Abstract
Background
Several reports associate an Italian-style Mediterranean diet (IMD) with lower risk of cardiovascular disease and morbidity. The present study aimed to explore the effects of an Italian Mediterranean organic diet (IMOD) versus low-protein diet (LPD) in chronic kidney disease (CKD) patients, according to patients’ carrier status for the methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism.
Methods
A total of 40 male patients with CKD and stable renal function (Kidney Disease Outcomes Quality Initiative stages 2 and 3) were classified according to MTHFR polymorphism as carrier T(+) or non carrier T(−). At the time of enrolment (T0) patients’ diet consisted of LPD; they were then administered IMD for 14 days (T1), thereupon IMOD for 14 days (T2). Patients underwent a complete medical history, body composition assessment and biochemical analysis.
Results
Baseline homocysteine levels were on average 8.24 mol/l higher (95 % confidence interval 6.47, 10.00) among T(+) than T(−) and the difference was statistically significant (p < 0.001). We found a significant interaction between MTHFR status and the effect of both the IMD and IMOD on homocysteine levels compared to LPD (p for interaction <0.001). Both the IMD and IMOD resulted in significant variations of anthropometric and laboratory measurements.
Conclusions
IMD and IMOD diets could represent a viable alternative to LPD in CKD patients on conservative therapy. The effect of these diets seems to be influenced by MTHFR genotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with chronic kidney disease (CKD), the rate of mortality from cardiovascular disease is 10- to 20-fold higher than that seen in the general population, even after correction for age, sex, race and the presence of diabetes [1]. Hyperhomocysteinemia has been identified as a predictor of atherosclerotic complications in the general population. It is also frequent among patients with renal failure [2] and several studies have shown that in CKD hyperhomocysteinemia is a risk factor for cardiovascular complications [3]. Hyperhomocysteinemia at an earlier stage of renal disease could also accelerate the progression of chronic renal disease. Homocysteine (Hcy) causes endothelial cell dysfunction and injury via production of reactive oxygen species during its autoxidation [4]. Hyperhomocysteinemia enhances vascular smooth muscle cell proliferation [5], increases platelet aggregation, acts on the coagulation cascade and fibrinolysis, directly inducing or acting in a synergistic manner with other risk factors to create a prothrombotic environment [6].
Serum and intracellular levels of Hcy are regulated by remethylation to methionine or trans-sulfuration to cysteine. The methyl donor in the vitamin B12-dependent remethylation is 5-methyltetrahydrofolate generated from the reduction of the 5,10-methylenetetrahydrofolate reductase (MTHFR) enzyme. Elevated plasma concentrations of total Hcy (tHcy) depend chiefly on genetic defects in the enzymes involved in homocysteine metabolism or in nutritional deficiency of the vitamin cofactors. A common C/T mutation at nucleotide position 677 (C677T) has been identified in the gene coding for MTHFR. This genetic mutation causes a valine for alanine substitution, which decreases MTHFR activity and tends to increase tHcy concentrations in individuals who are homozygous for the T/T genotype [7]. Two other MTHFR polymorphisms have been identified (G1793A and A1298C) [8]. A study has shown that in a large population of kidney transplant recipients, the patients carrying the MTHFR G1793A mutation had approximately 4 nmol/l higher plasma Hcy concentrations compared to individuals with the corresponding wild-type alleles [9].
Several observational studies have provided scientific evidence that diets rich in fruit, vegetables, legumes, whole grains, fish, and low-fat dairy products are associated with lower incidence of various chronic diseases, including atherosclerosis, cardiovascular diseases, and cancer. Since the early 1990s, growing evidence indicates that the Mediterranean diet, a concept first proposed by Keys in the mid-1980s, has a beneficial influence on health and longevity. Previous studies have demonstrated that the Mediterranean diet (MD) with a lower risk of coronary heart disease (CHD) morbidity and mortality [10–12].
The mechanisms by which the Mediterranean diet exerts its favorable effects on the cardiovascular system are diverse and a number of plausible explanations have been provided, including regulation of arterial blood pressure levels, body weight, blood lipid concentrations, inflammation and coagulation processes, and endothelial function.
It has been suggested that organic products could contain 10–50 % more phytochemicals than non-organic products. Previous data highlighted a possible impact on human health of a Mediterranean diet comprising organic products versus conventional, due to the effect on the total plasma anti-oxidant capacity, i.e. an increase in plasma antioxidant capacity was observed in the subjects receiving the organic diet [13].
Conscious that, regardless of its organic or conventional origin, a well-balanced diet is necessary to improve health and that the administration of a single or a few organic foods within the habitual diet would probably not reveal any beneficial effect, we undertook the present study to explore the effects of the Italian Mediterranean organic diet (IMOD) versus the low-protein diet (LPD) on chemical–clinical parameters and body composition in CKD patients, according to the C677T MTHFR polymorphism.
Subjects and methods
Study population
In order to avoid potential confounding factors following menstrual cycle hormone fluctuations, we excluded women from the study. A total of 50 male patients (mean age 46.25 ± 5.97 years; range 42–54) with CKD and stable renal function [stages 2 and 3 according to the Kidney Disease Outcomes Quality Initiative (K-DOQI) 2003 classification] were recruited from the Department of Internal Medicine, Hypertension and Nephrology Unit, “Tor Vergata” University Hospital, Rome (Italy) according to the level of kidney function. We selected 40 patients with GFR <70 and >45 ml/min corresponding to stages 2 and 3 CKD of K-DOQI 2003 [14]. The causes of primary renal failure were chronic glomerulonephritides. All patients were managed with standard conservative treatment. Participation in the study included a complete medical history to gather information on health status, current medications including supplements of vitamins and minerals, alcohol consumption, smoking, physical activity (PA) and family history of chronic diseases. Data on PA were collected using a simple questionnaire that grades the level of PA into five categories (sedentary, light, moderate, heavy and agonistic) based on the time spent in activities of daily living on programmed physical exercise. No change of total energy intake (kcal/die) was required during the course of the study, nor was there any change in subjects’ physical activity during the study, and no change in resting metabolic rate (RMR) was expected.
The subjects were categorized into body mass index (BMI) subgroups according to World Health Organization (WHO) criteria [15–17]. Moreover, gender and age were also used to classify the total population. Patients were classified based on carrier status for the MTHFR polymorphism as: carrier T(+) or non carrier T(−).
All patients gave their informed consent before entering the study. The protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki, and was approved by the “Tor Vergata” University Medical Ethical Committee, Rome, Italy.
Diet assessment
Compliance was assessed by 3-day diet records (3DDRs) completed during the study. Participants were asked to complete a 3-day weighed diet record including 2 weekdays and 1 weekend day at baseline and after 7 days of dietary intervention. Detailed instruction on how to collect diet records was verbally given to each participant by a trained researcher. Written instructions were also included in the 3DDR booklet provided. A researcher reviewed all 3DDRs upon return for completeness and accuracy.
Low protein diet (LPD)
In CKD, nutritional therapy means designing diets to reduce the patient’s intake of proteins, phosphorus and sodium, while preserving adequate energy intake. Different nutritional strategies can be devised according to the protein needs of the patient [18]. At the time of enrolment (T0) our patients had been following a diet with controlled protein intake [recommended dietary allowance (RDA) 0.7 g/kg/day of protein] and low-phosphorus intake (phosphorus 300–400 mg/day) for 6 months. The potential renal acid load index was −10.39 mEq/100 g [19]. The sodium chloride content of the LPD was kept between 2 and 5 g/day according to individual needs. The energy intake was 2,000 kcal/day.
The macronutrient composition of the dietary regimen was as follows: carbohydrates, 50.2 % kcal/day; proteins, 12.8 % kcal/day; total fat, 29.3 % kcal/day [saturated fat 14.34 g; polyunsaturated fatty acids (PUFA) 8.06 g: 5–6 % of n-6 PUFA and 1–2 % of n-3 PUFA; monounsaturated fatty acids (MUFA), 38.47 g; cholesterol consumption of 160 mg/day], 17.2 g of fibre, folic acid 328 mcg, pyridoxine 1.4 mg, cyanocobalamin 2.1 mg per day. No alcoholic beverages were allowed except 100 ml/day of red wine (7.7 % kcal/day). The plan for each subject was obtained from a dietetic software package (Dietosystem, DS Medica, Milan, Italy).
Italian Mediterranean diet (IMD) and Italian Mediterranean organic diet (IMOD)
For 14 days (T1) all selected subjects consumed conventional products according to the IMD, the so-called Nicotera diet [20, 21]. Following this, for a further 14 days (T2) they followed an exclusively “organic” diet, according to the IMOD [22, 23]. The potential renal acid load index was −10.47 mEq/100 g [19]. The sodium chloride content of LPD was kept between 2 and 5 g/day according to individual needs. The energy intake was 2,000 kcal/day.
The macronutrient composition of the dietary regimen was as follows: carbohydrates, 54.75 % kcal/day; proteins, 14.9 % kcal/day (0.9 g/kg/day); total fat, 22.65 % kcal/day (saturated fat 14.07 g; PUFA 6.62 g: 5–6 % of n-6 PUFA and 1–2 % of n-3 PUFA; MUFA, 32.55 g; cholesterol consumption of 147.83 mg/day), 30.16 g of fibre, folic acid 421.60 mcg, pyridoxine 1.82 mg, cyanocobalamin 2.79 mg per day. No alcoholic beverages were allowed except 100 ml/day of red wine (7.7 % kcal/day). The plan for each subject was obtained from a dietetic software package (Dietosystem, DS Medica, Milan, Italy). The only differences in composition between IMD and IMOD were: folic acid >450 mcg, pyridoxine 2.18 mg and cyanocobalamin 3.38 mg per die. The Italian RDA were incorporated to ensure adequate vitamin and mineral intake [24]. The potassium intake met the dietary reference intakes of the Institute of Medicine of the National Academies, Washington, DC, USA. The IMD and IMOD were evaluated by a dietetic software package (DS Medigroup, Milan, Italy).
MTHFR genotype
Genomic DNA was extracted from peripheral whole blood using the QIAamp DNA Mini Kit (Quiagen, Valencia, CA, USA). MTHFR was selected for genotyping. The C677T polymorphism of the MTHFR gene was screened by the restriction fragment–length polymorphism after digestion with HinfI restriction enzyme, as previously described [7]. The TT and the CT genotypes were grouped and indicated as T carriers T(+), while the CC genotype were named as T non carriers T(−). Among the general European population, genotype frequencies are: CC = 45 %, CT = 45 %, TT = 10 %. The genotype distribution observed in European hemodialysis patients was: CC 51.2 % (n = 41), CT 37.5 % (n = 30) and TT 11.2 % (n = 9).
Anthropometric measurements
Anthropometric parameters were measured according to standard methods [25]. BMI was calculated as body weight divided by height squared (kg/m2).
Dual X-ray absorptiometry (DXA)
The total body composition was assessed by DXA (iDXA, G.E. Medical Systems, WI, USA), according to the previously described procedure [26]. The coefficient of variation (CV) (standard deviation [SD]/mean) for repeated measurements is 1.0–2.2 % in our laboratory depending on the application. Subjects were classified as pre-obese/obese according to a World Health Organization (WHO) Technical Report and a WHO Technical Report Series [27, 28].
Analysis of blood samples
Fasting blood samples were collected, and analyzed according to standard techniques by the accredited Clinical Chemical Laboratories of the “Tor Vergata” Policlinico (PTV) of Rome, Italy.
GFR estimation
The estimated GFR (e-GFR) was calculated using the CKD epidemiology collaboration (CKD-EPI) formula [29].
Statistical analysis
The main aim of the study was to analyze whether the presence of the MTHFR C677T polymorphism would modify the effect of two different diets, IMD and IMOD, on circulating levels of homocysteine. Repeated measurements for each patients were analyzed with the use of random-intercept linear mixed models with homocysteine as the dependent variable; the effect modification by MTHFR status on the prescribed diet was investigated by including in the model an interaction term between MTHFR status and diet. Marginal means and differences with 95 % confidence intervals (CI) were estimated from the model, using the LPD as reference, and reported according to MTHFR status.
We also analyzed the main effects of the IMD and IMOD on a number of other anthropometric and laboratory variables with random-intercept linear mixed models with each measured parameter as dependent variable and diet as explanatory variable. For these analyses, we chose a conservative approach and only looked at contrasts between LPD and IMD and IMOD when the overall test for the effect of diet was statistically significant. Furthermore, to avoid over-inflation of the type I error from multiple testing, the Bonferroni correction was applied: with 12 pre-planned comparisons, the corrected p value for statistical significance was fixed at p = 0.004.
A χ 2 test was also used to evaluate the Hardy–Weinberg equilibrium of the observed genotype frequencies with respect to the general population. The level of significance was fixed at p ≤ 0.05 for all procedures. Statistical analysis was performed using computer software packages (SPSS for Windows, version 13.0, SPSS, Chicago, IL, USA; and Stata version 12.1, StataCorp, TX, USA).
Results
Among 50 Caucasian Italian males subjects recruited for the study, 7 were excluded at screening (two had prostate cancer and five were diabetic), and 3 were withdrawn for missing data in some of the variables considered. Thus, a total of 40 subjects completed the study, and their data were eligible for data analysis. The demographic and clinical characteristics of the participants are presented in Table 1.
The distribution of the MTHFR genotypes in our study group was compatible with the Hardy–Weinberg equilibrium (p ≤ 0.05). The T allele frequency was 45 %, and the CC, CT, and TT genotype frequencies were 55 % (n = 22), 35 % (n = 14), and 10 % (n = 4), respectively. The T allele frequency in our sample was similar to that in other white populations [30].
The degree of compliance was high in all groups but was greater in LPD (99.5 %) than IMOD (98.4 %) and IMD (94.6 %) (p = 0.05). However the degree of palatability was higher in IMOD (99.4 %) and IMD (94.6 %) than in LPD (60.0 %) (p = 0.05).
Baseline homocysteine levels were on average 8.24 mol/l higher (95 % CI 6.47, 10.00) among T(+) participants than T(−) and the difference was statistically significant (p < 0.001). We found a significant effect modification of MTHFR status on the effect of both the IMD and IMOD on homocysteine levels compared with that of the LPD (p for interaction <0.001). In particular, among T(−) patients homocysteine levels for IMD did not differ significantly from LPD (average difference −0.25 mol/l, 95 % CI −1.92, 1.43; p = 0.77), whereas they were significantly lower for IMOD (average difference −2.17 mol/l, 95 % CI −3.85, −0.49; p = 0.01). Conversely, among T(+) patients homocysteine levels were significantly lower, with respect to LPD, for both IMD (average difference −3.08 mol/l, 95 % CI −4.94, −1.23; p = 0.001) and IMOD (average difference −9.18 mol/l, 95 % CI −11.04, −7.33; p < 0.001). Compared with IMD, homocysteine levels after IMOD were lower for both T(−) patients (average difference −1.92 mol/l, 95 % CI −3.60, −0.24; p = 0.03) and T(+) patients (average difference −6.10 mol/l, 95 % CI −7.96, −4.24; p < 0.001). The relationships between diet and MTHFR status on homocysteine levels are illustrated in Fig. 1.
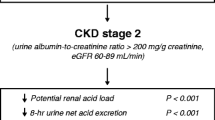
Since we did not find any significant interaction between MTHFR status and diet on the other measured variables, we only report the main effects of each diet without further stratification for MTHFR status. Since the overall test for differences between diets was statistically significant for all the measured parameters, we performed paired comparisons between diets for each parameter (Table 2). The e-GFR during the entire study period did not change significantly.
Discussion
Several studies have found that adherence to IMD, for its particular combination of micro- and macronutrients, is associated with beneficial effects on metabolic syndrome, cardiovascular disease, and major chronic degenerative diseases, reducing the overall and cardiovascular mortality, and with improved weight management [31–34]. Our results demonstrate that the administration of IMOD, according to the Nicotera diet guideline, is associated with a variety of benefits in CKD patients. This study, for the first time, describes an important gene–environment interaction in CKD patients, providing evidence of an interaction between a genetic variant of MTHFR, the C677T polymorphism, and a balanced IMD/IMOD nutritional intervention and its influence on biochemical values, anthropometric and body composition parameters.
The variant homozygous genotype of MTHFR affects genomic DNA methylation through an interaction with folate [35] and it is associated with elevated plasma homocysteine levels [36–39]. Moreover, as proposed by Lambrinoudaki et al. [40], the genetic variants affecting Hcy metabolism may result in impaired tHcy catabolism which, at a cellular level, may lead to tissue dysfunction thus causing metabolic disturbances and related body composition modification. Because of the association of MTHFR C677T polymorphism with cardiovascular disease risk [41] osteoporosis and sarcopenia [42], we considered the T(+) carriers as ‘at risk’ subjects.
The IMOD was associated with significant changes in body composition of all patients, despite no alteration in total energy intake (kcal/day), physical activity and life style during the course of the study. In particular, the effect of the nutritional interventions was associated with significant changes in body composition, e.g. a significant reduction of total body (TB)Fat (p < 0.05) and BMI (p < 0.05), and a significant increase of TBLean (p < 0.05). The enhancement of TBLean is directly correlated to the increase of body cell mass and, consequently, of the resting metabolic rate. Therefore, while prescribing an isocaloric diet we observed a significant weight loss, in terms of BMI and TBFat, during IMD and IMOD diets compared to the LPD.
Liu et al. [42] recently demonstrated that MTHFR gene variants are associated with lean mass, sustaining findings linking genetic determination of BMI and lean mass to chromosome 1p36, where the MTHFR gene is located. Moreover, epidemiological studies have found that tHcy correlates with lean mass and BMI [43]. Although further biochemical studies are needed to elucidate the molecular mechanisms that underlie and explain the relationship between MTHFR, TBFat and TBLean, herein we have highlighted a significant reduction of tHcy levels in T(+) carriers, combined with a reduction of TBFat, and an increase of TBLean after IMOD nutritional intervention.
Moreover, the increase in muscle mass following the IMOD nutritional intervention could mean a reduction in risk of sarcopenia for CKD patients. Reduction in lean body mass per se is an important risk factor for sarcopenia, a serious health problem that has not yet received sufficient attention. Sarcopenia is a syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength with a risk of adverse outcomes such as physical disability, poor quality of life, and increased morbidity and mortality [44]. It has been demonstrated that the MTHFR gene is highly expressed in skeletal muscle, and the formation of muscles is associated with the simultaneous formation of homocysteine in connection with creatine/creatinine synthesis [45]. The recovery of muscle mass and the simultaneous reduction of tHcy and of other risk factors such as total cholesterol, phosphate and albuminuria levels, confirm the higher quality of the IMOD nutritional intervention in comparison to recommended dietary plans.
In 1989, the National Authorities of USA together with an expert advisory group of academic nephrologists sponsored and conducted a multicenter prospective study known as the modification of diet in renal disease (MDRD) study, in order to test the hypothesis that restricting dietary protein and lowering blood pressure could slow the progression of renal disease among 1,840 patients with various stages of chronic kidney disease. The results of this study, published in 1994, showed that dietary protein restriction had a slight beneficial effect on declining renal function only in patients with moderate renal disease and the benefit of lowering blood pressure was only seen in patients with albuminuria greater than one gram per day [46].
Although low-protein diets have often been recommended as a means of slowing the progression of CKD [47, 48], adherence to these diets is poor because of the lack of variety in menus and the limitations on consumption of many foods [49]. Moreover, reduced food intake in these patients often worsens the situation and increases the chances of inadequate intake of micronutrients such as folate and vitamins B6 and B12, abundant in protein-rich foods [50, 51]. These vitamins are known to be involved in the metabolism of homocysteine, with deficient levels favoring hyperhomocysteinemia. This cardiovascular risk factor is particularly worrisome in patients with CKD. In patients with uremia the mortality rate attributable to cardiovascular disease is 30 % higher than in the general population, and hyperhomocysteinemia is the most prevalent risk factor [52].
Recently, the recognition of phosphate as an independent risk factor for cardiovascular disease even among non chronic kidney disease patients, as well as a risk factor for rapid deterioration of renal function among dialysis patients and experimental animals, set the investigation in another direction independent of protein diet and energy consumption. Moreover, the recent discovery of the critical role of FGF-23 and Klotho protein in phosphate homeostasis indicate the possibility that inorganic phosphate may be a toxic element for blood vessels, heart and kidneys [53–55].
In our study, we demonstrated a significant reduction of hyperphosphatemia after both diets, associated with an improvement in the lipid profile, which suggests less need of lipids for endothelial cell repair, and a lower risk for CVD. Albuminuria reflects a generalized impairment of endothelium and represents a marker of increased cardiovascular risk and of progression of renal failure [56]. In our study, at T2, in CKD patients, there was a significant reduction of albuminuria.
A limitation of this study is the relatively small sample size. However, it was large enough to provide us with adequate statistical power. Another limitation is the short time of observation, although this would have counterbalanced the frequently observed phenomenon of low compliance to dietary instructions. A further limitation is the potential carryover from one diet to another, that could have potentially biased our results. It is important to note that subjects experienced the most dramatic weight loss during the first quarter of the meal plan, because they were very compliant to the administered diet. Thus, in our study the IMD and IMOD nutritional interventions were programmed for a duration of only 2 weeks respectively, in order to reveal the true impact on weight loss, body composition and laboratory parameter changes.
Our data also provide a basis for personalized dietary recommendations based on the individual’s genetic makeup and information from other factors such as body composition and biochemical values, in the context of a nutritional intervention assigned to CKD patients.
In conclusion, our data highlight that a dietary pattern rich in some beneficial food groups such as fruit and vegetables, from organic agricultural practice, can reduce the incidence of cardiovascular disease risk in CKD subjects, reducing fasting baseline phosphate, total cholesterol concentrations, and albuminuria. In particular, with regard to the MTHFR polymorphism, we observed a significant reduction of tHcy in T(+) carriers after IMD and in both genotypes after IMOD. This may lead to a lower incidence of CVD and could be of particular significance in CKD patients. We suggest that IMOD may play a role in longevity and quality of life of CKD patients, pointing towards the beneficial value of organic food consumption.
Furthermore, prescription of IMOD may represent an appropriate primary therapeutic option for the global CVD risk prevention, in particular in CKD patients on conservative therapy, in line with recommendations of the Italian Pharmaceutical Agency (Agenzia Italiana del Farmaco, AIFA) note n.13 guidelines (D.G.R. 1209/2002), the National Cholesterol Education Program (NCEP), the American Heart Association (AHA), and the Therapeutic Lifestyle Change (TLC) [57].
References
Foley RN, Parfrey PS, Samak MJ (1998) Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32(5 Suppl 3):S112
Pastore A, De Angelis S, Casciani S et al (2006) Effects of folic acid before and after vitamin B12 on plasma homocysteine concentrations in hemodialysis patients with Known MTHFR Genotypes. Clin Chem 52(1):145–148
Busch M, Franke S, Muller A et al (2004) Potential cardiovascular risk factors in chronic kidney disease: AGEs, Total homocysteine and metabolites, and the C-reactive protein. Kidney Int 66:338–347
Zhang X, Li H, Jin H, Ebin Z, Brodsky S et al (2000) Effects of homocysteine on endothelial nitric oxide production. Am J Physiol Renal Physiol 279(4):F671–F678
Zou T, Yang W, Hou Z, Yang J (2010) Homocysteine enhances cell proliferation in vascular smooth muscle cells: role of p38 MAPK and p47phox. Acta Biochim Biophys Sin (Shanghai) 42(12):908–915. doi:10.1093/abbs/gmq102. Epub 2010 Nov 10
Malinowska J, Olas B (2011) Analysis of biological properties of selected elements of haemostasis after treatment with the oxidized form of homocysteine in vitro. Platelets 22(8):629–632. doi:10.3109/09537104.2011.579204. Epub 2011 May 31
Frosst P, Blom HJ, Milos R et al (1995) A candidate genetic risk factor for vascular disease : a common mutation in methylentetrahydrofolatereductase. Nat Genet 10:111–113
Rady PL, Szucs S, Grady J et al (2002) Genetic polymorphisms of methylenetetrahydrofolate reductase (MTHFR) and methionine synthase reductase (MTRR) in ethnic populations in Texas; a report of a novel MTHFR polymorphic site, G1793A. Am J Med Genet 107(2):162–168
Winkelmayer WC, Huber A, Wagner OF et al (2005) Associations between MTHFR 1793 G>A and plasma total homocysteine, folate, and vitamin B12 in kidney transplant recipients. Kidney Int 67:1980–1985
Chrysohoou C, Panagiotakos DB, Pitsavos C et al (2004) Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: the ATTICA study. J Am Coll Cardiol 44:152–158
Knoops KT, de Groot LC, Kromhout D et al (2004) Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA 292:1433–1439
Esposito K, Marfella R, Ciotola M et al (2004) Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 292:1440–1446
Di Renzo L, Di Pierro D, Bigioni M et al (2007) Is antioxidant plasma status in humans a consequence of the antioxidant food content influence? Eur Rev Med Pharmacol Sci 11:185–192
K-DOQI (2004) Clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis 43(5 Suppl 1):S1–S290
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation, WHO technical report series 894, Geneva, Switzerland
Parodi E, De Lorenzo A (2009) I disturbi del comportamento alimentare. Collana Universalia Enpam, vol 6
De Lorenzo A, Bianchi A, Maroni P et al (2013) Adiposity rather than BMI determines metabolic risk. Int J Cardiol 166(1):111–117. doi:10.1016/j.ijcard.2011.10.006
Cupisti A (2008) Definition of the nutritional therapy in the conservative treatment of chronic kidney disease. G Ital Nefrol 25(Suppl 42):S35–S38
Remer T, Manz F (1995) Potential renal acid of foods and its influence on urine pH. J Am Diet Assoc 95:791–797
Fidanza F, Alberti A, Fruttini D (2005) The Nicotera diet: the reference Italian Mediterranean diet. World Rev Nutr Diet 95:115–121
De Lorenzo A, Petroni ML, De Luca PP et al (2001) Use of quality control indices in moderately hypocaloric Mediterranean diet for treatment of obesity. Diabetes Nutr Metab 14(4):181–188
Di Renzo L, Di Pierro D, Bigioni M et al (2007) Is antioxidant plasma status in humans a consequence of the antioxidant food content influence? Eur Rev Med Pharmacol Sci 11:185–192
De Lorenzo A, Noce A, Bigioni M et al (2010) The effects of Italian Mediterranean organic diet (IMOD) on health status. Curr Pharm Des 16(7):814–824
LARN—Livelli di Assunzione di Riferimento di Nutrienti ed energia per la popolazione italiana. Revisione 2012. Documento di sintesi per il XXXV Congresso Nazionale SINU Bologna, 22–23 ottobre 2012
Lohman TG, Roche AF, Martorell R (1998) Anthropometric standardization reference manual. Human Kinetics, Champaign, IL, pp 3–8, 39–70
De Lorenzo A, Andreoli A, Candeloro N (1997) Within-subject variability in body composition using dual-energy X-ray absorptiometry. Clin Physiol 17:383–388
Word Health Organ Tech Rep Ser (2003) Diet, nutrition and the prevention of chronic diseases 916:1–149
Parodi E, De Lorenzo A. Diet, nutrition and prevention of chronic diseases. Geneva: WHO Technical Report Series; 2003. no. 916. www.enpam.it
Florkowski CM, Chew-Harris JS (2011) Methods of estimating GFR—different equations including CKD-EPI. Clin Biochem Rev 32(2):75–79
Dedoussis GV, Panagiotakos DB, Chrysohoou C et al (2004) Effect of interaction between adherence to a Mediterranean diet and the methylenetetrahydrofolate reductase 677C→T mutation on homocysteine concentrations in healthy adults: the ATTICA Study. Am J Clin Nutr 80(4):849–854
Sofi F, Abbate R, Gensini GF, Casini A (2010) Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 92(5):1189–1196. Epub 2010 Sep 1. Review
De Lorenzo A, Andreoli A, Sorge RP et al (1999) Modification of dietary habits (Mediterranean diet) and cancer mortality in a southern Italian village from 1960 to 1996. Ann NY Acad Sci 889:224–229
Kastorini CM, Milionis HJ, Esposito K et al (2011) The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol 57(11):1299–1313
Esposito K, Di Palo C, Maiorino MI et al (2010) Long-term effect of mediterranean-style diet and calorie restriction on biomarkers of longevity and oxidative stress in overweight men. Cardiol Res Pract 20(2011):293916. doi:10.4061/2011/293916
Friso S, Choi SW, Girelli D et al (2001) A common mutation in the 5,10 methylenetetrahydrofolate reductase gene affects genomic DNA methylation through an interaction with folate status. Proc Natl Acad Sci USA 99:5606–5611
Guinotte C, Burns M, Axume J et al (2003) Methylenetetrahydrofolatereductase 677C→T variant modulates folate status response to controlled folate intakes in young women. J Nutr 133:1272–1280
De Bree A, Verschuren WMM, Bjorke-Monsen Al, Van Der Put NMJ, Heil SG, Trijbels FJM, Bloom HJ (2003) Effect of the methylenetetrahydrofolate reductase 677C→T mutation on the relations among folate intake and plasma folate and homocysteine concentration in general population sample. Am J Clin Nutr 77:687–693
Brattstrom L, Wilcken DE (2000) Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr 72:315–323
Di Renzo L, Bigioni M, Bottini FG et al (2006) Normal weight obese syndrome: role of single nucleotide polymorphism Of Il-15rα and MTHFR 677C>T genes in the relationship between body composition and resting metabolic rate. Eur Rev Med Pharmacol Sci 10(5):235–245
Lambrinoudaki I, Kaparos G, Papadimitriou D et al (2008) Methylenetetrahydrofolate reductase C677T polymorphism is associated with central adiposity and increased androgenicity in healthy postmenopausal women. Eur J Endocrinol 159(3):233–241
Lewis SJ, Ebrahim S, Davey Smith G (2005) Meta-analysis of MTHFR 677C→T polymorphism and coronary heart disease: does totality of evidence support causal role for homocysteine and preventive potential of folate. BMJ 331:1053–1056
Liu X, Zhao LJ, Liu YJ, Xiong DH, Recker RR, Deng HW (2008) The MTHFR gene polymorphism is associated with lean body mass but not fat body mass. Hum Genet 123(2):189–196 Epub 2008 Jan 8
Gorlova OY, Amos CI, Wang NW et al (2003) Genetic linkage and imprinting effects on body mass index in children and young adults. Eur J Hum Genet 11:425–432
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in older people. Age Ageing 39(4):412–423. doi:10.1093/ageing/afq034. Epub 2010 Apr 13
Shmueli O, Horn-Saban S, Chalifa-Caspi V et al (2003) Gene Note: whole genome expression profiles in normal human tissues. C R Biol 326:1067–1072
Klahr S, Levey AS, Beck GJ et al (1994) The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. For the Modification of Diet in Renal Disease Study Group. N Engl J Med 330:877–884
Chazot C, Kopple JD (1997) Vitamin metabolism and requirements in renal disease and renal failure. In: Kopple JD, Massry SG (eds) Nutritional management of renal disease. Williams and Wilkins, Baltimore, pp 415–478
Beto JA, Fada RD, Bansal VK (2004) Medical nutrition therapy in chronic kidney failure: integrating clinical practice guidelines. J Am Diet Assoc 104:404–409
Johnson DW (2006) Dietary protein restriction as a treatment for slowing chronic kidney disease progression: the case against. Nephrology 11:58–62
Menon V, Wang X, Greene T et al (2005) Homocysteine in chronic kidney disease: effect of low protein diet and repletion with B vitamins. Kidney Int 67(4):1539–1546
Chien SC, Li SY, Chen YT et al (2013) Folic acid supplementation in end-stage renal disease patients reduces total mortality rate. J Nephrol 26(6):1097–1104. doi:10.5301/jn.5000276
Bostom AG, Lathrop L (1997) Hyperhomocysteinemia in end-stage renal disease: prevalence etiology, and potential relationship to arteriosclerotic outcomes. Kidney Int 52:10–20
Voormolen N, Noordzij M, Grootendorst DC et al (2007) Phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant 22:2909–2916
Kanbay M, Goldsmith D, Akcay A et al (2009) Phosphate—the silent stealthy cardiorenal culprit in all stages of chronic renal disease. Blood Purif 27:220–230
Komaba H, Fukagawa M (2009) FGF23: a key player in mineral and bone disorder in CKD. Nefrologia 29:392–396
Helimi JM, Hadjadj S, Aboyans V et al (2008) Microalbuminuria and urinary albumin excretion: French guidelines. Ann Biol Clin (Paris) 66:277–284
Lichtenstein AH, Ausman LM, Jalbert SM et al (2002) Efficacy of a therapeutic lifestyle change/step 2 diet in moderately hypercholesterolemic middle-aged and elderly female and male subjects. J Lipid Res 43:264–273
Acknowledgments
N.D.D, L.D.R. and N.A. designed the research and wrote the paper; M.R., F.S., E.D., L.I. conducted the research; N.A,.PM.F. and F.S. analyzed the data; A.D.L. had primary responsibility for the final content. All authors read and approved the final manuscript. This study was supported by grants from Ministero Politiche Agricole e Forestali, and Istituto Nazionale per la Dieta Mediterranea e la Nutrigenomica (I.N.DI.M): SABIO, D.M. 908001 May 26, 2004 and PACB, D.M. 91567 Dic 29, 2004. The authors thank Dr. Caius Gavrila for his contribution to the study.
The authors have no financial or personal interests in any organization sponsoring the research at the time the research was done.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Daniele, N., Di Renzo, L., Noce, A. et al. Effects of Italian Mediterranean organic diet vs. low-protein diet in nephropathic patients according to MTHFR genotypes. J Nephrol 27, 529–536 (2014). https://doi.org/10.1007/s40620-014-0067-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-014-0067-y