Abstract
Background
Hyperhomocysteinemia and vitamin B12 deficiency may be involved in the development of diabetic peripheral neuropathy (DPN). Metformin therapy may reduce vitamin B12 plasma levels, thus contributing to DPN.
Aim and methods
The purposes of this cross-sectional study were to assess (1) the potential associations of DPN with serum levels of homocysteine (tHcy), B-vitamins, and/or the common methylenetetrahydrofolate reductase (MTHFR) C677T mutation; (2) the influence of chronic treatment with metformin on tHcy and B-vitamins concentrations and, finally, (3) to evaluate whether, by this influence, metformin is a risk factor for DPN in a group of type 2 diabetic outpatients.
Results
Our data showed that fasting tHcy, folate, and vitamin B12 levels and the MTHFR C677T genotype distribution were comparable between subjects with (n = 79, 30 %) and without DPN (n = 184, 70 %). Metformin-treated subjects (n = 124, 47 %) showed significantly lower levels of vitamin B12 (P < 0.001), but the prevalence of DPN was not different when compared to those not treated with this drug (33 vs. 27 %, P = NS). At univariate regression analysis, DPN was associated with age, duration of diabetes, HbA1c, creatinine levels, and the presence of coronary heart disease (CHD), and negatively with HDL-C concentrations (P < 0.05 all), but at multivariate regression analysis, high creatinine levels (P = 0.06), low HDL-C levels (P = 0.013), and a higher prevalence of CHD (P = 0.001) were the only variables independently associated with DPN in this population.
Conclusions
In conclusion, in these type 2 diabetic outpatients circulating levels of tHcy, folate, and the MTHFR C677T mutation are not associated with DPN, which was predicted by creatinine levels, CHD, and dyslipidemia. Metformin therapy is associated with a mild vitamin B12 level reduction, but not with DPN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic peripheral neuropathy (DPN) is a very common and clinically relevant diabetic complication. In an Italian multicenter study conducted on 8757 patients with type 2 diabetes, the prevalence of DPN was 32.3 %, and its severity increased with aging and duration of diabetes [1]. Distal symmetric polyneuropathy is characterized by sensory and/or motor dysfunctions with a typical symmetrical distribution, and it represents the most frequent clinical form of DPN, affecting more than 90 % of patients with neuropathy [2].
Although chronic hyperglycemia is certainly the major determinant of DPN, several lines of evidence indicate that other nutritional, lifestyle, metabolic, and/or genetic factors may contribute to its occurrence.
In the last two decades, a number of studies have investigated the role of moderate hyperhomocysteinemia as an independent risk factor for both macro- and microvascular diabetic complications, including DPN [3, 4].
It has been shown that elevated levels of total homocysteine (tHcy) significantly correlated with DPN, independent of other risk factors [5–9]. In a cohort of patients with type 2 diabetes, a 23 % increase in the risk of DPN for every increase of 1 μmol of tHcy was demonstrated [6]. Similar results were reported in a Chinese population of 249 diabetic patients with DPN [7], and in the appropriate blood pressure control in diabetes (ABCD) trial [8].
Circulating levels of tHcy are finely regulated by vitamin B12 and folate plasma concentrations, as well as by the common C677T genetic variant in methylenetetrahydrofolate reductase (MTHFR) gene, both in the general [10] and in the diabetic population [11]. Hyperhomocysteinemia may be associated with DPN both directly or as an early marker of B-vitamins deficiency. Thus, folate deficit is involved in neural tube defects [12] and vitamin B12 contributes in the development and maintenance of the neural tube and axonal branching [13]. Furthermore, the role of vitamin B12 deficiency in the development of DPN is supported by several intervention studies demonstrating a beneficial effect of treatment with B-vitamins in DPN [14–18]. Also MTHFR mutation has been associated with a higher DPN risk [19, 20]. In contrast, other Authors have not observed any relationship of MTHFR mutation and/or B-vitamins deficiency with DPN [21].
It is well known that metformin treatment can be associated with a reduction in vitamin B12 levels, as well as with high levels of methylmalonic acid (MMA) and hyperhomocysteinemia [17, 22–25].
Since metformin is the first-line therapy in the management of type 2 diabetes, it is important to ascertain whether this drug is associated with an increased risk of DPN, which could be mediated by the modulation of tHcy, folate, and vitamin B12 levels.
Accordingly, the purposes of this study were (1) to assess the potential associations of DPN with serum levels of homocysteine, vitamin B12, folate, and the common MTHFR C677T polymorphism, (2) to explore the influence of chronic treatment with metformin on homocysteine, vitamin B12, and folate levels, and finally, (3) to evaluate whether, by this influence, metformin is a risk factor for DPN in a group of type 2 diabetic outpatients.
Patients and methods
Patients
This cross-sectional study was conducted in the diabetic outpatient clinic of the Department of Clinical and Experimental Medicine of the University Hospital of Messina and it involved 263 type 2 diabetic subjects who consecutively underwent a specific screening for DPN in the 3 months prior to the study. All subjects were prescribed a low-fat and low-glycemic index diet according to current guidelines [2] and they underwent to regular counseling about dietary habits.
All subjects were on stable hypoglycemic therapy, including metformin, for more than 6 months.
Patients were classified as non-smokers or current smokers, including among the latter those who had quit for less than a year.
Exclusion criteria included: type 1 diabetes, gestational diabetes or other forms of diabetes, pregnancy, active cancer, chronic inflammatory diseases, thyroid diseases, chronic renal failure, nutritional deficiencies, and neurological disorders potentially associated with neuropathic signs and/or symptoms. Subjects who referred a daily intake of alcohol >30 g for men, and >20 g for women were also excluded. Furthermore, pernicious anemia was excluded on the basis of complete blood count (CBC), which is performed as a part of routine laboratory testing at least once a year in the management of all type 2 diabetic outpatients. All subjects with abnormal CBC values are usually addressed to hematological specialist’s appointment and, eventually, second-level blood exams, including the dosage of anti-gastric mucosa Ab.
All study participants gave their written informed consent and the study was approved by the local Ethical Committee (Comitato Etico Interaziendale della Provincia di Messina).
Methods
Clinical and lifestyle information were collected by a standardized questionnaire. Blood pressure, body mass index (BMI), and waist circumference were measured by standard methods.
In all subjects, blood pressure was measured two times in the seated position after 5 min of rest and mean systolic and diastolic pressure values were recorded. Participants were classified as having hypertension if they reported the use of antihypertensive medications or presented blood pressure levels ≥140 mmHg of systolic blood pressure or ≥90 mmHg of diastolic blood pressure [26]. Dyslipidemia was defined as self-reported treatment with lipid‐lowering medications or having LDL cholesterol levels ≥100 mg/dl, or triglycerides levels >150 mg/dl, or HDL‐C <50 mg/dl in women or <40 mg/dl in men [2].
All participants underwent venipuncture after 12–14 h of fasting for laboratory examination. Glucose and creatinine levels and lipid concentrations were measured with standard automated laboratory methods (Roche Diagnostics, Milan, Italy). Glycated hemoglobin (HbA1c) was measured using an automated high-performance liquid chromatography (HPLC) analyzer (Diamat; Bio-Rad Laboratories, Milan, Italy). LDL cholesterol was calculated using the Friedewald formula [27]. Fasting tHcy plasma concentration was measured by HPLC and fluorimetric detection (Bio-Rad Laboratories, Milan, Italy); the coefficient of variation (CV) of the assay was 2.9 % and the normal laboratory range 5–15 μmol/l. Plasma folate and vitamin B12 concentrations were measured by radioassay (Bio-Rad Laboratories, Milan, Italy); CVs were 3.8 and 5.9 %, respectively.
Definition and diagnosis of diabetic neuropathy (DPN)
All study participants were screened for the presence of DPN in the 3 months prior to recruitment [2, 28]. At the screening visit, DPN was suspected based on the abnormalities of at least one of the following evaluations: accurate foot examination (deformities, dry skin, calluses, muscle wasting, hypertrophic nails, onychomycosis, infection, and cracks), pulse palpation of the dorsalis pedis artery, assessment of Achilles tendon reflex and pressure sensitivity (using Semmes–Weinstein monofilament 10 g), vibratory sensibility (by diapason calibrated to 128 Hz), discrimination (via pin prick on the dorsum of the foot), and tactile sensitivity (by staple cotton applied to the dorsum of the foot). DPN diagnosis was then confirmed by the measurement of conduction velocities of ulnar (motor and sensory), tibial, peroneal, performed by a neurologist.
Definition of other chronic complications
Diabetic micro- and macroangiopathy were screened according to the current Guidelines [2]. Retinopathy was diagnosed or excluded on the basis of a direct ophthalmoscopy (through a dilated pupil) performed by an expert ophthalmologist and/or by fluorescein angiography within 1 year before the start of the study.
Renal function was evaluated by measuring serum creatinine and calculating estimated glomerular filtration rate (eGFR) by the modification of diet in renal disease (MDRD) equation [29]. Microalbuminuria evaluation was available only in a subset of patients and it was therefore not included in the present analysis.
Coronary heart disease (CHD) was defined on the basis of cardiologist medical records and/or hospital discharge as a history of myocardial infarction, coronary artery bypass graft surgery, or coronary angioplasty. As part of the clinical screening, all patients also underwent a standard electrocardiogram evaluation in the 12 months prior to the study, to exclude asymptomatic myocardial infarction or arrhythmia.
Genetic analysis
Genomic DNA extraction was carried out on whole blood using QIAamp DNA blood Midi kits (Qiagen, Hilden, Germany) according to the manufacturer’s recommended protocol. MTHFR C677T genotyping was performed in all patients as previously described [11]. Briefly, a fragment of 198 bp in the MTHFR gene was amplified by polymerase chain reaction (PCR) using oligonucleotide primers. The PCR products were subjected to restriction enzyme analysis by digestion with HinfI (MspI, MBI Fermentas, Lithuania), and the fragments were separated by electrophoresis on agarose gel, and visualized by UV illumination, after ethidium bromide staining. The resulting fragments were 175 and 23 bp for the mutant T allele and 198 bp for the uncut wild-type C allele.
Statistical analysis
Statistical analysis was performed using SPSS 11.0 for Window package.
Preliminarily, the sample size calculation established a minimum number of 250 subjects to be enrolled in our study as necessary to guarantee a significance level alpha = 0.05.
Numerical data are expressed as mean ± standard deviation (SD) and categorical variables as number and percentage (%). Since the majority of the examined variables showed a normal distribution, as verified by Kolmogorov–Smirnov test, a parametric approach has been used. For each parameter the two-tailed Student’s t test was performed for statistical comparisons; in order to compare numerical variables, the χ 2 test or by Fisher’ s exact test was applied, as appropriate. To compare subjects with and without DPN, Chi-square test (χ 2) for categorical measures was used. In order to assess variables independently associated with DPN, a multivariate logistic regression analysis was performed, including in the model all variables that resulted significant at univariate regression analysis (age, diabetes duration, levels of HbA1c, HDL-C, creatinine, and the presence of CHD). Furthermore, a multivariate regression analysis including all study variables in the model was also performed, but because of multicollinearity, no independent correlations were identified.
Odds ratio and 95 % confidence intervals were calculated by exponentiation of logistic regression coefficients. To compare continuous variables ANOVA was used. All statistical comparisons were two-tailed, and a P value <0.05 was considered statistically significant.
Results
Clinical characteristics of the study population
The clinical characteristics of 263 type 2 diabetic outpatients participating in the study are shown in Table 1.
Study subjects (151 women and 112 men) had a mean age of 64 years (range 32–86 years) and a mean diabetes duration of 12 years (range 1–46 years). Overall, they were overweight (mean BMI 29 kg/m2, waist circumference 99 cm), with a HbA1c mean value of 7.4 % (57 mmol/mol) and a lipid profile characterized by values of LDL cholesterol (LDL-C) which were, on average, higher than those recommended for diabetic patients (mean LDL-C 129 mg/dl); the values of HDL cholesterol (HDL-C) and plasma triglycerides were within the recommended levels.
Creatinine values were within the normal range, with an eGFR of 77 mL/min/1.73 m2.
Plasma levels of tHcy (13.2 µol/l), folate (4.4 pg/ml), and vitamin B12 (605.6 pg/ml) were within the normal laboratory range, although a moderate hyperhomocysteinemia, as indicated by plasma levels of tHcy ≥ 15 µol/l, was detected in 63 subjects (24 %).
With regard to the treatment of diabetes, 47 % of subjects were treated with metformin (monotherapy or in combination with other hypoglycemic drugs), 55 % with sulfonylureas or repaglinide, 17 % with insulin (alone or in combination with oral hypoglycemic agents), and one subject was treated with glitazones.
Overall, 160 (61 %) study participants had hypertension on pharmacological treatment, and 99 (38 %) were affected by dyslipidemia (61 subjects treated with statins and 9 with fibrates).
Screening of chronic diabetic complications detected 79 subjects (30 %) with DPN, 82 subjects (31 %) with diabetic retinopathy, and 26 (10 %) with documented coronary heart disease (CHD).
Fasting tHcy and B-vitamins plasma levels according to MTHFR C677T genotype distribution
The distribution of MTHFR C677T polymorphism did not differ from the frequencies predicted by the Hardy–Weinberg equilibrium (P = NS), with a TT homozygous prevalence of 24.3 % (Table 2).
Fasting tHcy plasma levels were significantly higher (15.2 ± 8.4 vs 12.2 ± 3.6 μmol/l, P = 0.005) and folate levels were lower (3.9 ± 2.3 vs 4.8 ± 3.5 pg/ml, P = 0.066) in TT subjects as compared to CC subjects, whereas no difference in vitamin B12 concentrations was noted according to genotype (Table 2).
Clinical characteristics of the study population according to the presence of DPN
As shown in Table 3, subjects with DPN (n = 79) were in prevalence men (P = 0.023), older (P = 0.047), with a longer duration of diabetes (P = 0.027); they also showed higher levels of HbA1c (P = 0.017), creatinine (P < 0.001), and lower values of HDL-C (P = 0.027). Moreover, in the group with DPN the use of insulin was more frequent (P = 0.005) and CHD prevalence (P < 0.001) was higher.
Fasting tHcy and B-vitamins levels were not significantly different in subjects with and without DPN; also the percentage of subjects with the MTHFR mutation (T carriers) was similar in the two groups (66 vs. 72 %, P = NS) (Table 3).
Since age and diabetes duration were significantly different in subjects with and without DPN, an analysis adjusted for these two variables was also performed. However, as shown in Table 3, this adjustment did not change the trend of our results.
Fasting tHcy and B-vitamins levels and DNP prevalence according to treatment with metformin
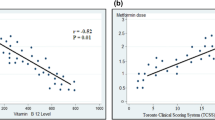
The distribution of subjects with or without DPN according to metformin therapy is shown in Fig. 1. The percentage of subjects with DPN was 33 % in the group treated with metformin and 27 % in the not-treated group, and this difference was not statistically significant.
The potential influence of metformin on major study variables is shown in Table 4. Study subjects treated with metformin (either alone or in combination with other hypoglycemic drugs) were younger (P < 0.001) and less frequently male (P = 0.05) compared with those not taking the drug. Fasting vitamin B12 levels were significantly lower in metformin-treated patients (P = 0.001), while there were no significant differences in the plasma levels of tHcy and folate levels and the prevalence of moderate hyperhomocysteinemia between the two groups.
Factors associated with DPN at univariate and multivariate regression analyses
At univariate regression analysis (Table 5), DPN was positively associated with age (P = 0.048), duration of diabetes (P = 0.029), HbA1c (P = 0.019), creatinine levels (P = 0.001), and the presence of CHD (P < 0.001) and negatively with HDL-C concentrations (P = 0.028).
At multivariate regression analysis, performed including all variables in the model that resulted significant at univariate regression analysis (age, diabetes duration, levels of HbA1c, HDL-C, creatinine, and the presence of CHD), higher creatinine levels (P = 0.06) and low plasma levels of HDL-C levels (P = 0.013) and the presence of CHD (P = 0.001) were the only factors that were associated with DPN (Table 5).
A multivariate regression analysis including all the study variables in the model was also performed, although no independent correlations with DPN were identified because of multicollinearity among the variables (data not shown).
Discussion
Type 2 diabetes is associated with microvascular complications that contribute to its increased morbidity and mortality risk, including DPN. In our study, DPN was diagnosed in 30 % of subjects undergoing clinical screening, in line with the prevalence previously reported in a large Italian cohort [1].
Beyond the undisputed role of chronic hyperglycemia in the pathogenesis of this debilitating complication, other factors could contribute to its incidence and/or progression. Among these, several data suggest the potential role of mild hyperhomocysteinemia, MTHFR C677T mutation, and/or vitamin B12 deficiency [5–9, 14–20].
We therefore evaluated the relationships between these variables and DPN in a group of type 2 diabetic outpatients, assessing the potential influence of metformin therapy.
In our cohort, fasting tHcy, vitamin B12, and folate levels were generally within the normal range and comparable between subjects with and without DPN.
Studies conducted to date have not provided unequivocal results about the association of hyperhomocysteinemia and/or its common genetic and vitamin determinants with several long-term diabetic complications, including DPN. However, these observations are still very sparse and inconclusive. In line with some of these studies [11, 21, 30], our results do not support a significant role of hyperhomocysteinemia or MTHFR mutation on the development of DPN, since in our cohort, tHcy levels and MTHFR genotype distribution were comparable between subjects with or without DNP.
According to these results, it seems that hyperhomocysteinemia does not have a causal role on DPN, but it may rather be a surrogate marker for vitamin B12 deficiency. It is well known that chronic vitamin B12 deficiency is associated with pernicious anemia and several neurological deficits and, consequently, it could also be involved in the development of DPN. Furthermore, the hypothesis that low levels of vitamin B12 are a risk factor for DPN is supported by several observations, including a limited number of intervention studies. Thus, in a population of type 2 diabetic subjects with DPN, the administration of methylcobalamin, the active form of vitamin B12, together with folate and pyridoxal 5′-phosphate reduced the frequency and intensity of symptoms and improved the density of epidermal nerve fibers in calf muscle biopsies [14]. Furthermore, in 20 type 2 diabetic patients with DPN, treatment with the same micronutrients for 1 year significantly improved the loss of skin sensitivity [15], and in another small group of patients supplemented for 4 months with multivitamins including vitamin B12, a significant improvement in the symptoms of neuropathy was observed [16].
Although all our study subjects were regularly counseled on diet according to current diabetes guidelines [2], dietary information was not available for this analysis. Since the mean age of our participants was >60 years, we cannot rule out that an age-related impairment of nutrition may have influenced vitamin levels, as reported in elderly subjects [31].
However, subjects recruited in our study had vitamin B12 levels within the normal laboratory range and comparable to those reported in other studies of the same background [10, 11, 17]. Furthermore, in order to limit our observation to subjects commonly attending diabetes outpatient clinics, vitamin B 12 deficiency-associated conditions, such as alcohol abuse or pernicious anemia, were carefully excluded in our study.
Beyond the nutritional or age-related causes of vitamin B12 deficit, other factors, such as hypoglycemic therapies, may impair vitamin B levels in diabetic subjects. The potential deleterious effects of vitamin B12 deficiency on DPN occurrence has attracted clinicians’ attention after noticing that the most widely used drug for the treatment of diabetes, i.e., metformin, may also reduce vitamin B12 levels [25, 32]. In line with other reports [24, 25, 32–34], our study confirmed that metformin treatment is associated with a reduction of vitamin B12 serum concentration, although in our population this reduction was mild and still within the reference range. The proposed mechanisms include alterations in small bowel motility and bacterial overgrowth, the competitive inhibitions in intrinsic factor levels, and interaction with the cubilin endocytic receptor [35]; metformin has also been shown to inhibit the calcium-dependent adsorption of the vitamin B12-IF complex at the terminal ileum [36].
Despite this effect on vitamin B12, treatment with metformin had no clinical consequences on DPN risk in our study subjects, accordingly to what reported by some Authors [32]; on the contrary, others have observed a dose-dependent DPN risk associated with this drug [34].
Notably, patients enrolled in our study were on stable hypoglycemic therapy and they were treated with metformin for more than 6 months at the maximum tolerated dosage, with 80 % of them taking ≥2 g/day (data not shown). Despite this relatively long treatment with therapeutic dosage of metformin, vitamin B12 levels were overall in the normal range, with only 20 % of subjects showing levels <300 pg/ml, suggesting that at least in a population of Mediterranean origin, like ours, the nutritional intake of B-vitamins is adequate and overcomes the effect of the drug.
Taken together, our data indicate that hyperhomocysteinemia, MTHFR mutation, and B-vitamin deficiency are not major risk factors for the development of neuropathic damage. Conversely, age, duration of diabetes, and HbA1c levels were positively associated with DPN in our population, thus confirming the role of glycemic control in its pathogenesis [37]. However, HDL-C, CHD, and creatinine levels, were the only factors independently associated with DPN at multivariate regression analysis, although with different degrees of significance.
The clinical meaning of the association of higher creatinine levels with DPN occurrence, also reported in other studies [38, 39], may be related to the concomitant presence of different microangiopathic complications in the same patients. However, retinopathy did not show the same trend, suggesting that beyond chronic hyperglycemia, nephropathy, and neuropathy may share the same underlying risk factors, for example low HDL-C levels.
Although still limited, the number of observations supporting the role of diabetic dyslipidemia, i.e., hypertriglyceridemia, higher sdLDL concentrations, and low HDL-C levels, in diabetic microangiopaty is increasing. Some Authors have reported that diabetic dyslipidemia including low HDL-C levels correlated with DPN and was an independent risk factor for its development [40–42]. Furthermore, several clinical studies have associated poor lipid profile with DPN development and progression, independent of glycemic control [43, 44].
The mechanisms by which circulating lipid levels may contribute to pathogenesis of DPN are still unknown, although several hypotheses have been proposed, including underlying insulin resistance or the generation of oxidized LDL particles induced by low HDL-C levels [42, 45, 46]. All these clinical and experimental evidences support an important role of diabetic dyslipidemia also on microvascular complications and in particular on DPN, and our results demonstrating that low HDL-C levels are an independent risk factor for DPN are well in line with this hypothesis.
Furthermore, our data show an association between CHD occurrence and DPN. This association between macro- and microvascular complications can be interpreted in the view of common risk factors, such as endothelial dysfunction, oxidative stress, and/or subclinical inflammation that may be elicited by high glucose or lipid levels in these patients. On the other hand, in non-diabetic subjects, neuropathy has been also associated with vascular factors such age, waist circumference, comorbidities, and peripheral arterial disease [47], and this could easily apply also to our diabetic patients.
Our study has some limitations, firstly related to its cross-sectional design, that does not allow us to fully explore the potential temporal and causal relationships between metformin treatment, vitamin B12 deficiency, and the onset of DPN. Furthermore, the sample size is relatively small, although the number of subjects included in our analysis was sufficient to detect meaningful differences. Moreover, our sample size was larger than that reported in the other few studies measuring vitamin B levels in addition to genotype analysis [19–21] and, unfortunately, in none of them metformin treatment was taken into account.
Also the specialty-based setting (tertiary referral center of diabetes) does not allow us to generalize our findings to all the people with type 2 diabetes. Finally, microalbuminuria evaluation was not included in the present analysis since it was available only in a subset of patients.
In conclusion, our results indicate that the presence of CHD and low levels of HDL-C, and to a lower extent higher creatinine concentrations are independently associated with DPN, while tHcy, folate, and vitamin B12 plasma levels and the common MTHFR C677T mutation do not play a significant role, even in metformin-treated subjects. Larger studies are needed to confirm the utility of treating diabetic dyslipidemia, and particularly low levels of HDL-C, in order to reduce not only the cardiovascular but also the neuropathic risk in diabetic subjects.
References
Fedele D, Comi G, Coscelli C, Cucinotta D, Feldman EL, Ghirlanda G et al (1997) A multicenter study on the prevalence of diabetic neuropathy in Italy. Italian Diabetic Neuropathy Committee. Diabetes Care 20:836–843
American Diabetes Association (2014) Standards of medical care in diabetes 2014. Diabetes Care 37(Supplement):1
Russo GT, Cucinotta D (2003) Hyperhomocysteinemia and cardiovascular risk in diabetes mellitus. Ann Ist Super Sanita 39:153–163
Audelin MC, Genest J Jr (2001) Homocysteine and cardiovascular disease in diabetes mellitus. Atherosclerosis 159:497–511
Molina M, Gonzalez R, Folgado J, Real JT, Martínez-Hervás S, Priego A et al (2013) Correlation between plasma concentrations of homocysteine and diabetic polyneuropathy evaluated with the Semmes–Weinstein monofilament test in patients with type 2 diabetes mellitus. Med Clin (Barc) 141:382–386
González R, Pedro T, Martinez-Hervas S, Civera M, Antonia Priego M, Catalá M et al (2012) Plasma homocysteine levels are independently associated with the severity of peripheral polyneuropathy in type 2 diabetic subjects. J Peripher Nerv Syst 17:191–196
Li JB, Cheng YZ, Shi M, Zhang HM, Dai Q, Zhang Y et al (2011) The relationship between plasma homocysteine levels and diabetic peripheral neuropathy. Zhonghua Nei Ke Za Zhi 50:14–17
Stablerr SP, Estacio R, Jeffers BW, Cohen JA, Allen RH, Schrier RW (1999) Total homocysteine is associated with nephropathy in non-insulin-dependent diabetes mellitus. Metabolism 48:1096–1101
Cohen JA, Jeffers BW, Stabler S, Schrier RW, Estascio R (2001) Increasing homocysteine levels and diabetic autonomic neuropathy. Auton Neurosci 87:268–273
Russo GT, Friso S, Jacques PF, Rogers G, Cucinotta D, Wilson PW et al (2003) Framingham Offspring Study Cohort. Age and gender affect the relation between methylenetetrahydrofolate reductase C677T genotype and fasting plasma homocysteine concentrations in the Framingham Offspring Study Cohort. J Nutr 133:3416–3421
Russo GT, Di Benedetto A, Giorda C, Alessi E, Crisafulli G, Ientile R et al (2004) Correlates of total homocysteine plasma concentration in type 2 diabetes. Eur J Clin Invest 34:197–204
Choi JH, Yates Z, Veysey M, Heo YR, Lucock M (2014) Contemporary issues surrounding folic acid fortification initiatives. Prev Nutr Food Sci 19:247–260
Moore E, Mander A, Ames D, Carne R, Sanders K, Watters D (2012) Cognitive impairment and vitamin B12: a review. Int Psychogeriatr 6:1–16
Jacobs AM, Cheng D (2011) Management of diabetic small-fiber neuropathy with combination l-methylfolate, methylcobalamin, and pyridoxal 5′-phosphate. Rev Neurol Dis 8:39–47
Walker MJ Jr, Morris LM, Cheng D (2010) Improvement of cutaneous sensitivity in diabetic peripheral neuropathy with combination l-methylfolate, methylcobalamin, and pyridoxal 5′-phosphate. Rev Neurol Dis 7:132–139
Farvid MS, Homayouni F, Amiri Z, Adelmanesh F (2011) Improving neuropathy scores in type 2 diabetic patients using micronutrients supplementation. Diabetes Res Clin Pract 93:86–94
Wile DJ, Toth C (2010) Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 33:156–161
Xu Q, Pan J, Yu J, Liu X, Liu L, Zuo X et al (2013) A Meta-analysis of methylcobalamin alone and in combination with lipoic acid in patients with diabetic peripheral neuropathy. Diabetes Res Clin Pract 101:99–105
Yigit S, Karakus N, Inanir A (2013) Association of MTHFR gene C677T mutation with diabetic peripheral neuropathy and diabetic retinopathy. Mol Vis 19:1626–1630
Wu S, Han Y, Hu Q, Zhang XJ, Cui GC, Li ZZ, Guan YT (2014) Effects of common polymorphisms in the MTHFR and ACE genes on diabetic peripheral neuropathy progression: a meta-analysis. Mol Neurobiol (Epub ahead of print)
Buysschaert M, Dramais A-S, Wallemacq PE, Hermans M (2000) Hyperhomocysteinemia in type 2 diabetes. Diabetes Care 23:1816–1822
Carlsen SM, Folling I, Grill V, Bjerve KS (1997) Metformin increases total serum homocysteine level in non-diabetic male patients with coronary heart disease. Scand J Clin Lab Invest 57:521
Aarsand AK, Carlsen SM (1998) Folate administration reduced circulating homocysteine levels in NIDDM patients on longterm metformin treatment. J Int Med 244:169
Beulens JW, Hart HE, Kuijs R, Kooijman-Buiting AM, Rutten GE (2015) Influence of duration and dose of metformin on cobalamin deficiency in type 2 diabetes patients using metformin. Acta Diabetol 52:47–53
Niafar M, Hai F, Porhomayon J, Nader ND (2015) The role of metformin on vitamin B12 deficiency: a meta-analysis review. Intern Emerg Med 10:93–102
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Joseph L et al (2003) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of high blood pressure: the JNC 7 report. JAMA 289:2560–2572
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Dyck PJ, Albers JW, Andersen H, Arezzo JC, Biessels GJ, Bril V, Feldman EL, Litchy WJ, O’Brien PC, Russell JW, Toronto Expert Panel on Diabetic Neuropathy (2011) Diabetic polyneuropathies: update on research definition, diagnostic criteria and estimation of severity. Diabetes Metab Res Rev 27:620–628
Levey A, Bosch J, Breyer Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine. Ann Intern Med 139:461–470
de Groot-Kamphuis DM, van Dijk PR, Groenier KH, Houweling ST, Bilo HJ, Kleefstra N (2013) Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med 71:386–390
Tucker KL, Mahnken B, Wilson PW, Jacques P, Selhub J (1996) Folic acid fortification of the food supply. Potential benefits and risks for the elderly population. JAMA 276:1879–1885 [Erratum in: JAMA 1997;277:714]
Liu Q, Li S, Quan H, Li J (2014) Vitamin B12 status in metformin treated patients: systematic review. PLoS One 9:e100379
Singh AK, Kumar A, Karmakar D, Jha RK (2013) Association of B12 deficiency and clinical neuropathy with metformin use in type 2 diabetes patients. J Postgrad Med 59:253–257
Sato Y, Ouchi K, Funase Y, Yamauchi K, Aizawa T (2013) Relationship between metformin use, vitamin B12 deficiency, hyperhomocysteinemia and vascular complications in patients with type 2 diabetes. Endocr J 60:1275–1280
Andrès E, Noel E, Goichot B (2002) Metformin-associated vitamin B12 deficiency. Arch Intern Med 162:2251–2252
Bauman WA, Shaw S, Jayatilleke E, Spungen AM, Herbert V (2000) Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care 23:1227–1231
UK Prospective Diabetes Study (UKPDS) Group (2002) Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33. Lancet 352:837–853
Wang DD, Bakhotmah BA, Hu FB, Alzahrani HA (2014) Prevalence and correlates of diabetic peripheral neuropathy in a Saudi Arabic population: a cross-sectional study. PLoS One 9:e106935
Hu Y, Liu F, Shen J, Zeng H, Li L, Zhao J et al (2014) Association between serum cystatin C and diabetic peripheral neuropathy: a cross-sectional study of a Chinese type 2 diabetic population. Eur J Endocrinol 171:641–648
Wiggin TD, Sullivan KA, Pop-Busui R, Amato A, Sima AA, Feldman EL (2009) Elevated triglycerides correlate with progression of diabetic neuropathy. Diabetes 58:1634–1640
Ansquer JC, Foucher C, Aubonnet P, Le Malicot K (2009) Fibrates and microvascular complications in diabetes–insight from the FIELD study. Curr Pharm Des 15:537–552
Vincent AM, Hinder LM, Pop-Busui R, Feldman EL (2009) Hyperlipidemia: a new therapeutic target for diabetic neuropathy. J Peripher Nerv Syst 14:257–267
Leiter LA (2005) The prevention of diabetic microvascular complications of diabetes: is there a role for lipid lowering? Diabetes Res Clin Pract 68(Suppl 2):S3–S14
Wiggin TD, Sullivan KA, Pop-Busui R, Amato A, Sima AA, Feldman EL (2009) Elevated triglycerides correlate with progression of diabetic neuropathy. Diabetes 58:1634–1640
Xie F, Fu H, Hou JF, Jiao K, Costigan M, Chen J (2013) High energy diets-induced metabolic and prediabetic painful polyneuropathy in rats. PLoS One 8:e57427
Obrosova IG, Ilnytska O, Lyzogubov VV, Pavlov IA, Mashtalir N, Nadler JL et al (2007) High-fat diet induced neuropathy of pre-diabetes and obesity: effects of “healthy” diet and aldose reductase inhibition. Diabetes 56:2598–2608
Baldereschi M, Inzitari M, Di Carlo A, Bovis F, Maggi S, Capurso A, ILSA Working Group et al (2013) Vascular factors predict polyneuropathy in a non-diabetic elderly population. Neurol Sci 34:955–962
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Russo, G.T., Giandalia, A., Romeo, E.L. et al. Diabetic neuropathy is not associated with homocysteine, folate, vitamin B12 levels, and MTHFR C677T mutation in type 2 diabetic outpatients taking metformin. J Endocrinol Invest 39, 305–314 (2016). https://doi.org/10.1007/s40618-015-0365-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0365-9