Abstract
The therapy of IgA nephropathy (IgAN) is cause for debate among nephrologists. Since the early 1980s, many therapeutic attempts have been proposed, but most of them did not prove efficacy. The recent KDIGO Clinical Practice Guideline for Glomerulonephritis recommend long-term ACE-I or ARB treatment when proteinuria is more than 1 g/day, with up-titration of the drug. For patients with GFR >50 ml/min and proteinuria persistently higher than 1 g/day, they suggest a 6-month course of corticosteroid therapy. Based on our experience and the results of the literature, we propose a progressive treatment, which takes into account the time the IgAN is recognized and the clinical conditions present at that time. The treatment can be summarize as follows: (1) in patients with macro-microscopic haematuria, in case with proteinuria less than 0.3 g/day, only annual controls; (2) in patients with proteinuria between 0.3 and 0.9 g/day, ACE-I and/or ARB, with titration of the drugs; (3) in patients with proteinuria higher than 1 g/day, in case with the presence of arterial hypertension and GFR up to 30 ml/min, 6 months course of corticosteroids, in addition to ACE-I and/or ARB; (4) in patients with GFR less than 30 ml/min, ACE-I/ARB, dialysis and kidney transplantation; corticosteroids should be in case considered for patients with persistently high or increasing proteinuria; (5) the immunosuppressants (cyclophosphamide and azathioprine) should be reserved for patients with progressive renal insufficiency or with vasculitic lesions on renal biopsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Therapy for immunoglobulin A nephropathy (IgAN) has been and continues to be a cause for debate among nephrologists. The recent Kidney Disease—Improving Global Outcomes (KDIGO) Clinical Practice Guideline for Glomerulonephritis [1] recommend long-term angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs) as treatment when proteinuria is more than 1 g/day, with up-titration of the drug depending on blood pressure. The guidelines also suggest ACE inhibitors or ARBs if proteinuria is between 0.5 and 1 g/day. For patients with glomerular filtration rate (GFR) >50 ml/min and proteinuria persistently higher than 1 g/day, despite 3–6 months of optimized supportive care (including ACE inhibitors or ARBs and blood pressure control), they suggest a 6-month course of corticosteroid therapy.
These therapeutic recommendations were proposed in 2012, i.e. 44 years after the first description of IgAN [2]. In the past, what was the therapeutic attitude of nephrologists towards this nephropathy? For a number of years, nephrologists did not treat IgAN because they considered it a benign nephropathy or a disease with a very slow progression of renal damage. However, over the years it was observed that many of the early patients first described with IgAN at Necker Hospital by Berger and Hinglais [2] went on to develop chronic renal insufficiency [3]. Therefore, from 1980 onwards, IgAN began to attract the attention of nephrologists, as can be seen from the number of publications in the scientific literature: less than 100 articles from 1968 to 1980 vs. more than 600 in the following 10 years. Since the early 1980s, many therapeutic approaches have been proposed, more than in other nephropathies: tonsillectomy, diet with reduced antigenic load, dapsone, diphenylhydantoin, disodium cromoglycate, danazol, plasmapheresis, eicosapentanoic acid, ACE inhibitors, ARBs, statins, endothelin receptor antagonists, high doses of intravenous (i.v.) immunoglobulins, antioxidants, vitamin E, corticosteroids, omega-3-fatty acids, warfarin, dipyridamole, heparin, cyclosporin, azathioprine, cyclophosphamide, mycophenolate mofetil, mizoribine, rituximab and budesonide. In spite of all these attempts, for many years the ideal therapy was not identified, suggesting to Appel an editorial in 2006, entitled: “To treat or not to treat IgA nephropathy? That is the question!” [4]. In the editorial, Appel explained that there was no consensus on which approach we should choose for these patients. Fortunately, in the last 10–15 years several randomized and controlled studies have been published, which have made the recent indications of KDIGO possible. A brief examination of the key studies that led to these therapeutic recommendations is warranted.
To evaluate the usefulness of renin-angiotensin system (RAS) blockers, Coppo et al. compared 32 patients with moderate proteinuria [1–3.5 g/day per 1.73 m2 and creatinine clearance (CrCl) >50 ml/min] who received benazepril (0.2 mg/kg) with 34 patients who received placebo [5]. The primary end-point, defined as a 30 % decrease in CrCl, was observed in one patient (3.1 %) in the benazepril group vs. five patients (14.7 %) in the placebo group. The composite end-point, defined as a 30 % decrease in CrCl and/or increase in proteinuria up to the nephrotic range, was reached in one patient (3.1 %) in the benazepril group vs. nine patients (26.5 %) in the placebo group, and the difference was found to be significant (p = 0.034). This study documented the usefulness of ACE inhibitors in IgAN, confirming what nephrologists had been doing in proteinuric nephropathies for several years.
The usefulness of corticosteroids remained uncertain for many years due to methodological shortcomings of the first published reports. To assess the advantages of these drugs, we published two papers reporting the mid- [6] and a long-term results [7] of a prospective, randomized study comparing 43 patients who received corticosteroids vs. 43 patients who received only supportive therapy. All patients had plasma creatinine less than 1.5 mg/dl and proteinuria in the moderate range (1–3.5 g/day). Patients assigned to the steroid group received 1 g methylprednisolone i.v. for three consecutive days, and this course was repeated 2 and 4 months later; oral prednisone was given at a dose of 0.5 mg/kg bodyweight on alternate days for 6 months. After 10 years, renal survival without reaching the primary end-point, which was defined as a doubling of plasma creatinine, was 97 % in the treated group and 53 % in the control arm; moreover, a median proteinuria during follow-up less than 1 g/day was observed in 70 % of treated vs. 30 % of control patients. Only one patient in the treated group showed important side effects (diabetes 2 years after the end of the treatment).
On the question of whether corticosteroids can provide additional benefits with respect to ACE inhibitors alone, two studies were published almost simultaneously [8, 9]. Lv et al. compared 30 patients who received ACE inhibitors alone with 33 patients who received ACE inhibitors plus oral prednisone for 6–8 months [8]. In the combination therapy group, oral prednisone was given at a dose of 1 mg/kg bodyweight for 2 months, and then the dose was tapered by 5–10 mg every 2 weeks. In both groups, cilazapril was administered at a dose of 5 mg/day. After a mean follow-up of 27 months, seven patients (24.1 %) in the ACE-inhibitor group and one patient (3 %) in the combination group reached the primary end-point, defined as a 50 % increase in plasma creatinine. A proteinuria decrease more than 50 % of baseline values was observed in 34 % of patients in the ACE-inhibitor group and in 71 % of the combination group. In another study, Manno et al. compared 49 patients who received ACE inhibitors alone with 48 patients who received ACE inhibitors plus oral prednisone for 6 months [9]. In the combination therapy group, the 6-month course of prednisone began with oral prednisone 1.0 mg/kg/day for 2 months and then the dose was tapered by 0.2 mg/kg/day every month. The maximal prednisone dose was fixed at 75 mg/day. In both groups, treatment with ramipril started at a dose of 2.5 mg/day and was then increased by 1.25 mg/day every month to maintain a blood pressure <120–80 mmHg and to reduce 24-h proteinuria to 1.0 g or less. After a mean follow-up of 60 months, 13 patients (26.5 %) in the monotherapy group and 2 (4.2 %) in the combination group reached the primary end-point, defined as a doubling of plasma creatinine. Renal survival after 8 years was 52.1 % in the monotherapy group and 85.2 % in the combination group. The authors of both studies concluded that the addition of corticosteroids to ACE inhibitors produces a more potent antiproteinuric effect and a better renal outcome than ACE inhibitors alone.
According to these results, the most effective treatment for IgAN patients with normal, or almost normal, renal function and moderate proteinuria should be a combination of RAS blockers and corticosteroids.
Among the other treatments, cyclophosphamide and mycophenolate mofetil deserve mention. Cyclophosphamide has shown considerable efficacy in a prospective and randomized study including 38 patients with progressive IgAN. In this particular group of patients, cyclophosphamide was able to reduce the frequency of end-stage renal failure [10]. Mycophenolate mofetil did not show benefits in the short-term in a number of randomized prospective studies. However, all these studies reported only short-term results, without assessing the possible benefits in the long-term. When one of these authors extended the observation from 2 to 6 years, he found that mycophenolate could provide renoprotection [11]. Therefore, it may be that cyclophosphamide and mycophenolate have a role to play in IgAN, but a final judgment is still premature.
IgAN has very often a silent onset, which means that diagnosis often is made late when, unfortunately, there are extensive chronic histological lesions and kidney function is severely deteriorated. Is there a treatment also for these patients? What drugs should be utilized and for what purpose? The KDIGO guidelines recommend the use of corticosteroids only in patients with an estimated GFR (eGFR) >50 ml/min and discourage it in those with eGFR <30 ml/min [1]. These recommendations are based on the belief that chronic damage makes any treatment ineffective and on the lack of good studies in patients with reduced renal function. We would like to offer some indications as the fruit of our own experience.
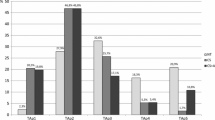
Recently, we submitted a paper analyzing the results obtained in 325 IgAN patients enrolled in three prospective, randomized, clinical trials [6, 12–14]. The patients were divided into three groups, according to their renal function, estimated with the chronic kidney disease—epidemiology (CKD-EPI) formula [15, 16]: eGFR >60 ml/min; eGFR 30–60 ml/min; eGFR <30 ml/min. Patients were further divided into three groups according to the treatment: supportive therapy (NT), steroids (S) and steroids plus azathioprine (S + A). The effectiveness of therapy was evaluated using time-average proteinuria (TA-proteinuria), confirmed to be one of the best outcome indicators in IgAN [17, 18]. We found that patients treated with S or S + A achieved significant proteinuria reduction also in advanced renal insufficiency. Indeed, after 6 months of treatment, proteinuria decreased to a similar extent in magnitude and rapidity in all degrees of chronic renal insufficiency, dropping below 1 g/day after 12 months of follow-up. In the long term, this mean reduction was sustained only in patients with eGFR >60 ml/min, while in patients with lower eGFR values at baseline, proteinuria tended to increase over time, remaining however below 1.5 g/day. In NT patients, TA-proteinuria did not decrease. Therefore, in the presence of advanced chronic renal failure, therapy with S or S + A fails to give a decisive remedy, but it can slow down the progression and postpone for years the need for renal substitution therapy. Lesions were evaluated histologically in 275 patients, using the World Health Organization (WHO) criteria as modified by Churg and Sobin: grade I: minimal glomerular lesions, n = 24 patients; grade II: active glomerular, tubular, and interstitial lesions, n = 105 patients; grade III: active and chronic lesions, n = 146 patients [8]. We were not able to use the Oxford classification, because many patients had undergone renal biopsy more than 10 years earlier and we had difficulties in retrieving and analyzing very old specimens. At baseline, proteinuria was higher in the patients at grade III compared to grades I and II. Considering the treated patients, mean 24-h proteinuria decreased similarly in the three grades of histological lesions and this reduction resulted evident mainly in the first 6 months. During follow-up, proteinuria remained nearly stable in almost all patients, without differences related to the degree of histological damage. In non-treated patients, proteinuria remained unchanged in the first 4 years of observation, regardless of the severity of histological lesions.
In a retrospective evaluation including 1147 patients from the VALIGA study, Tesar et al. found that 46 % of patients received immunosuppressants, of which 98 % received corticosteroids [19]. Although treated patients had greater clinical and pathologic risk factors of progression, they showed a significant reduction of proteinuria, a slower rate of renal function decline, and greater renal survival. Moreover, the benefits of corticosteroids extended to the patients with eGFR ≤50 ml/min and this effect was greater in patients with high levels of proteinuria. The authors concluded that the use of corticosteroids could be considered in patients with reduced renal function and elevated proteinuria, pending confirmation of these findings in a randomized trial.
But what are the possible treatments for the future?
In the ClinicalTrials.gov website (https://clinicaltrials.gov) there are about 70 trials listed in patients with IgAN, some of which are already completed, others in progress. Next to known drugs, we also find new products such as budesonide, sirolimus, rituximab, tripterigium wilfordii, fostamatinib, blisibimod, bortezomib, tacrolimus, and others. This leads to hope for more effective drugs in the coming years to treat all patients with IgAN.
However, for the present time we propose the following progressive treatment scheme, based on the time when IgAN is recognized and the clinical conditions present at that time (Fig. 1):
-
1.
patients with macro-microscopic hematuria, and proteinuria <0.3 g/day: annual check-up only;
-
2.
patients with proteinuria 0.3–0.9 g/day: ACE inhibitors and/or ARBs, with titration of dosage of the drugs;
-
3.
patients with proteinuria >1 g/day, and eventual presence of arterial hypertension and GFR up to 30 ml/min: a 6-month course of corticosteroids, in addition to ACE inhibitors and/or ARBs;
-
4.
patients with GFR <30 ml/min: ACE inhibitors/ARBs, dialysis and kidney transplantation.
Corticosteroids should be considered for patients with persistently high or increasing proteinuria. Immunosuppressants (cyclophosphamide and azathioprine) should be reserved for patients with progressive renal insufficiency or with vasculitic lesions on renal biopsy.
In conclusion, all IgAN patients should receive treatment, but the kind of treatment depends on the time when the disease is diagnosed and when the patient is taken in charge. The aim of treatment cannot be always the same: in some patients, it is to induce a complete and stable remission, while in others it is to slow down the progression of kidney damage. In any case, at the present time, the most effective therapeutic measures are RAS blockers and corticosteroids.
References
KDIGO clinical practice guidelines for glomerulonephritis (2012) Chapter 10: immunoglobulin A nephropathy. Kidney Int Suppl 2:S209–S217
Berger J, Hinglais N (1968) Le depots intercapillaire d’IgA-IgG. J Urol Nephrol 74:694–695
Chauveau D, Droz D (1993) Follow-up evaluation of the first patients with IgA nephropathy described at Necker Hospital. Contrib Nephrol 104:1–5
Appel GB (2006) To treat or not to treat IgA nephropathy? That is the question! Clin J Am Soc Nephrol 1:347–348
Coppo R, Peruzzi L, Amore A et al (2007) IgACE: a placebo controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol 18:1880–1888
Pozzi C, Bolasco PG, Fogazzi GB et al (1999) Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet 353(9156):883–887
Pozzi C, Andrulli S, Del Vecchio L et al (2004) Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol 15(1):157–163
Lv J, Zhang H, Chen Y et al (2009) Combination therapy of prednisolone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis 53:26–32
Manno C, Torres DD, Rossini M et al (2009) Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transplant 24:3694–3701
Ballardie FW, Roberts ISD (2002) Controlled prospective trial of prednisolone and cytotoxics in progressive IgA nephropathy. J Am Soc Nephrol 13:142–148
Tang SCW, Tang AWC, Wong SSH et al (2010) Long-term study of mycophenolate mofetil treatment in IgA nephropathy. Kidney Int 77(6):543–549
Pozzi C, Andrulli S, Pani A, Scaini P, Del Vecchio L, Fogazzi G, Vogt B, De Cristofaro V, Allegri L, Cirami L, Procaccini AD, Locatelli F (2010) Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. J Am Soc Nephrol 21(10):1783–1790
Pozzi C, Andrulli S, Pani A, Scaini P, Roccatello D, Fogazzi GB, Pecchini P, Del Vecchio L, Rustichelli R, Semeraro L, Locatelli F (2013) IgA nephropathy with severe chronic renal failure: a randomized controller trial with corticosteroids and azathioprine. J Nephrol 26:86–93
Sarcina C, Tinelli C, Ferrario F, Pani A, De Silvestri A, Scaini P, Del Vecchio L, Alberghini E, Buzzi L, Baragetti I, Pozzi C (2015) Changes in proteinuria and side effects of steroids alone or in combination with azathioprine at different stages of IgA nephropathy (submitted)
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 39(Suppl 1):S1–S246
Reich HN, Troyanov S, Scholey JW, Cattran D, For the Toronto Glomerulonephritis Registry (2007) Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 18:3177–3183
Sarcina C, Tinelli C, Ferrario F, Visciano B, Pani A, De Silvestri A, Fogazzi GB, Del Vecchio L, Terraneo V, Furiani S, Santagostino G, Corghi E, Pozzi C (2015) Corticosteroid treatment influences TA-proteinuria and renal survival in IgA nephropathy (submitted)
Tesar V, Troyanov S, Bellur S, Verhave JC, Cook HT, Feehally J, Roberts ISD, Cattran D, Coppo R, On behalf of the VALIGA Study of ERA-EDTA Immunonephrology Working Group (2015) Corticosteroids in IgA nephropathy: a retrospective analysis from the VALIGA study. J Am Soc Nephrol 26:2248–2258
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Author declares that he has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pozzi, C. Treatment of IgA nephropathy. J Nephrol 29, 21–25 (2016). https://doi.org/10.1007/s40620-015-0248-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0248-3