Abstract
Aim
To explore the specific association between sarcopenia and prediabetes based on large population samples.
Methods
A total of 16,116 U.S. adults aged 20–59 with dual energy X-ray absorptiometry (DXA) was identified from the National Health and Nutrition Examination Surveys (NHANES). Sarcopenia was defined according to appendicular skeletal muscle mass (ASM) adjusted for body mass index (BMI). Multivariable binary logistic regression models were used to ascertain odds ratios (ORs) for developing prediabetes. Stratified analyses were also performed.
Results
Prevalence of prediabetes was higher in the sarcopenia group (n = 1055) compared with the non-sarcopenia group (n = 15,061) (45.50% vs 28.74%, P < 0.001). Sarcopenia was strongly associated with an increased risk of prediabetes after full adjustment (OR = 1.21, 95CI%: 1.05, 1.39, P = 0.009). In the stratified analysis, this association remained significant independent of obesity, triglycerides, and low-density lipoprotein cholesterol levels. When sarcopenia subjects combined with obesity especially central obesity, the risk of prediabetes was the highest (OR = 2.63, 95CI%: 2.22, 3.11, P < 0.001). Furthermore, a greater proportion of any of impaired glucose tolerance (IGT) individuals was observed in the sarcopenia group compared to the non-sarcopenia group among prediabetes population (41.72% vs 24.06%, P < 0.001).
Conclusions
Sarcopenia was positively associated with prevalent prediabetes especially IGT in the non-elderly. Moreover, synergistic interactions between the sarcopenia and obesity could greatly increase the risk of prediabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the prevalence of prediabetes has shown a clear increasing trend. Up to 38% of U.S. adults could be diagnosed as prediabetes during 2017–2020 based only on fasting plasma glucose (FPG) and hemoglobin A1c (HbA1c) levels [1]. It is anticipated that around 470 million people will have prediabetes by 2030 [2]. A larger population with prediabetes is not only associated with rapid progression of diabetes mellitus (DM) and its complications [3,4,5] but also with high risk of cardiovascular disease, cognitive dysfunction, neoplasia, and mortality [2, 6, 7]. Hence, as a typical metabolic disease, identification of its risk factors and prompt intervention are important.
In addition to the known classical risk factors of metabolic diseases such as hypertension, hyperlipidemia and obesity, increasing attention has recently been paid to the effect of skeletal muscle. Skeletal muscle, as the largest target organ for insulin action, is involved in energy metabolism in the whole body. Growing studies have proven that skeletal muscle loss, commonly known as sarcopenia, plays an essential role in the development of various metabolic diseases. Sarcopenia manifests as age-related loss of muscle mass, muscle strength, and function [8]. Although sarcopenia is most common among the elderly, with changes in modern lifestyle, its occurrence has gradually shown a younger trend [9]. Sarcopenia could exacerbate insulin resistance and become an independent risk factor for many diseases, including DM, metabolic syndrome, osteoporosis, and non-alcoholic fatty liver disease [10,11,12,13]. However, the specific association between sarcopenia and prediabetes risk still remains to be elucidated with a larger sample population.
Dual-energy X-ray absorptiometry (DXA) is a relative ideal measurement method for diagnosing sarcopenia. Therefore, based on the aforementioned researches, this study aimed to clarify the association between prediabetes and sarcopenia evaluated by DXA. Furthermore, since obesity is a critical risk factor for prediabetes and closely associated with sarcopenia, we will also explore the joint effects of obesity and sarcopenia on prediabetes.
Methods
Study participants
Our study population was all drawn from the National Health and Nutrition Examination Surveys (NHANES) (1999–2006 and 2011–2018) since the primary variable dual energy X-ray absorptiometry (DXA) are included only in these data cycles. A total of 18,839 participants aged 20–59 years and with complete DXA data were studied. Next, we excluded partial population as follows: (1) participants with prior cancer diagnoses (n = 592); (2) participants with severe renal dysfunction (estimate glomerular filtration rate (eGFR) < 30 ml/min/1.73m2, n = 32); (3) participants with macroalbuminuria (ACR ≥ 300 mg/g, n = 218); (4) participants with abnormally energy intakes (< 500 or > 5000 kcal/day, n = 224); (5) participants diagnosed with diabetes mellitus (n = 1831). Finally, data of 16,116 participants were enrolled for the statistical analysis. See Fig. 1 for the flow diagram.
DXA assessments and definition of sarcopenia
Whole body DXA scans were taken with a Hologic QDR-4500A fan-beam densitometer (Hologic, Inc., Bedford, Massachusetts). Participants who were pregnant, obese (> 136 kg), tall (> 196 cm), and administrated with radiographic contrast material (barium) in past 7 days were unable to attend the DXA examination. Appendicular skeletal muscle mass (ASM) was defined as the sum of the bone-free lean mass of both arms and legs. Afterwards, ASM was divided by body mass index (BMI) to further define sarcopenia. Since the target population in our study was U.S. adults from NHANES, we used the National Institutes of Health (NIH) definition of sarcopenia (ASM/BMI < 0.789 for men and < 0.512 for women) [14].
Definition of prediabetes
Prediabetes was defined according to the American Diabetes Association (ADA) guidelines (2021) [15]. The diagnosis was confirmed when any one of the following criteria is met: (1) fasting plasma glucose (FPG) 100–125 mg/dL (5.6–6.9 mmol/L); (2) 2 h plasma glucose (2hPG) 140–199 mg/dL (7.8–11.0 mmol/L); (3) glycated hemoglobin A1c (HbA1c) 5.7–6.4% (39–47 mmol/mol). Prediabetes patients can be further classified as isolated impaired fasting glucose (i-IFG), isolated impaired glucose tolerance (i-IGT), and combined IFG and IGT. Any IFG and any IGT was considered any participants with IFG or IGT.
Other variables
Categorical variables were defined based on relevant guidelines and literature. Smoking status was divided into three categories through self-report (current, past, and never smokers) [16]. The consumption of alcohol was dichotomized on the basis of having at least 12 drinks per year. Poverty–income ratio (PIR) was stratified into three categories [17]: ≤ 1 (≤ 100% of the poverty threshold), 1–3 (100–300% of the poverty threshold), > 3 (> 300% of the poverty threshold). Total physical activity (PA) was calculated as the sum of the metabolic equivalents (METs) of three activity types (work/task activity, activities related to transportation, and muscle strengthening/recreational activities) per week. Then, participants were classified as recommended in the Physical Activity Guidelines for Americans (< 500 MET-min/week; ≥ 500 MET-min/week) [18]. Hypertension, hypercholesterolemia, and cardiovascular disease (CVD) were defined by subject self-report. Obesity was characterized by three common criteria: (1) BMI ≥ 30 kg/m2; (2) waist circumference > 102 cm for men and > 88 cm for women; (3) highest quintile of body fat percent (BF%) assessed using DXA [19]. Obesity with low lean muscle mass (OLLMM) were also defined for the both presence of sarcopenic and obesity, and the participants were categorized into four groups: normal, only sarcopenic, only obesity, and OLLMM.
Partial continuous variables were calculated using the standard formulas. Homeostatic model for assessment of insulin resistance (HOMA-IR): fasting serum insulin (μU/mL) × fasting plasma glucose (mmol/L)/22.5). Estimate glomerular filtration rate (eGFR) was estimated by the Modification of Diet in Renal Disease (MDRD) formula: 175 × standardized (serum creatinine, mg/dl) −1.154 × age−0.203 × 1.212 [if African American] × 0.742 [if female]. Data on energy intake were calculated as proportion of energy from the total energy intake (grams of each nutrient × energy coefficient / total energy × 100).
Statistical analysis
Given the complex sampling design of NHANES, all analyses were performed according to analytic guidelines using R (v.3.4.3) software packages and EmpowerStats software (http://www.empowerstats.com/en/). Continuous variables are expressed as weighted mean ± standard error and categorical variables as number and percentage. A chi-square test was conducted to compare the prevalence of prediabetes among different groups. Logistic regression models were used to assess the association between sarcopenia and risk of prediabetes. Four models were created to adjust for confounding factors in a stepwise manner. The variables incorporated into multivariable models were either demographic and socioeconomic factors or established risk factors for prediabetes [20, 21]. Model 1 was unadjusted. Model 2 was adjusted for sociodemographic factors, including age, sex, race, PIR, and educational level. Model 3 was further adjusted for lifestyle factors, including smoking status, alcohol consumption, total energy intake, carbohydrate intake, and PA. Model 4 was additionally adjusted for metabolic risk factors, including CVD, BMI, triglycerides (TG), total cholesterol (TC), systolic blood pressure (SBP), and eGFR. Age, total energy intake, carbohydrate intake, BMI, TG, TC, SBP and eGFR were adjusted as continuous variables, other variables were entered into the models as categorical variables, all variables are detailed in Table 1. Moreover, considering that obesity, hypertension, and lipid disorders are the established risk factors for both prediabetes and diabetes, analyses stratified according to BMI, waist circumference, SBP, DBP, TC, TG, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were performed to determine the independent effect of sarcopenia on prediabetes. In addition, we further screened the prediabetes population with complete glucose data from the 16,116 participants. Chi-square tests were used to compare the prevalence rates of prediabetes types (IFG, IGT, combined IFG and IGT, any IFG, and any IGT) between the sarcopenia group and the non-sarcopenia group. Statistical significance was set at P < 0.05 (two-tails).
Results
Participant characteristics
Baseline characteristics of the participants are shown by the presence or absence of sarcopenia (Table 1). As expected, the weighted mean age and standard error of sarcopenia group was 41.87 ± 0.42, and significantly older than the non-sarcopenia group (37.79 ± 0.18). Sarcopenia group presented a higher proportion of males and obese subjects. In addition, we observed higher levels of blood pressure, lipids, blood glucose, and lower levels of education, socioeconomic, PA, and total energy intake in sarcopenia participants (P < 0.001). However, sarcopenia group had lower proportions of current smokers (18.48% vs 22.91%) and alcoholic drinkers (58.39% vs 69.44%).
Associations between sarcopenia and prediabetes
The prevalence of prediabetes was 45.50% in sarcopenia group and 28.74% in non-sarcopenia group, Group differences in prevalence are shown in Fig. 2A for visualization. Subsequently, four models were established to elucidate the association between sarcopenia and the risk of prediabetes. In the unadjusted Model 1, compared to the non-sarcopenia participants, the sarcopenia group showed a significantly higher risk of prediabetes (OR = 2.07, 95CI%: 1.82, 2.35, P < 0.001). With progressive adjustment for covariates, the effect of sarcopenia on the risk of incident prediabetes was gradually reduced. However, statistically significant differences were consistently indicated. After being fully adjusted with 3 categories of factors including sociodemographic, lifestyle factors, and metabolic risk factors (Model 4), sarcopenia still increased the risk of prediabetes (OR = 1.21, 95CI%: 1.05, 1.39, P = 0.009). See Table 2 for detailed results.
Since sarcopenia was defined by ASM/BMI in our study, we further investigated the prevalence rates and risk situations of prediabetes among the tertile groups of ASM/BMI. The results revealed that the prevalence of prediabetes all exhibited a downward trend with the increasing ASM/BMI tertiles for both men and women (P for trend < 0.001) (Fig. 2B–C). Nevertheless, after full adjustment for confounding factors (same as the above Model 4), only the third tertile of ASM/BMI significantly decreased the prediabetes risk compared to the first tertile in men (OR = 0.77, 95CI%: 0.67, 0.89, P < 0.001) and no significant differences were found among tertiles groups in woman (P > 0.05) (Table S1).
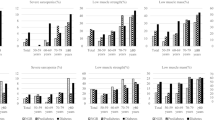
Stratified analysis association between sarcopenia and the risk of prediabetes
To further elucidate the independent effect of sarcopenia on prediabetes risk, we performed stratified analysis of the abovementioned factors and they were stratified based on cardiovascular risk indicators [22]. Figure 3 shows that among all stratification subgroups, compared with non-sarcopenia group, the sarcopenia group exhibited higher prediabetes rates and was consistent with the trend in overall prevalence of prediabetes. After fully adjusting the covariates (similar to Model 4), the association between sarcopenia and the risk of prediabetes remained stable in some subgroups, such as the obese subgroup defined by BMI (OR = 1.30, 95CI%: 1.08, 1.56, P = 0.001), the non-obese subgroup (OR = 1.19, 95CI%: 1.00, 1.41, P = 0.001), the centrally obese subgroup defined by waist circumference (OR = 1.32, 95CI%: 1.15, 1.52, P < 0.001), and the non-obese subgroup (OR = 1.28, 95CI%: 1.05, 1.56, P = 0.014). For subgroups stratified by TG and HDL-C levels, the above risk association still persisted (Fig. 3). Of notice, although differences in partial stratified analysis did not attain strict statistical significance (P = 0.052–0.054), strong trends in prediabetes risk were still considered evident. In addition, we observed no significant association between sarcopenia and increased risk of prediabetes across some high-risk subgroups (SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, TC ≥ 6.22 mmol/L, LDL-C ≥ 4.14 mmol/L, P > 0.05).
Overall effects of OLLMM on prediabetes
Regardless of the criteria used to define obesity, we found highest prevalence of prediabetes in the OLLMM groups with 47.47% (obesity defined by BF%), 49.43% (defined by waist circumference) and 51.47% (defined by BMI), respectively (Fig. 4). The prevalence of prediabetes was close among the only sarcopenia and the only obesity groups. Consistent with our expectations, after adjustment for confounders in logistic regression models, clear difference in risk between four groups could be observed. Compared to the reference group (normal group), the only sarcopenia group, the only obesity group and the OLLMM group exhibited a tendency for an increased risk of prediabetes progressively. Of these, the risk of prediabetes was most pronounced in the sarcopenia obesity group, especially when obesity defined by waist circumference (OR = 2.63, 95CI%: 2.22, 3.11, P < 0.001) (Fig. 4).
Preliminary assessment of the association between sarcopenic and type of prediabetes
To explore the association between sarcopenic and the type of prediabetes, we screened 1568 participants with prediabetes and complete blood glucose data (including FPG, 2hPG and HbA1c) from above study populations. 1417 were non-sarcopenic participants and 151 were sarcopenic participants. See Table S2 for baseline characteristics between groups. The prevalence of i-IFG, i-IGT, and combined IFG & IGT was 59.84%, 10.37%, and 13.69% in the nonsarcopenic group and 48.34%, 13.91%, and 27.81% in the sarcopenic group, respectively. Notably, the prevalence of any IGT was significantly different between the sarcopenic group and the nonsarcopenic group (41.72% vs 24.06%, P < 0.001) (Fig. 5). Any IFG prevalence was similar across groups (76.16% vs 73.54%, P = 0.559).
Discussion
Our study is the first to clarify the specific association between sarcopenic status and prediabetes risk through such a large sample size. The association was evident even after adjustment for multiple confounders, or in the partial stratified analyses. Additionally, the synergistic effect of sarcopenia and obesity was also confirmed. The risk of developing prediabetes was roughly doubled in OLLMM participants compared to individuals only with sarcopenia. Finally, we noted that sarcopenia might have more effects on postprandial plasma glucose and increased the prevalence of IGT.
At present, numerous studies have proved that the loss of muscle mass is closely associated with abnormal metabolic state [23]. However, most studies just focused on examining the association of sarcopenia with T2DM and diabetes-related complications, there are only few clinical studies on the association between sarcopenia and prediabetes. Previously, one study on an Indian population found patients with prediabetes had lower skeletal muscle mass and contractile quality as compared to the general population, suggesting the change of skeletal muscle mass and function might become a sensitive indicator of abnormalities in glucose metabolism [24]. However, the small sample size is a major limitation and there were differences between study populations. A prospective study from the United States demonstrated that decreased fat-free mass was associated with increased incidence of prediabetes [25]. Markedly though, fat-free mass could not completely substitute for skeletal muscle mass. In our study accurate skeletal muscle mass measurements were conducted using DXA and our results highlighted an association between sarcopenic status and prediabetes. In addition, a study using data from NHANES III showed that with each 10% increase in skeletal mass index (estimated skeletal muscle mass/total body weight), there was a relative reduction in prediabetes prevalence of 23% (95% CI: 11, 33). This is similar to our results, but some differences also existed. In our study, we found a 23% relative reduction in the prediabetes prevalence in the highest tertile of ASM/BMI compared to the lowest tertile only in males, but not in females. This discrepancy with our results may arise from the estimated skeletal muscle mass rather than exact values or different approaches with adjustment for potential confounders. An important point to note was that the included population in our study were all non-elderly aged 20–59, which may reduce the age-bias to some extent, since advanced age is strongly associated with metabolic status and skeletal muscle mass. Additionally, smoking is one of the known risk factor for sarcopenia; however, the current smokers were fewer in the sarcopenia group. This is in line with previous study using data from the Korean National Health and Nutrition Examination Surveys [26]. This may be related to the lower sample size in the sarcopenia group.
Results of stratified analysis by traditional cardiovascular risk factors suggested that sarcopenia might be an independent risk factor for predia1betes. Nevertheless, no statistically significant results were observed in hypertensive subgroups and partial hyperlipidemic subgroups. This might be related to the small sample size in the above subgroups. Also, the possibility that the effect of blood pressure, TG, and HDL-C on the prediabetes were more significant than sarcopenia cannot be excluded. In line with most studies, the results of our study further revealed that the prevalence of dysglycemia was highest and can reach as high as 50% in OLLMM populations. Especially in a recent publication, authors stated that the prevalence of OLLMM was high worldwide and OLLMM patients had higher risk of developing metabolic diseases [27]. This is similar to our results and again demonstrated the ubiquitous and synergistic effect between sarcopenia and obesity. Of course, the synergistic effect on prediabetes was not limited to glucose metabolism. OLLMM is also associated with increased risk of metabolic syndrome, non-alcoholic fatty liver disease, hypertension, and arteriosclerotic cardiovascular disease [28,29,30]. Therefore, the increased risk of prediabetes in sarcopenic obese individuals is multifactorial.
All the above-mentioned risk results could not be separated from an important pathologic link—insulin resistance (IR) [31]. Previous study showed that skeletal insulin resistance was a vital link between sarcopenia and dysglycemia [32], and the mechanism might involve mitochondrial dysfunction in skeletal muscle, enhanced oxidative stress response, dysregulated myokine secretion, and chronic low-grade inflammation [33,34,35]. As insulin resistance continues to develop, muscle strength and muscle mass may decline further, leading to a vicious cycle. It was also clear from our study that sarcopenic patients exhibited higher HOMA-IR values. In addition, obesity, especially central obesity, is a strong risk factor for the development of IR. Similarly, our findings showed that participants with the co-existence of sarcopenia and central obesity defined by waist circumference were at highest risk of prediabetes. Central obesity was related to the accumulation of visceral adipose tissue, which showed a more pronounced IR and thus obviously increased risk of metabolic diseases [36, 37]. A notable result was that sarcopenia group had lower amount of energy intake, however had higher BMI. Table 1 shows that compared with non-sarcopenic counterparts, sarcopenic patients exhibited a higher percentage of energy from carbohydrates. Further, while sarcopenia group had higher amount of unrecorded PA, sarcopenic patients showed a higher percentage of low PA among patients with a documented PA assessment and had low metabolic rate [38, 39]. Therefore, sarcopenic patients were more likely to have a higher BMI.
After refining the specific types of prediabetes, we found a reduction in muscle mass might be more relevant to the abnormal increase in postprandial blood glucose level. As we all know, skeletal muscle is responsible for approximately 80% of dietary glucose and served as a buffer for the body's blood glucose balance [40]. When skeletal muscle mass decreases or even develops into sarcopenia, the decrease in glucose metabolism and the delay of glucose absorption could occur simultaneously in the muscle tissue, predisposing to increased postprandial glucose [41]. Multiple studies have also confirmed that muscle strength training and increased lean muscle mass can effectively improve glucose tolerance [42, 43]. In contrast, impaired fasting glucose level is mainly associated with metabolism in liver [44, 45]. Therefore, in the present study, insignificantly different proportions of patients with IFG were noted among the groups.
There are several implications in our study. First, we showed a definite association between sarcopenia and prediabetes through large sample populations. This suggested that we should be vigilant for the excess loss of muscle even not in old age and avoid a sedentary lifestyle. Strengthening exercise could positively influence occurrence and development of prediabetes. Secondly, the coexistence of sarcopenia and obesity will significantly increase the risk of developing prediabetes. Therefore, fat reduction is particularly important for patients with low skeletal muscle mass and obesity, especially abdominal obesity. Finally, our study highlighted the close association between the loss of muscle mass and postprandial glucose levels. Since postprandial hyperglycemia contributed more to the development of chronic diabetes complications, keeping the focus on postprandial glucose control of sarcopenic patients would be of greater clinical significance.
There are also limitations to the study. One is that our study was cross-sectional, so it was difficult to address causality. In addition, we could only estimate the prevalence of prediabetes in sarcopenic subjects, not incidence. Another one is that although sarcopenia can be diagnosed by muscle mass, the assessment of muscle function is equally important to define sarcopenia and should be further included in our future researches.
In conclusion, Sarcopenia could increase the risk of prediabetes especially IGT in the non-elderly. The risk association between the two exists independently of obesity, TG, and HDL-C. Additionally, OLLMM patients exhibited the highest prevalence of prediabetes. Based on the above results, focusing on muscular exercise and weight control might be effective in preventing prediabetes.
References
American Diabetes A (2019) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care 42:S13–S28
Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M (2012) Prediabetes: a high-risk state for diabetes development. Lancet 379:2279–2290
Plantinga LC, Crews DC, Coresh J, Miller ER 3rd, Saran R et al (2010) Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin J Am Soc Nephrol 5:673–682
Ziegler D, Rathmann W, Dickhaus T, Meisinger C, Mielck A et al (2008) Prevalence of polyneuropathy in pre-diabetes and diabetes is associated with abdominal obesity and macroangiopathy: the MONICA/KORA Augsburg Surveys S2 and S3. Diabetes Care 31:464–469
Algvere P, Efendic S, Luft R, Wajngot A (1985) Retinal microangiopathy and pigment epithelial lesions in subjects with normal, borderline, and decreased oral glucose tolerance. Br J Ophthalmol 69:416–419
Pour OR, Dagogo-Jack S (2011) Prediabetes as a therapeutic target. Clin Chem 57:215–220
Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet 393:2636–2646
Bauer J, Morley JE, Schols A, Ferrucci L, Cruz-Jentoft AJ et al (2019) Sarcopenia: a time for action. An SCWD position paper. J Cachexia Sarcopenia Muscle 10:956–961
Qiao YS, Chai YH, Gong HJ, Zhuldyz Z, Stehouwer CDA et al (2021) The association between diabetes mellitus and risk of sarcopenia: accumulated evidences from observational studies. Front Endocrinol (Lausanne) 12:782391
Nishikawa H, Asai A, Fukunishi S, Nishiguchi S, Higuchi K (2021) Metabolic syndrome and sarcopenia. Nutrients 13:3519
Peng TC (2018) Role of sarcopenia in nonalcoholic fatty liver disease: definition is crucially important. Hepatology 68:788–789
Petermann-Rocha F, Ferguson LD, Gray SR, Rodriguez-Gomez I, Sattar N et al (2021) Association of sarcopenia with incident osteoporosis: a prospective study of 168,682 UK biobank participants. J Cachexia Sarcopenia Muscle 12:1179–1188
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
American Diabetes A (2021) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 44:S15–S33
Gong R, Luo G, Wang M, Ma L, Sun S et al (2021) Associations between TG/HDL ratio and insulin resistance in the US population: a cross-sectional study. Endocr Connect 10:1502–1512
Becker DJ, Oloya J, Ezeamama AE (2015) Household socioeconomic and demographic correlates of cryptosporidium seropositivity in the United States. PLoS Negl Trop Dis 9:e0004080
MacGregor KA, Gallagher IJ, Moran CN (2021) Relationship between insulin sensitivity and menstrual cycle is modified by BMI, fitness, and physical activity in NHANES. J Clin Endocrinol Metab 106:2979–2990
Han E, Lee YH, Kim G, Kim SR, Lee BW et al (2016) Sarcopenia is associated with albuminuria independently of hypertension and diabetes: KNHANES 2008–2011. Metabolism 65:1531–1540
Wang J, Yan AF, Cheskin LJ, Shi Z (2022) Higher serum testosterone level was associated with a lower risk of prediabetes in US adults: findings from nationally representative data. Nutrients 15:9
Benjamin SM, Valdez R, Geiss LS, Rolka DB, Narayan KM (2003) Estimated number of adults with prediabetes in the US in 2000: opportunities for prevention. Diabetes Care 26:645–649
Kim JK, Ailshire JA, Crimmins EM (2019) Twenty-year trends in cardiovascular risk among men and women in the United States. Aging Clin Exp Res 31:135–143
Srikanthan P, Karlamangla AS (2011) Relative muscle mass is inversely associated with insulin resistance and prediabetes. findings from the third national health and nutrition examination survey. J Clin Endocrinol Metab 96:2898–2903
Sambashivaiah S, Harridge SDR, Sharma N, Selvam S, Rohatgi P et al (2019) Asian Indians with prediabetes have similar skeletal muscle mass and function to those with type 2 diabetes. Front Nutr 6:179
LeCroy MN, Hua S, Kaplan RC, Sotres-Alvarez D, Qi Q et al (2021) Associations of changes in fat free mass with risk for type 2 diabetes: Hispanic community health study/study of Latinos. Diabetes Res Clin Pract 171:108557
Leem AY, Kim YS, Chung KS, Park MS, Kang YA et al (2022) Sarcopenia is associated with cardiovascular risk in men with COPD, independent of adiposity. Respir Res 23:185
Murdock DJ, Wu N, Grimsby JS, Calle RA, Donahue S et al (2022) The prevalence of low muscle mass associated with obesity in the USA. Skelet Muscle 12:26
Merli M, Lattanzi B, Aprile F (2019) Sarcopenic obesity in fatty liver. Curr Opin Clin Nutr Metab Care 22:185–190
Lu CW, Yang KC, Chang HH, Lee LT, Chen CY et al (2013) Sarcopenic obesity is closely associated with metabolic syndrome. Obes Res Clin Pract 7:e301-307
Zhang X, Xie X, Dou Q, Liu C, Zhang W et al (2019) Association of sarcopenic obesity with the risk of all-cause mortality among adults over a broad range of different settings: a updated meta-analysis. BMC Geriatr 19:183
Hong SH, Choi KM (2020) Sarcopenic obesity, insulin resistance, and their implications in cardiovascular and metabolic consequences. Int J Mol Sci 21:494
DeFronzo RA, Tripathy D (2009) Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32(Suppl 2):S157-163
Gan Z, Fu T, Kelly DP, Vega RB (2018) Skeletal muscle mitochondrial remodeling in exercise and diseases. Cell Res 28:969–980
Chang WT, Wu CH, Hsu LW, Chen PW, Yu JR et al (2017) Serum vitamin D, intact parathyroid hormone, and Fetuin A concentrations were associated with geriatric sarcopenia and cardiac hypertrophy. Sci Rep 7:40996
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM et al (2002) Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci 57:M326-332
Standl E (2012) Dysglycemia and abdominal obesity. Curr Vasc Pharmacol 10:678–679
Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S (2007) Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes 56:1010–1013
Batsis JA, Villareal DT (2018) Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol 14:513–537
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V (2008) Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis 18:388–395
Son JW, Lee SS, Kim SR, Yoo SJ, Cha BY et al (2017) Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES. Diabetologia 60:865–872
Thiebaud D, Jacot E, DeFronzo RA, Maeder E, Jequier E et al (1982) The effect of graded doses of insulin on total glucose uptake, glucose oxidation, and glucose storage in man. Diabetes 31:957–963
Frank P, Andersson E, Ponten M, Ekblom B, Ekblom M et al (2016) Strength training improves muscle aerobic capacity and glucose tolerance in elderly. Scand J Med Sci Sports 26:764–773
Miller WJ, Sherman WM, Ivy JL (1984) Effect of strength training on glucose tolerance and post-glucose insulin response. Med Sci Sports Exerc 16:539–543
Alatrach M, Agyin C, Adams J, DeFronzo RA, Abdul-Ghani MA (2017) Decreased basal hepatic glucose uptake in impaired fasting glucose. Diabetologia 60:1325–1332
Ter Horst KW, Gilijamse PW, Ackermans MT, Soeters MR, Nieuwdorp M et al (2016) Impaired insulin action in the liver, but not in adipose tissue or muscle, is a distinct metabolic feature of impaired fasting glucose in obese humans. Metabolism 65:757–763
Funding
This research was funded by the National Natural Science Foundation of China (82104786 and 82074381), Shanghai Municipal Key Clinical Specialty (shslczdzk05401), Construction of Special Disease Alliance of Traditional Chinese Medicine in East China Region and City Level-Construction of specialty alliance of Endocrine and Metabolic Diseases of Traditional Chinese Medicine in Yangtze River Delta (ZY(2021–2023)-0302) and Shanghai Key Laboratory of Traditional Chinese Clinical Medicine (14DZ2273200). We thank all the participants in this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The studies involving human participants were reviewed and approved by NCHS of the CDC.
Informed consent
The patients/participants provided their written informed consent to participate in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, J., Han, X., Chen, Q. et al. Association between sarcopenia and prediabetes among non-elderly US adults. J Endocrinol Invest 46, 1815–1824 (2023). https://doi.org/10.1007/s40618-023-02038-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02038-y