Abstract
Introduction
The aim of this study was to evaluate the association of breast cancer with thyroid diseases. Many authors have already studied the possible relationship between these two diseases, but the results are nowadays conflicting.
Materials and methods
Our study examining 867 patients with breast cancer (862 women and 5 men, average age = 61 years old) of whom 141 also had thyroid disease evaluated the recurrence of thyroid diseases and their association with different types of breast cancer. Statistical analyses were performed using SPSS software for Windows; we used nonparametric tests (Chi-square and Mann–Whitney), and the level of significance was set at p < 0.05.
Results
We found a significant association between breast cancer diagnosed after menopause and thyroid disease (p < 0.003). Moreover, we analyzed the role of thyroid autoimmunity identifying an association between chronic autoimmune thyroiditis and breast cancer diagnosed before menopause (p < 0.05). Regarding receptor profile of breast carcinoma, we have found an increased expression of estrogen receptors in patients with autoimmune thyroiditis compared to patients with any other thyroid diseases (p < 0.03). Contrariwise, we do not have found any difference between the group with every thyroid disease and the group without thyroid disease (p < 1.00). We did not find other statistically significant associations with breast cancer’s parameters like family history, tumor size, lymph node metastasis, distant metastasis, cancer clinical and pathological stage, differentiation grade and expression of Ki67, p53 and Her2 in the two main groups with or without thyroid disease. Likewise, we did not found other statistically significant association between hypothyroidism or hyperthyroidism and breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common tumor in women: In 2013, in Italy, about 46,000 new cases were diagnosed (only 2 % were males). Thyroid diseases are also very common in Italy: About 11,000 new cases of thyroid cancer were diagnosed in women, and about 4000 were diagnosed in men. Additionally, 10 % of Italian people shows thyroid functional alterations, and from 1 to 23 % have goiter (in different regions). In Italy, every year about 40,000 thyroidectomies are performed in dedicated Endocrinological Surgical Units with specific surgical instruments such as intra-operative neuromonitoring (IONM) of recurrent laryngeal nerves [1].
The possible existence of a correlation between thyroid disease and breast cancer has been discussed in the literature since many years. Myhill and Sincher’s studies, respectively, in 1966 and 1967, examined thyroid function in patients with breast cancer, hypothesizing a possible correlation between these diseases and the interference of thyroid hormones on prognosis of breast cancer [2, 3].
This theme deepened over the years by many authors, but with contrasting results. The relationship between these two diseases remains still controversial.
Several recent studies concluded that breast cancer and thyroid disease are closely related, such as Muller who observed that in patients with benign thyroid diseases, there is a high prevalence of breast cancer [4]. On the other hand, in 2009 Michalaki et al. did not find statistically significant differences between the incidence of thyroid diseases in breast cancer patients and controls [5]. Similarly, in 2012, Grani et al. did not find statistically significant correlations in the frequency of nodular thyroid diseases in breast cancer patients and controls, while showing an increased incidence of autoimmune disease in breast cancer patients compared to in controls, but not proved to be statistically significant [6].
The exact mechanisms that bind thyroid disease and breast cancer have not yet been found, although a series of hypotheses have been proposed. The presence of the sodium iodide symporter, which is both in thyroid tissue and in breast cancer tissue, has led to the hypothesis that absorption and oxidation of iodine could play a relevant role in breast cancer development. In 2000, Tazebay et al. demonstrated an increased expression of the sodium iodide symporter in breast cancer tissue compared to peritumoral tissue and breast tissue in healthy subjects. This over-expression of this symporter in malignant breast tissues could have implications in the development of future therapies [7, 8]. The possible interaction between thyroid gland and breast tissue may be explained by the presence of TSH receptors in fatty tissue that is abundant in mammary gland [9].
In 2006, Conde et al. studied the thyroid hormone receptor expression profiles: He demonstrated that in samples from benign diseases and carcinoma in situ, there is a higher TR-α (thyroid receptor α) expression compared to samples of infiltrating carcinoma. This deregulation suggests a triggering role in the development of breast cancer [10].
Although many studies suggested an association between breast cancer and autoimmune thyroid disease or the presence of anti-TPOAb (antithyroid peroxidase antibodies), few is known about the possible increased risk of developing breast cancer in patients with autoimmune thyroid disease. In 2005, Kuijpens et al. researched this correlation in a group of 2775 women, of whom 278 were positive for anti-TPOAb, but he failed to identify a sure correlation between the presence of anti-TPOAb and the onset of breast cancer during the follow-up [11]. Other studies analyzed the possible influence of thyroid autoimmunity on breast cancer. Among these, Farahati et al. in 2012 observed that the positivity of anti-TPOAb is associated with a significantly lower frequency of distant metastases and Muller observed that women with anti-TPOAb and breast cancer have a better prognosis [12, 13]. In 2006, Giustarini et al. showed that the prevalence of anti-TPOAb and anti-thyroglobulin antibodies in breast cancer patients is significantly higher than in patients with benign breast nodules and healthy controls, confirming a strict relationship between thyroid autoimmunity and breast cancer [14].
Patients and methods
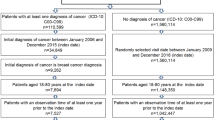
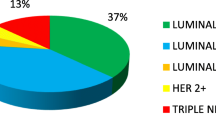
This study includes 867 consecutive patients (862 female patients and 5 male patients) with breast cancer. They were treated from January 2009 to December 2013 at the General Surgery Unit of Circolo Hospital in Varese-Insubria University. The average age was 61 years; 725 patients had ductal carcinoma: 61 were ductal carcinoma in situ (DCIS), and 664 were invasive ductal carcinoma (DCI); 71 patients had lobular carcinoma, including 2 lobular carcinoma in situ (LCIS) and 69 invasive lobular carcinoma (LCI). The remaining 71 patients had rare histological types of breast cancer: 18 mucinous carcinoma, 13 mixed ductal-lobular carcinoma, 13 neuroendocrine carcinoma, 12 papillary carcinoma, 9 tubular carcinoma, 3 apocrine carcinoma, 2 medullary carcinoma and 1 cribriform carcinoma. One hundred forty-one patients (16 %) had benign or malignant thyroid disease (138 benign thyroid disease and 3 malignant). The remaining 725 had no history of thyroid pathology.
In the subgroup of 141 patients with thyroid disease (140 female patients and 1 male patient), 55 cases of primary hypothyroidism (39 %) were detected, 23 cases of hyperthyroidism (16 %) and 63 cases with other euthyroid thyroid diseases (45 %).
We have also investigated the possible autoimmune etiology of thyroid disorders: 67 % (37 cases) of hypothyroidism cases were autoimmune, while 33 % (18 cases) had negative antithyroid antibody; 48 % (11 cases) of hyperthyroidism cases were associated with Graves–Basedow disease, and the remaining 52 % (12 cases) is due to autonomous functioning thyroid nodules. Finally, 5 patients (7 %) had a chronic autoimmune thyroiditis in spontaneous functional compensation.
In our study, the group of 141 patients, of whom 140 were female, with breast cancer and thyroid disease was compared with the group including the remaining 726 patients, of whom 722 were female, with breast cancer not associated with a thyroid disease. A further comparison was made within the group of patients with both breast cancer and thyroid disease, and between patients with chronic autoimmune thyroiditis and patients with other non-autoimmune thyroid diseases.
Statistical analyses were performed using SPSS software for Windows; we used nonparametric tests (Chi-square and Mann–Whitney), and the level of significance was set at p < 0.05.
Results
Association of thyroid disease with breast cancer
The group of female patients (862) was divided into two subgroups on the basis of hormonal status: patients with breast cancer that arose before and after menopause. The results were the following: in 306 women who developed breast cancer before menopause, only 11 % (34 cases) also had a thyroid disease (18 cases of hypothyroidism, 6 cases of hyperthyroidism and 10 cases of thyroid diseases with spontaneous euthyroidism). In contrast, in 556 women who had breast cancer after menopause, 19 % (106 cases) had also a thyroid disease (37 cases of hypothyroidism, 17 cases of hyperthyroidism and 52 cases of thyroid diseases with spontaneous euthyroidism) (Table 1).
These data were analyzed using Chi-square test and were statistically significant for a higher association between breast cancer and thyroid disease in postmenopausal age (p < 0.003).
Autoimmune thyroid disease in patients with breast cancer
An important part of our study focused on the evaluation of occurrence of autoimmune thyroid disease in patients with breast cancer. In particular, female patients with breast cancer and thyroid disease (n = 140) were divided into two groups according to the onset of breast malignant disease, before or after menopause. The results are summarized in Table 2; they showed that in patients with thyroid disease and breast cancer before menopause, 44 % (15 cases of 34) had chronic autoimmune thyroiditis; instead, in the group with thyroid disease and breast cancer after menopause, only 25 % (27 cases of 106) had a chronic autoimmune thyroiditis. We found a statistically significant association between chronic autoimmune thyroiditis and breast cancer before menopause (p < 0.05).
If we consider the entire population (both women and men) with breast cancer and thyroid disease (141 cases) and we divide them into two groups (younger and older than 45 years), we found similar association between chronic autoimmune thyroiditis and breast cancer diagnosed before the age of 45 (p < 0.03) (Table 3).
Breast cancer’s receptor profile in patients with thyroid disease
Among patients with chronic autoimmune thyroiditis, about 98 % (41 cases out of 42) had estrogen receptors positive, and among patients with other thyroid diseases, only 85 % had estrogen receptors positive (84 cases out of 99). This difference was statistically significant (p < 0.03). According to these results, there might be a correlation between the positivity of receptors for estrogen and breast cancer in patients with chronic autoimmune thyroiditis.
This important difference is shown just in the group of patients with thyroid disease: Among the total population (867 cases), there was no difference in the expression of estrogen receptors (with or without thyroid disease). Among patients with thyroid disease, 89 % (125 cases) expressed estrogen receptors, while 11 % (16 cases) did not express them. Similar results were obtained in patients without thyroid disease: 89 % expressing estrogen receptors (643 cases) and 11 % (83 cases) did not.
We obtained similar results about progesterone receptors in patients with or without thyroid disease (Table 4).
We did not find other statistically significant associations with breast cancer’s parameters like family history, tumor size, lymph node metastasis, distant metastasis, cancer clinical and pathological stage, differentiation grade and expression of Ki67, p53 and Her2 in the two main groups with or without thyroid disease. In this study, hypothyroidism and hyperthyroidism have not been associated with breast cancer.
Comparing the family history, positive or negative, of patients in two groups with or without thyroid disease, we have seen that they had a positive family history in 26 % (37 cases) of patients with thyroid disease and in 25 % (184 cases) of patients without thyroid disease, while a negative family history was recorded in 74 % (104 cases) of patients with thyroid disease and in 75 % (542 cases) of patients without thyroid disease.
Regarding the histopathological classification of breast cancer, the recurrence of different histological types is distributed as shown in Table 5: In both groups, with or without thyroid disease, we observed the prevalence of ductal cancer cells. In 82 % (116 cases) of patients with thyroid disease, we found a ductal cell tumor; in patients without thyroid disease, 84 % (606 cases) had a malignancy with ductal cells.
Also regarding the differentiation grade, the results are similar in the two groups, with a prevalence of moderate differentiation variant.
Both groups of patients with and without thyroid disease showed no significant differences in tumor size, histopathological classification, grade of differentiation, molecular classification and TNM staging (Table 5).
Discussion
In the literature, there are many experimental, clinical and epidemiological studies which suggest an association between thyroid disease and the risk of developing breast cancer. However, despite large population studied, the relationship between these two diseases remains controversial, and conflicting results are reported. The purpose of this work was to investigate whether there could be a correlation between these diseases.
The diagnosis of breast cancer in postmenopausal women with a thyroid disease is significantly higher than in the group of patients with breast cancer before the menopause. This result may also be explained by increased incidence of thyroid diseases with the increase in age. On the contrary, Prinzi et al. [15] published a study in which women with thyroid disease have a significantly higher risk of developing breast cancer, but this risk was significantly higher in young age patients (<45 years). Many other previous studies, such as Muller’s et al. study [4] observed in patients with benign thyroid diseases a high prevalence of breast cancer.
Our study also investigated the presence of autoimmune thyroid disorders in patients with breast cancer. These observations have been carried out before the patients afforded therapeutic strategies, both medical and surgical care for breast cancer. It was observed that there is a strong association between chronic autoimmune thyroiditis and breast cancer occurring in young age (before age 45 considering both men and women affected by breast cancer or before menopause considering only female patients). This association is also found by Hardefeldt et al. [16], who suggested a strong relationship between thyroid autoimmunity and breast cancer, and by Giustarini et al. [15] who showed that the prevalence of anti-TPOAb and anti-thyroglobulin antibodies in breast cancer patients is significantly higher than in healthy controls, confirming a strict relationship between thyroid autoimmunity and breast cancer. Many previous reports demonstrated an increased prevalence of autoimmune thyroid disease in patients with breast cancer [17, 18], and particularly, they found that in patients with breast cancer, the presence of autoimmune thyroiditis was more common in younger patients [19].
Among patients with thyroid diseases, this study showed the presence of a relationship between the receptor profile of breast carcinoma and the presence of chronic autoimmune thyroiditis. In patients with chronic autoimmune thyroiditis, the estrogen receptors are mostly positive. This important difference is shown just in the group of patients with thyroid disease: Among the total population, there was no difference in the expression of estrogen receptors (with or without thyroid disease).
This study did not demonstrate the presence of a relationship between the receptor profile of breast carcinoma and the presence of thyroid disease. Both groups of patients, with or without thyroid disease, had equal percentages of tumors expressing receptors for estrogen and/or progesterone. This consideration is similar to Giani et al.’s results [18] that do not find a relationship among ER and PgR status. But in our study, statistically relevant data were found in the subgroup of patients with both thyroid disease and breast cancer. According to these results, there might be a correlation between the positivity of receptors for estrogen and breast cancer in patients with chronic autoimmune thyroiditis.
In this study, we did not find any statistically significant associations with different types of thyroid diseases and breast cancer characteristics.
Likewise, we did not find other statistically significant associations with breast cancer’s parameters like family history, tumor size, lymph node metastasis, distant metastasis, cancer clinical and pathological stage, differentiation grade and expression of Ki67, p53 and Her2 in the two main groups with or without thyroid disease.
The aim of this study was the identification of a subgroup of patients with a higher risk of developing breast cancer in order to intensify clinical-radiological surveillance to reach early diagnosis. Considering the impact that early diagnosis has on breast cancer prognosis, the chance to discover new categories of people who have a higher risk is an important resource. We still need further research to specify these data and investigate the role that the thyroid autoimmunity may play in breast cancer.
According to the results of this study, we can now say that there is an association between autoimmune thyroid disease, in particular chronic autoimmune thyroiditis, and the onset of breast cancer in young age. However, the pathophysiological mechanism that links the two diseases still needs to be investigated.
More multicentric studies are needed to confirm the correlation between these diseases, to identify a subpopulation of patients with higher risk of developing breast cancer, in order to increase clinical and radiological surveillance to get a diagnosis of breast cancer in early stage.
References
Dionigi G et al (2014) Intraoperative neuromonitoring in thyroid surgery: a point prevalence survey on utilization, management, and documentation in Italy. Updates Surg 66(4):269–276
Myhill J et al (1966) Thyroid function in breast cancer. Acta Endocrinol (Copenh) 51(2):290–300
Sicher K et al (1967) Thyroid activity in relation to prognosis in mammary cancer. Br J Cancer 21(3):512–518
Muller I et al (2011) High prevalence of breast cancer in patients with benign thyroid diseases. J Endocrinol Invest 34(5):349–352
Michalaki V et al (2009) Breast cancer in association with thyroid disorders. J Balk Union Oncol 14(3):425–428
Grani G et al (2012) Thyroid diseases in women with breast cancer. Clin Ter 163(6):e401–e404
Tazebay UH et al (2000) The mammary gland iodide transporter is expressed during lactation and in breast cancer. Nat Med 6(8):871–878
An JH et al (2015) A possible association between thyroid cancer and breast cancer. Thyroid 25(12):1330–1338
Davies TF (1994) The thyrotrophin receptors spread themselves around. J Clin Endocrinol Metabol 79:1232–1238
Conde I et al (2006) Influence of thyroid hormone receptors on breast cancer cell proliferation. Ann Oncol 17(1):60–64
Kuijpens JL et al (2005) Hypothyroidism might be related to breast cancer in post-menopausal women. Thyroid 15(11):1253–1259
Farahati J et al (2012) Anti-thyroid peroxidase antibodies are associated with the absence of distant metastases in patients with newly diagnosed breast cancer. Clin Chem Lab Med 50(4):709–714
Muller I et al (2014) Does thyroid peroxidase provide an antigenic link between thyroid autoimmunity and breast cancer? Int J Cancer 134(7):1706–1714
Giustarini E et al (2006) Thyroid autoimmunity in patients with malignant and benign breast diseases before surgery. Eur J Endocrinol 154(5):645–649
Prinzi N et al (2014) Prevalence of breast cancer in thyroid diseases: results of a cross-sectional study of 3,921 patients. Breast Cancer Res Treat 144(3):683–688
Hardefeldt PJ et al (2012) Benign thyroid disease is associated with breast cancer: a meta-analysis. Breast Cancer Res Treat 133(3):1169–1177
Gogas J et al (2001) Autoimmune thyroid disease in women with breast carcinoma. Eur J Surg Oncol 27:626–630
Smyth PPA (2003) The thyroid, iodine and breast cancer. Breast Cancer Res 2003(5):235–238
Giani G et al (1996) Relation between breast cancer and thyroid disease: relevance of autoimmune thyroid disorders in breast malignancy. J Clin Endocrinol Metabol 81:990–994
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have stated that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No informed consent.
Rights and permissions
About this article
Cite this article
Chiappa, C., Rovera, F., Rausei, S. et al. Breast cancer and thyroid diseases: analysis of 867 consecutive cases. J Endocrinol Invest 40, 179–184 (2017). https://doi.org/10.1007/s40618-016-0543-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0543-4