Abstract
Background/aim
To study the characteristics of interleukin 6 (IL6), soluble form of interleukin 6 receptor (sILR)/IL6 complex in obese children and adolescents and its relationship with insulin resistance (IR).
Subjects and methods
66 obese children and adolescents [34 boys, mean age 10.3 ± 2.9 years, z-score of body mass index (BMI) 4.76 ± 1.36] and 24 non-obese healthy sex- and age-matched controls. Fasting levels of glucose, insulin, IL6, sIL6, sgp130 were measured. IR was assessed by homeostasis model assessment of IR (HOMA-IR).
Results
Obese subjects showed increased levels of insulin and IL-6 and higher HOMA-IR compared to controls (117.67 ± 50.9 vs. 62.42 ± 29.4 pmol/L, 2.73 ± 0.98 vs. 1.07 ± 0.41 pg/ml and 4.03 ± 2.16 vs. 1.83 ± 1.05 for insulin, IL-6 and HOMA-IR, respectively, p < 0.01 in all cases). sIL-6R levels were significantly lower in obese subjects (34.7 ± 14.2 vs. 55.6 ± 15.2 ng/ml in controls, p = 0.005), whereas sgp130 levels were not significantly different. In obese subjects, IL-6 directly correlated with z-score BMI (r = 0.481, p = 0.009) and with waist-to-height ratio (r = 0.494, p = 0.007), while sIL6-R was inversely related to HOMA-IR (r = −0.522, p = 0.002). Insulin resistant subjects showed higher levels of IL6 and lower levels of sIL6R (3.31 ± 0.72 vs. 2.25 ± 0.64 pg/ml, p = 0.020 and 25.3 ± 9.3 vs. 42.5 ± 10.4 ng/ml, p = 0.013, respectively).
Conclusions
In obese children and adolescents, IR is associated with elevated levels of IL-6 and diminished values of sIL-6R.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood obesity has become an ever-increasing problem and is now considered a disease of epidemic proportions. There is substantial evidence that obesity in childhood lays the metabolic groundwork for adult type 2 diabetes, metabolic syndrome, and cardiovascular disease [1, 2].
Some experimental and clinical studies have demonstrated that interleukin-6 (IL-6) concentrations increase with weight gain and are associated with the development of type 2 diabetes and insulin resistance (IR) [3, 4].
IL-6 is an immunomodulatory cytokine belonging to the family of four helical cytokines and shows potent proinflammatory and endocrine actions. On target cells, this cytokine interacts with its receptor complex, which consists of the IL-6 receptor (IL-6R) and two molecules of gp130 and leads to the initiation of intracellular signaling. While gp130 is present on most cells of the body, IL-6R is only present on some cells, mainly hepatocytes and several leukocytes. Cells that only express gp130 and no IL-6R are refractory to the IL-6 signal [5]. These cells can be stimulated by a complex of IL-6 and the soluble form of IL-6R (sIL-6R) that is generated by proteolytic cleavage of IL-6R at the site adjacent to the transmembrane domain or by differential mRNA splicing. This protein renders cells that only express gp130 responsive towards the cytokine IL-6. The activity of the IL-6/sIL-6R complex is counteracted by the presence of a soluble form of gp130—sgp130—which tightly regulates the activity of the IL-6/sIL-6R complex. This pathway has been termed “transsignalling” [6]. It has been suggested that IL-6 exerts its anti-inflammatory actions via traditional signaling, whereas the proinflammatory effects, such as recruitment of mononuclear cells, are triggered through transsignalling [7].
Considering the prevalent influence of IL-6 in the pathogenesis of IR in obese subjects, we decided to evaluate all components of IL-6 biological systems, including sIL-6R and sgp130, in a group of obese children and adolescents. To the best of our knowledge, these parameters have been evaluated in few studies concerning adults [8].
Subjects and methods
Patients
A total of 125 consecutive obese patients (z-score of BMI >2) [9] belonging to an outpatient clinic for severe obesity of children and adolescents of Rummo Hospital (Benevento, Italy) were proposed to enter the study. Among 96 patients retained after considering selection criteria (see below), 66 accepted to participate to the study (34 boys and 32 girls of Caucasian Italian descent, mean age 10.3 ± 2.9 years, mean z-score BMI 4.76 ± 1.36, 48 prepubertal). All patients have early-onset obesity (i.e., onset before the physiologic time of “adiposity rebound”, at the age of 6 years). 24 non-obese healthy sex- and age-matched were studied as controls. The latter were recruited among a group of children and adolescents investigated for idiopathic short stature in whom complete diagnostic work-up failed to reveal any organic disease.
Exclusion criteria were the presence of syndromes, anomalous growth pattern suggesting a secondary obesity, diabetes, the use of medication that alters glucose metabolism, familial dyslipidemia and/or incomplete medical data (i.e., absence of auxological data allowing the analysis of growth dynamic). A temporary exclusion criterion was the presence of an underlying illness at the time of the first examination. Subjects with a Tanner stage ≥2 were considered pubertal.
Auxological measurements
All anthropometric measurements were taken by the same well-trained investigator (GDF). Weight was measured to the nearest 0.1 kg with subjects standing barefoot in light clothing. Height was measured to the nearest 1 mm using a portable stadiometer, with the subject upright and the head in the Frankfurt plane. BMI was calculated as weight (kg)/height2 (m2) and expressed as a z-score [10]. Waist circumference (WC) was measured using a tape measure just above the uppermost lateral border of the right ilium at the end of a normal expiration and was recorded to the nearest millimeter, and the waist-to-height ratio (WTHR) (WC in cm/height in cm) was calculated.
The homeostasis model of assessment-insulin resistance (HOMA-IR) index was calculated by the following formula: glucose mmol/l × insulin mUI/l/22.5 [11]. IR was defined on the basis of a HOMA-IR higher than 95th percentile for sex and pubertal stage, according to Italian percentiles [12].
Laboratory procedures and assays
Enrolled subjects in complete well-being were directed to a centralized laboratory to provide blood samples after a 12 h overnight fast for the measurement of glucose, insulin, total cholesterol, triglycerides, high-density lipoprotein cholesterol, IL-6, sIL-6R, and sgp130. Serum samples were separated within 1 h of collection, stored in 1 ml aliquots, and kept frozen at −80 °C. All biochemical parameters were evaluated in duplicate and contextually for patients and controls.
Serum levels of IL-6, sIL-6R, and sgp130 were determined using commercially available ELISA kits (Quantikine, R&D Systems, Minneapolis, USA) having sensitivity of 0.70 pg/ml, 7 and 0.08 ng/ml for IL-6, sIL-6R, and sgp130, respectively. The intra- and inter-assay CVs were <5 % for IL-6 and sgp130 serum levels, and <10 % for sIL-6R serum levels.
Statistical analysis
Results are expressed as mean ± standard deviation for continuous variables and as absolute (percent) values for discrete variables. The unpaired Student’s t test was used for continuous variables to evaluate between-group differences for a given variable. For comparison of discrete variables, the χ 2 or Fisher’s exact test was used. Pearson’s correlation coefficient was used to determine relationships between different parameters. A p value lower than 0.01 was considered significant.
Ethical approval
The study was approved by the local ethical committee of Gaetano Rummo Hospital, Italy. Written parental informed consent and the assent of patients and controls were taken prior to their enrollment into the study.
Results
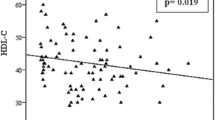
Clinical and biochemical characteristics of patients and controls are detailed in Table 1. As expected, obese subjects showed increased serum levels of insulin and IL-6 and higher HOMA-IR compared to healthy controls (117.67 ± 50.9 vs. 62.42 ± 29.4 pmol/L, 2.73 ± 0.98 vs. 1.07 ± 0.41 pg/mL and 4.03 ± 2.16 vs. 1.83 ± 1.05 for insulin, IL-6 and HOMA-IR, respectively, p < 0.01 in all cases). Moreover, serum levels of sIL-6R were significantly lower in obese patients compared to controls (34.7 ± 14.2 vs. 55.6 ± 15.2 ng/mL, p = 0.005), whereas sgp130 were not significantly different between the two study groups. In obese subjects, IL-6 levels directly correlated with z-score BMI (r = 0.481, p = 0.009; Fig. 1a) and with WTHR (r = 0.494, p = 0.007; Fig. 1b) while sIL6-R serum levels were inversely related to HOMA-IR index (r = −0.522, p = 0.002) (Fig. 2). The analysis after adjustment for age (in the former) and for age and z-score BMI (in the latter) confirmed these relationships, not observed in healthy controls.
When obese subjects were classified as IR (n = 30, 18 females, mean age 10.9 ± 3 years) and not IR (n = 36, 14 female, mean age 9.3 ± 1.6 years), the former showed higher levels of IL6 and lower levels of sIL6R (3.31 ± 0.72 vs. 2.25 ± 0.64 pg/mL, p = 0.020 and 25.3 ± 9.3 vs. 42.5 ± 10.4 ng/ml, p = 0.013 (Fig. 3).
Discussion
Our data demonstrate that a hallmark of IR in pediatric subjects resides in the association between increased levels of IL-6 and reduced levels of sIL-6R, and suggest that these abnormalities precede the onset of overt carbohydrate intolerance in insulin resistant subjects. This observation is not shared by other authors who found elevated levels of IL-6 but also of sIL6-R and gp130 in adult obese patients with metabolic syndrome [7]. One explanation for this discrepancy could be the duration of obesity, which is shorter by definition in our patients, and the raw number of adipocytes secreting IL-6 that is closely associated with obesity and IR [13].
Furthermore, previous reports in the literature evidenced that high levels of sgp130 were associated with hypertriglyceridemia, hypertension and elevated fasting glucose [8]; all findings absent in our cohort.
Adipose tissue IL-6 expression accounts for almost 30 % of systemic IL-6, and circulating IL-6 concentrations are positively correlated with obesity, impaired glucose tolerance, and IR [14].
Plasma IL-6 concentrations predict the development of type 2 diabetes [15], and peripheral administration of IL-6 induces hyperlipidemia, hyperglycemia, and IR in rodents and humans [16, 17].
Some studies have suggested that IL-6 could be involved in IR and its complications [18]. A mechanism of IL-6-induced IR in the liver has been proposed, which involves the activation of STAT3 (signal transducer and activator of transcription 3) and the subsequent induction of a suppressor of SOCS3 (cytokine signaling 3) [19]. Since hepatocytes express IL-6R, the biological actions of IL-6 in these cells were not mediated by sIL-6R. The lower circulating levels of sIL-6R in obese children could reduce the metabolic action of IL-6 in tissues without constitutive expression of IL-6R (i.e., adipose and skeletal muscle) and thus increase the relative availability of IL-6 for cells that constitutively express IL-6R, in particular hepatocytes. In these cells, IL-6 response through the membrane-bound IL-6R is not influenced by the reduced bioavailability of sIL-6R. The inverse relationship between sIL-6R levels and the HOMA-IR index observed in obese children confirms indirectly this hypothesis. However, the reduced serum levels of sIL-6R observed in patients with higher levels of HOMA-IR could be considered a compensatory mechanism, attempting to determine a functional inhibition of this pathway, in order to reduce further IL-6-related systemic damage.
The strengths of the study are the strict selection criteria (permitting to exclude secondary and/or syndromic obesity) and the ethnical homogeneity of the studied population, avoiding confounding factors belonging to inter-ethnic variation in insulin sensitivity.
The major limit of our study is the choice of HOMA-IR and not of the euglycemic clamp to evaluate IR. In the literature, cut-off levels change from 2.5 for adults [20] to 4 for adolescents [21]. A study concerning adolescent patients suggested 3.16 [22]. We have chosen to define IR on the basis of Italian percentiles of HOMA-IR [12]. Furthermore, our data show a correlation with the degree of IR according to HOMA-IR index, independently from the cut-off point. Another limit of the study is the exclusion of a diabetic state on the basis of the medical history and fasting plasma glucose, without performing an oral glucose tolerance test and/or HbA1c dosage. It has to be argued that the young age of our cohort limits the risk of underestimating the diagnosis of diabetes in presence of normal fasting glucose levels.
Conclusions
Our data suggest that in pediatric and adolescent obese patients IR is associated with elevated levels of IL-6 and diminished values of sIL-6R. Over years, this perturbed pattern could precede the impairment of the entire system previously described in adults. Further experimental evidence for the suggested model is needed.
Abbreviations
- BMI:
-
Body mass index
- HOMA-IR:
-
Homeostasis model of assessment-insulin resistance
- IR:
-
Insulin resistance
- IL-6:
-
Interleukin 6
- IL-6R:
-
Interleukin 6 receptor
- sIL-6R:
-
Soluble form of interleukin 6 receptor
References
Weiss R, Dziura J, Burgert TS et al (2004) Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350:2362–2374
Viggiano D, De Filippo G, Rendina D et al (2009) Screening of metabolic syndrome in obese children: a primary care concern. J Pediatr Gastroenterol Nutr 49:329–334
Senn JJ, Klover PJ, Nowak IA, Mooney RA (2002) Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes 51:3391–3399
Galcheva SV, Iotova VM, Yotov YT, Bernasconi S, Street ME (2011) Circulating proinflammatory peptides related to abdominal adiposity and cardiometabolic risk factors in healthy prepubertal children. Eur J Endocrinol 164:553–558
Scheller J, Rose-John S (1997) Interleukin-6 family of cytokines. Annu Rev Immunol 15:797–819
Kallen KJ (2002) The role of transsignalling via the agonistic soluble IL-6 receptor in human diseases. Biochim Biophys Acta 1592:323–343
Schuett H, Luchtefeld M, Grothusen C et al (2009) How much is too much? Interleukin 6 and its signalling in atherosclerosis. Thromb Haemost 102:215–222
Weiss TW, Arnesen H, Selijefot I (2013) Components of the Interleukin-6 transsignalling system are associated with the metabolic syndrome, endothelial disfunction and arterial stiffness. Metab Clin Exp 62:1008–1013
Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7:284–294
Cole TJ (2002) A chart to link centiles of body mass index, weight and height. Eur J Clin Nutr 56:1194–1199
Mattews DR, Hosker JP, Rudeski AS et al (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
D’Annunzio G, Vanelli M, Pistorio A et al (2009) Insulin resistance and secretion indexes in healthy Italian children and adolescents: a multicentre study. Acta Biomed 80:21–28
Fernández-Real JM, Ricart W (2003) Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev 24:278–301
Bastard JP, Maachi M, Lagathu C et al (2006) Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw 17:4–12
Vozarova B, Weyer C, Hanson K, Tataranni PA, Bogardus C, Pratley RE (2001) Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obes Res 94:14–417
Stith RD (1994) Luo J Endocrine and carbohydrate responses to interleukin-6 in vivo. Circ Shock 44:210–215
Petersen EW, Carey AL, Sacchetti M et al (2005) Acute IL-6 treatment increases fatty acid turnover in elderly humans in vivo and in tissue culture in vitro. Am J Physiol Endocrinol Metab 288:E155–E162
Bastard JP, Maachi M, Tran Van Nhieu J et al (2002) Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro. J Clin Endocrinol Metab 87:2084–2089
Mooney RA, Senn J, Cameron S et al (2001) Suppressors of cytokine signaling-1 and -6 associate with and inhibit the insulin receptor. A potential mechanism for cytokine-mediated insulin resistance. J Biol Chem 276:25889–25893
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Reinehr T, Andler W (2004) Changes in the atherogenic risk factor profile according to degree of weight loss. Arch Dis Child 89:419–422
Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C (2005) Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 115:e500–e503
Acknowledgments
This study was supported by a grant of University of Foggia (Italy).
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
G. De Filippo and D. Rendina contributed equally.
Rights and permissions
About this article
Cite this article
De Filippo, G., Rendina, D., Moccia, F. et al. Interleukin-6, soluble interleukin-6 receptor/interleukin-6 complex and insulin resistance in obese children and adolescents. J Endocrinol Invest 38, 339–343 (2015). https://doi.org/10.1007/s40618-014-0176-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-014-0176-4