBF, Dr. A. Limido; Multimedica, Dr. S. Bertoli; Paderno Dugnano, Dr. C. Rovati; Policlinico Monza, Dr. C. Ballabeni; Milano San Faustino, Dr. R. Galato; Humanitas, Dr. S. Badalamenti; Pavia Fond. Maugeri, Prof. A. Dal Canton; Pavia S. Matteo, Dr. C. Esposito; Vigevano, Dr. R. Bellazzi; Voghera, Dr. F. Milanesi; Sondrio, Dr. C. Colturi; Busto Arsizio, Dr. A. Castiglioni; Gallarate, Dr. E. Caretta; Varese Macchi, Dr. G. Rombolà; Tradate, Dr. P. Scalia; Castellanza, Dr. S. Bertoli.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
As the study is retrospective, observational and data were extracted from the administrative database of Lombardy Region in an anonymous way, the ethical committees evaluation is not necessary.
Research involving human participants and/or animals
Not applicable because the study was observational and retrospective.
Informed consent
All data of the present study regarding patients were extracted already anonymized from the administrative databases of the Lombardy Region and analyzed in an anonymous way; therefore informed consent is not applicable.
Additional information
The list of authors of ReNe (Renal Lombardy Network) are listed in acknowledgments.
Rights and permissions
About this article
Cite this article
Roggeri, A., Roggeri, D.P., Zocchetti, C. et al. Healthcare costs of the progression of chronic kidney disease and different dialysis techniques estimated through administrative database analysis. J Nephrol 30, 263–269 (2017). https://doi.org/10.1007/s40620-016-0291-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0291-8