Abstract
Purpose
This study aimed to evaluate the effect f angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB) on renal or cardiovascular outcomes in patients with diabetic nephropathy (DN).
Methods
PubMed, Embase, and Cochrane Library were searched for randomized controlled trials (RCTs) evaluating the treatment effects of ACEI and ARB on renal or cardiovascular outcomes in patients with DN until August 2017. The outcomes included end-stage renal disease (ESRD), doubling of serum creatinine levels, all-cause mortality, major cardiovascular events (MACEs), myocardial infarction (MI), stroke, and cardiac death. Relative risks (RR) with 95% confidence intervals (CIs) were used for calculating the summary results using a random-effects model.
Results
Twenty-four RCTs including 57,818 patients with DN and 891 events of ESRD, 1050 doubling of serum creatinine concentration, 4352 all-cause mortality, 6342 MACEs, 1073 MI, 2900 stroke, and 1674 cardiac deaths were reported. Overall, the summary results suggested that in patients with DN, receiving ACEI did not have a significant effect on ESRD, doubling of serum creatinine levels, all-cause mortality, MI, stroke, and cardiac death, while ACEI significantly reduced the risk of total MACEs. Furthermore, ARB therapy was associated with a low risk of ESRD and doubling of serum creatinine levels, while it did not differ significantly on all-cause mortality, MACEs, MI, stroke, and cardiac death in patients with DN.
Conclusions
Patients with DN receiving ACEI had significantly reduced the risk of total MACEs, and ARB could reduce the incidence of ESRD and the doubling of serum creatinine levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a major global health concern with an estimated 463 million patients worldwide in 2019 and projected to reach 700 million by 2045, according to The International Diabetes Federation (IDF) [1, 2]. Previous trials have demonstrated that patients with DM are associated with an increased risk of vascular complications and cardiac death compared with the general population [3]. In addition, DM is associated with microalbuminuria and diabetic nephropathy (DN), which is the leading cause of end-stage renal disease (ESRD) [3, 4]. Furthermore, the main goal of management in patients with DM is the prevention of vascular complications; thus, treatments that can lower the blood pressure should be used since hypertension is associated with the risk of macrovascular events [3].
Renin–angiotensin system blockers, including angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB), are widely used as the first line of treatment for microalbuminuria in patients with DM, which could decelerate the progression of DN in hypertensive patients [5, 6]. Previous studies demonstrated the effect of ACEI and ARB therapies in hypertensive patients, while the treatment effect in patients with DM yet remains controversial [7, 8]. Therefore, elucidating the treatment effects of ACEI and ARB on renal or cardiovascular outcomes is crucial in patients with DN. The effects of ACEI/ARB treatment in patients with DN has been studied in several randomized controlled trials (RCTs). In this study, we summarized the available RCTs to determine the effect of ACEI/ARB therapy on the incidence of renal and cardiovascular outcomes in patients with DN. In addition, we compared the treatment effects among patients with different characteristics.
Methods
Data sources, search strategy, and selection criteria
This review was conducted and reported according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA) Statement issued in 2009 (Checklist S1) [9].
Any RCTs that examined the effect of ACEI and ARB on renal and cardiovascular outcomes were eligible for inclusion in the present study without regarding language or publication status (published, in press, or in progress). We searched the PubMed, Embase, and Cochrane Library electronic databases for articles published through August 2017 and used (“ACEIs” OR “captopril” OR “enalapril” OR “cilazapril” OR “enalaprilat” OR “fosinopril” OR “lisinopril” OR “perindopril” OR “ramipril” OR “saralasin” OR “angiotensin-receptor antagonists” OR “ARBs” OR “losartan” OR “irbesartan” OR “valsartan” OR “olmesartan” OR “candesartan” OR “eprosartan” OR “telmisartan”) AND (“diabetes” OR “DM” OR “diabetic nephropathy” OR “DN”) AND “randomized controlled trials” AND “human” as the search terms. The ongoing RCTs, which have already been registered as completed but not yet published in https://www.ClinicalTrials.gov, were also searched. In addition, we conducted manual searches of the reference lists from all relevant original and review articles to identify the additional eligible studies. The study topic, methods, patient disease status, study design, intervention, control, and investigated outcomes were used to identify the relevant studies.
The literature search was independently undertaken by two authors using a standardized approach. Any inconsistencies between these two authors were settled by group discussion to achieve a consensus. The studies that fulfilled the following criteria were eligible for inclusion: (1) the study was a randomized controlled trial; (2) all the included patients had DN; (3) the study investigated the effect of ACEI or ARB therapy in comparison to the treatment regimens without ACEI and ARB; (4) the study reported at least one of the following outcomes: ESRD, doubling of serum creatinine concentration, all-cause mortality, major cardiovascular events (MACEs), myocardial infarction (MI), stroke, and cardiac death. If multiple studies from the same populations were identified, only the most complete publication was included.
Data collection and quality assessment
The data extraction and quality assessment were conducted independently by two authors. The information was examined and adjudicated independently by an additional author referring to the original studies. The data collected included the first author or the name of the study group, publication year, country, sample size, mean age, percentage of male, body mass index (BMI), HbA1c, DM types, diabetes duration, mean systolic blood pressure (SBP), mean diastolic blood pressure (DBP), intervention, control, and follow-up duration. The quality of the study was assessed by the Jadad scale, based on randomization, concealment of treatment allocation, blinding, completeness of follow-up, and the use of intention-to-treat analysis [10]. A “star system” (range 0–5) was developed for assessment. A study with a score ≥ 4 was regarded as high quality.
Statistical analysis
We examined the effect of ACEI or ARB on the risk of renal and cardiovascular outcomes based on the number of events and sample size in each group published in each trial. We used the random-effects model to calculate the summary RRs and 95% confidence intervals (CIs) for ACEI or ARB vs. patients without ACEI/ARB therapy on the risk of renal or cardiovascular outcomes, which speculated that the true underlying effect varied among the included trials [11, 12]. Heterogeneity between studies was investigated by the Q statistic, and P < 0.10 was considered as significant heterogeneity [13, 14]. Subgroup analyses were conducted on the basis of mean age (≥ 60.0 and < 60.0 years), percentage male (≥ 60.0% and < 60.0%), BMI (≥ 25.0 and < 25.0 kg/m2), HbA1c (≥ 8.0% and < 8.0%), DM types (I and II), duration of DM (≥ 10.0 and < 10.0 years), and follow-up duration (≥ 3.0 and < 3.0 years). The ratio between the subgroups was calculated by the chi-square test and meta-regression [15]. A sensitivity analysis was performed by removing the studies individually from the meta-analysis [16]. The Egger test [17] and the Begg test [18] were used to assess the publication bias statistically. All reported P values were two sided, and P values < 0.05 were considered statistically significant. The statistical analyses were performed using the STATA software (version 10.0; Stata Corporation, College Station, TX, USA).
Results
Literature search
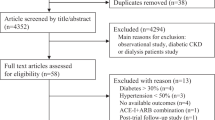
The results of the study-selection process are shown in Fig. 1. We identified 2388 articles initially, of which, 2301 were excluded as duplicates, irrelevant studies, and other study designs. A total of 87 potentially eligible studies were retrieved, and after a detailed evaluation, 27 were excluded as the patients originated from the same population, 21 were excluded as the trial did not report the events of investigation, and 15 studies were excluded due to no appropriate controls. Finally, 24 RCTs were selected for the final meta-analysis [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. A manual search of the reference lists of these studies did not yield any additional eligible studies. The general characteristics of the included studies are presented in Table 1 and Supplemental Table S1.
Study characteristics
The 24 included trials included a total of 57,818 patients with DN. The follow-up duration for the patients with DN was 1.0–5.0 years, while 32–11,140 patients were included in each study. The mean age of the patients in the included trials ranged from 29.7 to 66.2 years, and the mean BMI ranged 22.6–34.6 kg/m2. Seven trials included patients with type 1 DM, 13 trials included patients with type 2 DM, and 4 trials included both patients with type 1 and 2 DM. Ten trials investigated the risk of ESRD, 8 investigated the risk of doubling of serum creatinine levels, 21 reported the risk of all-cause mortality, 12 reported the risk of MACEs, 9 reported the risk of MI, 10 reported the risk of stroke, and 8 reported the risk of cardiac death. The quality of the studies was assessed using the Jadad scale, and six trials had a score of 5, fourteen presented a score of 4, three had a score of 3, and one had a score of 2.
End-stage renal disease
The effect of ACEI on the risk of ESRD was studied in a total of 19,664 patients with DN; 216 events of ESRD were reported. No significant difference was observed between ACEI and control (RR 0.78; 95% CI 0.60–1.01; P = 0.063; with no evidence of heterogeneity, Fig. 2). According to the sensitivity analysis, we excluded the study conducted by the ADVANCE study group, which specifically used a large sample size and weight. Consequently, ACEI significantly reduced the risk of ESRD (RR 0.67; 95% CI 0.49–0.90; P = 0.008; Table 2; Supplemental 1: Table S1). The subgroup analysis suggested that ACEI was associated with a low risk of ESRD if mean age < 60.0 years, percentage of male ≥ 60.0%, and follow-up duration < 3.0 years (Supplemental 2: Table S1).
Data for the effect of ARB on the risk of ESRD was collected from a total of 3224 patients with DN; 675 events of ESRD were reported. Notably, ARB therapy was associated with a low risk of ESRD (RR 0.82; 95% CI 0.71–0.93; P = 0.003; with no evidence of heterogeneity, Fig. 2). The findings of the sensitivity analysis were variable due to the small number of trials included (Table 2; Supplemental 1: Table S1). The subgroup analysis indicated a noticeable significant difference when the mean age ≥ 60.0 years, percentage of male ≥ 60.0%, BMI ≥ 25.0 kg/m2, HbA1c ≥ 8.0%, and type II DM (Supplemental 2: Table S1).
Doubling of serum creatinine levels
Data for the effect of ACEI on the risk of doubling of serum creatinine levels were collected from a total of 6686 patients with DN, and 235 events of doubling of serum creatinine concentration reported. ACEI did not exert a significant effect on doubling of serum creatinine levels (RR 0.69; 95% CI 0.44–1.08; P = 0.101; Fig. 3), and moderate heterogeneity was detected (I2 = 55.4%; P = 0.062). Sensitivity analysis suggested that after excluding the Micro-HOPE trial that included patients with higher HbA1c and both type 1 and 2 DM, ACEI was associated with a low risk of doubling of serum creatinine concentration (RR 0.58; 95% CI 0.36–0.94; P = 0.027; Table 2; Supplemental 1: Table S2). The subgroup analysis indicated that ACEI therapy was associated with a low risk of doubling of serum creatinine levels when the mean age of patients was < 60.0 years, the male proportion was < 60.0%, BMI < 25.0 kg/m2 and type 1 DM (Supplemental 2: Table S2). The effect of ACEI on the doubling of serum creatinine levels in patients with high BMI was greater than those with low BMI (ratio between subgroups 6.20; 95% CI 1.46–26.38).
The effect of ARB on the risk of doubling of serum creatinine levels encompassed 3224 patients with DN, and 815 events of doubling of serum creatinine levels were reported. The summary result indicated that ARB therapy significantly reduced the risk of doubling of serum creatinine levels (RR 0.82; 95% CI 0.73–0.92; P = 0.001; Fig. 3), and slight heterogeneity was observed (I2 = 0.4%; P = 0.366). A sensitivity analysis was conducted, and after each study was sequentially excluded from the pooled analysis, the conclusion was not affected (Table 2; Supplemental 1: Table S2). Subgroup analysis suggested that the treatment effect was significantly focused on patients with mean age < 60.0 years, proportion of males ≥ 60.0%, BMI ≥ 25.0 kg/m2, HbA1c ≥ 8.0%, type 2 DM, and regarding of long or short follow-up duration periods (Supplemental 2: Table S2).
All-cause mortality
The data for the effect of ACEI on the risk of all-cause mortality was collected from a total of 22,364 patients with DN, and 2143 events of all-cause mortality were reported. Overall, the ACEI therapy did not affect all-cause mortality significantly (RR 0.91; 95% CI 0.78–1.06; P = 0.235; Fig. 4). Although moderate heterogeneity was observed in the magnitude of the effect across the studies (I2 = 40.5%; P = 0.079), after the sequential exclusion of each study from the pooled analysis, the conclusion was not affected (Table 2; Supplemental 1: Table S3). The findings of the subgroup analysis indicated that ACEI therapy significantly reduced the risk of all-cause mortality if the percentage of males was < 60.0%, HbA1c ≥ 8.0%, and duration of DM was ≥ 10.0 years (Supplemental 2: Table S3). Furthermore, patients with DN and HbA1c ≥ 8.0% and who received ACEI presented a lower risk of all-cause mortality compared with those with HbA1c < 8.0% (ratio between subgroups 0.79; 95% CI 0.63–0.99).
The effect of ARB on the risk of all-cause mortality was collected from a total of 34,967 patients with DN, and 2209 events of all-cause mortality were reported. No significant difference was observed between ARB and control (RR 1.03; 95% CI 0.95–1.12; P = 0.459; no evidence of heterogeneity, Fig. 4). Sensitivity analysis was conducted after the sequential exclusion of each trial from the pooled analysis; the conclusion was not affected by the exclusion of any specific trial (Table 2; Supplemental 1: Table S3). Furthermore, ARB therapy was not associated with the risk of all-cause mortality in all predefined subsets (Supplemental 2: Table S3).
Major cardiovascular events
The effect of ACEI on the risk of total MACEs involved a total of 21,266 patients with DN, and 2680 MACEs were reported. We noted that ACEI therapy significantly reduced the risk of total MACEs (RR 0.89; 95% CI 0.81–0.98; P = 0.015; Fig. 5), and mild heterogeneity was observed (I2 = 36.8%; P = 0.176). The findings of the sensitivity analysis were variable due to different statistical power (Table 2; Supplemental 1: Table S4). The significant difference for ACEI occurred primarily in patients with mean age ≥ 60.0 years, percentage of male < 60.0%, BMI ≥ 25.0 kg/m2, HbA1c ≥ 8.0%, type 1 DM, duration of DM ≥ 10.0 years, and follow-up duration ≥ 3.0 years (Supplemental 2: Table S4). Furthermore, the effect of ACEI in the HbA1c ≥ 8.0% (ratio between subgroups 0.84; 95% CI 0.71–0.99) and type 1 DM (ratio between subgroups 0.84; 95% CI 0.71–0.99) groups was lower than the corresponding comparison groups.
The data for the effect of ARB on the risk of total MACEs involved a cohort of 29,736 patients with DN, and 3662 MACEs were reported. The results of the pooled analysis neither revealed any association between ARB therapy and total MACEs nor any evidence of heterogeneity (RR 0.94; 95% CI 0.89–1.00; P = 0.054; Fig. 5). According to the sensitivity analysis, we excluded the study by Mauer et al., as the trial specifically included type 1 DM and mean blood pressure was normalized. Consequently, we concluded that ARB significantly reduced the risk of total MACEs by 6% (RR 0.94; 95% CI 0.88–0.99; P = 0.031; Table 2; Supplemental 1: Table S4). The treatment effects were primarily based on the percentage of males ≥ 60.0% (Supplemental 2: Table S4).
Myocardial infarction
The data for the effect of ACEI on the risk of MI were collected from 10,520 patients with DN, and 649 events of MI were reported. The summary RR showed that the ACEI therapy was not associated with MI (RR 0.89; 95% CI 0.70–1.13; P = 0.341; Fig. 6), but moderate heterogeneity was seen (I2 = 41.9%; P = 0.160). After excluding the VA NEPHRON-D trial that included patients with high BMI and contributed high weight for the pooled analysis, ACEI was associated with a low risk of MI (RR 0.79; 95% CI 0.67–0.93; P = 0.004; Table 2; Supplemental 1: Table S5). Subgroup analysis suggested that the ACEI therapy was associated with low risk of MI when HbA1c ≥ 8.0%, duration of DM ≥ 10.0 years, and follow-up duration of ≥ 3.0 years (Supplemental 2: Table S5). Furthermore, patients with long follow-up duration were associated with a beneficial effect on MI (ratio between subgroups 0.61; 95% CI 0.39–0.94).
The data for the effect of ARB on the risk of MI were collected from 28,397 patients with DN, and 424 events of MI were reported. No significant association was observed between ARB and MI (RR 0.98; 95% CI 0.67–1.45; P = 0.926; Fig. 6), and mild heterogeneity was observed in the magnitude of the effect across the studies (I2 = 35.4%; P = 0.185). After the sequential exclusion of each study from the pooled analyses, the conclusion was not changed (Table 2; Supplemental 1: Table S5), and no significant difference was observed according to the subgroup analysis (Supplemental 2: Table S5).
Stroke
The data for the effect of ACEI on the risk of stroke encompassed a total of 21,660 patients with DN, and 1048 events of stroke were reported. We noted that ACEI had little or no effect on the risk of stroke (RR 0.90; 95% CI 0.78–1.05; P = 0.181; Fig. 7), and mild heterogeneity was observed (I2 = 20.4%; P = 0.285). The findings of the sensitivity analysis were in agreement with the overall analysis (Table 2; Supplemental 1: Table S6). Furthermore, the subgroup analysis indicated that ACEI might exert a beneficial effect on stroke when HbA1c ≥ 8.0% and duration of DM ≥ 10.0 years (Supplemental 2: Table S6). In addition, the beneficial effect of ACEI was large in HbA1c ≥ 8.0% (ratio between subgroups 0.71; 95% CI 0.52–0.97) and duration of DM ≥ 10.0 years (ratio between subgroups 0.71; 95% CI 0.52–0.97).
The effect of ARB on the risk of stroke was assessed on 28,397 patients with DN, and 1852 events of stroke were reported. The pooled analysis results did not reveal any association between ARB and stroke (RR 0.94; 95% CI 0.86–1.02; P = 0.144; no evidence of heterogeneity; Fig. 7). The findings of the sensitivity analysis did not demonstrate a significant difference (Table 2; Supplemental 1: Table S6). Furthermore, the subgroup analysis also did not find any significant difference in all the predefined subsets (Supplemental 2: Table S6).
Cardiac death
The effect of ACEI on the risk of cardiac death was investigated in 19,629 patients with DN, and 1106 events of cardiac death were reported. ACEI was not found to affect the risk of cardiac death (RR 0.82; 95% CI 0.63–1.06; P = 0.127; Fig. 8); a potential evidence of significant heterogeneity was observed (I2 = 79.5%; P = 0.008). According to the sensitivity analysis, we excluded the study by Mauer et al., wherein ACEI significantly reduced the risk of cardiac death (RR 0.73; 95% CI 0.57–0.94; P = 0.013; Table 2; Supplemental 1: Table S7). Moreover, the subgroup analysis suggested that ACEI was associated with a low risk of cardiac death if the proportion of males was < 60.0%, HbA1c ≥ 8.0%, and the duration of DM ≥ 10.0 years (Supplemental 2: Table S7). The effect of ACEI on cardiac death in HbA1c ≥ 8.0% (ratio between subgroups 0.70; 95% CI 0.51–0.96) and the duration of DM ≥ 10.0 years (ratio between subgroups 0.70; 95% CI 0.51–0.96) were superior to the corresponding group.
Data for the effect of ARB on the risk of cardiac death involved a total of 28,397 patients with DN, and 568 events of cardiac death were reported. Although ARB therapy increased the risk of cardiac death by 28%, it was not statistically significant (RR 1.28; 95% CI 0.71–2.32; P = 0.416; Fig. 8). Although substantial heterogeneity was observed (I2 = 67.6%; P = 0.015), after the sequential exclusion of each study, the conclusion was not affected (Table 2; Supplemental 1: Table S7). The subgroup analysis suggested that ARB significantly increased the risk of cardiac death if HbA1c < 8.0% (Supplemental 2: Table S7). Furthermore, ARB treatment greatly affected the cardiac death if included patients’ HbA1c ≥ 8.0% (ratio between subgroups 0.18; 95% CI 0.06–0.51).
Publication bias
The publication biases for the investigated outcomes are presented in Table 3. The results of the Egger and Begg tests did not demonstrate any evidence of publication bias for ESRD (PEgger [ACEI]: 0.906 and PBegg [ACEI]: 0.764; PEgger [ARB]: 0.467 and PBegg [ARB]: 0.296), doubling of serum creatinine concentration (PEgger [ACEI]: 0.439 and PBegg [ACEI]: 0.806; PEgger [ARB]: 0.452 and PBegg [ARB]: 1.000), all-cause mortality (PEgger [ACEI]: 0.557 and PBegg [ACEI]: 0.755; PEgger [ARB]: 0.220 and PBegg [ARB]: 0.371), MACEs (PEgger [ACEI]: 0.793 and PBegg [ACEI]: 1.000; PEgger [ARB]: 0.652 and PBegg [ARB]: 1.000), MI (PEgger [ACEI]: 0.556 and PBegg [ACEI]: 0.308; PEgger [ARB]: 0.610 and PBegg [ARB]: 0.462), stroke (PEgger [ACEI]: 0.681 and PBegg [ACEI]: 0.462; PEgger [ARB]: 0.593 and PBegg [ARB]: 0.462), and cardiac death (PEgger [ACEI]: 0.680 and PBegg [ACEI]: 1.000; PEgger [ARB]: 0.204 and PBegg [ARB]: 0.462).
Discussion
The present study was based on RCTs and explored the potential effect of ACEI/ARB on renal or cardiovascular outcomes in patients with DN. This comprehensive quantitative study included 57,818 patients from 24 trials encompassing a broad range of populations. The findings suggested that ACEI therapy was associated with lower risk of MACEs, while it did not exert any significant effect on the outcomes of ESRD, doubling of serum creatinine levels, all-cause mortality, MI, stroke, and cardiac death. Moreover, the ARB therapy significantly reduced the risk of ESRD and doubling of serum creatinine levels, but did not affect the incidence of all-cause mortality, MACEs, MI, stroke, and cardiac death in patients with DN. In addition, the effect of ACEI might differ by HbA1c, DM types, duration of DM, and follow-up duration. Finally, the treatment effect of ARB might differ according to patients with different HbA1c levels. These findings could provide an appropriate and useful assessment of the relative efficiency of ACEI/ARB therapy in patients with DN.
A previous meta-analysis included 24 trials, of which, 20 studies evaluated the treatment effect of ACEI, and the remaining four trials evaluated the treatment effect of ARB in patients with DN [43]. These studies indicated that patients with DN receiving ACEI or ARB therapy were associated with a lower incidence of ESRD and doubling of serum creatinine levels, while no effect was found on all-cause mortality. The inherent limitation of this study was that about half of the included trials did not report the events of renal outcomes and only provided the qualitative results. Furthermore, the summary results for cardiovascular outcomes, including MACEs, MI, stroke, and cardiac death, were not investigated. The follow-up duration in several included studies was shorter than necessary to display a clinical benefit due to event rates being lower than expected and associated broad CIs, i.e., no statistically significant difference. In addition, the treatment effects of ACEI or ARB in patients with specific characteristics were not calculated. Therefore, we conducted this study to evaluate the potential effect of ACEI/ARB in patients with DN.
The summary results suggested that ACEI therapy did not affect the incidence of renal outcomes, while ARB therapy significantly reduced the risk of ESRD and doubling of serum creatinine concentration. The findings of this study are in agreement with those from a previous meta-analysis [43]; only the treatment effect of ACEI and ARB on doubling of serum creatinine levels was inconsistent. The VA NEPHRON-D investigators included 1448 patients with 2.2 years of follow-up and suggested that combination therapy of ACEI and ARB might play a major role in ESRD; it also increased the risk of hyperkalemia and acute kidney injury [32]. Furthermore, Ravid et al. demonstrated that ACEI in the treatment of early stages of DN was associated with a low risk of doubling of serum creatinine concentration [21]. In addition, Lewis et al. demonstrated that captopril therapy slowed the deterioration of renal function in patients with type 1 DM and caused DN [22]. This might be attributed to the dose-dependent treatment effect of ACEI on renal or cardiovascular outcomes. A number of included trials were designed to evaluate the HbA1c or renal function as the primary outcome. Hence, clinically significant differences in renal events were not found.
Next, we noted that ACEI therapy was beneficial on MACEs, while the treatment effect of ARB on individual cardiovascular outcomes was not statistically significant. This discrepancy is probably of a statistical nature. Not all studies reported the individual MACE components or all of them. In addition, MACE is a composite endpoint frequently used in cardiovascular research, comparable to the composite endpoint all-cause mortality. Despite the widespread use of the term in clinical trials, the definitions of MACE can differ among studies, which makes comparison of similar studies difficult. This is a limitation of meta-analyses. Furthermore, several RCTs included in this systemic review reported conflicting results. Marre et al. suggested that although ramipril could lower the SBP, DBP, and favor microalbuminuria and proteinuria, a difference between ACEI and controls for the cardiovascular events was not detected [29]. Mauer et al. indicated that both ACEI and ARB could not affect the progression of nephropathy; it could slow the progression of retinopathy, and ACEI and ARB could not affect the incidence of MACEs [31]. Finally, the VA NEPHRON-D trial indicated that either therapy did not benefit the all-cause mortality and MACEs [32]. This phenomenon might be attributed to the imbalance in the use of other hypertensive drugs, which might play a crucial role in the absence of treatment effects on MACEs. Consequently, the events that occurred were smaller than expected due to the short follow-up duration, which, in turn, might lower the statistical power.
The subgroup analysis indicated that the treatment effects of ACEI might induce biases according to the mean BMI, HbA1c, DM types, duration of DM, and follow-up duration. First, BMI is an independent risk factor for the progression of cardiovascular outcomes, which might correlate with the HbA1c levels [44]. Second, HbA1c and duration of DM are associated with the severity of DM, and the risk levels of cardiovascular events were varied [45]. Third, the treatment effect of ACEI/ARB on the renal and cardiovascular outcomes might differ between types 1 and 2 DM. Finally, patients with DN with long-term follow-up duration could acquire a larger number of events than those with a short-term follow-up duration.
The findings of this study could provide better knowledge of ACEI and ARB for the treatment of patients with DN, which might help in decision-making for clinicians and patients. Nevertheless, our results have several limitations. First, inevitable heterogeneity was observed among the eligible studies. The baseline characteristics of the patients also varied among the different studies. The doses and duration of ACEI/ARB were different among studies. Second, the quality of the included studies was different. The Jadad scale score ranged from 2 to 5. Third, the patients included in this study with different characteristics might affect the progression of renal and cardiovascular outcomes. Fourth, the analysis used pooled data as the individual data were not available, which restricted the detailed analysis. Finally, due to non-uniform reporting and differences in definitions, microalbuminuria vs. macroalbuminuria and eGFR < 60 vs. eGFR ≥ 60 ml/min/1.73 m2 could not be analyzed. In addition, not all studies reported the individual conditions grouped as MACEs and some studies called them cardiovascular events instead of MACEs. Therefore, to be able to carry out statistical analyses, we grouped all of them as MACEs.
In conclusion, ACEI shows significant improvements in MACEs, and ARB shows a satisfactory effect on ESRD and doubling of serum creatinine levels for the treatment of patients with DN. Furthermore, the treatment effects of ACEI and ARB in patients with DN might show beneficial effects in patients with specific characteristics. Nevertheless, large-scale RCTs should be conducted to verify the effect of ACEI/ARB in future studies.
References
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
IDF Diabetes Atlas, 9th edition 2019. https://diabetesatlas.org/en/resources/. Retrieved 2 Dec 2019
(2019) Introduction: standards of medical care in diabetes-2019. Diabetes Care 42:S1–S2. https://doi.org/10.2337/dc19-Sint01
Albvr VR, Tan SH, Candasamy M, Bhattamisra SK (2019) Diabetic nephropathy: an update on pathogenesis and drug development. Diabetes Metab Syndr 13:754–762
Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML et al (2005) Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care 28:164–176
Levey AS, Cattran D, Friedman A, Miller WG, Sedor J et al (2009) Proteinuria as a surrogate outcome in CKD: report of a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis 54:205–226
Lv Y, Zou Z, Chen GM, Jia HX, Zhong J et al (2010) Amlodipine and angiotensin-converting enzyme inhibitor combination versus amlodipine monotherapy in hypertension: a meta-analysis of randomized controlled trials. Blood Press Monit 15:195–204
Wu L, Deng SB, She Q (2014) Calcium channel blocker compared with angiotensin receptor blocker for patients with hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens (Greenwich) 16:838–845
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Ades AE, Lu G, Higgins JP (2005) The interpretation of random-effects meta-analysis in decision models. Med Decis Making 25:646–654
Deeks JJ, Higgins JPT, Altman DG (2008) Analyzing data and undertaking meta-analyses. In: Higgins JP, Green S (eds) Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, Oxford, p 501
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326:219
Tobias A (1999) Assessing the influence of a single study in meta-analysis. Stata Tech Bull 47:15–17
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Parving HH, Hommel E, Damkjaer Nielsen M, Giese J (1989) Effect of captopril on blood pressure and kidney function in normotensive insulin dependent diabetics with nephropathy. BMJ 299:533–536
Bauer JH, Reams GP, Hewett J, Klachko D, Lau A et al (1992) A randomized, double-blind, placebo-controlled trial to evaluate the effect of enalapril in patients with clinical diabetic nephropathy. Am J Kidney Dis 20:443–457
Ravid M, Savin H, Jutrin I, Bental T, Katz B et al (1993) Long-term stabilizing effect of angiotensin-converting enzyme inhibition on plasma creatinine and on proteinuria in normotensive type II diabetic patients. Ann Intern Med 118:577–581
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD (1993) The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med 329:1456–1462
Laffel LM, McGill JB, Gans DJ (1995) The beneficial effect of angiotensin-converting enzyme inhibition with captopril on diabetic nephropathy in normotensive IDDM patients with microalbuminuria. North American Microalbuminuria Study Group. Am J Med 99:497–504
Maschio G, Alberti D, Janin G, Locatelli F, Mann JF et al (1996) Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med 334:939–945
Sano T, Hotta N, Kawamura T, Matsumae H, Chaya S et al (1996) Effects of long-term enalapril treatment on persistent microalbuminuria in normotensive type 2 diabetic patients: results of a 4-year, prospective, randomized study. Diabet Med 13:120–124
Nankervis A, Nicholls K, Kilmartin G, Allen P, Ratnaike S et al (1998) Effects of perindopril on renal histomorphometry in diabetic subjects with microalbuminuria: a 3-year placebo-controlled biopsy study. Metabolism 47:12–15
(2000) Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart outcomes prevention evaluation study investigators. Lancet 355:253–259
Katayama S, Kikkawa R, Isogai S, Sasaki N, Matsuura N et al (2002) Effect of captopril or imidapril on the progression of diabetic nephropathy in Japanese with type 1 diabetes mellitus: a randomized controlled study (JAPAN-IDDM). Diabetes Res Clin Pract 55:113–121
Marre M, Lievre M, Chatellier G, Mann JF, Passa P et al (2004) Effects of low dose ramipril on cardiovascular and renal outcomes in patients with type 2 diabetes and raised excretion of urinary albumin: randomised, double blind, placebo controlled trial (the DIABHYCAR study). BMJ 328:495
Patel A, Grop AC, MacMahon S, Chalmers J, Neal B et al (2007) Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 370:829–840
Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A et al (2009) Renal and retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med 361:40–51
Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA et al (2013) Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 369:1892–1903
Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S et al (2001) The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 345:870–878
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA et al (2001) Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345:851–860
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE et al (2001) Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345:861–869
Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S et al (2008) Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med 359:1225–1237
Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J et al (2008) Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet 372:1394–1402
Bilous R, Chaturvedi N, Sjolie AK, Fuller J, Klein R et al (2009) Effect of candesartan on microalbuminuria and albumin excretion rate in diabetes: three randomized trials. Ann Intern Med 151(11–20):W13–14
Sjolie AK, Klein R, Porta M, Orchard T, Fuller J et al (2008) Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet 372:1385–1393
Imai E, Chan JC, Ito S, Yamasaki T, Kobayashi F et al (2011) Effects of olmesartan on renal and cardiovascular outcomes in type 2 diabetes with overt nephropathy: a multicentre, randomised, placebo-controlled study. Diabetologia 54:2978–2986
Haller H, Ito S, Izzo JL Jr, Januszewicz A, Katayama S et al (2011) Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N Engl J Med 364:907–917
Yamashita K, Kondo T, Muramatsu T, Matsushita K, Nagahiro T et al (2013) Effects of valsartan versus amlodipine in diabetic hypertensive patients with or without previous cardiovascular disease. Am J Cardiol 112:1750–1756
Sarafidis PA, Stafylas PC, Kanaki AI, Lasaridis AN (2008) Effects of renin-angiotensin system blockers on renal outcomes and all-cause mortality in patients with diabetic nephropathy: an updated meta-analysis. Am J Hypertens 21:922–929
Wang ZJ, Zhou YJ, Galper BZ, Gao F, Yeh RW et al (2015) Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: a systematic review and meta-analysis. Heart 101:1631–1638
Qi W, Zhang N, Korantzopoulos P, Letsas KP, Cheng M et al (2017) Serum glycated hemoglobin level as a predictor of atrial fibrillation: A systematic review with meta-analysis and meta-regression. PLoS ONE 12:e0170955
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, X., Ma, L. & Li, Z. Effects of renin–angiotensin system blockers on renal and cardiovascular outcomes in patients with diabetic nephropathy: a meta-analysis of randomized controlled trials. J Endocrinol Invest 43, 959–972 (2020). https://doi.org/10.1007/s40618-020-01179-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01179-8