Abstract
Purpose
To explore the effects of mobile health (mHealth) intervention on pregnancy weight management, blood glucose control and pregnancy outcomes.
Methods
A total of 124 patients with gestational diabetes mellitus (GDM) were selected. Patients were randomly divided into two groups. The 60 patients in the control group received standard outpatient treatment, while the remaining 64 patients received a nurse’s online guidance both through a mobile medical App installed on their phone and through regular offline clinical treatment in the mHealth group. Patients were treated for an average of 13 weeks and general conditions, compliance, blood glucose, glycosylated hemoglobin, weight gain, pregnancy, and neonatal outcomes were monitored in both groups longitudinally.
Results
The mHealth group demonstrated higher levels of compliance (83.3 ± 12.5% vs. 70.4 ± 10.1%, t = − 6.293, df = 122, p < 0.001), lower frequency of outpatient service (8.1 ± 1.3 vs. 11.2 ± 1.1, t = 14.285, df = 122, p < 0.001), lower hemoglobin A1C before delivery (4.7 ± 0.2 vs. 5.3 ± 0.3, t = 13.216, df = 122, p < 0.001) as well as the rates of off-target measurements both fasting (4.6 ± 0.4% vs. 8.3 ± 0.6%, t = 40.659, df = 122, p < 0.001) and 2 h post-prandial (7.9 ± 0.7% vs. 14.7 ± 0.8%, t = 50.746, df = 122, p < 0.001). Weight gain in the mHealth group was less than control group (3.2 ± 0.8 vs. 4.8 ± 0.7, t = 11.851, df = 122 p < 0.001).
Conclusion
Mobile health intervention management of gestational diabetes mellitus improves patients’ compliance and blood glucose control, and reduces weight gain, thereby reducing the rates of complications in both pregnant women and fetuses during delivery during pregnancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prevalence of GDM, defined as glucose intolerance with onset or first recognition during pregnancy, is increasing worldwide [1, 2]. In 2013, a survey conducted by the International Diabetes Federation (IDF) found that GDM affected 14.2% of pregnant women globally [3]. A survey of 17,186 pregnant women in 13 hospitals in China between 2010 and 2012 showed that the prevalence of GDM was as high as 17.5% [4]. Research has demonstrated that obesity prior to pregnancy and excess weight gain during pregnancy are closely linked to the occurrence of GDM, which in turn results in an increased risk of obesity and metabolic syndrome in offspring during both their childhood and adulthood. People with gestational diabetes are at increased risk of preeclampsia, preterm birth, stillbirth, and macrosomia. Although the blood glucose values of most women tend to be stable after the birth of the fetus, the risk of developing type 2 diabetes mellitus (T2DM) is elevated in women previously diagnosed with GDM [5, 6].
It has been conclusively shown that strict control of blood glucose, weight control, and good compliance with medical advice can reduce the rates of complications in both pregnant women and fetuses during delivery, and can reduce the rates of adverse outcomes such as macrosomia and shoulder dystocia [7, 8]. At present, the health education of GDM patients primarily relies upon medical personnel teaching patients relevant details about their condition, leaving the patient to passively absorb this information. Providing diabetes self-management education and support to GDM patients is an effective means of controlling GDM [9]. Mobile health care is a relatively new emerging technology that is gradually being adapted as an effective management tool for myriad diseases. A recent meta-analysis shows that a T2DM-focused mobile medical App is easy for patients to use and can improve their cooperation and compliance, ultimately strengthening their T2DM self-management skills [10, 11]. Many previous studies have focused on the effects of mobile medical treatment on blood glucose in patients with GDM, while there are few studies on the effects of mobile medical treatment on maternal weight management and pregnancy outcomes. In this study, a mobile medical App was used to educate and manage GDM patients and to explore the effects of mobile medical interventions on weight management, blood glucose control and pregnancy outcomes in these patients.
Objectives and methods
Study objectives
Patients diagnosed with gestational diabetes mellitus (GDM) between 24 and 28 weeks of pregnancy in the Metabolic Disease Hospital of Tianjin Medical University between December 2015 and December 2017 were selected. Patients were 21–45 years old, pregnant with a single fetus, skilled at using smartphones, and were willing to cooperate with research and regular follow-up visits. Patients with pre-pregnancy diabetes, multiple pregnancies, or severe illness were excluded. The purpose and significance of the study was explained to participants and their informed consent was obtained. All patients signed informed consent forms, and the study was approved by the Ethics Committee of the Metabolic Disease Hospital of Tianjin Medical University (Number: 20150503). The study conforms to the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013).
The GDM diagnosis was made based on the diagnostic criteria for gestational diabetes introduced by the American Diabetes Society in 2011. Pregnant women who had not previously been diagnosed with overt diabetes were challenged with 75 g OGTT during weeks 24 and 28 of pregnancy after an 8 h fast. Blood glucose levels were measured before and 1 and 2 h after oral administration of glucose. If elevation of blood glucose during pregnancy was in accordance with one of the following criteria: fasting blood glucose ≥ 5.1 mmol/L, or blood glucose 1 h after OGTT ≥ 10.0 mmol/L, or blood glucose 2 h after OGTT ≥ 8.5 mmol/L, then GDM was diagnosed. According to the recommended standard in the IOM guidelines, for females a BMI of ≥ 25 kg/m2 and < 29.9 kg/m2 is defined as overweight, while a BMI of ≥ 30 kg/m2 is defined as obese before pregnancy.
Research method
Patients were randomly divided into two groups using the Excel table random sampling method. One group receiving a conventional outpatient treatment regimen (n = 60) served as the control group. The other group used a combination of “mobile medical management and outpatient treatment” (n = 64), serving as the Mobile health (mHealth) group.
Mobile medical management model of GDM
-
1.
The outpatient treatment model includes personalized dietary guidance by an educational nurse during a patient’s first visit. This nurse calculates the amount of protein, fat, and carbohydrates the patient needs daily based on their weight and activity level, develops a training plan, helps patients choose appropriate aerobic exercise, and checks their diet and exercise performance on a return visit. The specialist established the outpatient medical service file for each patient to record data for each visit, including blood glucose and weight, which can help with disease assessment and treatment planning. For their initial visits, patients are required to make one visit a week for 3 consecutive weeks. Fasting and post-prandial glucose self-measurements are monitored at least 3 days per week, and are manually recorded using a paper diary for review with their doctors at each visit. During the return visit, the educational nurses evaluate the implementation of the diet and exercise plans and the physician adjusts the treatment plan as needed. After patient blood glucose had stabilized, patients were required to visit once every 2–4 weeks. Blood glucose was monitored for at least 2 days per week, and fasting and post-prandial blood glucose were measured within 1 day. Patients were required to return to the clinic 3 months after delivery. The education nurse would call patients in the two groups to remind them of their consultation time, and patients needed to provide medical records of childbirth. At this time, the 75 g OGTT was performed again.
-
2.
Patients allocated to the control group received the aforementioned care. Patients assigned to the Mobile health (mHealth) group received our standard care, and in addition had an application installed to their smartphones. The mobile health (mHealth) group requires patients to download the Dnurse App (Beijing Dnurse Technology Co., Ltd) in which they used the outpatient mode. Fasting and post-prandial glucose self-measurements could be monitored using the Dnurse blood glucose meter (automatic data upload or manual data upload). Blood glucose data were compiled into tables and charts that were then uploaded and transmitted to the Doctor’s version of Dnurse App where they were subsequently viewed by the outpatient service doctor. Patients’ blood glucose meters were required to regularly undergo comparisons with hospital laboratory blood glucose meters (Biosen C-Line Blood Glucose Analyzer, EKF, Germany) to correct for any testing error. The education nurse provided online instruction available to patients every night from 7:00 PM to 9:00 PM, including answering questions about diet, exercise, blood glucose monitoring, insulin injection, and any other relevant topics. When the patient uploaded an abnormal blood glucose result, they were notified and the underlying cause is analyzed. Patients could also learn more about gestational diabetes by reading additional information about diet, exercise, medicine, and diabetes education in the Dnurse App.
Statistical method
Statistical analyses were conducted using the SPSS11.5 statistical software package. The measured data that were in accordance with a normal distribution are represented by x̄ ± s. T test were used to compare the mean of the two groups. The χ2 test was used to compare the composition ratios of the two groups. p < 0.05 was considered statistically significant.
Results
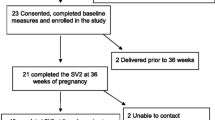
A total of 124 patients were randomized, 60 were assigned to the control group and 64 were assigned to the Mobile health (mHealth) group. No statistically significant differences were found between the groups in terms of maternal age, gestational age at first visit, family history, education level, chronic hypertension, abortion history, nulliparity, previous GDM, assisted reproductive technology, history of macrosomia childbirth, the value of HbAlc at diagnosis, oral glucose tolerance test (OGTT) values at diagnosis (p > 0.05). No statistical differences were found in pre-pregnancy BMI or weight gain at first visit, No statistical difference was found between the groups in overweight (%) and obesity (%). Weight was measured before delivery, the comparison in two groups after treatment showed that the weight gain of the mHealth group was less than the control group (3.2 ± 0.8 vs. 4.8 ± 0.7, t = 11.851, df = 122 p < 0.001) (Table 1).
The glycemic control characteristics are shown in Table 2. Patient compliance defined as the actual blood glucose measurements/instructed measurements X100, was higher in the mHealth group as compared to the control group (83.3 ± 12.5% vs. 70.4 ± 10.1%, t = − 6.293, df = 122, p < 0.001). Frequency of outpatient service in mHealth group was less than in the control group. (8.1 ± 1.3 vs. 11.2 ± 1.1, t = 14.285, df = 122, p < 0.001). Hemoglobin A1C before delivery was lower in mHealth group compared to the control group (4.7 ± 0.2 vs. 5.3 ± 0.3, t = 13.216, df = 122, p < 0.001), as well as the rates of off-target measurements both fasting (4.6 ± 0.4% vs. 8.3 ± 0.6%, t = 40.659, df = 122, p < 0.001) and 2 h post-prandial(7.9 ± 0.7% vs. 14.7 ± 0.8%, t = 50.746, df = 122, p < 0.001). No statistical difference was found between the groups in OGGT-fasting or 120 min value at diagnosis, or OGTT-fasting value after 3 months of delivery.
Delivery characteristics and neonatal outcomes are summarized in Table 3. There were no differences between the groups in any of the measured characteristics and outcomes.
Discussion
HAPO’s studies have shown that patients with gestational diabetes increases in blood glucose levels are associated with the corresponding increase in the risk of adverse pregnancy outcomes for mothers and infants [12]. The basic aim of GDM therapy is both to control diet and increase activity levels. Because patients have only limited opportunities to directly interact with a doctor, they often forget the specific medical advice offered by their physicians in a short time. As such, medical personnel are constantly looking for better ways to encourage healthy behavior. An advanced mobile medical App based on smartphones can remind patients to monitor their blood glucose on time, and can be used for daily doctor–patient communication and feedback, urging patients to conduct self-glycemic monitoring and improve compliance, so as to jointly improve medical results.
Emerging mobile medical (mhealth) technology has offered a new medical management model for the mobility, digitization and high efficiency management of diabetes mellitus, and as a result this approach has become popular topic at home and abroad [13,14,15].
Ming et al. study on telemedicine for gestational diabetes mellitus showed a decrease in HbA1c levels, which is consistent with the results of our study [16]. In this study, the mobile health (mHealth) group showed higher compliance with blood glucose monitoring, lower hemoglobin A1C levels before delivery, and a lower percentage of off-target fasting glucose and 2 h post-prandial glucose measurements. The number of outpatient visits in the mHealth group patients decreased. The patients were able to upload blood glucose, diet and exercise information at any time through their mobile phones. The education nurse was additionally available for online instruction every night and urged the patient to measure blood glucose on time. The doctor promptly identified problems and communicated these with the patient to rapidly provide the correct medical guidance. All these innovations serve to increase patients’ compliance, make it easier to achieve normal blood glucose, and save patients’ time and money.
The “Fetal Metabolism Programming Hypothesis” states that malnutrition or overnutrition during early life, including during pregnancy and/or lactation, have a long-term adverse effect on children, leading to a significantly higher risk of metabolic diseases such as obesity, diabetes, and cardiovascular disease in adulthood [17]. Therefore, the monitoring and control of BMI is of great importance for patients with GMD. Weight during pregnancy should be strictly controlled and individual guidance should be given based on a patient’s BMI to effectively minimize adverse outcomes for mother and child and to reduce the incidence of long-term metabolic syndrome in children [18,19,20]. In this study, there was no statistical difference in the pre-pregnancy BMI and weight gain at the time of treatment. After treatment, the mobile health (mHealth) group gained less weight than the control group. These patients uploaded the diet and exercise condition each day through the mobile phone App, while the education nurses communicated with the patients in real time and provided information on an appropriate diabetes-friendly diet education if the uploaded data suggested inappropriate nutrition. This led to better control of daily total calorie intake, allowing for improved blood glucose control thanks to a reasonable diet. Improved diets reduced rates of weight gain in pregnant women, thereby reducing the rate of adverse delivery outcomes and the risk that their children will suffer from metabolic diseases. Compared with the control group, the mHealth group exhibited improved GDM self-management behavior, and this management efficiency was improved through individualized remote guidance.
Studies have shown that pregnancy outcomes are closely linked to blood glucose and weight control in expectant mothers. Strict control of blood glucose and good compliance can reduce maternal and fetal complications during delivery. Blood glucose monitoring is the main mean by which doctors are able to develop glucose reduction protocols for GDM patients, and patients with GDM can benefit from advanced technology platforms to improve their compliance and thus improve pregnancy outcomes [21, 22].
Our research also has limitations. First, the study found that the mHealth group had a clear improvement in the control of blood glucose and body weight among these GDM patients; however, there was no statistically significant difference between these two groups in terms of pregnancy outcomes. We were able to identify some trends, such as the lower incidence of macrosomia and the lower incidence of adverse risk to newborns in the mHealth group. Second, our study only included patients with smartphones and proficiency in the use of mobile Apps, the majority of whom already have a high level of cultural literacy, indicating that the included participants may not be representative of expectant mothers in high-risk and low socioeconomic groups. Third, this study currently lacks long-term follow-up, and the research on the impact of Mobile Health intervention on postpartum progression to type 2 diabetes in patients with gestational diabetes is insufficient. We plan to conduct further research on this in the future.
In conclusion, advanced mobile medical technology can be used to facilitate communication and feedback between doctors and patients in real time, thereby improving the medical outcomes. In this study, the mHealth group exhibited good compliance and ideal blood glucose and weight control, thus reducing rates of complications for pregnant women and fetuses during delivery.
References
DeSisto CL, Kim SY, Sharma AJ (2014) Prevalence estimates of gestational diabetes mellitus in the United States. Pregnancy risk assessment monitoring system (PRAMS) 2007–2010. Prev Chronic Dis 11:E104
Nguyen CL, Pham NM, Binns CW, Duong DV, Lee AH (2018) Prevalence of Gestational diabetes mellitus in Eastern and Southeastern Asia: a systematic review and meta-analysis. J Diabetes Res 2018:6536974
Guariguata L, Linnenkamp U, Beagley J, Whiting DR, Cho NH (2014) Global estimates of the prevalence of hyperglycaemia in pregnancy. Diatetes Res Clin Pract 103(2):176–185
Zhu WW, Yang HX, Wei YM, Yan J, Wang ZL, Li XL et al (2013) Evaluation of the value of fasting plasma glucose in the first prenatal visit to diagnose gestational diabetes mellitus in china. Diabetes Care 36(3):586–590
Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB (2016) Change in obesity prevalence across the United States is influenced by recreational and healthcare contexts, food environments, and hispanic populations. PLoS One 11(2):e0148394
Jenum KA, Richardsen KR, Berntsen S, Mørkrid K (2013) Gestational diabetes, insulin resistance and physical activity in pregnancy in a multi-ethnic population—a public health perspective. Norsk Epidemiol 23(1):45–54
Yogev Y, Xenakis EM, Langer O (2004) The association between preeclampsia and the severity of gestational diabetes: the impact of glycemic control. Am J Obstet Gynecol 191(5):1655–1660
Skupień J, Cyganek K, Małecki MT (2014) Diabetic pregnancy: an overview of current guidelines and clinical practice. Curr Opin Obstet Gynecol 26(6):431–437
Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P (2012) Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med 10:47
Jo S, Park HA (2016) Development and evaluation of a smartphone application for managing gestational diabetes mellitus. Healthc Inform Res 22(1):11–21
Given JE, Bunting BP, O’Kane MJ, Dunne F, Coates VE (2015) Tele-Mum: a feasibility study for a randomized controlled trial exploring the potential for telemedicine in the diabetes care of those with gestational diabetes. Diabetes Technol Ther 17(12):880–888
HAPO Study Cooperative Research Group (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002
Mirember H, Ben-Ari T, Betzer T, Raphaeli H, Gasnier R, Barda G et al (2018) The impact of a daily smartphone-based feedback system among women with gestational diabetes on compliance, glycemic control, satisfaction, and pregnancy outcome: a randomized controlled trial. Am J Obstet Gynecol 218(4):453.e1–453.e7
Skar JB, Garnweidner-Holme LM, Lukasse M, Terragni L (2018) Women’s experiences with using a smartphone app (the pregnant + app) to manage gestational diabetes mellitus in a randomised controlled trial. Midwifery 58:102–108
Payne HE, Lister C, West JH, Bernhardt JM (2015) Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR Mhealth Uhealth 3(1):e20
Ming WK, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, Levy JC et al (2016) Telemedicine technologies for diabetes in pregnancy: a systematic review and meta-analysis. J Med Internet Res 18(11):e290
Kennelly MA, Ainscough K, Lindsay K, Gibney E, Mc Carthy M, McAuliffe FM (2016) Pregnancy, exercise and nutrition research study with smart phone app support (pears): study protocol of a randomized controlled trial. Contemp Clin Trials 46:92–99
Hirst JE, Mackillop L, Loerup L, Kevat DA, Bartlett K, Gibson O et al (2015) Acceptability and user satisfaction of a smartphone-based, interactive blood glucose management system in women with gestational diabetes mellitus. J Diabetes Sci Technol 9(1):111–115
Brown J, Ceysens G, Boulvain M (2017) Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst Rev 6:CD012202
Leng JH, Li WQ, Zhang S, Liu HK, Wang LS, Liu GS et al (2015) GDM women’s pre-pregnancy overweight/obesity and gestational weight gain on offspring overweight status. PLoS One 10(6):e129536
Polsky S, Garcetti R (2017) CGM, pregnancy, and remote monitoring. Diabetes Technol Ther 19(s3):S49–S59
Roeckner JT, Sanchez-Ramos L, Jijon-Knupp R, Kaunitz AM (2016) Single abnormal value on 3-h oral glucose tolerance test during pregnancy is associated with adverse maternal and neonatal outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol 215(3):287–297
Funding
This work was supported by the National Natural Science Foundation of China (no. 81470187). Natural Science Foundation of Tianjin (no. 15ZXHLSY00460). Startup Funding of Scientific Research, Tianjin Medical University Metabolic Diseases Hospital and Tianjin Institute of Endocrinology (no. 2016DX02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Guo, H., Zhang, Y., Li, P. et al. Evaluating the effects of mobile health intervention on weight management, glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus. J Endocrinol Invest 42, 709–714 (2019). https://doi.org/10.1007/s40618-018-0975-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0975-0