Abstract
Purpose
To investigate the effect of 18 months’ parathyroid hormone 1–84 (PTH 1–84) treatment on serum levels of bone morphogenetic protein 4 (BMP4) and vascular endothelial growth factor (VEGF), in postmenopausal women with established osteoporosis.
Methods
Thirty-seven postmenopausal women with osteoporosis (mean age 72.9 ± 8.1 years old) and 23 healthy controls (mean age 68.9 ± 9.9 years old) were enrolled. Patients were treated with daily subcutaneous injections of PTH (1–84) 100 mcg for 18 months, plus calcium 1 gr and vitamin D 800 IU per os daily. Blood samples were taken every 6 months during the study.
Results
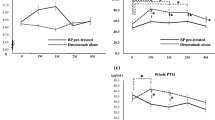
At baseline, there were no differences considering anthropometric parameters, co-morbidities, current medications used between patients and controls. Mean serum VEGF levels were significantly higher in osteoporotic patients compared to controls (436.7 ± 259.7 vs. 260.3 ± 184.3 pg/ml, p = 0.006), while there were no differences in mean serum values of BMP4 (5.3 ± 1.7 vs. 5.7 ± 1.6 pg/ml, p = 0.40). Serum VEGF levels increased by approximately 20% after 12 months of PTH (1–84) treatment compared to baseline (p = 0.03) and by 22% after 18 months (p = 0.01). A significant increase of 10% in mean serum BMP4 levels was observed after 18 months of PTH (1–84) treatment compared to baseline (p = 0.02). In the control group we found no differences after 18 months compared to baseline in BMP4 (5.7 ± 1.6 vs. 6.0 ± 1.5 pg/ml, p = 0.53) and VEGF (260.3 ± 184.3 vs. 257.4 ± 107.1 pg/ml, p = 0.94).
Conclusions
PTH (1–84) treatment increased serum levels of VEGF and BMP4 in postmenopausal women with severe osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anabolic therapy with human recombinant intact parathyroid hormone 1–84 (PTH 1–84) has been shown to reduce fracture risk in osteoporotic patients [1–3]. Furthermore, some experimental data seem to demonstrate that PTH 1–84 promote fracture healing due to increased osteoblast recruitment and survival [4].
A number of studies, mainly in rodents or in vitro, have elucidated the molecular aspects of the anabolic action of PTH on bone; however, there are difficulties in unequivocally defining these mechanisms in humans, mainly because they probably involve multiple cell types and pathways. Indeed, accumulated evidence indicates that the anabolic action of PTH results from an orchestration of the effects of local factors such as bone morphogenetic proteins (BMPs); these are members of the TGF-beta superfamily that possess a number of physiologic activities including the maintenance and stimulation of osteoblast differentiation [5].
Several studies have attempted to determine the osteogenic potential of individual BMPs in comparison to one another. Suzawa et al. identified the significance of the regulatory action of BMP2 and BMP4 (which have 80% amino acid sequence homology of molecules) on osteoblastic cells, as one of the principal pathways in the pathogenesis of bone-losing diseases such as osteoporosis [6]. A recent paper demonstrated that estrogen facilitates osteoblast differentiation by upregulating BMP4, in vitro, rendering this BMP a potential culprit in the development of postmenopausal osteoporosis [7].
There is evidence of synergism between BMP2/BMP4 and vascular endothelial growth factor (VEGF), a potent angiogenic factor, predominantly in the early phases of bone healing [8]. Functional VEGF receptors have been identified on primary osteoblasts, allowing VEGF to promote bone remodeling acting directly on survival and activity of osteoblasts [9]. Moreover, the strong association reported between vasodilatation and bone volume suggests that bone arteriolar function is critical for PTH-induced bone anabolism [10].
Data on serum VEGF levels in osteoporotic patients are conflicting. Indeed, some studies show differences in mean VEGF serum levels between osteoporotic and normal subjects [11], while others do not [12, 13].
Only one study analyzed serum levels of BMP4 in patients with osteoporosis, showing no difference with the control group [14]. In addition, the effect of PTH (1–84) treatment of osteoporotic postmenopausal women on serum BMP4 and VEGF circulating levels is unknown. The aim of this study was therefore to investigate the influence of PTH (1–84) treatment on BMP4 and VEGF serum circulating levels in postmenopausal osteoporotic women.
Subjects and methods
The study population included 37 women with postmenopausal osteoporosis, recruited between January 2011 and January 2012 at different Hospitals in Italy. In the same period of time, 23 healthy volunteer postmenopausal women of the same age were enrolled as controls at our Mineral Metabolism Center. Patients were enrolled if they had a new moderate vertebral fracture, according to Genant method [15], and/or a hip fracture occurring while on antiresorptive therapy with oral bisphosphonates taken for at least one year. At that time in Italy, these criteria allowed the reimbursability of anabolic therapy with PTH (1–84), while currently only PTH (1–34) is available. Control subjects had normal or osteopenic T-score values at femoral neck and lumbar spine. The exclusion criteria for both groups included: estimated creatinine clearance <60 ml/min, neoplasia, HCV and/or HBV co-infection and previous diagnosis of secondary osteoporosis, diabetes mellitus, metabolic syndrome.
Patients and controls were already on daily oral calcium (1000 mg/day) and vitamin D (800I U/day) since at least three months before enrollment. Osteoporotic patients (n = 37) were treated with PTH (1–84) 100 µg subcutaneously (sc) every day, for 18 months. Blood samples were collected at baseline and every 6 months for 18 months. Calcium, creatinine and uric acid were assessed, as previously described [16, 17]. Serum samples were stored at −80 °C until assayed for BPM4 (BMP4 ELISA R&D Systems, Minneapolis, MN) and VEGF (Quantikine® ELISA kits, R&D Systems, Minneapolis, MN, USA). The inter and intra assay coefficients of variation for BPM4 were 4.4 and 5.3%, respectively, whereas the coefficients of variation for VEGF were 4.5 and 7.0%, respectively.
Each patient and control subject underwent standardized lateral radiographs of the thoracic and lumbar spine, centered at T8 and L3, respectively, at a film focus distance of 105 cm. After visual inspection of these radiographs by two independent experienced observers, vertebral deformity was defined when anterior, middle or posterior height loss was more than 20% with respect to the adjacent vertebra, according to Genant’s method. Every patient provided written informed consent. The study was approved by our local hospital Ethics Committee (PROT. 929/10).
Statistical analysis
Results are presented as mean values ±1 standard deviation (SD). Frequencies were compared using the chi-squared test. Between-group differences at baseline were assessed by Student’s t-test. The differences between groups in their change from baseline were assessed with Wilcoxon test. Pearson correlation coefficient was used to assess the relationship between continuous variables. The results were considered significant when the significance value of the test was less than 0.05% (р value < 0.05). The statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS) software (release 10, SPSS Inc., Chicago, IL, USA).
Results
There was no significant difference considering anthropometric parameters, co-morbidities and current medications between patients and controls (Table 1). As expected by inclusion criteria, 91% patients had vertebral fractures, 16% had hip fractures and 8% had a history of wrist fractures (Table 1).
At baseline mean serum VEGF levels were significantly higher in osteoporotic patients compared to controls (436.7 ± 259.7 vs. 260.3 ± 184.3 pg/ml, p = 0.006), while there were no differences in mean serum values of BMP 4 (5.3 ± 1.7 vs. 5.7 ± 1.6 pg/ml, p = 0.40) (Table 1). We found no association in the osteoporotic group between both serum levels of BMP4 and VEGF with age, BMI, creatinine, except for a positive association between VEGF and serum creatinine (β = 0.34, p = 0.04).
There was no correlation between serum levels of VEGF and BMP4 at baseline and after 18 months of treatment in the patients group. Serum VEGF levels increased approximately by 20% after 12 months of PTH (1–84) treatment compared to baseline (p = 0.03) and by 22% after 18 months (p = 0.01). A significant increase of 10% in serum BMP 4 levels was observed after 18 months of PTH (1–84) treatment compared to baseline (p = 0.02) (Fig. 1). In the control group we found no differences between BMP4 at baseline and after 18 months (5.7 ± 1.6 vs. 6.0 ± 1.5 pg/ml, p = 0.53), nor for VEGF (260.3 ± 184.3 vs. 257.4 ± 107.1 pg/ml, p = 0.94). After 18 months, there was no differences in BMP4 values between patients and controls (5.81 ± 2.16 vs. 6.0 ± 1.5, p = 0.71), while VEGF was higher in patients than in controls (500.4 ± 285.8 vs. 257.4 ± 107.1 pg/ml, p = 0.0003).
Neither new clinical fractures were not reported in the study period, nor serious side effects.
In the patients group, we observed an increase of mean serum calcium levels without hypercalcemia at 18 months (calcium at baseline vs calcium at 18 months: 9.6 ± 0.7 vs. 9.8 ± 0.6 mg/dl, p = 0.01). In addition, a tendency to an increase of serum uric acid was observed (4.6 ± 1.2 vs. 5.6 ± 1.6 mg/dl, p = 0.001). We found no statistically significant difference in urinary calcium and creatinine levels at baseline compared to 18 months (creatinine 0.8 ± 0.2 vs 0.8 ± 0.2 mg/dl; p = 1.0, and urinary calcium 24 h 181.9 ± 108.0 vs. 160.7 ± 109.3 mg/24 h; p = 0.18).
Discussion
Our study shows for the first time that treatment with PTH (1–84) induces a significant increase in mean serum VEGF and BMP4 levels in postmenopausal patients with established osteoporosis.
We found that in basal conditions osteoporotic patient had higher serum levels of VEGF compared to control group, as found by Costa et al., even if in the last study the difference was not significant [13]. It could be argued that our population sustained a recent osteoporotic fracture so that the healing process involving VEGF was already started when the therapy was administered; however, since most of the vertebral fractures were morphometric, the exact time of vertebral fracture could not be ascertained in each patient. The patients group was treated with bisphosphonates, before enrollment for anabolic therapy, which could be also a factor that has modified VEGF levels compared to controls.
Interestingly, we found an increase in VEGF after therapy; this new finding may lead to a further understanding of the biochemical mechanism involved in the anabolic effects of PTH. There are only two studies in the literature regarding the interaction between PTH and VEGF in humans. The first one looked at the serum levels of VEGF in primary hyperparathyroidism, a disease characterized by elevated levels of PTH; higher VEGF levels compared to control subjects were reported [18]. The second study analyzed the effect of PTH (1–84) on serum VEGF levels in hypoparathyroidism patients, characterized by low levels of PTH, showing that serum VEGF levels were altered [19]. In this second study, the increase of VEGF levels in the eight subjects treated was at least 10% at 6 or 12 months, based on the raw values; the authors hypothesize that PTH (1–84) administration in these subjects influenced residual parathyroid cell function by stimulating VEGF [19]. It should be noted that the dose of PTH (1–84) utilized for the treatment of hypoparathyroidism is different from that utilized for the treatment of osteoporosis. In fact, 50 µg daily to 100 µg every 3 days was used in case of hypoparathyroid subjects, while for osteoporotic patients, the standard treatment is represented by 100 µg daily of PTH (1–84). This may explain the different response magnitude of VEGF to PTH therapy in postmenopausal osteoporotic women. Indeed, we observed an increase of 20% after 12 months, while in hypoparathyroidism an increase of 10% was reported [19]. It is interesting to note that other therapies currently prescribed for osteoporosis, such as both continuous combined hormone therapy and tibolone therapy, have been shown to increase plasma VEGF, in a cohort of postmenopausal women [20].
Moreover, our study showed an increase in serum BMP4 values after 18 months of treatment. Studies in mice demonstrated that osteoblast receptors, which transduce canonical BMP ligands BMP2 and BMP4, negatively regulate endogenous bone mass and WNT/B catenin signaling [21]. This regulation is possibly mediated by sclerostin and Dickkopf-1(DKK1), which are specific WNT antagonists expressed by osteoblasts and osteocytes [21]. Thus, it is possible that also in humans BMP4 interacts with sclerostin and DKK1, molecules that have been shown to be involved in the anabolic effect of PTH. In postmenopausal women treated with PTH (1–34), an increase of DKK1 has been demonstrated after 18 months of this treatment. The authors of this study suggest that the increase of DKK1 is associated with the decline in the anabolic action of PTH(1–34) at the end of treatment as indicated by the decrease in the markers of bone formation in their cohort [22]. A decrease in sclerostin levels after PTH (1–34) treatments has been described, in short term studies, as another possible mechanism to explicate PTH anabolism [23, 24]. Unfortunately, we did not perform the measurements of BMP4 before six months of treatment, to assess this possible interaction. Another possible explanation involves cortisol level changes during anabolic therapy. Indeed, it was reported that cortisol level may increase under PTH 1–34 treatment [25]. Glucocorticoids may modulate both BMPs and VEGF in vitro and in animal models [26, 27], thus a possible contribution of cortisol changes during therapy that influences both molecules could be speculated also in humans.
Our study suffers some limitations. We included patients with recent fractures; thus an early fracture repair is expected, which may have influenced VEGF levels. We did not measure DKK1, sclerostin, cortisol and bone turnover markers which could have provided some additional information. We also did not assess vitamin D levels, which could have influenced VEGF and BMP4 levels, however the supplementation of vitamin D, administered starting since 3 months before enrollment, most probably likely assured normal vitamin D level in all subjects.
In conclusion, our study showed a significant increase of serum VEGF and BMP4 levels in osteoporotic postmenopausal women treated with PTH (1–84), suggesting a possible involvement of these molecules in the anabolic effect of PTH.
References
Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, Blosch CM, Mathisen AL, Morris SA, Marriott TB, Treatment of Osteoporosis with Parathyroid Hormone Study Group (2007) Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med 146:326–339
Adler RA (2016) Osteoporosis treatment: complexities and challenges. J Endocrinol Invest 39(7):719–720
Lewiecki EM, Binkley N (2016) What we don’t know about osteoporosis. J Endocrinol Invest 39:491–493
Jilka RL (2007) Molecular and cellular mechanisms of the anabolic effect of intermittent PTH. Bone 40:1434–1446
Biver E, Hardouin P, Caverzasio J (2013) The “bone morphogenic proteins” pathways in bone and joint diseases: translational perspectives from physiopathology to therapeutic targets. Cytokine Growth Factor Rev 24:69–78
Suzawa M, Takeuchi Y, Fukumoto S, Kato S, Ueno N, Miyazono K, Matsumoto T, Fujita T (1999) Extracellular matrix-associated bone morphogenetic proteins are essential for differentiation of murine osteoblastic cells in vitro. Endocrinology 140:2125–2133
Matsumoto Y, Otsuka F, Takano-Narazaki M, Katsuyama T, Nakamura E, Tsukamoto N, Inagaki K, Sada KE, Makino H (2013) Estrogen facilitates osteoblast differentiation by upregulating bone morphogenetic protein-4 signaling. Steroids 78:513–520
Peng H, Wright V, Usas A, Gearhart B, Shen HC, Cummins J, Huard J (2002) Synergistic enhancement of bone formation and healing by stem cell-expressed VEGF and bone morphogenetic protein-4. J Clin Invest 110:751–759
Street J, Lenehan B (2009) Vascular endothelial growth factor regulates osteoblast survival evidence for an autocrine feedback mechanism. J Orthop Surg Res 16:4–19
Prisby R, Menezes T, Campbell J (2013) Vasodilation to PTH (1–84) in bone arteries is dependent upon the vascular endothelium and is mediated partially via VEGF signaling. Bone 54:68–75
Senel K, Baykal T, Seferoglu B, Altas EU, Baygutalp F, Ugur M, Kiziltunc A (2013) Circulating vascular endothelial growth factor concentrations in patients with postmenopausal osteoporosis. Arch Med Sci 9:709–712
Cebi H, Aksahin E, Yuksel HY, Celebi L, Aktekin CN, Ha Pa O (2010) Plasma vascular endothelial growth factor levels are similar in subjects with and without osteoporosis. Eklem Hastalik Cerrahisi 21:91–97
Costa N, Paramanathan S, Mac Donald D, Wierzbicki AS, Hampson C (2009) Factors regulating circulating vascular endothelial growth factor (VEGF): association with bone mineral density (BMD) in post-menopausal osteoporosis. Cytokine 46:376–381
Dincel VE, Sepici-Dincel A (2014) The importance and the differences of bone morphogenetic proteins for osteoporotic hip fractures. Acta Orthop Belg 80:216–221
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. JBMR 9:1137–1148.
Russo S, Carlucci L, Cipriani C, Ragno A, Piemonte S, Fiacco Rd, Pepe J, Fassino V, Arima S, Romagnoli E, Minisola S (2011) Metabolic changes following 500 μg monthly administration of calcidiol: a study in normal females. Calcif Tissue Int 89:252–257
Paglia F, Dionisi S, De Geronimo S, Rosso R, Romagnoli E, Raejntroph N, Ragno A, Celi M, Pepe J, D’Erasmo E, Minisola S (2001) Biomarkers of bone turnover after a short period of steroid therapy in elderly men. Clin Chem 47:1314–1316
Brunner S, Theiss HD, Murr A, Negele T, Franz WM (2007) Primary hyperparathyroidism is associated with increased circulating bonemarrow-derived progenitor cells. Am J Physiol Endocrinol Metab 293:E1670–E1675
Cusano NE, Rubin MR, Zhang C, Anderson L, Levy E, Costa AG, Irani D, Bilezikian JP (2014) Parathyroid hormone 1–84 alters circulating vascular endothelial growth factor levels in hypoparathyroidism. J Clin Endocrinol Metab 99:E2025–E2028
Christodoulakos G, Lambrinoudaki I, Panoulis C, Papadias C, Sarandakou A, Liakakos T, Alexandrou A, Creatsas G (2004) Effect of hormone therapy, tibolone and raloxifene on circulating vascular endothelial growth factor in Greek postmenopausal women. Eur J Endocrinol 151:187–192
Kamiya N, Kobayashi T, Mochida Y, Yu PB, Yamauchi M, Kronenberg HM, Mishina YJ (2010) Wnt inhibitors Dkk1 and Sost are downstream targets of BMP signaling through the type IA receptor (BMPRIA) in osteoblasts. JBMR 25:200–210.
Gatti D, Viapiana O, Idolazzi L, Fracassi E, Rossini M, Adami S (2011) The waning of teriparatide effect on bone formation markers in postmenopausal osteoporosis is associated with increasing serum levels of DKK1. J Clin Endocrinol Metab 96:1555–1559
Piemonte S, Romagnoli E, Bratengeier C, Woloszczuk W, Tancredi A, Pepe J, Cipriani C, Minisola S (2012) Serum sclerostin levels decline in postmenopausal women with osteoporosis following treatment with intermittent PTH. J Endocrinol Invest 35:866–868
Drake MT, Srinivasan B, Mödder UI, Peterson JM, McCready LK, Riggs BL, Dwyer D, Stolina M, Kostenuik P, Khosla S (2010) Effects of parathyroid hormone treatment on circulating sclerostin levels in postmenopausal women. J Clin Endocrinol Metab 95:5056–5062
Lasco A, Catalano A, Morabito N, Gaudio A, Basile G, Trifiletti A, Atteritano M (2011) Adrenal effects of teriparatide in the treatment of severe postmenopausal osteoporosis. Osteoporos Int 22:299–303
Luppen CA, Chandler RL, Noh T, Mortlock DP, Frenkel B (2008) BMP-2 versus BMP-4 expression and activity in glucocorticoid-arrested MC3T3-E1 osteoblasts: Smad signaling, not alkaline phosphatase activity, predicts rescue of mineralization. Growth Factors 26:226–237
Pufe T, Scholz-Ahrens KE, Franke AT, Petersen W, Mentlein R, Varoga D, Tillmann B, Schrezenmeir J, Glüer CC (2003) The role of vascular endothelial growth factor in glucocorticoid-induced bone loss: evaluation in a minipig model. Bone 33:869–876
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pepe, J., Cipriani, C., Cantatore, F.P. et al. The effect of parathyroid hormone (1–84) treatment on serum bone morphogenetic protein 4 and vascular endothelial growth factor in postmenopausal women with established osteoporosis. J Endocrinol Invest 40, 663–667 (2017). https://doi.org/10.1007/s40618-017-0636-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0636-8