Abstract
Purpose
According to American Thyroid Association (ATA) guideline, papillary thyroid cancer (PTC) with minimal extrathyroidal extension (mETE) is classified at “intermediate risk” of persistent/recurrent disease. However, the impact of mETE per se on patients’ outcome is not fully understood. The aim of our study was to evaluate the prognostic significance of mETE in patients with PTC not submitted to therapeutic or prophylactic lymph node dissection, according to tumor size and other prognostic factors.
Patients and methods
We retrospectively evaluated a total of 514 PTC patients: 127 (24.7%) had mETE (pT3Nx) and 387 (75.3%) had negative margins (pT1-2Nx). At a median follow-up of 9.1 years, patients were divided in two groups: patients with “good outcome” (no evidence of disease) and patients with “poor outcome” (persistent structural disease or recurrent disease or tumor-related death).
Results
The rate of patients with “poor outcome” was significantly higher in patients with mETE compared with patients with negative margins (11.8 versus 5.1%; OR 2.4576, 95% CI 1.2178–4.9594, p = 0.01). However, mETE was significantly associated with poor outcome only in patients with tumors larger than 1.5 cm.
Conclusions
mETE is an unfavorable prognostic factor in tumors larger than 1.5 cm, suggesting that, in the absence of other unfavorable characteristics, smaller tumors with mETE should be classified and managed as “low risk” tumors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extrathyroidal extension of PTC is one of the pathological features predicting a poor prognosis, and has been classified in two grades of extension: “minimal extrathyroidal extension (mETE)” (primary tumor extension to the sternothyroid muscle and/or perithyroid soft tissue) or “extensive extrathyroidal extension” (primary tumor extension to subcutaneous soft tissue, trachea, larynx, esophagus or laryngeal nerves) [1].
While extensive extrathyroidal extension has been associated with mortality and recurrence in patients with PTC [2, 3], the real impact of mETE on clinical outcome is less clear, in particular for small PTC [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Some studies report that the presence of mETE carries a worse outcome [4,5,6,7,8]. However, other studies did not confirm these data and reported that mETE is not associated with reduced disease-free survival (DFS) [9,10,11,12,13,14,15,16,17,18] or increased mortality [19]. In particular, Ito et al. [9], found no difference in DFS between patients with or without mETE, even when adjusted for tumor size.
Recently the American Thyroid Association (ATA) guidelines [20], confirmed that mETE should be considered as a criterion for classifying patients at intermediate risk of recurrence, possibly leading to completion thyroidectomy and radioactive iodine (RAI) ablation [21, 22]. On the contrary, in the recent updated of AJCC/TNM Staging System for Differentiated thyroid cancer, mETE detected only on histological examination was removed from the definition of T3 disease, and therefore, has no impact on either T category or overall stage [23].
The aim of the present study was to evaluate the prognostic significance of mETE in patients with PTC not submitted to prophylactic lymphadenectomy, according to tumor size and other prognostic variables.
Patients and methods
Study group
Epidemiological and clinical features of patients are reported in Table 1. We retrospectively reviewed 514 patients with PTC treated with total thyroidectomy without therapeutic or prophylactic lymph node dissection at the Section of Endocrinology, University of Siena, Italy. Inclusion criterion was the absence of clinical lymph node metastases at the pre-surgical evaluation and at histology. Exclusion criterion was the presence of macroscopical extrathyroidal extension. There were 375 females (73%) and 139 males (27%), aged 6–84 years (mean ± SD = 48.5 ± 15.4) at the time of diagnosis. After surgery, 418/514 patients (81.3%) received RAI ablation therapy at median activity of 2627 Mbq (range 555–5550 MBq). One hundred and eighty-five/514 (36%) patients had multifocal PTC in one lobe and 126/514 (24.5%) had bilateral tumors. Aggressive variants of PTC were present in 49/514 (9.5%) patients. mETE (defined as tumor cells extending to the sternothyroid muscle and/or parathyroid soft tissue) [1] was documented in 127/514 (24.7%) patients. Median follow-up was 9.1 years. As a standard procedure, patients had given their consent for using their data for research purpose.
Criteria used to define the clinical status
At the end of follow-up patients with undetectable basal and/or stimulated serum thyroglobulin (Tg), negative AbTg and no evidence of disease (at clinical examination, neck ultrasound (US), and diagnostic 131-I whole body scan (WBS) when performed) were defined in complete remission. Patients with detectable basal and/or stimulated serum Tg but no evidence of disease at cross sectional imaging (at chest X-ray, 131I WBS, 18FDG-PET, CT, MRI, bone scan) were classified as having biochemical disease. Structural disease was defined as the presence of radiological, cytological or histological evidence of disease. Both biochemical and structural disease was defined as recurrence when detected in patients previously defined in clinical remission.
Statistical analysis
Epidemiological data are presented as the mean ± SD and median when needed. The t test for independent data was performed for normal variables. To evaluate significant differences in data frequency we analyzed contingency tables. Tables with size larger than 2 × 2 were examined by the Chi-squared test or a numerical approximation of the Fisher exact test, when all cell frequencies were greater than 4 or not, respectively. The following variables were studied by univariate analysis: age at diagnosis, sex, mETE, multifocality, bilaterality, tumor diameter and adverse histology. Statistically significant variables found in univariate analysis were entered into a binary logistic regression analysis to identify those with independent prognostic significance and to calculate the odds ratio. To perform this analysis, patients were classified as having a “good outcome” when they did not have structural evidence of disease. Patients with structural persistent disease, with recurrent disease or patients dead for thyroid cancer were classified as having “poor outcome”. A CHAID (Chi-squared Automatic Interaction Detection) decision tree analysis was applied to identify prognostic factors and to determine their relationship with the clinical outcome.
For this analysis, clinical outcome (“good outcome” or “poor outcome”) was the dependent variable and patient/tumor characteristics statistically significant at univariate analysis were included as covariate. Statistical analysis was performed using the software StatView for Windows version 5.0.1 (SAS Institute, Cary, NC, USA) and the SPSS Statistics version 22.0. A p value < 0.05 was considered statistically significant.
Results
Comparison of patients with (Group 1) and without (Group 2) minimal extrathyroidal extension (mETE)
According to the pathology report, patients were divided in two groups: Group 1 including 127 (24.7%) patients with mETE (pT3) and Group 2 including 387 (75.3%) patients with negative margins (pT1-T2). Clinical and pathological data (age, sex, use of adjuvant RAI, tumor size, multifocality, bilaterality, aggressive histology, tumor stage and follow-up duration) are shown in Table 2. Ablation patients in Group 1 (pT3) were more likely to have multifocal PTC (44.1 versus 33.3%, p = 0.03), bilateral disease (36.2 versus 20.7%, p = 0.0008), aggressive variant of PTC (19.7 versus 6.2%, p < 0.0001) and were more likely to receive radioactive ablation therapy (96 versus 76.5%, p < 0.0001) when compared with Group 2 patients.
Clinical outcome in patients with (Group 1) and without (Group 2) minimal extrathyroidal extension (mETE)
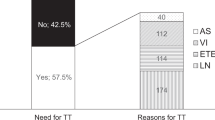
At the end of follow-up, the clinical outcome was significantly different between the two groups (p = 0.03). This difference was due to the higher rate of persistent structural disease (7.1 versus 2.0%, p = 0.02) and a lower rate of clinical remission (80.3 versus 89.7%, p = 0.008) in Group 1 patients when compared with Group 2. On the contrary, the rate of persistent biochemical disease, recurrent disease and mortality was not statistically different between Group 1 and Group 2 (Fig. 1).
Risk factors for poor outcome at last follow-up (univariate and multivariate analysis)
At univariate analysis significant risk factors for “poor outcome” were age greater than 55 years (p = 0.04), mETE (p = 0.01), tumor diameter (p < 0.0001) and aggressive variant of PTC (p = 0.01) but not male sex (p = 0.32), multifocality (p = 0.17) and bilaterality (p = 0.44). With multivariate analysis, only mETE, tumor diameter and age greater than 55 years were significantly and independently associated with the clinical status at the last follow-up. However, the large tumor diameter was found to be the strongest predictor for poor outcome (Odd ratio 1.77; 95% CI 1.415–2.224, p = 0.000) (Table 3).
Final outcome according to tumor margins (mETE yes/not) and tumor size
To evaluate the clinical impact of mETE according to the tumor size, we compared the clinical status according to the presence/absence of mETE in 3 subgroups of patients: PTC patients with tumor diameter ≤ 1 cm, with tumor diameter > 1 and ≤ 1.5 cm and with tumor diameter > 1.5 cm. The rate of patients with “poor outcome” was similar in Group 1 and 2 when patients had tumor diameter ≤ 1 cm [1/39 (2.5%) and 2/163 (1.2%), p = 0.47] or between 1 and 1.5 cm [1/38 (2.6%) versus 4/81 (1.2%), p > 0.99] whereas a significant worse outcome was observed in Group 1 with tumor diameter > 1.5 cm compared with Group 2 patients [13/50 (26.0%) versus 14/132 (10.6%), p = 0.01] (Fig. 2).
Identification of patients’ subgroups with different clinical outcome using a “CHAID tree-building algorithm”
We analyzed whether the mETE was associated with the clinical outcome also in a multivariate model, using a “CHAID tree-building algorithm”, integrating different prognostic factors significantly associated at univariate analysis such as: older age, tumor size, minimal extrathyroidal extension and adverse histology. A CHAID (Chi-squared Automatic Interaction Detection) decision tree analysis was applied to identify prognostic factors and determine their relationship with clinical outcome of PTC patients.
The CHAID algorithm first split the patients exclusively according to the tumor size. The rate of poor outcome rose from 6.8% in the whole cohort to 14.8% in patients with tumors > 1.5 cm (p = 0.000, x2 = 29). mETE was predictor of poor outcome only in tumor larger than 1.5 cm. The rate of poor outcome rose from 6.8% in the whole cohort to 26.0% in patients with tumors > 1.5 cm and mETE (p = 0.009, x2 = 6). In the cohort of patients with tumor diameter ≤ 1 cm the rate of poor outcome rose significantly in patients older than 55 years (from 1.4 to 3.9%; p = 0.019; x2 = 5) (Fig. 3).
Discussion
mETE is a controversial prognostic factors in PTC. Although some studies reported that the presence of mETE is related to a lower rate of disease-free-survival [4, 5, 7, 8] and overall survival [6], other authors have reported that mETE is not correlated with worse outcome in PTC patients [9,10,11,12,13,14,15,16,17,18,19]. A recent metanalysis concluded that mETE is a risk factor for poor prognosis in patients with PTC [8]. However, the authors hypothesized that a worse prognosis could be due to the higher rate of bilateral involvement, the larger tumor size and the higher rate of lymph node metastases in patients with mETE compared with patients without mETE [8]. In the majority of the studies evaluating the prognostic significance of mETE, using a multivariate analysis, lymph node metastases were found to be the only or the strongest predictor factor for poor outcome in PTC patients [9, 13, 15, 16, 18].
For this reason and to better understand what is the impact of the presence of mETE in PTC, we excluded from the study group, patients with lymph node metastases at diagnosis. According to previous studies [13,14,15, 17, 18], our patients with mETE were more likely to have multifocal PTC, bilateral disease, and aggressive variant of PTC. At a median follow-up of 9.1 years, the rate of patients with poor outcome (structural disease/death/recurrent disease) was significantly higher in patients with mETE compared to patients with negative margins. This difference was due to a higher rate of persistence structural disease while the persistent biochemical disease, the mortality and the recurrence rates were similar between PTC patients with and without mETE. The clinical impact of mETE has been also confirmed at binary logistic regression analysis together with older age (> 55 years) and tumor diameter. However, using a CHAID decision tree analysis, tumor size was the strongest predictor of poor outcome, indicating that tumor diameter > 1.5 cm increased the risk of poor outcome in PTC patients. mETE was predictor of poor outcome only in tumor larger than 1.5 cm and the risk of poor outcome is further increased in patients with tumors larger than 1.5 cm and mETE. On the contrary, in smaller tumor (≤ 1.5 cm) with mETE, older age was the best prognostic indicator of poor prognosis. Accordingly to our results, several studies performed in patients with microPTC, did not report any association between mETE and poor outcome [12, 14, 16]. Similarly, Kluijfhout et al. [18] reported that a microscopic positive margin found only on final pathology does not increase the risk of recurrence in T1-T2 differentiated thyroid carcinoma. More recently, it has been reported that patients with tumor diameter < 4 cm with mETE had no significant worse survival compared to patients with tumor diameter < 4 cm without mETE [19]. Our results support the recent update of the TNM/AJCC staging system where minor extrathyroidal extension detected only on histological examination was removed from the definition of T3 disease, and therefore, has no impact on either T category or overall stage [23]. The TNM/AJCC system is optimized to predict survival in patients with cancer and, in our study, the mortality rate was not different in patients with and without mETE. On the contrary, our results do not completely support the recent ATA risk stratification in which all patients with mETE are upgraded to intermediate risk group regardless the tumor size [20]. We demonstrate that the prognostic impact of mETE is related to tumor diameter and that small tumor size (≤ 1.5 cm) with mETE did not have any greater risk of persistent structural/recurrent disease when compared with small tumor size without mETE. According to our results, patients with small tumor (< 1.5 cm) should be classified as low risk. After surgery, the management of these patients should be defined according to their real risk of persistent/recurrent disease. Radioiodine remnant ablation could not be necessary in most of them. For this reason a selective use of radioiodine based on serum Tg levels and neck US after surgery, might be useful in these patients.
Some limitations of this study are intrinsic to its retrospective nature, particularly the performance of initial surgery at different institutions. Nonetheless, the data have several strengths including a similar post-surgery therapeutic approach and follow-up strategies in the same institution. In addition, to our knowledge, this is the first study evaluating the clinical impact of mETE in patients with PTC after exclusion of patients with lymph node metastases.
In conclusion, according to our results, in patients with PTC without lymph node metastases at diagnosis, mETE is an unfavorable prognostic factor only in tumor larger than 1.5 cm. On the contrary, in tumor ≤ 1.5 cm mETE is not an unfavorable prognostic factor and thus, in the absence of other unfavorable characteristics, these tumors should be classified and managed as “low risk” tumors.
References
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474. https://doi.org/10.1245/s10434-010-0985-4
Andersen PE, Kinsella J, Loree TR, Shaha AR, Shah JP (1995) Differentiated carcinoma of the thyroid with extrathyroidal extension. Am J Surg 170:467–470
Ortiz S, Rodríguez JM, Soria T, Pérez-Flores D, Piñero A, Moreno J, Parrilla P (2001) Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg 124:261–265
Santos MJ, Bugalho MJ (2016) Papillary thyroid carcinoma: different clinical behavior among pT3 tumors. Endocrine 53:754–760. https://doi.org/10.1007/s12020-016-0927-4
Jung SP, Kim M, Choe JH, Kim JS, Nam SJ, Kim JH (2013) Clinical implication of cancer adhesion in papillary thyroid carcinoma: clinicopathologic characteristics and prognosis analyzed with degree of extrathyroidal extension. World J Surg 37:1606–1613. https://doi.org/10.1007/s00268-013-2034-5
Youngwirth LM, Adam MA, Scheri RP, Roman SA, Sosa JA (2017) Extrathyroidal extension is associated with compromised survival in patients with thyroid cancer. Thyroid 27(5):626–631. https://doi.org/10.1089/thy.2016.0132
Radowsky JS, Howard RS, Burch HB, Stojadinovic A (2014) Impact of degree of extrathyroidal extension of disease on papillary thyroid cancer outcome. Thyroid 24:241–244. https://doi.org/10.1089/thy.2012.0567
Yin DT, Yu K, Lu RQ, Li X, Xu J, Lei M (2016) Prognostic impact of minimal extrathyroidal extension in papillary thyroid carcinoma. Medicine (Baltimore) 95(52):e5794. https://doi.org/10.1097/MD.0000000000005794
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A (2006) Prognostic significance of extrathyroid extension of papillary thyroid carcinoma: massive but not minimal extension affects the relapse-free survival. World J Surg 30:780–786
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A (2006) Minimal extrathyroid extension does not affect the relapse-free survival of patients with papillary thyroid carcinoma measuring 4 cm or less over the age of 45 years. Surg Today 36:12–18
Arora N, Turbendian HK, Scognamiglio T, Wagner PL, Goldsmith SJ, Zarnegar R, Fahey TJ 3rd (2008) Extrathyroidal extension is not all equal: implications of macroscopic versus microscopic extent in papillary thyroid carcinoma. Surgery 144:942–947. https://doi.org/10.1016/j.surg.2008.07.023
Moon HJ, Kim EK, Chung WY, Yoon JH, Kwak JY (2011) Minimal extrathyroidal extension in patients with papillary thyroid microcarcinoma: is it a real prognostic factor? Ann Surg Oncol 18:1916–1923. https://doi.org/10.1245/s10434-011-1556-z
Shin JH, Ha TK, Park HK, Ahn MS, Kim KH, Bae KB, Kim TH, Choi CS, Kim TK, Bae SK, Kim SH (2013) Implication of minimal extrathyroidal extension as a prognostic factor in papillary thyroid carcinoma. Int J Surg 11:944–947. https://doi.org/10.1016/j.ijsu.2013.06.015
Ahn D, Sohn JH, Jeon JH, Jeong JY (2014) Clinical impact of microscopic extrathyroidal extension in patients with papillary thyroid microcarcinoma treated with hemithyroidectomy. J Endocrinol Invest 37:167–173. https://doi.org/10.1007/s40618-013-0025-x
Jin BJ, Kim MK, Ji YB, Song CM, Park JH, Tae K (2015) Characteristics and significance of minimal and maximal extrathyroidal extension in papillary thyroid carcinoma. Oral Oncol 51:759–763. https://doi.org/10.1016/j.oraloncology.2015.05.010
Woo CG, Sung CO, Choi YM, Kim WG, Kim TY, Shong YK, Kim WB, Hong SJ, Song DE (2015) Clinicopathological significance of minimal extrathyroid extension in solitary papillary thyroid carcinomas. Ann Surg Oncol 22:S728–S733. https://doi.org/10.1245/s10434-015-4659-0
Wang LY, Ghossein R, Palmer FL, Nixon IJ, Tuttle RM, Shaha AR, Shah JP, Patel SG, Ganly I (2015) Microscopic positive margins in differentiated thyroid cancer is not an independent predictor of local failure. Thyroid 25:993–998. https://doi.org/10.1089/thy.2015.0141
Kluijfhout WP, Pasternak JD, Kwon JS, Lim J, Shen WT, Gosnell JE, Khanafshar E, Duh QY, Suh I (2016) Microscopic positive tumor margin does not increase the risk of recurrence in patients with T1–T2 well-differentiated thyroid cancer. Ann Surg Oncol 23:1446–1451. https://doi.org/10.1245/s10434-015-4998-x
Al-Qurayshi Z, Shama MA, Randolph GW, Kandil E (2017) Minimal extrathyroidal extension does not affect survival of well-differentiated thyroid cancer. Endocr Relat Cancer 24:221–226. https://doi.org/10.1530/ERC-16-0509
Haugen BR, Alexander EK, Bible KC et al (2016) American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133. https://doi.org/10.1089/thy.2015.0020
Castagna MG, Cantara S, Pacini F (2016) Reappraisal of the indication for radioiodine thyroid ablation in differentiated thyroid cancer patients. J Endocrinol Invest 39:1087–1094. https://doi.org/10.1007/s40618-016-0503-z
Pacini F, Brianzoni E, Durante C, Elisei R, Ferdeghini M, Fugazzola L, Mariotti S, Pellegriti G (2016) Recommendations for post-surgical thyroid ablation in differentiated thyroid cancer: a 2015 position statement of the Italian Society of Endocrinology. J Endocrinol Invest 39:341–347. https://doi.org/10.1007/s40618-015-0375-7
Tuttle M, Morris LF, Haugen B, Shah J, Sosa JA, Rohren E, Subramaniam RM, Hunt JL, Perrier ND (2017) Thyroid differentiated and anaplastic carcinoma (Chapter 73). In: Amin MB, Edge SB, Greene F, Byrd D, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC, Jessup JM et al (eds) AJCC cancer staging manual, 8th edn. Springer International Publishing, New York City
Funding
This work was supported in part by Grants from the Italian Ministry of Health (Grant #RF-2011-02950673).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Castagna, M.G., Forleo, R., Maino, F. et al. Small papillary thyroid carcinoma with minimal extrathyroidal extension should be managed as ATA low-risk tumor. J Endocrinol Invest 41, 1029–1035 (2018). https://doi.org/10.1007/s40618-018-0854-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0854-8