Abstract
Background
Colistin pharmacokinetics data are scarce regarding patients undergoing renal replacement therapy (RRT), or even absent as in patients treated with sorbent technologies potentially capable of removing colistin by extensive absorption on many polymeric materials.
Methods
Twelve septic shock patients with acute kidney injury (AKI) undergoing RRT [continuous venovenous hemodiafiltration (CVVHDF) n = 7, coupled-plasma filtration adsorption-HF (CPFA-HF) n = 4, hemoperfusion n = 1] treated with colistin methanesulfonate at a dose of 4.5 × 106 U bid were studied. Colistin A (Col-A) and colistin B (Col-B) concentrations on plasma and effluent at time 0, 0.2, 1, 3, 6, 12, 24 and 48 h were determined by the liquid chromatography-tandem mass spectrometry method.
Results
With CVVHDF the sieving coefficient was lower for Col-A, peaked early (0.40 for Col-A at 10 min, and 0.59 for Col-B at 3 h) and declined after 48 h (0.22 and 0.30 for Col-A and Col-B, respectively). Colistin’s filter clearance showed a similar pattern, with the highest clearance value of 18.7 ml/min for Col-B at 1 h. With CPFA-HF after the cartridge the Col-A and Col-B levels were negligible (<0.2 mg/l) or not detectable. The sum of the effluent and cartridge clearances reached values of 30 and 40 ml/min for Col-A and Col-B, respectively. With hemoperfusion the postcartridge concentrations for Col-A and Col-B were about 30 % lower than those determined precartridge.
Conclusions
During CPFA-HF and CVVHDF, the extent of colistin removal is high, and patients should receive an unreduced dosage. However, due to risk of accumulation in long-term administration colistin plasma levels determination is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colistin (polymyxin E), a re-emerged antibiotic for multidrug-resistant gram-negative bacterial infections [1–4], is an antibiotic mixture containing more than 30 components differing in amino-acid and fatty-acid residue composition. The two major components of the mixture are colistin A (polymyxin E1) and colistin B (polymyxin E2) [4]. Colistin A and B have a discrete neuro- and nephrotoxicity [5–8]. To reduce colistine nephro- and neurotoxicity, the drug is currently administered intravenously as sodium colistimethate (CMS), an inactive prodrug which is hydrolyzed in vivo to the active colistin base moiety [2–4]. The risk of colistin nephrotoxicity proved to be clinically significant after 14 days administration [5]; it appeared to be linked to its cumulative dosage [6], was associated with advancing age and receipt of concurrent nephrotoxic agents [7], and was predicted by the plasma colistin level [8].
Pharmacokinetics and pharmacodynamics of colistin are complex, and data are relatively scarce for critically ill patients with acute kidney injury (AKI) undergoing continuous venovenous hemodiafiltration (CVVHDF) or hemodialysis, which provide inconstant clearance of colistin in addition to endogenous clearance [9–16].
The colistin pharmacokinetics issue has become even more relevant in septic shock patients treated by some new renal replacement therapy (RRT) approaches recently proposed to increase the removal of endotoxin, bacterial products and both pro- and anti-inflammatory mediators [15, 17–19]. These new treatments, including high volume hemofiltration/hemodiafiltration [15], coupled plasmafiltration adsorption (CPFA-HF) [17, 18] and hemoperfusion [19], are potentially capable of removing colistin, due to its hydrophobic character that allows its extensive absorption on many polymeric materials [9, 15]. However, less than 20 cases have been reported so far on conventional continuous RRT (CRRT) accomplished with different membranes [9–16], and no data are available for patients treated with sorbent technologies. Although glomerular filtration rate is the parameter used to guide dose adjustment, kidney disease does affect non-renal clearances, and this aspect has not been adequately considered in most pharmacokinetic studies [20].
Recently, we implemented the quantitative evaluation of colistin A and B using high pressure liquid chromatography-tandem mass spectrometry (HPLC–MS/MS), and obtained preliminary data from 4 patients undergoing CVVHDF [21]. Subsequently, we kept investigating the distribution of colistin between plasma and effluent in further patients treated with CRRT and sorbent technology. The results presented here reveal that sorbent technology is associated to an efficient clearance of colistin through the polysulfone filter and cartridge, and pose the question of colistin maintenance dosage for these patients.
Subjects and methods
Patients
Twelve critically ill patients, median (interquartile range) age 60 (39.5–81.5) years, with septic shock according to current definitions [22] were studied. All patients presented systemic infection sustained by a strain of multiresistant gram-negative bacteria with only residual sensitivity to colistin and suffered from AKI needing RRT [23]. Patients received the conventional pharmacological therapy including crystalloid solutions, broad-spectrum antibiotics, diuretics, vasopressor agents and colistin as part of their standard care. The causes of the primary injury, the causative bacteria, the administered antibiotics, the severity of illness score, and the outcome are reported in Table 1.
Out of 12 patients, seven were treated by CVVHDF (group CVVHDF, n 7 sessions), four by CPFA-HF (group CPFA-HF, n 4 sessions) and one patient with hemoperfusion cartridge (n 2 sessions). Preliminary data from three patients of group CVVHDF were part of the validation of the HPLC–MS/MS method described in [21].
All patients started CVVHDF or CPFA-HF with the citrate anticoagulation protocol [24, 25] to prevent their high bleeding risk (defined as the bleeding alert at catheter insertion site, tracheostomy, gastrointestinal tract, or in surgical wounds) or due to frank bleeding necessitating transfusion of red packed cells.
The study protocol was in accordance with the principles contained in the Helsinki Declaration. Informed written consent was obtained from either a close relative or a legal representative.
CVVHDF protocol
CVVHDF procedures were carried out with a Multifiltrate apparatus (Fresenius Medical Care AG, Bad Homburg, Germany) equipped with a high flux polysulfone filter (AV1000, Fresenius Medical Care) at a blood flow rate of 120 ml/min. Fluid infusion, dialysate flow rates and citrate anticoagulation were done as previously described [24].
CPFA-HF protocol
CPFA-HF was performed by a five-pump CRRT machine [Lynda, Bellco, Mirandola, (MO), Italy] equipped with a polyethersulfone plasmafilter (0.45 m2, MPS 05, Bellco) placed in series with a highly permeable polyethersulfone hemodialyzer (1.4 m2, BLS814G, Bellco). The plasma was produced at a rate of 15–20 % blood flow, and subsequently underwent absorption on an unselective hydrophobic resin cartridge [17, 18, 25].
For the hemofiltration treatment, a sterile bicarbonate-calcium containing solution was infused in postdilution at a rate of 1,500 ml/h. The circuit anticoagulation was done by a calcium-free citrate-containing solution infused in predilution mode at 25–30 % blood flow [25].
Hemoperfusion protocol
One patient underwent hemoperfusion using a Polymyxin-B Fiber cartridge (Toraymyxin, Toray Industries, Tokyo, Japan) following the manufacturer’s instructions [19]. The treatment lasted for 2 h and a further treatment was repeated 24 h later (QB 120 ml/min). As anticoagulation, we followed the manufacturer’s protocol which indicated as sole anticoagulant a heparin bolus dose of 2,000 U at the start of the hemoperfusion session.
Colistin methanesulphonate infusion and sampling protocol
Colistin methanesulphonate [Colimicina, UCB Pharma SpA, Pianezza (TO), Italy] was administered by i.v. infusion over 60 min at a dose of 4.5 × 106 U [2] in 250 ml of a normal saline solution every 12 h. Since no specific recommendations based on clinical evidence were prescribed for patients undergoing CRRT, standard colistin methanesulphonate (CMS) dose was adopted [26]. All biological samples were collected after the 3rd day of therapy at the steady state condition of colistin pharmacokinetics.
The samples were collected at time 0, 10 min, 1, 3, 6, 12, 24 and 48 h after the beginning of the CVVHDF session, and at time 0, 1, 3, 6, and 9 h for the CPFA-HF sessions. Infusion of colistin was done during the first hour of CPFA-HF.
Samples were drawn from systemic arterial blood, circuit venous line, effluent line and in the CPFA-HF session from precartridge line and postcartridge line, immediately stored at −22 °C and analyzed within a week. In addition, in burn patient n. Eight treated with colistin for 24 days we sequentially determined systemic arterial blood on the 1st and 2nd CPFA-HF (at day 6 and 7 of colistin therapy) and on the 6th and 7th CPFA-HF (day 16 and 17 of colistin therapy) (see Fig. 3).
Pharmacokinetic parameters including sieving coefficient (SC), effluent clearance (Clear_effl, ml/min), filter clearance (Clear_filter, ml/min) and cartridge clearance (Clear_cartridge, ml/min) were calculated with standard formula (see supplementary material).
Determination of colistin in plasma and ultrafiltrate
Colistin A and B were determined using the HPLC–MS/MS method described in detail in a previous study [21]. The analytical methods for plasma and ultrafiltrate samples were validated following the common procedures recommended by the Guideline on bioanalytical method validation of the European Medicines Agency [27].
Statistical methods
The software program Statistica (Statistica 6.1, StaSoft Inc, Tulsa, OK, USA) was used for descriptive statistics, ANOVA with the Duncan multicomparison test, Student’s test, and linear regression analysis for quantitative variables and graphs. Values were expressed as median (interquartile range). p values <0.05 were considered statistically significant.
Results
Clinical and dialysis data
The clinical data and outcome of patients treated with colistin are reported in Table 1. Only four patients survived out of 12. Seven patients were severely burned (two survived) and five were admitted to the intensive care unit after a polytrauma event (two survived). Most of patients were affected by multiple infections, and treated with several antibiotics.
Table 2 shows dialysis flow rates in groups CVVHDF, CPFA-HF and Hemoperfusion. Blood flow rates were significantly higher in CPFA-HF than in CVVHDF (100.0 vs. 135.0 ml/min). Also the effluent volumes, obtained by the sum of infusion and dialysate volumes, were significantly different (3,800 vs. 1,550 ml/h, p < 0.05). In addition, in group CPFA-HF the rate of treated plasma reached median values higher than 20 ml/min.
Colistin handling in group CVVHDF
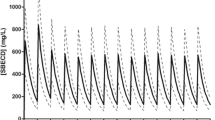
SCcvvhdf was significantly lower for colistin A than for colistin B over the entire CVVHDF session (Fig. 1a). SCcvvhdf values peaked (SCmax) early during each session (SCmax = 0.40 at 10 min for colistin A, SCmax = 0.59 at 3 h for colistin B), and slightly declined after 48 h (SCcvvhdf = 0.22 for colistin A and SCcvvhdf = 0.30 for colistin B, see Fig. 1a).
Colistin A and B removal on CVVHDF. a (upper panel) Shows SCcvvhdf of colistin A and B. b (middle panel) and c (lower panel) Show effluent (Clear_effl) and filter clearances (Clear_filter) for colistin A and B, respectively. Data are given as median (interquartiles). Numbers of box plots with whiskers indicate the individual data points. CVVHDF continuous venovenous hemodiafiltration, SC sieving coefficient
Figure 1b and c show the Clear_effl and Clear_filter for colistin A and B, respectively. Most Clear_filter values overlied Clear_effl values, except for an early peak found 1 h after infusion for both colistin A and B. Declining clearance values were progressively observed, reaching half of the starting values at 48 h.
No correlation between blood flow rate and colistin A sieving coefficient was found (Fig. 5, panel a, n 40 points), whereas a weak negative correlation was present with colistin B sieving coefficient (Fig. 5, panel b, n 40 points).
Colistin handling in group CPFA-HF
During CPFA-HF sessions, the colistin A Cpl_in decreased roughly 4-fold (from basal level of 10.4 to 2.6 mg/l at 9 h) (Fig. 2a). Colistin A and B precartridge levels were about 4 and 2 mg/l, respectively, representing about 50–60 % of the levels present in systemic plasma. Postcartridge, the colistin levels were lower than 0.2 mg/l (see Fig. 2a), or not detectable any longer (see Fig. 2b).
Colistin A and colistin B concentrations and clearances throughout 9-h CPFA-HF treated patients (n 4 sessions). a and b Show concentrations of colistin A (upper left panel) and colistin B (upper right panel) in systemic, precartridge and postcartridge plasmas. c and d Show extracorporeal and effluent clearances of colistin A (lower left panel) and colistin B (lower right panel). Extracorporeal clearances are obtained by the sum of cartridge and effluent clearance (n 4 sessions). Data are given as median (interquartiles). Numbers of box plots with whiskers indicate the individual data points. CPFA-HF coupled-plasma filtration adsorption-HF
The extracorporeal plasma clearance of colistin (the sum of the effluent and cartridge clearance) was slightly higher for colistin B than for colistin A, with values of approximately 40 and 30 ml/min, respectively (Fig. 2c, d).
In a burn patient (n. 8) treated with colistin for 24 days the systemic levels for colistin A and B on day 16 and 17 of colistin therapy (6th and 7th CPFA-HF sessions) showed an accumulation with peak values of 20 and 4 mg/l, respectively (Fig. 3b), double in comparison to those determined on day 6 and 7 of colistin therapy (1st and 2nd CPFA-HF) (Fig. 3a).
No correlation between blood flow rate and colistin A and B sieving coefficient was found (Fig. 5, panel c, d, respectively, n 16 points).
Colistin handling in the patient undergoing hemoperfusion
In the initial part of the 2-h hemoperfusion session, the postcartridge concentrations for colistin A and B were about 30 % lower than those measured before the cartridge (Fig. 4, panel a). Clearance for both colistin A and B showed similar patterns, declining to a minimal level of 2–3 ml/min at the end of the 2-h session (Fig. 4, panel b).
Colistin A and B concentrations and clearances during hemoperfusion. a Shows precartridge and postcartridge plasma concentrations of colistin A and B throughout 2-h hemoperfusion (one patient, 2 consecutive sessions). b Shows colistin A and B plasma clearance throughout 2-h hemoperfusion (one patient, 2 consecutive sessions)
Discussion
Blood extracorporeal treatments by CVVHDF, CPFA-HF and hemoperfusion all efficiently remove a significant amount of active forms of colistin, the highest clearance values being observed with plasma sorbent technology.
So far, only a few reports based on a limited number of patients have addressed the issue of colistin clearance due to extracorporeal treatments [9–16]. Some information was related to hemodialfiltration and intermittent hemodialysis, and most data were collected upon treatments with polyacrylonitrile membrane [9, 11, 15]. In addition, the reported pharmacokinetics data were not homogeneous, and led to contradictory dosage adjustments to ensure optimal concentrations of active colistin [9–14]. As a matter of fact, presence of residual renal function, dialysis dose, differences in RRT techniques, including the use of filter membrane with different adsorption capacity, might offer a partial explanation for the discrepancies observed in the effluent or filter clearance [9, 13, 15]. As shown in Table 2, the delivered dialysis dose in both groups CVVHDF and CPFA-HF roughly reached (500 ml/kg/day), that is the currently suggested target of dialysis adequacy [23]. To date, no data are available for patients undergoing sorbent technology treatments, such as plasma adsorption or hemoperfusion, and also in the present case findings on colistin extracorporeal clearance obtained from CVVHDF with polysulfone membrane exceed the ones so far reported. This new high-permeability membrane allows improved clearance of middle-size molecules without an increase in albumin loss [28]. At the moment, clearance data for this dialyzer are available for small and some middle-size molecules only, because of the novelty of this type of membrane.
In CVVHDF, the extracorporeal clearance of colistin depends on its elimination through the large exchange area (1.8 mq) of high-flux polysulfone membrane. Polysulfone material is characterized by an anionic surface without significant protein absorption properties, and freely permeable to substances with molecular weight up to 30 kDa [29]. A higher SC for colistin B than for colistin A was confirmed [21], as colistin A is likely to be more extensively bound to albumin than colistin B due to its longer fatty acid residue [4]. As expected, the extent of Clear_effl and Clear_filter (the latter representing the sum of effluent and adsorption clearance) in the patients treated with CVVHDF were substantially the same (Fig. 1b, c), as the polysulfone membrane has small and transient adsorption capacity [29].
In four patients (2 with severe burns and 2 with polytrauma) affected by AKI and refractory septic shock, a CPFA-HF treatment was applied [17, 18, 24]. By measuring the clearance of colistin for hemofilter and sorbent cartridge separately, we found that the plasma colistin A and B present in the precartridge (after the plasmafilter) were fully adsorbed by the cartridge, leaving negligible concentrations in the postcartridge sampling site, as shown in Fig. 2a, b. Interestingly, the concentrations of colistin determined in the precartridge plasma were proportional to those present in the systemic plasma, and comparatively higher for colistin B, probably because of its lower binding to proteins [4]. Thus, the measured cartridge clearance (roughly 15–20 ml/min) added to the effluent clearance of the hemofilter, produces for the 9 h of treatment a total extracorporeal clearance as extensive as 34 and 43 ml/min for colistin A and B, respectively. These extracorporeal clearance values should be added to the endogenous clearance of both colistin and its prodrug CMS, which are in turn affected by renal failure [11]. Even if the decreased renal function implies that a larger fraction of the CMS dose (mainly eliminated by the kidneys) is converted to colistin, renal clearance of colistin represents only a minimal fraction (about 4 %) of its extrarenal clearance of 48.7 ml/min [30]. The CPFA-HF extracorporeal colistin clearance of 40 ml/min for 9 h is close to that recently reported in a patient on extended dialysis by Strunk et al. [31], demonstrating no accumulation of drug after 9 days of treatment. In effect, in our burn patient on CPFA-HF, after 16–17 days of treatment colistin peaked at 20 mg/l. On the other hand, the patient responded well to this antibiotic therapy, and he survived with a complete recovery of renal function.
Since both SC and clearance depend on many dialytic parameters, such as blood flow, ultrafiltrate flow, albumin fraction sampling time, and patency of circuit (which is also affected by the type of anticoagulant), a separate evaluation of the effect of the anticoagulant used is very difficult. The same applies to the relationship between SC and blood flow (see Fig. 5), which are substantially uncorrelated during CVVHDF (Fig. 5, panel a, b) and CPFA-HF (Fig. 5, panel c, d) over the operative conditions of blood flow variations (100 vs. 135 ml/min, see Table 2).
Correlation between blood flow rate and colistin A and B sieving coefficient. a and b Show correlations during CVVHDF for colistin A and B, respectively (n 40 points). c and d Show correlations during CPFA-HF for colistin A and B, respectively (n 16 points). CVVHDF continuous venovenous hemodiafiltration, CPFA-HF coupled-plasma filtration adsorption-HF
Equivalent clearance values of 15 ml/min for colistin A and B were observed at the beginning of the two consecutive hemoperfusion sessions carried out in a patient with infection from Klebsiella KPC. However, the short time of application (2 h) likely resulted in a negligible impact of hemoperfusion on the daily total body colistin clearance. Recently some endotoxin adsorbents for extracorporeal blood purification have been compared [32]. Among them, only the polymyxin B-based adsorbers were able to reduce the lipopolysaccharide (LPS) activity. This study [32] showed that during toraymyxin hemoperfusion in vitro (the sorbents used in our clinical setting of hemoperfusion) the reduction in LPS activity was caused by polymyxin B desorption, which inactivated the endotoxins [32]. However, in our clinical settings we found no significant variation in polymyxin B area signal of effluent and circuit blood samples, so we could not confirm this phenomenon (polymyxin B was our internal standard).
In conclusion, we demonstrated that during CPFA-HF and CVVHDF with high-flux polysulfone filter, colistin A and B were efficiently removed. The extent of this removal, quite well predicted by parameters of dialysis efficiency (volume of effluent, volume of plasmafiltrate) and by free fraction of drug, can counterbalance or overcome the increased bioavailability of colistin due to renal failure. These data suggest that patients on CVVHDF and, even more, patients on CPFA-HF should receive an unreduced CMS dosage, although, with long-term administration, determination of colistin plasma levels is recommended on account of the risk of drug accumulation.
References
Wareham DW, Bean DC, Khanna P et al (2008) Bloodstream infection due to Acinetobacter spp.: epidemiology, risk factors and impact of multi-drug resistance. Eur J Clin Microbiol Infect Dis 27:607–612
Li J, Nation RL, Turnidge JD, Milne RW, Coulthard K, Rayner CR, Paterson DL (2006) Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect Dis 6:589–601
Falagas ME, Kasiakou SK (2005) Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis 40:1333–1341
Bergen PJ, Landersdorfer CB, Zhang J et al (2012) Pharmacokinetics and pharmacodynamics of ‘old’ polymyxins: what is new? Diagn Microbiol Infect Dis 74:213–223
Koch-Weser J, Sidel VW, Federman EB, Kanarek P, Finer DC, Eaton AE (1970) Adverse effects of sodium colistimethate. Manifestations and specific reaction rates during 317 courses of therapy. Ann Intern Med 72:857–868
Hartzell JD, Neff R, Ake J et al (2009) Nephrotoxicity associated with intravenous colistin (colistimethate sodium) treatment at a tertiary care medical center. Clin Infect Dis 48:1724–1728
Collins JM, Haynes K, Gallagher JC (2013) Emergent renal dysfunction with colistin pharmacotherapy. Pharmacotherapy 33:812–816
Sorlí L, Luque S, Grau S et al (2013) Trough colistin plasma level is an independent risk factor for nephrotoxicity: a prospective observational cohort study. BMC Infect Dis 13:380
Li J, Rayner CR, Nation RL, Deans R et al (2005) Pharmacokinetics of colistin methanesulfonate and colistin in a critically ill patient receiving continuous venovenous hemodiafiltration. Antimicrob Agents Chemother 49:4814–4815
Marchand S, Frat JP, Petitpas F et al (2010) Removal of colistin during intermittent haemodialysis in two critically ill patients. J Antimicrob Chemother 65:1836–1837
Garonzik SM, Li J, Thamlikitkul V, Paterson DL et al (2011) Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother 55:3284–3294
Healy DP, Sombun AD, Gardner JC et al (2011) Pharmacokinetics of colistin in an adolescent boy with extensive burn injury. J Burn Care Res 32:e7–e11
Markou N, Fousteri M, Markantonis SL et al (2012) Colistin pharmacokinetics in intensive care unit patients on continuous venovenous haemodiafiltration: an observational study. J Antimicrob Chemother 67:2459–2462
Karvanen M, Plachouras D, Friberg LE et al (2013) Colistin methanesulfonate and colistin pharmacokinetics in critically ill patients receiving continuous venovenous hemodiafiltration. Antimicrob Agents Chemother 57:668–671
Honore PM, Jacobs R, Lochy S et al (2013) Acute respiratory muscle weakness and apnea in a critically ill patient induced by colistin neurotoxicity: key potential role of hemoadsorption elimination during continuous venovenous hemofiltration. Int J Nephrol Renovasc Dis 6:107–111
Luque S, Sorli L, Li J et al (2014) Effective removal of colistin methanesulphonate and formed colistin during intermittent hemodialysis in a patient infected by polymyxin-only-susceptible Pseudomonas aeruginosa. J Chemother 26:122–124
Ronco C, Inguaggiato P, D’Intini V et al (2003) The role of extracorporeal therapies in sepsis. J Nephrol 16(Suppl 7):S34–S41
Livigni S, Bertolini G, Rossi C, On behalf of GiViTI et al (2014) Efficacy of coupled plasma filtration adsorption (CPFA) in patients with septic shock: a multicenter randomised controlled clinical trial. BMJ Open 4(1):e003536
Cruz DN, Perazella MA, Bellomo R et al (2007) Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Crit Care 11(2):R47
Matzke GR, Aronoff GR, Atkinson AJ Jr et al (2011) Drug dosing consideration in patients with acute and chronic kidney disease-a clinical update from kidney disease: improving global outcomes (KDIGO). Kidney Int 80:1122–1137
Leporati M, Bua RO, Mariano F et al (2014) Determination by LC-MS/MS of colistins A and B in plasma and ultrafiltrate from critically ill patients undergoing continuous venovenous hemodiafiltration. Ther Drug Monit 36:182–189
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign guidelines committee including the pediatric subgroup. surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) group. Crit Care 8:R204–R212
Mariano F, Tedeschi L, Morselli M, Stella M, Triolo G (2010) Normal citratemia and metabolic tolerance of citrate anticoagulation for hemodiafiltration in severe septic shock burn patients. Intensive Care Med 36:1735–1743
Mariano F, Tetta C, Stella M, Miletto A, Triolo G (2004) Regional citrate anticoagulation in critically ill patients treated with plasma filtration and adsorption. Blood Purif 22:313–319
Plachouras D, Karvanen M, Friberg LE et al (2009) Population pharmacokinetic analysis of colistin methanesulfonate and colistin after intravenous administration in critically ill patients with infections caused by gram-negative bacteria. Antimicrob Agents Chemother 53:3430–3436
Guideline on bioanalytical method validation (2011). European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2011/08/WC500109686.pdf (553 EMEA/CHMP/EWP/192217/2009)
Schmidt JJ, Hafer C, Clajus C et al (2012) New high-cutoff dialyzer allows improved middle molecule clearance without an increase in albumin loss: a clinical crossover comparison in extended dialysis. Blood Purif 34:246–252
Heilmann K, Keller T (2011) Polysulfone: the development of a membrane for convective therapies. Contrib Nephrol 175:15–26
Couet W, Grégoire N, Gobin P et al (2011) Pharmacokinetics of colistin and colistimethate sodium after a single 80-mg intravenous dose of CMS in young healthy volunteers. Clin Pharmacol Ther 89:875–879
Strunk AK, Schmidt JJ, Baroke E, Bode-Böger SM, Martens-Lobenhoffer J, Welte T, Kielstein JT (2014) Single- and multiple-dose pharmacokinetics and total removal of colistin in a patient with acute kidney injury undergoing extended daily dialysis. J Antimicrob Chemother 69:2008 (Epub ahead of print) (PubMed PMID: 24651826)
Harm S, Falkenhagen D, Hartmann J (2014) Endotoxin adsorbents in extracorporeal blood purification: do they fulfill expectations? Int J Artif Organs 37:222–232
Acknowledgments
For this study we did not receive any specific financial support.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mariano, F., Leporati, M., Carignano, P. et al. Efficient removal of colistin A and B in critically ill patients undergoing CVVHDF and sorbent technologies. J Nephrol 28, 623–631 (2015). https://doi.org/10.1007/s40620-014-0143-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-014-0143-3