Abstract
Introduction
Graves’ disease (GD) is an autoimmune disorder responsible for 60–90% of thyrotoxicosis, with an incidence of 1 to 2 cases per 1000 population per year in England. Graves’ orbitopathy (GO) is the most frequent extrathyroidal manifestation, not provoked directly by abnormal thyroid hormone levels, but by the consequence of the underlying autoimmune process. The aetiology of autoimmune disorders is due to an interplay between susceptibility genes and environmental factors, such as infections and stress. What triggers the autoimmune reaction to a specific site of the body is not yet clearly understood. The lack of knowledge in GD and GO pathogenesis implicates therapies that only limit damage but do not prevent disease onset.
Material and methods
We performed on PubMed and the Cochrane Library a literature search for the articles published until July 2016 by using the search terms ‘graves disease’ and ‘microbiome’, ‘orbitopathy’ and ‘autoimmune pathogenesis’. Reference lists of relevant studies were hand-searched for additional studies.
Conclusion
In this scenario, a Marie Sklodowska–Curie funded project INDIGO (http://www.indigo-iapp.eu/) is investigating the role of the gut bacteria in GD and GO pathogenesis. The gut is the first and the widest area of bacteria access, with the highest concentration of T cells in the human body and trained to react to microorganisms. Interestingly, all the environmental factors involved in GD and GO pathogenesis can alter the balance within the microorganisms located in the gut, and influence the immune system, in particular the proportions of regulatory Treg and inflammatory TH17 cells. It is hoped that investigating GD and GO pathogenesis from this novel aspect will identify new targets for prevention and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Graves’s disease (GD) is one of the most common organ-specific autoimmune disorders. Characterized by thyrotoxicosis, diffuse goiter and the presence of thyroid-stimulating antibodies (TSAB), GD represents 60–90% of all causes of thyrotoxicosis, in areas where populations are exposed to adequate iodine intake. It typically affects people between 30 and 60 years old, with an incidence of 1–2 cases per 1000 population per year in England and roughly eight times greater in women than in men [1].
Graves’ orbitopathy (GO) is the most frequent extrathyroidal manifestation [2]. The inflammation of intraorbital tissues, increased adipogenesis and accumulation of glycosaminoglycans within the extraocular muscles induce expansion and remodeling of the orbital contents. A recent study shows that the orbital fat volume is associated with the duration, while the eye muscle volume is related to the severity of the disease [3]. As reported in some recent epidemiological studies, 20.1% of GD patients present at least one of the typical manifestations of GO (e.g., periorbital edema, eyelid retraction, proptosis, conjunctival redness and strabismus) [4]. Fortunately, the incidence of moderate-to-severe form is approximately 5% and only 2% of GO patients develop the sight-threatening ocular disease due to dysthyroid optic neuropathy (DON) [5]. The age-adjusted annual incidence of clinically relevant GO is 16 per 100,000 population in women and 2.9 in men [6]. Even though spontaneous improvement or stabilization may occur in mild GO, many patients need treatment that impact on quality of life.
As in all autoimmune diseases, when self-tolerance is broken, T cells recognize self-antigens and B cells produce antibodies targeting host cells; this amplifies when they recruit and activate other immune cells. Concerning GO, it is widely accepted that the underlying autoimmune process and not abnormal thyroid hormone levels, is responsible [7].
The etiology of autoimmune disorders is due to interplay between susceptibility genes and environmental factors, such as infections, stress, drugs and radiation [8]. What triggers the autoimmune reaction against the thyroid instead of other sites of the body is not yet clearly understood, but single-nucleotide polymorphisms in the TSH receptor (TSH-R) (please see below) might be implicated. The lack of knowledge in GD and GO pathogenesis means that available therapies treat signs and symptoms, without changing the natural course of the disease or preventing disease onset.
We will review what is known about GD and GO pathogenesis and then focus on a possible link between thyroid, eyes and gut.
What is the target of the autoimmunity?
Patients with GD have cell-mediated immune reactivity and antibodies against the TSH-R (TRAb) [9] whose central importance is supported by the development of animal models [10, 11]. Most GD patients also have thyroid peroxidase (TPO) and less frequently thyroglobulin antibodies, while up to 25% of active GD show low-level titers of antibodies to DNA and to liver mitochondria.
Moreover, thyreopathies are not uncommon in subjects affected by other “organ-specific” autoimmune diseases including chronic gastritis, ACTH deficiency, Addison’s disease, chronic hepatitis, celiac disease, diabetes mellitus type 1, myasthenia gravis, premature ovarian failure, primary biliary cirrhosis, vitiligo or “systemic autoimmune diseases” as rheumatoid arthritis, multiple sclerosis, systemic lupus erythematosus, systemic sclerosis, urticaria and angioedema [12]. Thus, GD can be part of a complex autoimmune reaction against thyroid tissue, due to a generalized dysregulation of the immune system. Finally, several autoimmune endocrinopathies can cluster in polyglandular autoimmune syndromes (PAS). The first classification of polyglandular failure divided two broad categories: PAS type I and PAS type II. PAS I also known as APECED is characterized by mucocutaneous candidiasis, autoimmune hypoparathyroidism and adrenal insufficiency; the more common type II, also known as Schmidt syndrome, comprises the obligatory occurrence of autoimmune Addison disease in combination with thyroid autoimmune diseases and/or type 1 diabetes mellitus. An additional group, PAS type III (PAS III), was subsequently described and is the co-occurrence of autoimmune thyroid disease with two other autoimmune disorders, including diabetes mellitus type 1, pernicious anemia or a non-endocrine, organ-specific autoimmune disorder in the absence of Addison disease.
Autoimmune thyroid disorders (AITD) are the main manifestation of PGA II and III. In particular, the most frequent disease combinations in PGA II are type 1 diabetes and AITD (41%) followed by AITD and Addison’s disease.
The close temporal relationship between the onset of GD and GO suggests that these two conditions might share the same etiology. Autoreactive T lymphocytes directed against one or more antigens shared by the thyroid and orbit are assumed to infiltrate the orbital tissue and the perimysium of extraocular muscles; however, the putative autoantigens and the exact link between thyroid and orbit are still unclear.
The TSH-R was the first structure considered as a candidate autoantigen. TSH-R transcripts have been reported in adipose retro-orbital tissues of healthy people and GD patients using polymerase chain reaction, northern blot and liquid hybridization [13]. It is generally accepted that TSH-R expression increases during adipogenesis in any fat depot (ref). Zhang et al. [14] investigated the biological effects of TSH-R activation in cultures of orbital adipose tissues and showed that it stimulates early preadipocyte differentiation and favors formation of brown adipose tissue; in contrast, it seems to render preadipocytes refractory to PPAR-γ-induced adipogenesis. Kumar et al. [15] demonstrated that a human monoclonal TSAB enhances adipogenesis by signaling via PI3K. The immune response to TSH-R is also involved in the production of cytokines in orbital tissue. Both Th1 (e.g., IFN-γ, TNF-α, IL-1-β, and IL-6) and Th2 cytokines (e.g., IL-4 and IL-10) may play a role, although the former are found primarily in eye muscles and the latter in orbital fat. Even serum cytokine levels are elevated in GO patients compared to controls [16].
The role of TSH-R is also supported by the correlation between GO activity and TRAb levels and the fact that GD patients who relapse retain high TRAb levels and are the most likely to develop GO [17]. However, the TSH-R is expressed in several other tissues not involved in GD and GO (such as ovary, testis, kidney, skin, bone marrow, white and brown adipose tissue, bone), and, at lower levels, in normal orbital fibro-adipose tissue samples and cultures. Finally, Banga’s group have developed a murine GO model, using immunization with human TSH A subunit by in vivo electroporation and this has been reproduced in another laboratory [18, 19].
The presence of increased insulin-like growth factor 1 receptor (IGF-1R) levels in orbital fibroblast, B and T lymphocytes from GO patients prompts a possible role of IGF-1R in the pathogenesis. Moreover, the colocalization of TSH-R and IGF-1R on fibroblasts and thyrocytes shown by some researchers suggests a possible functional link between them [20]. Interestingly, only a minority of GO patients have circulating antibodies to the IGF-1R. This could be related to the low sensitivity and specificity of detection tests used or it may suggest a relevant role only for antibodies locally produced in the orbit [21] or, again, the cross talk between the TSH-R and IGF-1R may be important, rather than direct activation of the surface IGF-1R [22]. Other autoantigens, including several eye muscle antigens, acetylcholinesterase, thyroperoxidase, thyroglobulin, alpha fodrin, have been proposed, but their true role is uncertain.
Genetic predisposition
The relatively high incidence of GD and GO in families and among siblings (sibling risk ratio 11.6) [23] indicates a strong genetic influence. Studies on twins suggest that genetics accounts for 79% of the liability to developing the disease, and environmental factors for the remaining 21% [24].
Predisposition to autoimmunity in general results from variation (polymorphisms) in genes implicated in the acquisition of central and peripheral tolerance by regulatory T cells (Treg) and also the costimulation of T cells and APCs in the immunological synapse [25].
A prime example is mutation in the autoimmune regulator (AIRE) gene, expressed in thymic medullary epithelial cells, which induce loss of self-tolerance and lead to autoimmune polyglandular syndrome type 1. However, AIRE mutations are rarely present in AITD patients (in about 0.3–0.6% of autoimmune hyperthyroidism) and are not implicated in the more common autoimmune endocrinopathies [26].
There are several studies characterizing Tregs in autoimmune thyroid disease (AITD). Nakano et al. [27] showed decreased proportion and apoptotic Tregs in thyroid tissue of GD patients; Marazuela et al. [28] and Glick et al. [29], on the other hand, found increased T infiltration in thyroid tissue, but impaired T cell function. Thus, whether the number or the function of Tregs is altered in GD remains uncertain.
T cells react against epitopes complexed in human leukocyte antigen (HLA) proteins on antigen-presenting cells (APC). HLA antigen D-related (HLA-DR) molecules are the most important as their amino acids sequences determine the shape of the antigen-presenting cleft. However, the relationship between DR gene inheritance and GD accounts for about a twofold–fivefold increment in risk, which is certainly not enough to explain the marked increase in risk seen in many families.
Moreover, the genetic effects of DR genes interact with that of cytotoxic T lymphocyte antigen (CTLA-4) which is expressed by T cells and is the receptor for an adhesion molecule expressed on APC. Specifically, the positive effect of CTLA-4 mitigates in part the negative effect of DRB1*0701, but does not interact with the positive influence of DRB1*0301 [30].
Some studies investigated the role of regulators of the immune response. Ban et al. [31] focused their attention on protein tyrosine phosphatase non-receptor type 22 (PTPN22) gene that encodes for a powerful inhibitor of T cell activation. A single-nucleotide polymorphism was shown to inhibit function of the gene and to be associated with GD and other autoimmune diseases. Since knockout mice deficient in this gene do not develop autoimmunity, the role of PTPN22 gene in the etiology of AITD is unclear.
Vitamin D and its receptor are involved in control of immunity and CYP27B1 catalyzes the conversion of 25-OH-D to the active form 1.25-OH-D. An association between polymorphisms in these genes and GD is not surprising even if the mechanism is not clear [32].
Results relating to a specific polymorphism of the TSH receptor (PRO52THR) are contradictory [33, 34], but alleles in intron 7 of this gene were found to be associated with GD not only in the Japanese population but also in Caucasian [35, 36]. Moreover, two single-nucleotide polymorphisms (rs179247 and rs12101255) within TSH-R intron 1 exhibited strong association with GD in three independent European cohorts [37].
Attempts have been made to distinguish from the pool of all patients with GD those who are most likely to develop GO. Studies have focused on immunomodulatory genes including HLA-DR3, CTLA-4, IL-1, IL-23 receptor (IL-23R), CD40, PTPN22, T cell receptor b chain (TCR-b), tumor necrosis factor-b (TNF-b) and various immunoglobulin heavy chain-associated genes. Since both TSH-R expression and adipogenesis are enhanced in the orbit of GO patients, the adipogenesis-related gene peroxisome proliferator-associated receptor-γ (PPAR-γ) and the TSH-R gene have been investigated, as have genes encoding thyroglobulin and the glucocorticoid receptor.
The only polymorphisms associated with GO, rather than GD are in IL-23R (rs10889677 and rs2201841; OR 1.8,), IL-1 alpha 889C/T polymorphism (OR of 5.7 for TT genotype) and IL-1 receptor antagonist (IL-1RA) with Mspa-1 11100C/T polymorphism (OR of 6.7 for CC genotype) [38, 39].
Genetic factors have been identified in differing GO disease states; e.g., CTLA-4A/G polymorphism at codon 17 and G allele in polymorphic sites Jo31 (rsl1571302) and CT60 of CTLA-4 gene were more common in severe GO but Pro(12)Ala PPAR-γ polymorphism in milder and less active ocular disease [40, 41].
Finally, no significant association of glucocorticoid receptor polymorphisms ER22/23EK, N363S and Bcl1 with either the therapeutic response to glucocorticoids treatment or the occurrence of side effects was observed [42].
Humoral factors
Further evidence of ongoing autoimmunity in hyperthyroid patients is the increase in adhesion molecules as ICAM-1, which could facilitate the recruitment of T cells to the orbit [43], and in proinflammatory cytokines [interleukin (IL)-17, IL-22, IL-6 and IL-8], chemokines (IFN-γ, TNF-α, CXCL10, IL23, BAFF, etc.) and their receptors suggesting a possible target for new therapies [44, 45].
Analysis of T-cell clones from GO orbital tissues has shown both Th1 cytokine (interleukin-2, interferon gamma, tumor necrosis factor alpha) and Th2 cytokine (interleukin-4, interleukin-5, interleukin-10) secretory profiles, possibly related to different stages of the disease, with Th1 cytokines predominating early and Th2 cytokines late in the course of GO. Cytokines produced by T cells, macrophages and fibroblasts perpetuate the ongoing inflammatory process through induction of expression of HLA class II antigens, heat-shock proteins, CD40, prostaglandins, adhesion molecules, proliferation of fibroblasts, differentiation of preadipocyte fibroblasts into adipocytes and stimulation of fibroblasts to synthesize and secrete glycosaminoglycans [46, 47].
Understanding that each stage of the natural course of GO has a different inflammatory pattern is essential to select the ideal treatment for each patient. Thus, e.g., corticosteroids are effective in the initial active phase but not in burnout GO when they may elicit harm. Also more innovative drugs, whose use in GO is still matter of research, could have an efficacy influenced by time of administration. For example, contradictory results were obtained in two randomized clinical trials employing rituximab, a chimeric mouse–human monoclonal antibody that targets CD20. The rationale for using RTX in GO is the potential blockade of pathogenic autoantibody generation and production of inflammatory cytokines or the depletion of B cells as antigen-presenting cells. Data recently published showed a significantly different efficacy maybe due to a different disease duration and severity of patients recruited that means a different inflammatory pattern [48].
Environmental factors
As mentioned above, not everyone who inherits a sufficient load of genes positively related to the disease will develop an AITD. An environmental factor is necessary to induce the disease and several factors have been.
Treatments and drugs
Firstly, any thyroid injury that leads to exposure of thyroidal antigens can induce an autoimmune reaction. Both irradiation to the neck for Hodgkin’s disease and irradiation caused by nuclear accident have a detrimental effect on the thyroid; even radioactive treatment (RAI) and ethanol injection for toxic multinodular goiter can induce GD. The risk is higher if anti-TPO antibodies are present before the treatment, supporting the importance of a genetic predisposition [49]. Moreover, an increase in TRAb levels is common immediately after RAI treatment, with a high risk of GO worsening, mainly in smokers [50, 51].
Administration of immunosuppressant drugs can induce the deterioration or the onset of an AITD, mainly in the period of immune reconstitution. Some of these factors also induce expression of major histocompatibility component (MHC) on thyroid tissue; thyrocytes can then act as APC perpetuating the autoimmune process [52].
Sex
The high rate of autoimmune diseases in women suggests a possible causative role of estrogen receptors. A Polish study showed, in both sexes, an association between ESR2-A allele and GD with a strength comparable to polymorphisms of PTPN22 and CTLA4 CT60 loci [53].
Intrathyroidal fetal cell microchimerism is another possible etiologic agent in autoimmunity. Male fetal origin cells were detected in thyroid tissue specimens from patients with GD, but their role is still unclear since recent studies suggested a possible protective influence [54].
A potential explanation of the higher incidence of GD and GO in women could derive from an epigenetic determinant such as X chromosome inactivation. Yin et al. [55] found more skewed X chromosome inactivation (≥80% inactivation of one X chromosome in the same tissue) in GD when compared to healthy individuals, but the mechanisms through which this inactivation leads to higher risk are not yet known.
Environmental factors
The increased rates of autoimmune disorders reported in urban residential areas in Africa, Asia, Southern and Eastern Europe and Latin America suggest the relevant role of environmental factors more common in Western countries, such as smoking, specific infections, Western nutritional habits, xenobiotics, as well as physical and psychological stress [56].
Psychological stress
Psychological stress has been considered as a risk factor for many years, since GD onset is common after a stressful life event and the GD incidence increased during World War II. Theoretically, stress might cause activation of the adrenal cortex or the sympathetic nervous system and hypercortisolism would tend to suppress autoimmunity. However, studies on this topic showed contradictory results [57, 58].
Smoking
Among proinflammatory factors, smoking is one of the most common. The consistent connection between cigarette smoking and development or worsening of GD and GO firstly described in the end of 1980s was then confirmed by further studies. In particular, Brix et al. [59] found that the discordant monozygotic twin with GD was more likely to have smoked when compared to the healthy sibling.
A meta-analysis of studies investigating the association between smoking and thyroid diseases confirmed the increased risk of developing or worsening of GO beyond that associated with GD [60]. Interestingly, the risk of developing GO relates more to the number of cigarettes smoked following development of GD than to the life-cumulative smoking burden. In addition, its cessation appears to improve treatment response and to lower risk. The exact mechanism underlying the deleterious effects of smoking remains uncertain. Besides an obvious direct irritative effect on the ocular surface, smoking modulates immune reactions in the orbit is associated with an increase in the orbital connective tissue volume as assessed by MRI and with an increased adipogenesis and hyaluronic acid production in in vitro cultured orbital fibroblasts [61].
Viral and bacterial factors
Infections could play a role in the development of autoimmune disorders through different mechanisms: molecular mimicry of microorganisms, direct damage to the organ, induction of adhesion molecules and stimulation of immune cells response.
For years, viral infections have been thought to have an etiological role in autoimmune diseases. Some studies detected DNA from human foamy viruses in peripheral DNA of GD patients and proteins of human foamy virus in diseased thyroid tissues. Unfortunately, others failed to confirm these findings; thus, it remains unclear whether human foamy virus infection might be associated with GD [62]. In addition, enterovirus capsid protein and RNA have been identified in thyroid tissue from GD patients more often than in people without autoimmune disease; thus, a low-grade chronic enteroviral infection might be involved GD pathogenesis [63].
A transient increase in thyroid autoantibodies is possible after subacute thyroiditis, a virus-associated syndrome, maybe due to exposure of thyroid antigens after viral damage. Virus infection might also augment autoimmunity by causing non-specific secretion of IL-2, or by inducing MHC class II expression on thyroid cells. That could be the mechanism used by human T lymphotropic virus-1, repeatedly associated with AITD [64]. Moreover, a recent study suggested a possible contribution of Epstein–Barr virus in TRAb production following reactivation of the disease after viral infection [65].
As concerns bacteria, several possible links between thyroid tissue and Yersinia enterocolitica (YE) have been found.
The presence of peptides having sequence similarity within and on the surface of this intestinal parasite and the TSH-R was shown about 20 years ago. Moreover, the same authors recognized that immunoglobulins of patients recovering from YE infections exhibit GD-like activity in human thyroid membranes and a higher proportion of GD patients have been infected by YE compared to the general population. More recent data obtained by Hargreaves and coauthors suggest that YE porins could induce B cells somatic hypermutation to acquire a cross-reactive pathogenic response to TSH-R [66].
Another bacterium that may have an effect on the development of autoimmune thyroid disease is Helicobacter pylori (HP) infection of the gastric mucosa. An increased rate of prevalence of HP expressing the cytotoxin-associated gene A antigen (CagA) was found not only in ongoing autoimmune hyperthyroidism, but also in all GD patients compared to heathy controls [67]. A study on the Chinese population confirmed this and found that patients with CagA-positive HP and negative HLA-DQA1 0201 or positive HLA-DQA1 0501 were more likely exposed to GD compared with those with only one of these indices [68].
Finally, thyroid antigens can also interact by molecular mimicry with Clostridium botulinum neurotoxin which shares amino acid homology with thyroid autoantigens with some of the homologous regions containing HLA-DR3- and/or HLA-DR7-binding motifs [69].
Dietary habits
The increased rate of autoimmune disorders in urban residential areas of some countries could also be related to a change in dietary habits. People from urban areas could have a different food intake, in terms of calories and diversity, and a higher exposure to xenobiotics, such as food additives and preservatives, compared to rural dwellers. Interestingly, a recent paper showed a low risk of hyperthyroidism in people following a vegan, lacto-ovo and pesco vegetarian diets compared with omnivores [70].
Thus, if considered one by one all these environmental factors could be involved in triggering the disease in genetically predisposed people, but the link between all of them is unclear.
The gut microbiota
In this scenario, a group of researchers from different backgrounds started the INDIGO project, a multicenter European funded project to investigate the role of the gut bacteria in GD and GO pathogenesis.
There are several reasons for focusing on the gut. It is the first and the widest area of bacteria access that is why the highest concentration of T cells in the human body is located in the intestinal mucosa. It is even home to an enormous and complex community of commensal bacteria, known as the gut microbiota.
The “normal” adult human microbiota is extremely diverse and consists of hundreds of bacterial species reaching densities of up to 1012 bacteria per gram content in the large intestine. Since the intrauterine environment is sterile, bacteria do not colonize fetal body surfaces and intestine until the delivery. In the natural delivery, colonization occurs through contact with the maternal fecal and vaginal microbiota. In contrast, babies born by cesarean section have the first microbial contact from other sources such as mother’s skin.
Establishment of a stable microbiota takes several years and events occurring during early life are much more relevant in defining the richness and the diversity of the gut microbiota than those of adult life.
Neonatal microbiota is very similar to the maternal and it is then shaped by physiologic and pathological events such as feeding practice, introduction of solid food, diet, hygienic living conditions and use of antibiotics. Thus, for instance, babies that are breast-fed harbor a different microbiota than babies that are formula-fed [71].
Gut microbiota provides benefits to its host in many ways, including digestion, production of nutrients, detoxification, protection against pathogens and, especially, regulation of the immune system. In fact, in the gut mucosa, our lymphocytes are trained to react to microorganisms and the gut microbiota can regulate not only the local intestinal immune system but also systemic immune responses.
As described above, the microbiota and gut immune system coevolve and create an interaction useful for both. Thus, a key feature of intestinal APCs is their ability to protect the body against infection while still maintaining immune tolerance to the normal gut microbiota. For example, gut macrophages develop a unique phenotype, so-called inflammation anergy, referring to the non-inflammatory profile of intestinal macrophages when they encounter microbial stimuli in homeostatic conditions [72].
Interestingly, all the environmental factors listed so far can induce dysbiosis, an altered balance within the gut microbiota. Clearly, bowel infection, such as triggered by Y. enterocolitica or Clostridium botulinum, has a direct effect on the gut microbiota. Even if infection does not involve the gastrointestinal tract, dysbiosis can arise after administration of antibiotics or antivirals.
The discovery of the enteric nervous system in the nineteenth century confirmed and explained the existence of an intimate connection between gut and nervous system. Stress may affect different physiologic functions of the gastrointestinal tract including gastric secretion, gut motility, mucosal permeability and barrier function, visceral sensitivity and mucosal blood flow [73]. Interestingly, stress induces changes in neurotransmitter and proinflammatory cytokine levels, which can alter the growth, motility and virulence of pathogenic and commensal bacteria. For example, norepinephrine increases the virulence of some bacteria such as Escherichia coli or Campylobacter jejuni [74].
Cigarette smoking has a proinflammatory effect on several tissues and it is fascinating the direct role it can have on the gut, even in healthy people. In fact, intestinal microbiota composition changes after smoking cessation as characterized by an increase in key representatives from the phyla of Firmicutes and Actinobacteria as well as a decrease in Bacteroidetes and Proteobacteria [75]. Moreover, in healthy controls recruited in a clinical trial on Crohn’s disease, smokers also had higher Bacteroides–Prevotella (34.8%) than non-smokers (24.1%) (P = 0.038) [76].
Finally, several recent studies have shown that dietary factors alter the microbial community beyond the postnatal period both in animals and in humans. Trials on mice indicate that diet has a dominating role in shaping the gut microbiota and changing key populations may transform healthy gut microbiota into a disease-inducing entity. For example, in mice fed a low-fat, plant polysaccharide-rich diet and then switched to a “Western” diet, the microbiota composition shifted to an overgrowth of Firmicutes including Clostridium innocuum, Eubacterium dolichum, Catenibacterium mitsuokai and Enterococcus spp., as well as a significant reduction in several Bacteroides spp. [77].
Vegetarianism alters intestinal microbiota in humans because high amounts of fiber result in increased short-chain fatty acid production by microbes, which decrease the intestinal pH. This prevents the growth of potentially pathogenic bacteria such as E. coli and other members of the Enterobacteriaceae [78]. A clinical trial comparing the gut microbiota of children from different regions, in particular Europe and rural Africa, confirmed these findings. Interestingly, European children have a microbiota depleted of Bacteroidetes and enriched in Enterobacteriaceae, which the authors attributed to low dietary fiber intake [79].
The complex interplay between immune cells and microbiota explains the relevance of any disequilibrium in the gut.
The main actors in this process are the dendritic cells (DC), specialized antigen-presenting cells located in intraepithelial pockets, which play a “sentinel” role to protect our body from putative aggressors and to induce tolerogenic responses toward harmless antigens. DCs quickly adapt to changes in microenvironment and their functions are dictated by several factors including the encounter with external cues [80]. DCs are recruited to the lamina propria of the small intestine after bacterial infection, and their number depends on the pathogenicity of the microorganisms encountered.
Germ-free animals are experimental animals reared in a sterile environment and never exposed to any microorganisms, and they show a reduced number of intestinal but not systemic dendritic cells. Monocolonization of germ-free animals with E. coli was sufficient to recruit DCs to their intestines [81]. While some microorganisms can directly bind to epithelial cells, DCs can also monitor the contents of the intestinal lumen sending periscope-like dendrites outside the epithelium. They then produce a variety of soluble factors, including chemokines and cytokines, which promote the recruitment and activation of other DC. They even migrate into the mesenteric lymph nodes where they induce the differentiation of naïve CD4+ T cells into four major subtypes: T helper 1 (Th1), Th2, Th17, or regulatory T cell. The proper regulation and balance of T-cell subtypes is a crucial factor in determining health status. Treg are key mediators of immune tolerance and its dysfunction can lead to autoimmune disorders with specific bacterial species even being associated with development of particular T-cell subtypes. Bacteroides fragilis was shown to induce the development of a systemic Th1 response through its polysaccharide A molecules. In contrast, segmented filamentous bacteria (SFB) were found to be potent inducers of Th17 cells in the lamina propria [82]. Recently, Clostridia, particularly those of cluster IV and XIVa, were shown to be capable of promoting the induction of colonic Tregs [83].
Although not required to shape the systemic CD8+ T cell repertoire, the gut microbiota plays an important role in conditioning CD8+ T cells to modulate other peripheral immune cells, such as marginal zone B cells [84].
Gut-associated B cells are mostly immunoglobulin (Ig) A-secreting plasma cells located in the Peyer’s patches.
Germ-free animals have a reduced number and cellularity of the Peyer’s patches and, consequently lower IgA levels and reduced plasma cells numbers in their intestine. Bacterial-specific IgA, produced following colonization, is both likely to adapt to changes in the microbial composition and to shape it [85].
Thus, there is a constant collaboration and interplay between gut microbiota and immune system, not only in newborns, whose immune system is immature, but lifelong. It is clear that every condition that alters the gut microbiota’s balance can influence the systemic immune system. Several studies evidenced the link between bowel disease and autoimmune disorders. One of the most complete is that of Shor DB’s group who aimed to determine the prevalence of gastrointestinal autoantibodies in patients with several autoimmune disorders, such as antiphospholipid syndrome (APS), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), diabetes mellitus type 1 (DM), autoimmune thyroid disease, pemphigus vulgaris, polyarteritis nodosa (PAN), Sjögren’s syndrome, cryoglobulinemia, Wegener’s granulomatosis, Churg–Strauss syndrome, giant cell (temporal) arteritis, microscopic polyangiitis, Crohn’s disease, ulcerative colitis (UC) and systemic sclerosis [86].
Prevalence of IgA antigliadin was significantly higher in APS (7.1%, P = 0.012) and in pemphigus vulgaris (25%, P = 0.008) patients, as compared with healthy controls. The presence of IgG antigliadin was more common among Crohn’s disease (20.5%, P = 0.023) and RA (6.5%, P = 0.027) patients and finally, IgG antitissue transglutaminases were frequently observed in APS (6.1%, P = 0.012), in giant cell arteritis (11.5%, P = 0.013) and in UC (11.1%, P = 0.018) patients. Interestingly, they also reported an association also with autoimmune thyroid disease; GD patients showed a higher prevalence of IgG anti-Saccharomyces cerevisiae (highly specific for Crohn’s disease) compared to healthy controls (5.7% in Graves’ disease vs. 0.5% in controls P = 0.018). Some preliminary results obtained in the INDIGO project confirm this point. In fact, fecal samples of GD patients with severe ocular involvement showed the highest presence of yeast (expressed as colony forming unit/g). The association between both Hashimoto’s thyroiditis and GD and inflammatory bowel disease, mainly Crohn’s disease and UC, has been long known while a very recent paper reviewed the literature on cases of concomitant inflammatory bowel disease (IBD) and thyroid disorders. After the first case of concomitant GD and UC in 1968, the authors identified a further 16 cases but there was no clear tendency in the order of GD/UC diagnosis nor in the time interval between the two disorders or in the type/severity of colitis. As for Crohn’s disease, the author identified three case reports [87].
Except case reports, no prospective studies have been done to assess the association between inflammatory bowel disease and autoimmune thyroid disorders. Moreover, there are even fewer data regarding GO patients.
Kahaly’s group analyzed about 1000 records of AITD patients in a retrospective cross-sectional study and found a positive association between GD and celiac disease (10.8% of celiac disease in GD group, P value <0.001). Moreover, multivariate analysis showed that celiac disease was associated positively with ocular involvement (13.3% of GO vs. 4.3% without ocular involvement, P value <0.001) [88].
The Indigo project (http://www.indigo-iapp.eu/) hypothesizes that in people with GD/GO, either microbial species favoring development of inflammatory TH17 cells predominate or species leading to increased Treg cells are underrepresented. It will apply 16S rRNA sequencing to analyze the gut microbiomes of GD/GO patients and compare them with healthy controls from the same geographic region. It also aims to seek prognostic biomarkers of GD and GO in order to facilitate early preventative intervention and will assess how probiotics may help to avoid or reduce disease progression The project will compare antibody responses in GD patients and controls to determine whether microbial or food derived antigens are involved in triggering disease or associated with GO progression. In particular, it will determine in the GD population not only the prevalence of IgA and IgG antideamidated gliadin and tissue transglutaminases but also assess a possible hypersensitivity against several food antigens, such as cow’s milk, egg white and yolk, white fish and shellfish, corn rice, oak and several others. Moreover, the same immune reaction will be tested in the cohort of patients who develop ocular involvement in order to find a possible risk factor link to the gut.
References
DeGroot LJ (2016) Graves’ disease and the manifestations of thyrotoxicosis in www.thyroidmanager.com, last update 14 July 2016. Published by ENDOCRINE EDUCATION Inc, South Dartmouth, MA
Bartalena L, Fatourechi V (2014) Extrathyroidal manifestations of Graves’ disease: a 2014 update. J Endocrinol Investig 37(8):691–700. doi:10.1007/s40618-014-0097-2
Potgieser PW, Wiersinga WM et al (2015) Some studies on the natural history of Graves’ orbitopathy: increase in orbital fat is a rather late phenomenon. Eur J Endocrinol 173(2):149–153. doi:10.1530/EJE-14-1140
Abraham-Nordling M, Byström K et al (2011) Incidence of hyperthyroidism in Sweden. Eur J Endocrinol 165(6):899–905. doi:10.1530/EJE-11-0548
Laurberg P, Berman DC et al (2012) Incidence and clinical presentation of moderate to severe graves’ orbitopathy in a Danish population before and after iodine fortification of salt. J Clin Endocrinol Metab 97(7):2325–2332. doi:10.1210/jc.2012-1275
Perros P, Žarković M et al (2015) PREGO (presentation of Graves’ orbitopathy) study: changes in referral patterns to European Group On Graves’ Orbitopathy (EUGOGO) centres over the period from 2000 to 2012. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-306733
Wang Y, Smith TJ (2014) Current concepts in the molecular pathogenesis of thyroid-associated ophthalmopathy. Investig Ophthalmol Vis Sci 55(3):1735–1748. doi:10.1167/iovs.14-14002
Marinò M, Latrofa F, Menconi F, Chiovato L, Vitti P (2015) Role of genetic and non-genetic factors in the etiology of Graves’ disease. J Endocrinol Investig 38(3):283–294. doi:10.1007/s40618-014-0214-2
Rapoport B, McLachlan SM (2014) Graves’ hyperthyroidism is antibody-mediated but is predominantly a Th1-type cytokine disease. J Clin Endocrinol Metab 99(11):4060–4061. doi:10.1210/jc.2014-3011
Ludgate M (2000) Animal models of Graves’ disease. Eur J Endocrinol 142:1–8
Nagayama Y (2007) Graves’ animal models of Graves’ hyperthyroidism. Thyroid 17(10):981–988
Jenkins RC, Weetman AP (2002) Disease associations with autoimmune thyroid disease. Thyroid 12(11):977–988
Draman MS, Ludgate M (2016) Thyroid eye disease-an update. Expert Rev Ophthalmol. doi:10.1080/17469899.2016.1202113
Zhang L, Baker G et al (2006) Biological effects of thyrotropin receptor activation on human orbital preadipocytes. Investig Ophthalmol Vis Sci 47(12):5197–5203
Kumar S, Nadeem S et al (2011) A stimulatory TSH receptor antibody enhances adipogenesis via phosphoinositide 3-kinase activation in orbital preadipocytes from patients with Graves’ ophthalmopathy. J Mol Endocrinol 46(3):155–163. doi:10.1530/JME-11-0006
Wakelkamp IM, Gerding MN et al (2000) Both Th1- and Th2-derived cytokines in serum are elevated in Graves’ ophthalmopathy. Clin Exp Immunol 121:453–457
Eckstein AK, Plicht M et al (2006) Thyrotropin receptor autoantibodies are independent risk factors for Graves’ ophthalmopathy and help to predict severity and outcome of the disease. J Clin Endocrinol Metab 91(9):3464–3470
Banga JP, Moshkelgosha S et al (2015) Modeling Graves’ orbitopathy in experimental Graves’ disease. Horm Metab Res 47(10):797–803. doi:10.1055/s-0035-1555956. (Erratum in: Horm Metab Res 2015 Sep 47(10):e4)
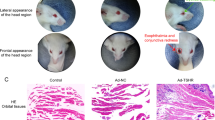
Berchner-Pfannschmidt U, Moshkelgosha S et al (2016) Comparative assessment of female mouse model of graves’ orbitopathy under different environments, accompanied by proinflammatory cytokine and T-cell responses to thyrotropin hormone receptor antigen. Endocrinology 157(4):1673–1682. doi:10.1210/en.2015-1829
Smith TJ, Huetwell FGL et al (2012) Role of insulin-like growth factor-1 (IGF-1) pathway in the pathogenesis of Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26:291–302
Song D, Wang R et al (2012) Locally produced insulin-like growth factor-1 by orbital fibroblasts as implicative pathogenic factor rather than systemically circulated IGF-1 for patients with thyroid-associated ophthalmopathy. Graefes Arch Clin Exp Ophthalmol 250:433–440
Krieger CC, Neumann S et al (2015) Bidirectional TSH and IGF-1 receptor cross talk mediates stimulation of hyaluronan secretion by Graves’ disease immunoglobins. J Clin Endocrinol Metab 100(3):1071–1077. doi:10.1210/jc.2014-3566
Villanueva R, Greenberg DA et al (2003) Sibling recurrence risk in autoimmune thyroid disease. Thyroid 13(8):761–764
Brix TH, Kyvik KO et al (2001) Evidence for a major role of heredity in Graves’ disease: a population-based study of two Danish twin cohorts. J Clin Endocrinol Metab 86:930–934
Lee HJ, Li CW et al (2015) Immunogenetics of autoimmune thyroid diseases: a comprehensive review. J Autoimmun. doi:10.1016/j.jaut.2015.07.009
Effraimidis G, Wiersinga WM (2014) Mechanisms in endocrinology: autoimmune thyroid disease: old and new players. Eur J Endocrinol 170(6):R241–R252. doi:10.1530/EJE-14-0047
Nakano A, Watanabe M et al (2007) Apoptosis-induced decrease of intrathyroidal CD4(+)CD25(+) regulatory T cells in autoimmune thyroid diseases. Thyroid 17(1):25–31
Marazuela M, Garcia-Lopez MA et al (2006) Regulatory T cells in human autoimmune thyroid disease. J Clin Endocrinol Metab 91(9):3639–3646
Glick AB, Wodzinski A et al (2013) Impairment of regulatory T-cell function in autoimmune thyroid disease. Thyroid 23(7):871–878
Kula D, Bednarczuk T et al (2006) Interaction of HLA-DRB1 alleles with CTLA-4 in the predisposition to Graves’ disease: the impact of DRB1*07. Thyroid 16(5):447–453
Ban Y, Tozaki T et al (2005) The codon 620 single nucleotide polymorphism of the protein tyrosine phosphatase-22 gene does not contribute to autoimmune thyroid disease susceptibility in the Japanese. Thyroid 15(10):1115–1118
Lopez ER, Zwermann O et al (2004) A promoter polymorphism of the CYP27B1 gene is associated with Addison’s disease, Hashimoto’s thyroiditis, Graves’ disease and type 1 diabetes mellitus in Germans. Eur J Endocrinol 151(2):193–197
Cuddihy RM, Dutton CM, Bahn RS (1995) A polymorphism in the extracellular domain of the thyrotropin receptor is highly associated with autoimmune thyroid disease in females. Thyroid 5:89–95
Kotsa KD, Watson PF, Weetman AP (1997) No association between a thyrotropin receptor gene polymorphism and Graves’ disease in the female population. Thyroid 7:31
Hiratani H, Bowden DW et al (2005) Multiple SNPs in intron 7 of thyrotropin receptor are associated with Graves’ disease. J Clin Endocrinol Metab 90(5):2898–2903
Dechairo BM, Zabaneh D et al (2005) Association of the TSHR gene with Graves’ disease: the first disease specific locus. Eur J Hum Genet 13(11):1223–1230
Płoski R, Brand OJ et al (2010) Thyroid stimulating hormone receptor (TSHR) intron 1 variants are major risk factors for Graves’ disease in three European Caucasian cohorts. PLoS ONE 5(11):e15512. doi:10.1371/journal.pone.0015512
Huber AK, Jacobson EM et al (2008) Interleukin (IL)-23 receptor is a major susceptibility gene for Graves’ ophthalmopathy: the IL-23/T-helper 17 axis extends to thyroid autoimmunity. J Clin Endocrinol Metab 93:1077–1081
Khalilzadeh O, Anvari M et al (2009) Graves’ ophthalmopathy and gene polymorphisms in interleukin-1alpha, interleukin-1beta, interleukin-1 receptor and interleukin-1 receptor antagonist. Clin Exp Ophthalmol 37:614–619
Daroszewski J, Pawlak E et al (2009) Soluble CTLA-4 receptor an immunological marker of Graves’ disease and severity of ophthalmopathy is associated with CTLA-4 Jo31 and CT60 gene polymorphisms. Eur J Endocrinol 161:787–793
Alevizaki M, Mantzou E et al (2009) The Pro12Ala PPARgamma gene polymorphism: possible modifier of the activity and severity of thyroid-associated orbitopathy (TAO). Clin Endocrinol (Oxf) 70:464–468
Vannucchi G, Covelli D et al (2013) The therapeutic outcome to intravenous steroid therapy for active Graves’orbitopathy is influenced by the time of response but not polymorphisms of the glucocorticoid receptor. Eur J Endocrinol 170(1):55–61. doi:10.1530/EJE-13-0611
Feldon SE, Park DJJ et al (2005) Autologous T-lymphocytes stimulate proliferation of orbital fibroblasts derived from patients with Graves’ ophthalmopathy. Investig Ophthalmol Vis Sci 46:3913–3921
Antonelli A, Ferrari SM et al (2015) Autoimmune thyroid disorders. Autoimmun Rev 14(2):174–180. doi:10.1016/j.autrev.2014.10.016
Campi I, Tosi D et al (2015) B cell-activating factor (BAFF) and Baff receptor expression in autoimmune and non autoimmune thyroid diseases. Thyroid 25(9):1043–1049. doi:10.1089/thy.2015.0029
Prabhakar BS, Bahn RS, Smith TJ (2003) Current perspective on the pathogenesis of Graves’ disease and ophthalmopathy. Endocr Rev 24:802–835
Ajjan AR, Weetman AP (2004) New understanding of the role of cytokines in the pathogenesis of Graves’ ophthalmopathy. J Endocrinol Investig 27:237–245
Salvi M, Campi I (2015) Medical treatment of Graves’ orbitopathy. Horm Metab Res 47(10):779–788. doi:10.1055/s-0035-1554721
Schmidt M, Gorbauch E et al (2006) Incidence of postradioiodine immunogenic hyperthyroidism/Graves’ disease in relation to a temporary increase in thyrotropin receptor antibodies after radioiodine therapy for autonomous thyroid disease. Thyroid 16(3):281–288
Laurberg P, Wallin G et al (2008) TSH-receptor autoimmunity in Graves’ disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur J Endocrinol 158(1):69–75. doi:10.1530/EJE-07-0450
Träisk F, Tallstedt L et al (2009) Thyroid Study Group of TT 96. Thyroid-associated ophthalmopathy after treatment for Graves’ hyperthyroidism with antithyroid drugs or iodine-131. J Clin Endocrinol Metab 94(10):3700–3707. doi:10.1210/jc.2009-0747
Mukuta T, Arreaza G et al (1997) Thyroid xenografts from patients with Graves’ disease in severe combined immunodeficient mice and NIH-beige-nude-xid mice. Clin Investig Med 20:5–15
Kisiel B, Bednarczuk T et al (2008) Polymorphism of the oestrogen receptor beta gene (ESR2) is associated with susceptibility to Graves’ disease. Clin Endocrinol (Oxf) 68(3):429–434
Cirello V, Rizzo R et al (2015) Fetal cell microchimerism: a protective role in autoimmune thyroid diseases. Eur J Endocrinol 173(1):111–118. doi:10.1530/EJE-15-0028
Yin X, Latif R et al (2007) Thyroid epigenetics: X chromosome inactivation in patients with autoimmune thyroid disease. Ann N Y Acad Sci 1110:193–200
Carmi G, Amital H (2011) The geoepidemiology of autoimmunity: capsules from the 7th international congress on autoimmunity, Ljubljana, Slovenia, May 2010. Isr Med Assoc J 13(2):121–127
Chiovato L, Pinchera A (1996) Stressful life events and Graves’ disease. Eur J Endocrinol 134:680–682
Effraimidis G, Tijssen JG et al (2012) Involvement of stress in the pathogenesis of autoimmune thyroid disease: a prospective study. Psychoneuroendocrinology 37(8):1191–1198. doi:10.1016/j.psyneuen.2011.12.009
Brix TH, Hansen PS et al (2000) Cigarette smoking and risk of clinically overt thyroid disease: a population-based twin case-control study. Arch Intern Med 160:661–666
Vestergaard P (2002) Smoking and thyroid disorders: a meta-analysis. Eur J Endocrinol 146:153–161
Cawood TJ, Moriarty P et al (2007) Smoking and thyroid-associated ophthalmopathy: a novel explanation of the biological link. J Clin Endocrinol Metab 92(1):59–64
Wick G, Trieb K et al (1993) Possible role of human foamy virus in Graves’ disease. Intervirology 35:101–107
Hammerstad SS, Tauriainen S et al (2013) Detection of enterovirus in the thyroid tissue of patients with graves’ disease. J Med Virol 85(3):512–518. doi:10.1002/jmv.23476
Tomoyose T, Komiya I et al (2002) Cytotoxic T-lymphocyte antigen-4 gene polymorphisms and human T-cell lymphotrophic virus-1 infection: their associations with Hashimoto’s thyroiditis in Japanese patients. Thyroid 12:673–677
Nagata K, Higaki K et al (2014) Presence of Epstein–Barr virus-infected B lymphocytes with thyrotropin receptor antibodies on their surface in Graves’ disease patients and in healthy individuals. Autoimmunity 47(3):193–200. doi:10.3109/08916934.2013.879863
Hargreaves CE, Grasso M et al (2013) Yersinia enterocolitica provides the link between thyroid-stimulating antibodies and their germline counterparts in Graves’ disease. J Immunol 190(11):5373–5381. doi:10.4049/jimmunol.1203412
Bassi V, Santinelli C et al (2010) Identification of a correlation between Helicobacter pylori infection and Graves’ disease. Helicobacter 15(6):558–562. doi:10.1111/j.1523-5378.2010.00802.x
Wang Y, Zhu S et al (2013) Interaction between gene A-positive Helicobacter pylori and human leukocyte antigen II alleles increase the risk of Graves disease in Chinese Han population: an association study. Gene 531(1):84–89. doi:10.1016/j.gene.2013.07.069
Gregoric E, Gregoric JA et al (2011) Injections of Clostridium botulinum neurotoxin A may cause thyroid complications in predisposed persons based on molecular mimicry with thyroid autoantigens. Endocrine 39(1):41–47. doi:10.1007/s12020-010-9410-9
Tonstad S, Nathan E et al (2015) Prevalence of hyperthyroidism according to type of vegetarian diet. Public Health Nutr 18(8):1482–1487. doi:10.1017/S1368980014002183
Dominguez-Bello MG, Costello EK et al (2010) Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci USA 107:11971–11975
Smythies LE, Sellers M et al (2005) Human intestinal macrophages display profound inflammatory anergy despite avid phagocytic and bacteriocidal activity. J Clin Investig 115:66–75 PMID:15630445
Soderholm JD, Perdue MH (2001) Stress and gastrointestinal tract. II. Stress and intestinal barrier function. Am J Physiol Gastrointest Liver Physiol 280:G7–G13
Lyte M, Vulchanova L, Brown DR (2011) Stress at the intestinal surface: catecholamines and mucosa-bacteria interactions. Cell Tissue Res 343:23–32
Biedermann L, Brülisauer K et al (2014) Smoking cessation alters intestinal microbiota: insights from quantitative investigations on human fecal samples using FISH. Inflamm Bowel Dis 20(9):1496–1501
Benjamin JL, Hedin CR et al (2012) Smokers with active Crohn’s disease have a clinically relevant dysbiosis of the gastrointestinal microbiota. Inflamm Bowel Dis 18(6):1092–1100
Turnbaugh PJ, Ridaura VK et al (2009) The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med. doi:10.1126/scitranslmed.3000322
Zimmer J, Lange B et al (2012) A vegan or vegetarian diet substantially alters the human colonic faecal microbiota. Eur J Clin Nutr 66:53–60
De Filippo C, Cavalieri D et al (2010) Impact of diet in shaping gut microbiota revealed by a comparative study in children from europe and rural africa. Proc Natl Acad Sci USA 107:14691–14696
Rescigno M (2015) Dendritic cell functions: learning from microbial evasion strategies. Semin Immunol 27(2):119–124. doi:10.1016/j.smim.2015.03.012
Williams AM, Probert CS et al (2006) Effects of microflora on the neonatal development of gut mucosal T cells and myeloid cells in the mouse. Immunology 119:470–478
Gaboriau-Routhiau V, Rakotobe S et al (2009) The key role of segmented filamentous bacteria in the coordinated maturation of gut helper T cell responses. Immunity 31:677–689. doi:10.1016/j.immuni.2009.08.020
Atarashi K, Tanoue T et al (2011) Induction of colonic regulatory T cells by indigenous Clostridium species. Science 331:337–341. doi:10.1126/science.1198469
Wei B, Su TT et al (2008) Resident enteric microbiota and CD8 + T cells shape the abundance of marginal zone B cells. Eur J Immunol 38(12):3411–3425. doi:10.1002/eji.200838432
Wu HJ, Wu E (2012) The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes 3(1):4–14. doi:10.4161/gmic.19320
Shor DB, Orbach H et al (2012) Gastrointestinal-associated autoantibodies in different autoimmune diseases. Am J Clin Exp Immunol 1(1):49–55
Shizuma T (2016) Concomitant thyroid disorders and inflammatory bowel disease: a literature review. Biomed Res Int 2016:5187061. doi:10.1155/2016/5187061
Ponto KA, Schuppan D et al (2014) Thyroid-associated orbitopathy is linked to gastrointestinal autoimmunity. Clin Exp Immunol 178(1):57–64. doi:10.1111/cei.12395
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The article does not contain any data using human subjects or animal experiments performed by the authors.
Informed consent
No informed consent.
Rights and permissions
About this article
Cite this article
Covelli, D., Ludgate, M. The thyroid, the eyes and the gut: a possible connection. J Endocrinol Invest 40, 567–576 (2017). https://doi.org/10.1007/s40618-016-0594-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0594-6