Abstract
Purpose
Gender dysphoria (GD) is associated with clinically significant distress and impairment in social, scholastic, and other important areas of functioning, especially when early onset is reported. The aim of the present study is to assess the psychopathological features associated with GD in adolescence, comparing a group of gender dysphoric adolescents (GDs) with a group of non-referred adolescents (NRs), in terms of body uneasiness, suicide risk, psychological functioning, and intensity of GD.
Methods
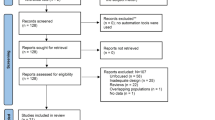
A sample of 46 adolescents with GD and 46 age-matched NRs was evaluated (mean ± SD age = 16.00 ± 1.49 and 16.59 ± 1.11 respectively, p > 0.05). Subjects were asked to complete the Body Uneasiness Test (BUT) to explore body uneasiness, the Youth Self Report (YSR) to measure psychological functioning, the Multi-Attitude Suicide Tendency Scale (MAST) for suicide risk, and the Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults (GIDYQ-AA) for GD assessment.
Results
Adolescents with GD reported significantly higher levels of body uneasiness (BUT-GSI, F = 380.13, p < 0.0001), as well as a worse psychological functioning (YSR, F = 13.06 and p < 0.0001 for “total problem scale” and F = 12.53, p = 0.001 for “internalizing” scale) as compared to NRs. When YSR subscales were considered, GDs showed significantly higher scores in the “withdrawal/depression”, “anxiety/depression”, and “social problems” (all p < 0.0001). In addition, GDs showed significantly higher levels in the “attraction to death” and “repulsion by life” scales and lower scores in the “attraction to life” scale (all p < 0.0001). Finally, GIDYQ-AA score was significantly lower (meaning a higher level of gender dysphoria symptoms) in GDs vs. NRs (p < 0.0001).
Conclusions
GD adolescents reported significantly higher body dissatisfaction and suicidal risk compared to NRs. In addition, results confirmed a significant impairment in social psychological functioning in adolescents with GD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gender dysphoria (GD) is a condition characterized by a marked incongruence between one’s experienced/expressed gender and the assigned one, and is associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning, especially when an early onset is reported [1]. Indeed, gender dysphoric youths are described as a psychologically and socially vulnerable population. Several studies have reported that young people with GD more often show behavioral and emotional problems as compared with peers, and, in particular, significantly higher levels of internalizing problems (i.e., inner-directed and generating distress in the individual) than externalizing ones (i.e., outer-directed and generating discomfort and conflict in the surrounding environment) [2–5]. In addition, this population suffers from higher rates of suicidality (i.e., suicidal thoughts, suicide attempts, and rates) and self-harm behaviors; in both cases, age has been identified as an important vulnerability factor [6–10].
Psychological functioning is described as negatively affected by social marginalization and poor relations with peers [2, 11]. Indeed, the strongest predictors of co-occurring psychopathologies seem to be social ostracism and peer victimization, mainly related to low tolerance and acceptance of gender-variant behaviors [2, 12]. Furthermore, the difficulties experienced by adolescents with GD to connect socially and romantically with peers in the desired gender role may contribute to increased bulling and violence risk [3]. A cross-clinic comparative study on adolescents referring to a Canadian and a Dutch gender clinic showed significantly more behavioral and emotional problems in the Toronto-referred sample as compared with the Amsterdam one [2]. According to the authors, this result may reflect the effect of a lower acceptance of gender non-conforming youth in some societies as compared to others [2, 13–15].
Although the Italian context has been reported as being poorly able to properly deal with gender dysphoric adolescents [3], studies investigating the psychological functioning of this population are lacking. In addition, although the centrality of body image concerns in GD development is well established [16–24], there are no studies investigating levels of body uneasiness in gender dysphoric adolescents.
Aims
To assess psychopathological features associated with GD in adolescence, comparing a group of gender dysphoric adolescents (GDs) with a group of non-referred adolescents (NRs), in terms of body uneasiness, suicide risk, and psychological functioning.
Methods
Study design
The study was conducted at the Sexual Medicine and Andrology Unit of the University of Florence and in the Gender Clinics of Rome, Milan, and Naples University Hospitals.
A consecutive series of gender-referred adolescents was evaluated on the first day of admission to the clinics by means of a clinical and psychometric assessment. In addition, a control group of non-referred (NRs) schoolmates was also considered.
The study protocol was approved by the Institution’s Ethics Committee.
Study procedures were fully explained during the first routine visit and prior to the data collection; after that, all the patients and control subjects as well as their parents provided a written informed consent to participate in the study.
Participants
Gender-referred adolescents attending several Italian Gender Clinics were enrolled in the study between September 2014 and February 2016, provided that they met the following inclusion criteria:
-
Age younger than 18 years;
-
Diagnosis of GD based on formal psychiatric classification criteria [1] and performed through several sessions with two different mental health professionals with a specific training in child and adolescent developmental psychopathology and skilled in GD.
For the NRs group, the inclusion criteria included age below 18 years.
The exclusion criteria for both cases and controls were as follows:
-
The use at any point in life of gonadotropin-releasing hormone analogues and cross-sex hormonal treatment;
-
genital reassignment surgery;
-
illiteracy;
-
mental retardation.
Measures
Socio-demographic and clinical data were collected from both groups. In addition, GDs and NRs were asked to complete several psychometric tests, such as the Body Uneasiness Test (BUT, [25–27]), the Multi-Attitude Suicide Tendency Scale for adolescents (MAST [28–31]), the Youth Self Report (YSR, [32, 33]), and the Gender Identity/Gender Dysphoria Questionnaire (GIDYQ-AA, [34, 35]).
The Body Uneasiness Test (BUT, [27]) is a self-rating scale exploring different areas of body-related psychopathology [25, 26]. The instrument is composed of two parts: BUT-A (34 items) and BUT-B (37 items). The BUT-A explores five areas: weight phobia (WP, fear of being or becoming fat), body image concerns (BIC, i.e. worries related to physical appearance), avoidance (A; body image related avoidance behavior); compulsive self-monitoring (CSM; compulsive checking of physical appearance) and depersonalization (D; detachment and estrangement feelings toward the body). Mean scores of the items composing each subscale are obtained, together with a Global Severity Index (GSI), that is the average rating of all 34 items composing the BUT-A. The BUT-B lists 37 body parts and functions, asking respondents to rate how often they happen to dislike each experience or each body part. Two scores are derived from respondents’ ratings to the BUT-B: the positive symptom total (PST, i.e., the number of symptoms rated higher than zero) and the Positive Symptom Distress Index (PSDI, i.e., the average rating of those items constituting the PSI). For all subscales, higher scores indicate greater body uneasiness.
Behavioral and emotional problems were assessed through the Italian version of the YSR [33]. The YSR tests are part of the system of evaluation on an empirical basis by Achenbach et al. [32, 33, 36] and aim to evaluate the presence of potentially problematic behaviors listed within behavioral scales. The answers can be rated on a three-point scale (0 = not true; 1 = sometimes true; 2 = very true). The scales consist of about 100 items, grouped in 8 syndrome scales according to a dimensional approach: “anxiety and depression” (evaluates the presence of depressive symptoms such as sadness, irritability, loneliness, low self-esteem, and not feeling loved); “withdrawal and depression” (evaluates social closure, tendency to isolate, shyness, and discretion); “somatic complaints” (evaluates the tendency to express anxiety and concern through physical disorders such as nausea, stomach pain, and headache); “social problems” (evaluates the difficulty within the relationships with peers such as being teased and not getting along with peers); “problems of thought” (evaluates the presence of thoughts and perceptions that are not reflected in reality); “problems of attention” (evaluates the difficulty in maintaining concentration and the tendency towards hyperactive behaviors such as impulsivity, irritability, and motor restlessness); “rule transgression behavior” (evaluates the tendency to assume delinquent behaviors such as stealing, lying, setting fires, and using alcohol or drugs); and “aggressive behavior” (evaluates the presence of aggressive, provocative, and destructive behaviors towards people or property). Moreover, it is possible to evaluate behavior through the following three general scales: the “total problem scale”, as well as the “internalizing” scale (i.e., indicating inner-directed behaviors and generating distress in the individual) and the “externalizing” scale (i.e., indicating outer-directed behaviors and generating discomfort and conflict in the surrounding environment). Regarding psychometric properties, Achenbach et al. [32, 33] can be consulted.
The MAST is a 30-item scale, which measures attitudes on four components: “attraction to life”, “attraction to death”, “repulsion by life”, and “repulsion by death” [28, 29]. In particular, the “repulsion by life” component reflects such experiences as pain and stress; “attraction to death” represents religious convictions or perceptions that death is a superior way of being; “attraction to life” is based on the degree of satisfaction with life and a sense of well-being; and “repulsion by death” reflects fears of death. Each item is presented on a 5-point scale from 1 (strongly agree) to 5 (strongly disagree). To facilitate interpretation of data analyses, the items for each subscale were reverse scored. A mean item response is calculated for each of the four attitude subscales, with higher scores reflecting greater agreement. Studies validating an Italian version of the MAST are not available yet, although some preliminary data on its the reliability and validity have been provided [30, 31].
The Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults (GIDYQ-AA) is a 27-item questionnaire evaluating GD [34, 35]. Each item is rated on a 5-point response scale, with the past 12 months as the timeframe. The response options are always (coded as 1), often (2), sometimes (3), rarely (4), or never (5). Lower scores are associated with higher GD. Internal coherence was satisfactory for the Italian validated version (α value of about 0.97 [34, 35]).
Finally, data on reported height and weight were collected to obtain body mass index (BMI).
Statistical analyses
Continuous variables were reported as mean ± standard deviation, or median and quartiles, for non-normally distributed variables, whereas categorical variables were reported as numbers and percentages. The independent sample t test and the χ 2 were used for continuous and categorical variables, respectively, to compare GDs and NRs and male-to-female (MtFs) with female-to-male persons (FtMs). A univariate analysis of variance (ANCOVA) was used to compare the continuous variables among groups, entering age as a covariate and BMI, when appropriate. Post-hoc paired contrasts with Tukey B test were performed for the pairwise comparison among the groups. Pearson’s correlation was used to evaluate the associations between different variables within each group. Finally, linear and logistic regression analyses were used for multivariate analysis (adjusting for age) whenever appropriate. All analyses were performed using SPSS version 23 (SPSS Inc., Chicago, IL, USA).
Results
Differences in terms of psychological well-being between GDs vs. NRs
Of the 47 GDs who met the participation criteria, 46 (97.1%) agreed to participate to the study (mean ± SD age = 16.35 ± 1.32 years). The MtF:FtM sex ratio of the GD sample was 1:1.3. No significant differences were found in terms of age between MtFs and FtMs (16.00 ± 1.49 vs. 16.59 ± 1.11 years old, p > 0.05), as well as in other socio-demographic characteristics, as reported in Table 1.
A control group of 46 NRs, of similar age, was also enrolled (15.78 ± 2.13 years, p = 0.13 vs. GD). The M:F sex ratio of the NR sample was 1:1.6. In addition, GDs did not differ in terms of educational level and rates of parental cohabitation compared to NRs (10.35 ± 0.26 vs. 9.78 ± 0.26 years of education; 97.8 vs. 95.7% cohabited with both parents; both p > 0.05). Moreover, no differences in terms of BMI were found between GDs and NRs (21.62 ± 2.72 vs. 20.76 ± 1.94 kg/m2, p > 0.05).
Because several of the assessed psychological features are generally considered age-correlated, all the following results have been adjusted for age. In addition, because BMI may influence body dissatisfaction [21, 22, 27], all results related to BUT were adjusted also for BMI.
Considering YSR, GD adolescents reported significantly higher T scores in both the “total problems” (60.91 ± 7.46 vs. 55.30 ± 6.16; F = 13.06, p < 0.0001, Fig. 1a) and “internalizing” scales (62.43 ± 11.18 vs. 53.57 ± 11.64; F = 12.53, p = 0.001, Fig. 1b), when compared to NRs. No significant differences were found in the “externalizing” scale (Fig. 1c). The percentage of adolescents scoring in the clinical range (T > 63) on both the “total problems” and “internalizing” scales was significantly higher in GDs vs. NRs (17.4 vs. 10.9 and 47.8 vs. 17.4%, respectively, for the “total problems” and “internalizing” scales; both p < 0.0001). No significant differences were found between the rates of adolescents within the clinical score (T > 63) in the “externalizing” scale (13 vs. 19.6%, p > 0.05).
YSR “total problems”, “internalizing problems”, “externalizing problems” scales (a–c) and “withdrawn/depression”, “anxiety/depression”, and “social problems” subscales (d–f) in GDs and NRs. Statistics: Univariate analysis of variance (ANCOVA) entering age as covariate. YSR Youth Self Report, GDs adolescents with gender dysphoria, NRs non-referred adolescents
When YSR subscales were analyzed, significant differences were found between groups in the “withdrawn/depression”, “anxiety/depression”, and “social problems”, with GDs showing significantly higher scores (all p < 0.005 vs. NRs, Fig. 1d–f).
Considering suicidal risk, according to the MAST test, GDs showed significantly higher scores in the “attraction to death” (2.98 ± 0.57 vs. 2.17 ± 0.58; F = 46.22, p < 0.0001, Fig. 2a) and “repulsion by life” scales (3.04 ± 0.46 vs. 2.08 ± 0.56, F = 78.5, p < 0.0001, Fig. 2b), and lower scores in the “attraction to life” (3.32 ± 0.55 vs. 4.05 ± 0.49, F = 44.14, p < 0.0001, Fig. 2c).
MAST “attraction to death” (a), “repulsion by life” (b), and “attraction to life” (c) scales in GDs and NRs. Statistics: univariate analysis of variance (ANCOVA) entering age as covariate. MAST Multi-Attitude Suicide Tendency Scale, GDs adolescents with gender dysphoria, NRs non-referred adolescents
When BUT was analyzed, GDs showed significantly higher body uneasiness compared with the NRs (BUT-GSI, 3.05 ± 0.49 vs. 0.61 ± 0.58, F = 380.13, p < 0.0001). Accordingly, scores of several BUT subscales (including: “weight phobia”, “depersonalization”, “avoidance”, “compulsive self-monitoring”, “body image concerns”, and “positive symptoms distress index”) were significantly higher in the GD group compared to the NR one (all p < 0.0001, Fig. 3b–g). In addition, GDs showed significantly higher BUT scores when compared with the normative ones (data not shown [26]).
BUT-Global Severity Index (BUG-GSI, a), “weight phobia” (BUT-WP, b), “avoidance” (BUT-AV, c), “compulsive self-monitoring” (BUT-CSM, d), “depersonalization” (BUT-DEP, d), “body image concerns” (BUT-BIC, e), and “Positive Symptoms Distress Index” (BUT-PSDI, g) in the GD group compared to the NR one. Statistics: univariate analysis of variance (ANCOVA) entering age and BMI as covariate. BUT Body Uneasiness Test, GDs adolescents with gender dysphoria, NRs non-referred adolescents
Moreover, GIDYQ-AA score was significantly lower (i.e., a higher level of gender dysphoria symptoms) in GDs vs. NRs (2.27 ± 0.40 vs. 4.92 ± 0.34, F = 1137.77, p < 0.000). Similar results were observed for the subjective indicator of GD (GIDYQ-AA, F = 639.62, p < 0.0001), as well as for the social, somatic, and legal GD indicators (all p < 0.0001).
When the GD sample was stratified according to gender, no significant differences were found in the YSR, MAST, BUT, and GIDYQ-AA scores between MtFs and FtMs (all p > 0.05).
Finally, Table 2 shows body uneasiness related to different body parts as derived by ANCOVA and Post-hoc Tukey B test. Results were obtained by stratifying the total sample according to gender (male NRs, female NRs, MtFs, and FtMs). MtFs showed significantly higher distress as compared to NRs in all the body areas (all p < 0.0001), with the exception of height. In addition, MtFs scored higher than FtMs in specific body areas (head shape, skin, eyes, nose, chin, mustache, beard, shoulders, arms, and knees; all p < 0.005). When FtMs were considered, they scored higher in height, breast, hips, and buttocks when compared to both MtFs and NRs (all p < 0.0001).
Correlates of behavior and emotional problems and body uneasiness in GDs
Considering the GD sample, the YSR total problems T score showed a significant correlation with general body uneasiness levels (BUT-GSI, r = 0.338, p = 0.022, Fig. 4a), as well as with body dissatisfaction related to weight phobia (BUT-WP, r = 0.321, p = 0.030, Fig. 4b) and avoidance (BUT-AV, r = 0.353, p = 0.016, Fig. 4c).
Furthermore, BUT-GSI showed a significant correlation with the legal indicator of gender dysphoria (GIDYQ-AA, r = −0.398, p = 0.006, Fig. 5a). In addition, BUT-GSI was positively correlated with MAST repulsion by life (r = 0.543, p < 0.001, Fig. 5b) and negatively with attraction to life (r = −0.498, p < 0.0001, Fig. 5c).
Correlation between GIDYQ-AA legal indicator, MAST repulsion by life, MAST attraction to life with BUT Global Severity Index in the GD sample (a–c). Statistics: linear regression analyses were used for multivariate analysis (adjusting for age and BMI). GIDYQ-AA Gender Identity Gender Dysphoria Questionnaire for Adolescents and Adults, MAST Multi-Attitude Suicide Tendency scale, BUT Body Uneasiness Test, GD gender dysphoria
All the aforementioned associations were confirmed at multiple linear regression analyses, after adjusting for age.
Discussion
To the best of our knowledge, this is the first study performed in Italy presenting data on the psychopathological correlates of a GD adolescent population. In particular, we provided information regarding body uneasiness, suicidal risk, and psychological distress, which represent relevant moderators of outcome for medical treatment options [37–39]. The main results of the present study are the following: (1) Italian adolescents with GD show significantly higher body uneasiness levels compared with the a group of NR youths of similar age; (2) Italian adolescents with GD show higher suicidal risk than the comparison group; (3) a sex ratio favoring MtFs was found; and (4) psychological problems (higher levels of internalizing condition vs. NR) and social functioning (poorer vs. NR) of Italian adolescents with GD confirm results from the previous studies from different countries.
Even though the centrality of body image concerns in GD development has frequently been reported [16–23], to date, no study had specifically focused on body dissatisfaction in adolescents with GD. Our data show that body-related uneasiness is significantly higher in adolescents with GD compared to a sample of NR pairs. A similar figure was observed when GDs’ BUT scores were compared to normative ones. In addition, when the GD sample was stratified according to gender, a significantly higher distress was observed in sexual dimorphic body parts (e.g., head shape, skin, nose, chin, mustache, beard, shoulders, and arms in MtFs vs. FtMs and in height, breast, hips, and buttock in FtMs vs. MtFs). These body parts are, in fact, gender-related and, once modified by pubertal modifications, they may prevent the adolescent with GD from intermingling with peers and may impair social relationships. Furthermore, the positive correlation observed between body uneasiness levels and poor psychological functioning highlights the important role of body image concerns on psychological well-being. Indeed, body dissatisfaction assessment should be part of clinical practice as it is associated with several psychological outcomes, such as poor self-esteem, sexual dysfunctions, as well as pathological eating behaviors, which may arise as a dysfunctional coping strategy to modify one’s body shape or weight [23, 40, 41]. Therefore, body uneasiness could be responsible of a series of different psychiatric co-occurring problems, including depression, eating disorders, and social phobia, which could interfere with both the psychological and medical treatments in GD adolescents.
In line with international recommendations [3, 42, 43], these results stress the importance of providing the early medical interventions, such as pubertal suppression with gonadotropin-releasing hormone analogues, in selected cases of GD in adolescence. Puberty suppression is, in fact, described to be beneficial for GD adolescents by giving a relief of their prolonged distress and by improving quality of life [3, 38, 44]. Furthermore, delaying treatment until adulthood or even late adolescence may have negative consequences on a psychological and physical level. Some GD adolescents may, in fact, develop psychiatric co-occurring problems such as anxiety or depression.
Regarding suicidal risk, we have here demonstrated, for the first time, that Italian adolescents with GD are significantly more vulnerable to suicide than NR ones using a specific assessment tool for suicide risk (the MAST, [28–31]). The previous studies, focusing on the pediatric population, have reported self-harm and suicidality as part of the clinical presentation of a considerable part of gender-referred children with GD aged 5–11 years [45]. In addition, a higher completed suicide rate has been reported in adults with GD, as compared to those without GD [11, 46, 47] Regarding adolescents, prevalence of self-harm and suicidal thoughts in clinical referred samples has been reported [48, 49] without comparison to a control group. Aitken [45] cited the unpublished data by Steensma et al. [12] on the prevalence of self-harm/suicidality in clinic-referred adolescents with GD from Canada and The Netherlands and compared the prevalence rates with the standardization data for referred and NR youth. Adolescents with GD of the Toronto sample had the highest rate of self-harm/suicidality, whereas the Dutch youth with GD had a rate closer to the referred youth. All three of these groups had higher rates than the non-referred youth. The explanation why adolescents with GD are more vulnerable to suicide risk yields different hypotheses, with social ostracism being considered one of the main factors [45]. Other reasons may rely on the condition of GD itself as causing high levels of distress and impairment or on its link with co-occurring behavioral and emotional problems [45].
Considering epidemiological data, the MtF:FtM sex ratio of the GD sample is 1:1.3. This value confirms the recent shift from a ratio favoring MtFs (prior to 2006) to a ratio favoring FtMs (2006–2013) [50]. The inversion of sex ratio recently reported may be related to the higher social stigma and difficulty in seeking professional help for transition experienced by natal boys compared to natal girls [50, 51].
Regarding psychological functioning, adolescents with GD showed significantly higher levels of “internalizing problems” according to the YSR scale, in particular in terms of depression and anxiety, as compared to the control group. These results in an Italian sample are in line with worldwide data [37, 38, 48, 49, 52, 53], reporting higher prevalence rates of co-occurring psychiatric problems in referred gender dysphoric adolescents, as compared with the general population. One explanation of the higher degree of behavioral and emotional problems among adolescents with GD is likely due to the level of tolerance or acceptance of gender-variant behaviors in different cultures [2], which confirms the central role of homo- and transphobic attitudes towads gender non-conforming behaviors [13–15]. Accordingly, a recent study showed that psychological distress and functional impairment in GD persons are more strongly predicted by experiences of social rejection and violence than by gender incongruence per se [54]. This hypothesis has been confirmed also by results from a series of cross-national, cross-clinic comparative studies [2] between the Toronto and Amsterdam clinics, where GD adolescents from the Canadian clinic showed significantly more co-occurring internalizing behavioral and emotional problems. This explanation could be applied also to our data, considering that the Italian context has been described as discriminating and with high levels of homo/transphobia [13–15, 55, 56]. When social functioning was analyzed, adolescents with GD had significantly higher rates in the “social problems” YSR subscale when compared to the control group. This data confirm results from other studies where social ostracism and peer victimization have been described to be risk factors for co-occurring general psychopathology in gender non-conforming youth [57, 58]. Furthermore, in a recent study [11], adolescents with GD resulted more vulnerable to bullying experiences, reporting significantly higher rates of gender/sexual forms of discrimination when compared to both clinical and non-clinical control groups. These findings have clinical implications suggesting the importance of reducing psychosocial vulnerability in gender non-conforming youth and improving knowledge and acceptance on gender non-conforming behaviors and feelings on cultural and social levels [2, 11].
Some limitations of this study have to be considered. First, regarding the sample characteristics, sample size is small and the possibility of type II errors should be considered. In addition, our sample is mainly made up of adolescents evaluated at a hospital-based clinic making it difficult to generalize results to patients who either seek private health care services or to adolescents who do not come to the professionals’ attention. However, GD is described as a rare condition and because of the difficulty in coming out for transgender adolescents due to social ostracism as previously described, subjects with gender issues still do not always seek help. From this perspective, the multicentric nature of the present study and the participation of gender clinics located in the northern, central, and southern part of the country is a considerable strength. Another limit is in the research method that relied on self-report measures by the adolescents without comparing these data with more information from other sources such as parents and/or teachers. Finally, validations studies for a MAST Italian version are missing.
In conclusion, the present study confirmed the importance of an accurate psychopathological assessment in adolescents with GD. Only a multidisciplinary approach integrating psychopathological and medical competences could challenge the profound distress in the early GD, associated with internalizing problems, body uneasiness, and high suicidal risk. This position is taken for granted in several western countries. However, there is an urgent need for this kind of approach in Italy, as the current Italian context has, in fact, been described as being poorly able to properly face the needs of transgender youth due to a lack of specialized services and to the high stigma associated with an atypical gender development or expression [3].
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5). DSM-5 tm, Washington DC
De Vries AL, Steensma TD, Cohen-Kettenis PT, VanderLaan DP, Zucker KJ (2015) Poor peer relations predict parent-and self-reported behavioral and emotional problems of adolescents with gender dysphoria: a cross-national, cross-clinic comparative analysis. Eur Child Adolesc Psychiatry 25(6):579–588
Fisher AD, Ristori J, Bandini E, Giordano S, Mosconi M, Jannini E, Greggio N, Godano A, Manieri C, Meriggiola C (2014) Medical treatment in gender dysphoric adolescents endorsed by SIAMS–SIE–SIEDP–ONIG. J Endocrinol Investig 37:675–687
Kaltiala-Heino R, Sumia M, Työläjärvi M, Lindberg N (2015) Two years of gender identity service for minors: overrepresentation of natal girls with severe problems in adolescent development. Child Adolesc Psychiatry Ment Health 9:1
Zucker KJ, Bradley SJ, Owen-Anderson A, Kibblewhite SJ, Wood H, Singh D, Choi K (2012) Demographics, behavior problems, and psychosexual characteristics of adolescents with gender identity disorder or transvestic fetishism. J Sex Marital Ther 38:151–189
Marshall E, Claes L, Bouman WP, Witcomb GL, Arcelus J (2016) Non-suicidal self-injury and suicidality in trans people: a systematic review of the literature. Int Rev Psychiatry 28:58–69
Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, Vance SR (2012) Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics 129(3):418–425
Grossman AH, D’Augelli AR (2007) Transgender youth and life-threatening behaviors. Suicide Life Threat Behav 37:527–537
Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB (2014) Monitoring the health of transgender and other gender minority populations: validity of natal sex and gender identity survey items in a US national cohort of young adults. BMC Public Health 14:1
Arcelus J, Claes L, Witcomb GL, Marshall E, Bouman WP (2016) Risk factors for non-suicidal self-injury among trans youth. J Sex Med 13:402–412
Shiffman M, VanderLaan DP, Wood H, Hughes SK, Owen-Anderson A, Lumley MM, Lollis SP, Zucker KJ (2016) Behavioral and emotional problems as a function of peer relationships in adolescents with gender dysphoria: a comparison with clinical and nonclinical controls. Psychology of Sexual Orientation and Gender Diversity © 2015. American Psychological Association, Washington, DC, pp 27–36
Steensma TD, Zucker KJ, Kreukels BP, VanderLaan DP, Wood H, Fuentes A, Cohen-Kettenis PT (2014) Behavioral and emotional problems on the Teacher’s Report Form: a cross-national, cross-clinic comparative analysis of gender dysphoric children and adolescents. J Abnorm Child Psychol 42:635–647
Ciocca G, Niolu C, Déttore D, Antonelli P, Conte S, Tuziak B, Limoncin E, Mollaioli D, Carosa E, Gravina G (2016) Cross-cultural and socio-demographic correlates of homophobic attitude among university students in three European countries. J Endocrinol Investig 1–7
Bandini E, Maggi M (2014) Transphobia. In: Corona G, Jannini E, Maggi M (eds) Emotional, physical and sexual abuse. Springer, New York, pp 49–59
Lingiardi V, Nardelli N (2014) Negative attitudes to lesbians and gay men: persecutors and victims. Springer, Corona
van de Grift TC, Cohen-Kettenis PT, Steensma TD, De Cuypere G, Richter-Appelt H, Haraldsen IR, Dikmans RE, Cerwenka SC, Kreukels BP (2016) Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav 45:575–585
van de Grift T, Cohen-Kettenis P, Elaut E, De Cuypere G, Richter-Appelt H, Haraldsen I, Kreukels B (2016) A network analysis of body satisfaction of people with gender dysphoria. Body Image 17:184–190
Jones BA, Haycraft E, Murjan S, Arcelus J (2016) Body dissatisfaction and disordered eating in trans people: a systematic review of the literature. Int Rev Psychiatry 28:81–94
Fisher AD, Castellini G, Bandini E, Casale H, Fanni E, Benni L, Ferruccio N, Meriggiola MC, Manieri C, Gualerzi A (2014) Cross-sex hormonal treatment and body uneasiness in individuals with gender dysphoria. J Sex Med 11:709–719
Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, Fanni E, Amato A, Bettini E, Mosconi M, Dèttore D, Ricca V, Maggi M (2016) Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-years follow-up data. J Clin Endocrinol Metab 101:4260–4269
Becker I, Nieder TO, Cerwenka S, Briken P, Kreukels BP, Cohen-Kettenis PT, Cuypere G, Haraldsen IRH, Richter-Appelt H (2016) Body image in young gender dysphoric adults: a European multi-center study. Arch Sex Behav 45:559–574
Bandini E, Fisher AD, Castellini G, Lo Sauro C, Lelli L, Meriggiola MC, Casale H, Benni L, Ferruccio N, Faravelli C (2013) Gender identity disorder and eating disorders: similarities and differences in terms of body uneasiness. J Sex Med 10:1012–1023
Ålgars M, Santtila P, Sandnabba NK (2010) Conflicted gender identity, body dissatisfaction, and disordered eating in adult men and women. Sex Roles 63:118–125
Ciocca G, Limoncin E, Cellerino A, Fisher AD, Gravina GL, Carosa E, Mollaioli D, Valenzano DR, Mennucci A, Bandini E (2014) Gender identity rather than sexual orientation impacts on facial preferences. J Sex Med 11:2500–2507
Cuzzolaro M, Vetrone G, Marano G, Battacchi M (1999) BUT, Body Uneasiness Test: a new attitudinal body image scale. Psichiatria dell’infanzia e dell’adolescenza 66:417–428
Cuzzolaro M, Vetrone G, Marano G, Garfinkel P (2006) The Body Uneasiness Test (BUT): development and validation of a new body image assessment scale. Eat Weight Disord 11:1–13
Marano G, Cuzzolaro M, Vetrone G, Garfinkel P, Temperilli F, Spera G, Dalle Grave R, Calugi S, Marchesini G, Group QS (2007) Validating the Body Uneasiness Test (BUT) in obese patients. eating and weight disorders-studies on anorexia. Bulim Obes 12:70–82
Orbach I, Milstein I, Har-Even D, Apter A, Tiano S, Elizur A (1991) A Multi-Attitude Suicide Tendency Scale for adolescents. J Consult Clin Psychol 3:398
Osman A, Barrios FX, Panak WF, Osman JR, Hoffman J, Hammer R (1994) Validation of the multi-attitude suicide tendency scale in adolescent samples. J Clin Psychol 50:847–855
Baiocco R, Ioverno S, Cerutti R, Santamaria F, Fontanesi L, Lingiardi V, Baumgartner E, Laghi F (2014) Suicidal ideation in Spanish and Italian lesbian and gay young adults: the role of internalized sexual stigma. Psicothema 26:490–496
Baiocco R, Ioverno S, Lonigro A, Baumgartner E, Laghi F (2015) Suicidal ideation among Italian and Spanish young adults: the role of sexual orientation. Arch Suicide Res 19:75–88
Achenbach TM (1991) Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles: Department of Psychiatry, University of Vermont
Frigerio A, Cattaneo C, Cataldo M, Schiatti A, Molteni M, Battaglia M (2004) Behavioral and emotional problems among Italian children and adolescents aged 4 to 18 years as reported by parents and teachers. Eur J Psychol Assess 20:124–133
Deogracias JJ, Johnson LL, Meyer-Bahlburg HF, Kessler SJ, Schober JM, Zucker KJ (2007) The gender identity/gender dysphoria questionnaire for adolescents and adults. J Sex Res 44:370–379
Prunas A, Mognetti M, Hartmann D, Bini M (2013) La valutazione della disforia di genere: la versione italiana del gender identity/gender dysphoria questionnaire. Rivista di Sessuologia Clinica.
Dèttore D, Ristori J, Antonelli P, Bandini E, Fisher A, Villani S, de Vries A, Steensma T, Cohen-Kettenis P (2015) Gender dysphoria in adolescents: the need for a shared assessment protocol and proposal of the AGIR protocol. J Psychopathol 21:152–158
De Vries AL, Doreleijers TA, Steensma TD, Cohen-Kettenis PT (2011) Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry 52:1195–1202
De Vries AL, Steensma TD, Doreleijers TA, Cohen-Kettenis PT (2011) Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med 8:2276–2283
Cohen-Kettenis PT, Delemarre-van de Waal HA, Gooren LJ (2008) The treatment of adolescent transsexuals: changing insights. J Sex Med 5:1892–1897
Kuiper B, Cohen-Kettenis P (1988) Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav 17:439–457
Vocks S, Stahn C, Loenser K, Legenbauer T (2009) Eating and body image disturbances in male-to-female and female-to-male transsexuals. Arch Sex Behav 38:364–377
Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, Gooren LJ, Meyer WJ III, Spack NP, Tangpricha V, Montori VM (2009) Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 94:3132–3154
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, Fraser L, Green J, Knudson G, Meyer WJ, Monstrey S, Adler RK, Brown GR, Devor AH, Ehrbar R, Ettner R, Eyler E, Garofalo R, Karasic DH, Lev AI, Mayer G, Meyer-Bahlburg H, Hall BP, Pfäfflin F, Rachlin K, Robinson B, Schechter LS, Tangpricha V, van Trotsenburg M, Vitale A, Winter S, Whittle S, Wylie KR, Zucker K (2011) Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend 13:165–232
Steensma TD, Kreukels BP, de Vries AL, Cohen-Kettenis PT (2013) Gender identity development in adolescence. Horm Behav 64:288–297
Aitken M, VanderLaan DP, Wasserman L, Stojanovski S, Zucker KJ (2016) Self-harm and suicidality in children referred for gender dysphoria. J Am Acad Child Adolesc Psychiatry 55:513–520
Asscheman H, Giltay EJ, Megens JA, van Trotsenburg MA, Gooren LJ (2011) A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 164:635–642
Dhejne C, Lichtenstein P, Boman M, Johansson AL, Långström N, Landén M (2011) Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One 6:e16885
Khatchadourian K, Amed S, Metzger DL (2014) Clinical management of youth with gender dysphoria in Vancouver. J Pediatr 164:906–911
Skagerberg E, Parkinson R, Carmichael P (2013) Self-harming thoughts and behaviors in a group of children and adolescents with gender dysphoria. Int J Transgend 14:86–92
Aitken M, Steensma TD, Blanchard R, VanderLaan DP, Wood H, Fuentes A, Spegg C, Wasserman L, Ames M, Fitzsimmons CL (2015) Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. J Sex Med 12:756–763
Fisher AD, Bandini E, Casale H, Ferruccio N, Meriggiola MC, Gualerzi A, Manieri C, Jannini E, Mannucci E, Monami M (2013) Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation. J Sex Med 10:408–419
Zucker KJ, Wood H, Singh D, Bradley SJ (2012) A developmental, biopsychosocial model for the treatment of children with gender identity disorder. J Homosex 59:369–397
Olson J, Forbes C, Belzer M (2011) Management of the transgender adolescent. Arch Pediatr Adolesc Med 165:171–176
Robles R, Fresán A, Vega-Ramírez H, Cruz-Islas J, Rodríguez-Pérez V, Domínguez-Martínez T, Reed GM (2016) Removing transgender identity from the classification of mental disorders: a Mexican field study for ICD-11. Lancet Psychiatry 3:850–859
Fisher AD, Castellini G, Ristori J, Casale H, Giovanardi G, Carone N, Fanni E, Mosconi M, Ciocca G, Jannini E, Ricca V, Lingiardi V, Maggi M (2016) Who has the worst attitudes toward sexual minorities? Comparison of transphobia and homophobia levels in gender dysphoric individuals, the general population and health care providers. J Endocrinol Investig 1–11.
Ciocca G, Tuziak B, Limoncin E, Mollaioli D, Capuano N, Martini A, Carosa E, Fisher AD, Maggi M, Niolu C (2015) Psychoticism, immature defense mechanisms and a fearful attachment style are associated with a higher homophobic attitude. J Sex Med 12:1953–1960
Baams L, Beek T, Hille H, Zevenbergen FC, Bos HM (2013) Gender nonconformity, perceived stigmatization, and psychological well-being in Dutch sexual minority youth and young adults: a mediation analysis. Arch Sex Behav 42:765–773
Wallien MS, Veenstra R, Kreukels BP, Cohen-Kettenis PT (2010) Peer group status of gender dysphoric children: a sociometric study. Arch Sex Behav 39:553–560
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the institution’s Ethics Committee.
Informed consent
All patients have provided their written informed consent to participate to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fisher, A.D., Ristori, J., Castellini, G. et al. Psychological characteristics of Italian gender dysphoric adolescents: a case–control study. J Endocrinol Invest 40, 953–965 (2017). https://doi.org/10.1007/s40618-017-0647-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0647-5