Abstract
Background
Vitamin D deficiency is a global health problem. Its role as an immune modulator has been recently emphasized. There is increasing evidence for the significant role of vitamin D in reducing the incidence of autoimmune diseases. However, little is known about the status of vitamin D in children and adolescents with autoimmune thyroiditis (AIT).
Objective
The goal of the present study was to assess vitamin D status in Egyptian children and adolescents with AIT and to explore its relation to biomarkers of autoimmunity and thyroid function.
Design
A prevalence case–control study that included 56 children with AIT and 56 healthy, age- and sex-matched subjects that served as the control group. The following was done for all participants: thorough history, physical examination, thyroid ultrasound, measurement of thyroid-stimulating hormone (TSH), free thyroxin (FT4), anti-thyroid peroxidase antibodies (TPOAb), anti-thyroglobulin antibody (TgAb) and assessment of serum 25-hydroxy vitamin D (25OHD) level.
Results
Overt hypothyroidism was detected in 42/56 while subclinical hypothyroidism was detected in 14/56 of the studied patients. Vitamin D deficiency rate was significantly higher in the AIT group compared to the control subjects (71.4 vs 21.4 %, P < 0.001). In AIT group, the mean level of 25OHD was significantly lower compared to the control group (16.2 ± 8.2 vs 33.9 ± 12.7 nmol/L, P < 0.001). The difference was more evident in patients with overt hypothyroidism than those with subclinical hypothyroidism (P < 0.01). There were significant negative correlations between serum 25OHD and age, duration of the disease, BMI, anti-TPOAb, anti-TGAb and TSH (P < 0.001 each). On the other hand, serum 25OHD correlated positively with FT4 levels. While 25OHD level was an independent risk factor for AIT, it failed to qualify as an independent risk for the progression of AIT to overt hypothyroidism after adjustment for other potential confounding factors; age, sex and BMI.
Conclusions
Low serum vitamin D is significantly associated with AIT in Egyptian children. However, vitamin D level is not an independent risk for the progression of AIT to overt hypothyroidism. BMI may have an influence on serum 25OHD levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, there has been a growing interest in the possible relationship between vitamin D, a secosteroid hormone that exerts widespread effects on cellular proliferation, differentiation, apoptosis, and angiogenesis, and variety of acute and chronic diseases [1, 2]. Vitamin D has been shown to affect the innate immunity by modulating monocyte/macrophage responses to bacterial infection via Toll-like receptors. Moreover, vitamin D receptors (VDR), nuclear receptors which regulate gene transcription by interacting with response elements in gene promoters, were discovered in immune system cells, such as monocytes, macrophages, dendritic cells, and activated lymphocytes [3]. The immune modulating effect of vitamin D was also highlighted by studies demonstrating an association between the incidence of several autoimmune diseases (including type 1 diabetes mellitus, multiple sclerosis, and systemic lupus erythematosus) and decreased serum levels of vitamin D [4]. While vitamin D status has been studied in different autoimmune diseases in adults, studies addressing its role in autoimmune thyroiditis, particularly in children, are generally few [5, 6]. An association between vitamin D status and AIT in Egyptian children has not been previously reported; up to our knowledge, this is the first study to address such potential role. In this study, we examined the prevalence of vitamin D deficiency in children with AIT and its relation to thyroid function tests and autoimmunity biomarkers.
Patients and methods
We consecutively enrolled 56 children and adolescents newly diagnosed with AIT. They were recruited as they attended the Endocrinology Clinic of Children Hospital, Assiut University, Egypt. Final enrollment in the study was confirmed by elevated serum level of anti-thyroid peroxidase antibodies and/or anti-thyroglobulin antibodies, and the typical finding of hypoechogenicity of the thyroid gland on high-resolution ultrasound scans [7, 8]. Subjects were excluded from the study if they had major illness or chronic inflammatory/autoimmune disease other than AIT. They were also excluded if they consumed vitamin D, multi-vitamins, calcium, or vitamin D/mineral fortified food during the previous 3 months. The control group comprised 56 healthy volunteers, of matched age and gender, who had no personal/family history of thyroid, autoimmune or chronic inflammatory illnesses. They had no clinical evidence of thyroid disease and had normal thyroid function and normal anti-TPO antibodies tests. A thorough history taking and complete physical examination aimed to find the signs of thyroid dysfunction or disease. The weight and height were measured and body mass index (BMI) was calculated (weight in kilograms divided by the square of the height in meters).
The study was approved by the ethics committee of Children Hospitals and Faculty of Medicine, Assiut University and was performed in accordance with the standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from the legal guardians of participants before enrollment in the study.
Laboratory investigations
Thyroid-stimulating hormone (TSH) serum level was determined by ultrasensitive immunometric assays (ImmuliteTM 2000 Third Generation, Diagnostic Products Corporation, Los Angeles, CA). Free thyroxin (FT4) was determined by radioimmunoassay (RIA) using an automated system (Roche Diagnostics).
The reference range for TSH was 0.4–4.0 mU/L, and for FT4 10.0–26.0 pmol/L. The coefficients of variations (CVs) were 5.0 and 5.1 % at TSH concentrations of 4.0 and 10.0 mU/L, respectively, and for FT4, the CV was 6.5 % at 10.0 pmol/L.
Subclinical hypothyroidism is defined as a serum thyroid-stimulating hormone (TSH) concentration above the statistically defined upper limit of the reference range when serum free T4 concentration is within its reference range. Overt hypothyroidism was defined as an elevated TSH in the presence of low free T4 levels [9].
Serum anti-thyroid peroxidase antibodies (TPOAb) and anti-thyroglobulin (TgAb) were measured by rapid enzyme-linked immunosorbent assay (ELISA); (Genesis Diagnostics, Littleport, UK). Tg Ab and TPO Ab concentrations more than 100 and 75 IU/ml, respectively, were considered positive and at least one positive antibody conferred the diagnosis of AIT.
Serum 25OH vitamin D level was estimated using a semi-automated solid-phase extraction, reverse-phase high-performance liquid chromatography assay [2]. Vitamin D status was classified according to the American Academy of Pediatrics (AAP)/LWEPS’s recommendations on the cutoff levels for states of vitamin D. A 25OH vitamin D level of <5 ng/ml was considered as severe deficiency, a level between 5 and 15 ng/ml as deficiency, a level of 15–20 ng/ml as insufficiency, and a level of 20–100 ng/ml as normal (sufficient) [10].
Statistical analysis
Simple statistics such as frequency, mean, and standard deviation (SD) were used. For comparison of two groups, Student’s t test was used for parametric data and Mann–Whitney U test for nonparametric data. Multiple groups were tested using ANOVA. Linear correlations were performed by Spearman’s or Pearson’s test. General linear model and logistic regression were used to test “between-subjects effects” and independent risk effectors, respectively. In regression model, the covariates are the quantitative variable (interval scale or ratio scale) and the factors are the qualitative variables (categorical/nominal). For all analyses, P values <0.05 were considered statistically significant. Data analysis was carried out using Statistical Package for Social Sciences (SPSS®, version 16).
Results
The mean age of the AIT patients was 14.32 ± 3.12 years and 78.6 % were female (44/56). Overt hypothyroidism was detected in 75 % of patients (42/56) while subclinical hypothyroidism was detected in 25 % (14/56).
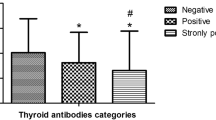
Children in the AIT group, compared to controls, had significantly higher BMI (P < 0.05), significantly higher vitamin D deficiency rates (71.42 vs 21.42 %, P < 0.0001) and significantly lower mean vitamin D levels (16.2 ± 8.2 vs 33.9 ± 12.7 nmol/L, P < 0.001); Table 1.
Children and adolescent with overt hypothyroidism, compared to the subclinical hypothyroidism group, were significantly older (15. 21 ± 4.32 vs 13.10 ± 3.56 years, P < 0.05), with significantly higher BMI (23.9 ± 3.33 vs 18.7 ± 3.54, P < 0.05), and significantly lower vitamin D levels (9.54 ± 3.21 vs 16.42 ± 7.51 nmol/L, P < 0.01).
Serum 25OH D showed a significant positive correlation with the free T4 level among AIT cases (r = 0.559, P < 0.001). However, it showed a significant negative correlation with each of the following (r is the correlation coefficient): age (r = −0.445), duration of the disease (r = −0.676), BMI (r = −0.765), anti-TPO (r = −0.533), anti-Tg (r = − 0.487) and serum TSH (r = −0.445) (P < 0.001 each).
General linear model of “between-subjects effect” showed that the age, BMI, and vitamin D deficiency rate were significantly associated with occurrence of overt hypothyroidism (P = 0.001, P = 0.012, and P = 0.0001, respectively) in AIT.
Multiple regression analysis showed that vitamin D deficiency is an independent risk factor for occurrence of AIT in our patients [odds ratio (OR) 8.2, 95 % confidence interval (CI) 4.2–27.7, P < 0.0001], and that normal vitamin D level is a protective factor in the control group (OR 2.32 CI 1.25–4.29, P = 0.007). However, serum 25OHD did not qualify as an independent risk factor for the progression of AIT to subclinical (OR 0.774, CI 0.278–5.386, P = 0.011) or overt hypothyroidism (OR 0.65, CI 0.48–1.9, P = 0.07); Table 2.
Discussion
In the present study, we reported a significantly higher vitamin D deficiency rate in the AIT group compared to the control group (P < 0.001). Our findings are in agreement with earlier studies showing lower serum vitamin D levels, and higher deficiency rates, in patients with Hashimoto’s thyroiditis [5, 11]. However, our findings are contradicted by other studies showing that vitamin D deficiency is not associated with thyroid autoimmunity [12, 13]. Hence, lower levels of vitamin D in AIT children may be a primary phenomenon involved in the pathogenesis of the disease, or may only represent an association caused by the higher rate of vitamin D deficiency in Egyptians [14]. In fact, earlier studies from Egypt showed that about 42 % of healthy children and 21 % of adolescent girls had vitamin D deficiency [15, 16]. Vitamin D deficiency in Egyptian children, despite availability of sunlight throughout the year, was explained by traditional and cultural factors in addition to a genetic predisposition [17].
In this study, vitamin D level showed a significant negative correlation with the serum levels of the autoimmune thyroid marker TPOAb. While the pathogenic role of TPOAb has not been clearly established, their presence denoted an ongoing thyroid destruction that may have started years before the establishment of thyroid hypofunction [18]. There is increasing body of evidence that vitamin D has direct regulatory effects on immune system components, including regulatory T cells, innate and adaptive immunity. Furthermore, vitamin D supplementation prevented the onset and/or progression of several autoimmune diseases in humans and animal models [4]. Modification of tolerance to self-antigens appears to be related to vitamin D-deficient status. One of the mechanisms described is the stimulation of the expression of FoxP3 in regulatory T cells that have a direct action on the adaptive tolerance to self-antigens [19]. Vitamin D inhibits the production of Th1 polarizing cytokine (IL-12), thereby indirectly shifting the polarization of T cells from a Th1 toward a Th2 phenotype and directly inhibits the production of Th1 cytokines (IL2 and IFNc), and enhances Th2 cytokine (IL-4) production. Vitamin D mediates its immunologic effects though binding VDR, and activation of the VDR-responsive genes [20, 21]. Several genetic variations have been identified in the VDR gene and were found to be associated with autoimmune diseases [22]. It is possible that vitamin D is contributing to the pathogenesis of AIT via genetic polymorphism.
Vitamin D level is a simple and inexpensive test that can serve as a prognostic marker for AIT [23, 24]. We noted a significantly lower vitamin D level in children and adolescents with overt hypothyroidism when compared to the subclinical group; vitamin D also correlated positively with the free T4 and negatively with TSH and TgAb. We can assume, from these observations, that assessment of vitamin D level early in AIT disease, in addition to vitamin D supplementation (if needed), may slow the progression of the autoimmune process and prevent the grave consequences of the disease [25]. However, further studies are needed to support these recommendations as vitamin D level was not an independent risk for the progression of AIT to overt hypothyroidism in our children.
Despite being significantly correlated with FT4 level, serum 25OH D did not qualify as an independent risk for the occurrence of overt hypothyroidism in children with AIT. This finding suggests that the effect of serum 25OH D on the clinical outcome of AIT would be confounded by other factors. In fact, children in the overt hypothyroidism group had a significantly higher age and BMI than the subclinical and control groups. Moreover, further analysis of our data confirmed that vitamin D levels correlated negatively and significantly with BMI. Generally, lower levels of vitamin D have been associated with obesity and increased BMI [26]. Vitamin D is a lipophilic hormone; it is possible that in obese patients it is stored in adipose tissue with increased catabolism and relative unavailability in the circulation to exert its physiological function. It is also possible that fatty liver disease, associated with obesity, reduces the hydroxylation of vitamin D to 25OH vitamin D [27, 28].
Our study has its limitations: the relative small number of cases, the complex nature of AIT pathogenesis, the effect of BMI on vitamin D homeostasis, and the possibility that an unknown factor like genetic polymorphism is implicated in the noted association of vitamin D deficiency and AIT progression. Further studies with larger number of patients are needed before conclusions can be drawn about the relation of vitamin D and AIT in children.
Conclusions
Low serum vitamin D is significantly associated with AIT in Egyptian children. However, vitamin D level is not an independent risk for the progression of AIT to overt hypothyroidism. BMI may have an influence on serum 25OHD levels. Further studies evaluating the pathophysiologic role of vitamin D in AIT children are needed.
Abbreviations
- FT4:
-
Free thyroxine
- AIT:
-
Autoimmune thyroiditis
- 25OHD:
-
25-Hydroxyvitamin D
- TSH:
-
Thyroid-stimulating hormone
- VDR:
-
Vitamin D receptor
- TPOAb:
-
Thyroid peroxidase antibodies
- TgAb:
-
Anti-thyroglobulin antibodies
- BMI:
-
Body mass index
References
Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C (2010) Vitamin D: modulator of the immune system. Curr Opin Pharmacol 10(4):482–496
Romagnoli E, Carnevale V, Biondi P, Minisola S (2014) Vitamin D supplementation: when and how? J Endocrinol Invest 37(7):603–607
Kamen DL, Tangpricha V (2010) Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity. J Mol Med 88(5):441–450
Shoenfeld N, Amital H, Shoenfeld Y (2009) The effect of mechanism and vitamin D synthesis on the incidence of autoimmune disease. Nat Clin Pract Rheumatol 5(2):99–105
Çamurdan OM, Döğer E, Bideci A, Çelik N, Cinaz P (2012) Vitamin D status in children with Hashimoto thyroiditis. J Pediatr Endocrinol Metab 25(5–6):467–470
Arslan MS, Topaloglu O, Ucan B et al (2015) Isolated vitamin D deficiency is not associated with nonthyroidal illness syndrome, but with thyroid autoimmunity. Sci World J 2015:239815
Brown RS (2009) Autoimmune thyroid disease: unlocking a complex puzzle. Curr Opin Pediatr 21(4):523–528
Hayashi N, Tamaki N, Konishi J et al (1986) Sonography of Hashimoto’s thyroiditis. J Clin Ultrasound 14(2):123–126
Garber JR, Cobin RH, Gharib H et al (2012) American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract 18(6):988–1028
Misra M, Pacaud D, Petryk A et al (2008) Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: a review of current knowledge and recommendations. Pediatrics 122:398–417
Mansournia N, Mansournia MA, Saeedi S et al (2014) The association between serum 25OHD levels and hypothyroid Hashimoto’s thyroiditis. J Endocrinol Invest 37(5):473–476
Sezgin G, Esref OM (2011) Relationship of vitamin D deficiency and autoimmune thyroid diseases. Eur J Internal Med 22:87
Effraimidis G, Badenhoop K, Tijssen JG et al (2012) Vitamin D deficiency is not associated with early stages of thyroid autoimmunity. Eur J Endocrinol 167:43–48
Arabi A, El Rassi R, El-Hajj Fuleihan G (2010) Hypovitaminosis D in developing Countries—prevalence, risk factors and outcomes. Nat Rev Endocrinol 6(10):550–561
Amr N, Hamid A, Sheta M et al (2012) Vitamin D status in healthy Egyptian adolescent girls. Georgian Med News 210:65–71
Lawson DE, Cole TJ, Salem SI et al (1987) Etiology of rickets in Egyptian children. Hum Nutr Clin Nutr 41(3):199–208
Baroncelli GI, Bereket A, El Kholy M et al (2008) Rickets in the Middle East: role of environment and genetic predisposition. J Clin Endocrinol Metab 93(5):1743–1750
Fountoulakis S, Tsatsoulis A (2004) On the pathogenesis of autoimmune thyroid disease: a unifying hypothesis. Clin Endocrinol 60(4):397–409
Kang SW, Kim SH, Lee N (2012) 1, 25-Dihyroxyvitamin D3 promotes FOXP3 expression via binding to vitamin D response elements in its conserved noncoding sequence region. J Immunol 188(11):5276–5282
Cantorna MT, Zhu Y, Froicu M et al (2004) Vitamin D status, 1,25-dihydroxyvitamin D3, and the immune system. Am J Clin Nutr 80:1717S–1720S
Ritterhouse LL, Crowe SR, Niewold TB et al (2011) Vitamin D deficiency is associated with an increased autoimmune response in healthy individuals and in patients with systemic lupus erythematosus. Ann Rheum Dis 70(9):1569–1574
Valdivielso JM, Fernandez E (2006) Vitamin D receptor polymorphisms and diseases. Clin Chim Acta 371(1):1–12
Tamer G, Arik S, Tamer I et al (2011) Relative vitamin D insufficiency in Hashimoto’s thyroiditis. Thyroid 21:891–896
Heaney RP (2014) Toward a physiological referent for the vitamin D requirement. J Endocrinol Invest 37(11):1127–1130
Antico A, Tampoia M, Tozzoli R et al (2012) Can supplementation with vitamin D reduce the risk or modify the course of autoimmune diseases? A systematic review of the literature. Autoimmun Rev 12:127–136
Bellone S, Esposito S, Giglione E et al (2014) Vitamin D levels in a paediatric population of normal weight and obese subjects. J Endocrinol Investig 37(9):805–809
Earthman CP, Beckman LM, Masodkar K et al (2012) The link between obesity and low circulating 25-hydroxy vitamin D concentrations: considerations and implications. Int J Obesity 37:387–396
Grethen E, Hill KM, Jones R et al (2012) Serum leptin, parathyroid hormone, 1,25-dihydroxyvitamin D, fibroblast growth factor 23, bone alkaline phosphatase, and sclerostin relationships in obesity. J Clin Endocrinol Metab 97:1655–1662
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethical approval
The study protocol was approved by the Ethics Committee of the Assiut Children University Hospital, Egypt. The current study was performed according to the Institutional Committee for the Protection of Human Subjects, which was adopted by the 18th World Medical Assembly, Helsinki, Finland and its later amendments.
Informed consent
Written informed consents were obtained from the parents of both patients and controls.
Rights and permissions
About this article
Cite this article
Metwalley, K.A., Farghaly, H.S., Sherief, T. et al. Vitamin D status in children and adolescents with autoimmune thyroiditis. J Endocrinol Invest 39, 793–797 (2016). https://doi.org/10.1007/s40618-016-0432-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0432-x