Abstract
Objective
To examine the association between race/ethnicity concordance and in-person provider visits following the implementation of the Affordable Care Act.
Design
Using 2014–2015 data from the Medical Expenditure Panel Survey, we examine whether having a provider of the same race or ethnicity (“race/ethnicity concordance”) affects the probability that an individual will visit a provider. Multivariate probit models are estimated to adjust for demographic, socioeconomic, and health factors.
Results
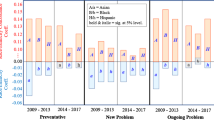
Race/ethnicity concordance significantly increases the likelihood of seeking preventative care for Hispanic, African-American, and Asian patients relative to White patients (coef = 1.46, P < 0.001; coef = 0.71, P = 0.09; coef = 1.70, P < 0.001, respectively). Race/ethnicity concordance also increases the likelihood that Hispanic and Asian patients visit their provider for new health problems (coef = 2.14, P < 0.001 and coef = 1.49, P < 0.05, respectively). We find that race/ethnicity concordance is also associated with an increase in the likelihood that Hispanic and Asian patients continue to visit their provider for ongoing medical problems (Hispanic coef = 1.06, P < 0.001; Asian coef = 1.24, P < 0.05).
Conclusions
There is an association between race/ethnicity concordance and the likelihood of patients visiting their provider. Our results demonstrate that racial disparities in health care utilization may be partially explained by race/ethnicity concordance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Racial and ethnic disparities in health care have been documented extensively. Despite improvements in Americans’ overall health, ethnic and racial minorities continue to have lower rates of utilization [1, 2], lower rates of adherence to prescribed medications and medical interventions [3, 4], and worse health outcomes and lower life expectancy [3, 4] and receive differential treatment and/or advice from their physicians [5]. The economic costs associated with racial health disparities were estimated in 2015 to be $35 billion in excess health care expenditures, $10 billion in illness-related productivity losses, and nearly $200 billion in premature death. Thus, reducing these disparities can also reduce both direct and indirect expenditures [6]. One factor that has been extensively documented as having a significant impact on utilization and health outcomes across a variety of medical specialties is patient-provider race/ethnicity concordance ([7,8,9,10,11,12,13,14,15,16]).
“Race/ethnicity concordance” is defined as occurring when the race/ethnicity of a patient matches the race/ethnicity of the individual’s provider whereas “race/ethnicity discordance” occurs when their respective races/ethnicities do not match. Previous studies have shown that, when given a choice, patients often choose providers of their own race and/or ethnicity [17,17,18,20]. Patients in race and/or ethnic concordant relationships with their providers often report higher levels of satisfaction with the care they receive, greater levels of trust in their provider, higher levels of perceived health care quality, and more accurate risk assessment of certain diseases [3, 4, 20,20,21,24]. It has also been shown that the quality of patient-provider communication during medical visits is impacted by race/ethnicity concordance. In a meta-analysis of the effects of race on communication, Shen et al. [25] found that race/ethnicity concordance affects patients’ clinical encounter experiences. While there was variability in the domains and measures of communication across studies, 11 out of 12 studies on race/ethnicity concordance in the review found that racial discordance consistently predicts poorer patient-physician communication (specifically poor communication in the domains of satisfaction, information-giving, partnership building, participatory decision-making, visit length, and respect of conversations). Quality of communication was the only communication domain found not to be affected by race/ethnicity concordance. There is much evidence to support the hypothesis that differences in provider treatment and linguistic or cultural barriers may negatively affect health outcomes for minority patients [26, 27]. Provider beliefs about minority patients have been shown to influence both the level of care provided to minority patients and physicians’ perceptions of minorities’ intelligence and education [25, 28]. Over the past decades, there has been an abundance of research, but no consensus, as to whether race/ethnic patient-provider concordance is associated with positive health outcomes for minorities [29].
In this paper, we examine data from the 2014–2015 Medical Expenditure Panel Survey (MEPS) to explore the association between patient-provider race/ethnicity concordance and health care utilization, specifically the link between race/ethnicity concordance and the patient’s likelihood of seeking preventative care as well as care for new and ongoing health problems. Previous studies utilizing MEPS data have used a range of years between 2002 and 2012 and found mixed results on the associations between race/ethnicity concordance and health care interactions ([16, 29]; and [14]). The data in this study was collected after the implementation of the Affordable Care Act Health Care Exchanges and thus provides an analysis on patient-provider interactions and behavior after health care access and coverage was greatly expanded. Evidence has shown that utilization rates increased after the ACA expansion [30]. Therefore, exploring factors associated with utilization, such as race/ethnicity concordance, is warranted.
Methods
Data
This study uses the 2014–2015 Medical Expenditure Panel Survey-Household Component (MEPS HC), a set of large-scale surveys of Americans which collect nationally representative data on demographic characteristics, health conditions, health status, use of medical care services, charges and payments, access to care, satisfaction with care, health insurance coverage, income, and employment. The set of households selected for each panel of the MEPS HC is a subsample of households participating in the previous year’s National Health Interview Survey (NHIS) conducted by the National Center for Health Statistics. This study limits data to adults who self-reported as non-Hispanic White (herein White), Hispanic, non-Hispanic African-American (herein African-American), and/or non-Hispanic Asian-American (herein Asian-American) and for whom complete data is available. Information pertaining to the race/ethnicity of the provider is reported by the participating households. The Health Belief Model posits that perception (e.g., perceived provider race/ethnicity) guides health promotion and maintenance behaviors [31, 32]. This is consistent with previous studies that have also relied on patients’ self-reports of their physician’s race [8, 18, 20, 21].
Figure 1 shows a breakdown of the MEPS sample included in our study. The sample size consists of 25,045 observations, including 10,625 White respondents, 7467 Hispanic respondents, 4956 African-American respondents, and 1997 Asian-American respondents. While some patients (755) self-identified as multiple races, this information is not available for the provider. As a result, we exclude these individuals from the analyses. A total of 18% (4548 cases) of patient-provider race/ethnicity concordance was observed in the data, with the majority being for White patients (3114 cases), followed by Hispanic patients (624 cases) and Asian-American patients (512 cases). The patient-provider race/ethnicity concordance is lowest for African-American patients with only 298 patient-provider matches.
Variables
Our outcome variables from the MEPS HC data include five standard measures of utilization. The first three measures are categorical (binary) outcome measures and include the probability of seeking preventive care, obtaining care for new health problem, and seeking continuing care for an ongoing health problem. We also include two numerical health care utilization measures: the number of any emergency department (ER) visits and the number of total physician visits. Figure 2 shows the hypothesized relationship between our dependent and independent variables of interest.
We build on the protocols outlined in Chen et al. [11] and Chen et al. [1] in selecting the covariates. Covariates from five general categories are included: race/ethnicity concordance, non-health-related socioeconomic and demographic factors, health-related characteristics, and clinical encounter factors such as provider communication characteristics and provider location characteristics. The race/ethnicity factors are White, African-American, Hispanic, and Asian-American, along with their respective provider concordance.
Our non-health-related socioeconomic and demographic covariates include immigration status (US-born citizens, those in the USA for less than 5 years, and those in the USA for greater than 5 years), age, sex, marital status (married/single), education (less than a high school degree, high school degree, and college/advanced degree), family income [< 100% federal poverty line (FPL), 100–200% FPL, and > 200% FPL], US Census region (northeast, midwest, south, and west), and insurance status. Health-related characteristics include self-reported physical condition (excellent, very good, good, fair, and poor), any functional limitations, and self-reported chronic conditions (hypertension, diabetes, cholesterol, heart diseases, and cancer). We also include an interaction term between the race/ethnicity concordance and the covariate indicating less than a high school degree as a measure of whether the effect of race/ethnicity concordance depends on the level of education of the patient. The provider characteristic covariates include both location and convenience factors (ease in contacting by phone, weeknight and weekend office hours, and “travel time is less than 30 min”), as well as communication factors such as whether the provider speaks the patient’s language and ratings of how well the provider communicates with the patient (listens, explains, has respect for patient, spends enough time with patient, and provides easy-to-understand instructions).
Analysis
Our main research objective is to examine the relationship between race/ethnicity concordance and the five measures of health utilization. We hypothesize that patients in race/ethnic concordant relationships with their provider will have a higher probability of seeing a health provider for an ongoing problem, a higher probability of seeing a health provider for a new problem, a higher probability of seeking preventative care, a decreased number of ER visits, and an increased total number of physician visits. In order to explore our research objective, we follow the protocol outlined in previous studies on concordance [1, 11]. Similar to Chen et al. [1], we estimate the multivariate non-linear probability models for each of the three dichotomous measures of health utilization using probit analyses. In addition, we also estimate multiple regressions for the numerical health measures. To provide a nationally representative estimate, we use survey weights provided with the MEPS data to adjust the sample characteristics. All models include the race/ethnicity concordance, non-health-related socioeconomic and demographics, health-related identifiers, and provider characteristics. We present the marginal effects for each of the probit models. The benefit of using probit analyses is that marginal effects can be estimated and directly interpreted. More specifically, the coefficients presented can be directly interpreted as the change in the probability of the utilization measure associated with a change in the covariates, such as race/ethnicity concordance. For example, the coefficient on race/ethnicity concordance is interpreted as the associated change in the probability of seeking care from a provider if that provider is the same race/ethnicity as the patient. To estimate the effect of race/ethnicity concordance, we define a match as cases in which a provider is identified as the same race/ethnicity as the patient. For example, a Hispanic race/ethnic concordant relationship would be one in which the individual identifies him or herself as Hispanic and answers yes to the following question in the survey: “Is provider Hispanic or Latino?” All analyses are carried out using Stata SE15.
Results
Table 1 presents the marginal effects of the multivariate non-linear probability models for each of the binary measures of utilization, “seeking preventative care,” “seeking care for a new problem,” and “seeking care for an ongoing problem.” Controlling for the covariates of race/ethnicity, non-health-related socioeconomic and demographic factors, health-related conditions, and provider characteristics, being in a race/ethnic concordant relationship is associated with significant increases in the probabilities of seeking preventive care for Hispanics and Asian-Americans relative to Whites (coef = 1.46, P < 0.001 and coef = 1.70, P < 0.001, respectively). Race/ethnicity concordance is associated with an increase in the likelihood of patients seeing their provider for new health problems for Hispanics and Asian-Americans relative to Whites (coef = 2.14, P < 0.001 and coef = 1.49, P < 0.05, respectively). The probability of seeking care for ongoing health problems is also positively correlated with race/ethnicity concordance for Hispanics and Asian-Americans (coef = 1.06, P < 0.001 and coef = 1.24, P < 0.05, respectively). The interaction between race/ethnicity concordance and those with less than a high school degree is only statistically significant for Hispanics seeking medical care for ongoing problems (coef = 1.28, P < 0.05).
In general, socioeconomic and demographic factors have a relatively limited impact on health utilization. The results in Table 1 show that patients between the ages of 45–54 are more likely than patients between the ages of 25–34 to utilize health care services. However, the increased likelihood is minimal ranging from 0.18 for seeking care for a new problem (coef = 0.18, P < 0.001) to 0.21 for visiting the provider for preventive care and ongoing problem (coef = 0.21, P < 0.001). The likelihood of seeking medical care (preventive care (coef = 0.29, P < 0.001), new problem (coef = 0.26, P < 0.001), and ongoing problem (coef = 0.35, P < 0.001) is slightly higher for those between the ages of 55–64 than for patients between the ages of 25–34. The likelihood of seeking health care services for preventive care and new problems is highest for patients 65 or older (coef = 0.37, P < 0.001 and coef = 0.28, P < 0.001; respectively) relative to all other age groups. Compared with US-born patients, foreign-born patients are slightly less likely to seek preventive care (coef = − 0.31, P < 0.05 for < 5 years in the USA and coef = − 0.13, P < 0.05 for > 5 years in the USA) or to seek care for new problems (coef = − 0.29, P < 0.05 for < 5 years in the USA and coef = − 0.14, P < 0.05 for > 5 years in the USA) or ongoing problems (coef = − 0.11, P < 0.05 for > 5 years in the USA). While family income for those “> 200% FPL” is statistically significant at the 5% level, the coefficient is equal to zero (coef = − 0.00, P < 0.05). Those patients living in the southern USA are slightly less likely to seek preventive care and care for new or ongoing problems compared with patients living elsewhere in the northeast (coef = − 0.23, P < 0.001; coef = − 0.21, P < 0.001; and coef = − 0.28, P < 0.001, respectively). Neither gender nor marital status has a significant effect on the probability of seeking preventive care, care for a new problem, or care for an ongoing problem.
The results for self-reported health status indicate some associations with the likelihood of someone receiving medical care. More specifically, self-reported health status of being in poor health is negatively associated with seeking care (coef = − 0.56, P < 0.001 for preventive care, coef = − 0.59, P < 0.001 for new problem, coef = − 0.44, P < 0.001 for ongoing problem). Among patients that self-reported having chronic conditions, having health issues such as hypertension (coef = 0.23, P < 0.001 for preventive care and coef = 0.17, P < 0.001 for ongoing problem) and high cholesterol (coef = 0.12, P < 0.001 for preventive care, coef = 0.11, P < 0.05 for new problems, and coef = 0.13, P < 0.05 for ongoing problem) are positively associated with seeking care. Similarly, having a heart condition, as well as diabetes, is also associated with an increased probability of seeking medical care (heart cond./disease: coef = 0.20, P < 0.0001 for new problem and coef = 0.15, P < 0.05 for ongoing problem; diabetes: coef = 0.17, P < 0.05 for ongoing problem). Patients living with any functional limitations are also more likely to seek medical attention (coef = 0.20, P < 0.001 for preventive care and coef = 0.21, P < 0.001 for ongoing problem).
Factors that have a greater association with the likelihood of seeking health care services include convenience and whether the provider speaks the same language as the patient. With the former, being able to contact the provider by phone is associated with an increase in the probability of seeking care by 1.53, 1.62, and 1.45 for preventive care (coef = 1.53, P < 0.001), new problem (coef = 1.62, P < 0.001), and ongoing problem (coef = 1.45, P < 0.001), respectively. The associated likelihood increases if the travel time to a provider is less than 30 min (preventive care (coef = 2.02, P < 0.001), new problem (coef = 2.14, P < 0.001), and ongoing problem (coef = 1.92, P < 0.001)). If the provider speaks the patient’s language, the likelihood of seeking medical care is also higher (preventive care (coef = 1.17, P < 0.001), new problem (coef = 0.93, P < 0.001), and ongoing problem (coef = 1.30, P < 0.001)). Moreover, there is a positive association between the patient’s perception of whether the provider clearly explains any health issues during the visit and seeking health care services for preventive care (coef = 0.19, P < 0.001) as well as for new problems (coef = 0.14, P < 0.05).
Table 2 shows that the race/ethnicity concordance is only significant for the interaction term with less than a high school education. More specifically, race/ethnicity concordance is negatively associated with Hispanics for the number of ER visits (coef = − 0.12, P < 0.001) and positively correlated with the number of provider visits for Hispanics and Asian American (coef = 1.29, P < 0.05 and coef = 1.69, P < 0.05, respectively). Patients reporting a chronic condition visit the provider more often.
Discussion
Our findings suggest that race/ethnicity concordance is associated with an increase in the probability that patients seek or receive medical care. This is particularly prominent for Hispanic and Asian patients, potentially due to language and cultural barriers. Having a provider who speaks the patient’s language has been shown to be associated with a higher probability of health utilization [18].
Compared with US-born patients, foreign-born patients are less likely to seek preventive care or care for ongoing or continuing medical problems. Family income is largely unassociated with seeking medical care. Gender does not have a significant effect on the probability of seeking preventive care, care for a new problem, or care for an ongoing problem. However, females visit their provider and the ER slightly more than males. Marital status also has very little effect on the decision to seek care, with married patients making slightly fewer ER visits than unmarried patients.
Those patients living in the southern USA are slightly less likely to seek preventive care or care for ongoing or new problems compared with patients living elsewhere in the USA. As expected, patients with diseases such as hypertension and high cholesterol are more likely to seek care. Having a higher level of education than a high school diploma and self-reported health status of “fair” or “better” also increases the likelihood of someone receiving medical care. However, in addition to these factors, this study has also demonstrated that factors other than socioeconomic and health factors, such as race/ethnicity concordance, remain an important feature of a patient’s decision to seek health care from a provider.
Previous findings that patients in race/ethnic concordant relationships with their provider report higher levels of satisfaction with medical treatment and greater patient-provider communication are consistent with our results that patients may be more willing to visit their provider for new problems and preventive care if they are in race/ethnic concordant relationships.
Our study has some limitations. First, we did not examine specific ethnicities within racial categories. Studies have identified disparities across multiple ethnic subgroups [19]. Future work should examine if our results generalize across ethnic subgroups. Second, we were not able to investigate the impact of the decreased number of visits resulting from discordant relationships on measurable health outcomes such as patient life expectancy. This would be a fruitful direction for future research. Third, the cross-sectional design limits our ability to make causal inferences on the association between race/ethnicity concordance and utilization.
We have shown that even after the greater access and coverage provided by the ACA, racial and ethnic disparities in utilization of medical services may continue to be driven in part by social factors. Given the substantial economic cost associated with racial and ethnic health disparities, analyzing the impact of patient-provider race/ethnicity concordance in increasing health utilization is only one of the many determinants that should be considered to close the gap in health utilization across racial/ethnic groups.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable written request.
References
Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Med Care. 2016;54(2):140–6.
Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666.
Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010a;25(11):1172–7.
Traylor AH, Subramanian U, Uratsu CS, Mangione CM, Selby JV, Schmittdiel JA. Patient race/ethnicity and patient-physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2010b;33(3):520–5.
Bleich SN, Simon AE, Cooper LA. Impact of patient–doctor race concordance on rates of weight-related counseling in visits by black and white obese individuals. Obesity. 2012;20(3):562–70.
Ayanian JZ. The costs of racial disparities in health care. Harv Bus Rev. 2015.
Ford CL, Konrad TR, Godette DC, Corbie-Smith G. Acceptance of routine ELISA testing among black women STD patients: relationship to patient-provider racial concordance. Sex Transm Dis. 2008;35(3):211–3.
LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;1:296–306.
LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. International Journal of Health Services. 2011;41(2):231–8
Alcalá HE, Chen J, Langellier BA, Roby DH, Ortega AN. Impact of the Affordable Care Act on health care access and utilization among Latinos. J Am Board Fam Med. 2017;30(1):52–62.
Chen J, Bustamante AV, Tom SE. Health care spending and utilization by race/ethnicity under the Affordable Care Act’s dependent coverage expansion. Am J Public Health. 2015;105(S3):S499–507.
Hernandez ND, Daley EM, Young L, Kolar SK, Wheldon C, Vamos CA, et al. HPV vaccine recommendations: does a health care provider’s gender and ethnicity matter to unvaccinated Latina college women? Ethn Health. 2017;22:1–7.
Jerant A, Bertakis KD, Fenton JJ, Tancredi DJ, Franks P. Patient-provider sex and race/ethnicity concordance: a national study of healthcare and outcomes. Med Care. 2011;1:1012–20.
Malhotra J, Rotter D, Tsui J, Llanos AA, Balasubramanian BA, Demissie K. Impact of patient–provider race, ethnicity, and gender concordance on cancer screening: findings from Medical Expenditure Panel Survey. Cancer Epidemiol Biomark Prev. 2017;26(12):1804–11.
Schoenthaler A, Allegrante JP, Chaplin W, Ogedegbe G. The effect of patient–provider communication on medication adherence in hypertensive black patients: does race concordance matter? Ann Behav Med. 2012;43(3):372–82.
Sweeney CF, Zinner D, Rust G, Fryer GE. Race/ethnicity and health care communication: does patient-provider concordance matter? Med Care. 2016;54(11):1005–9.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–9.
Gray B, Stoddard JJ. Patient-physician pairing: does racial and ethnic congruity influence selection of a regular physician? J Community Health. 1997;22(4):247–59.
Jang Y, Yoon H, Kim MT, Park NS, Chiriboga DA. Preference for patient–provider ethnic concordance in Asian Americans. Ethn Health. 2018:1–12.
Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Aff. 2000;19(4):76–83.
Johnson RL, Roter D, Powe NR, Cooper LA. n. Am J Public Health. 2004;94(12):2084–90.
Phillips KL, Chiriboga DA, Jang Y. Satisfaction with care: the role of patient-provider racial/ethnic concordance and interpersonal sensitivity. J Aging Health. 2012;24(7):1079–90.
Sohler NL, Fitzpatrick LK, Lindsay RG, Anastos K, Cunningham CO. Does patient–provider racial/ethnic concordance influence ratings of trust in people with HIV infection? AIDS Behav. 2007;11(6):884–96.
Schoenthaler A, Montague E, Baier Manwell L, Brown R, Schwartz MD, Linzer M. Patient–physician racial/ethnic concordance and blood pressure control: the role of trust and medication adherence. Ethn Health. 2014;19(5):565–78.
Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117–40.
Van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1):1–140.
Cooper LA, Powe NR. Disparities in patient experiences, health care processes, and outcomes: the role of patient-provider racial, ethnic, and language concordance. New York: Commonwealth Fund; 2004. Jul 9
Smedley BD, Stith AY, Nelson AR. 2003. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: confronting racial and ethnic disparities in healthcare.
Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient–provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14(1):107–30.
Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164(12):795–803.
Rosenstock IM. Health belief model. In: Kazdin AE, editor. Encyclopedia of Psychology. Wahshington, DC: American Psychological Association; 2000. p. 78–80.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, A., Sanchez, A. & Ma, M. The Impact of Patient-Provider Race/Ethnicity Concordance on Provider Visits: Updated Evidence from the Medical Expenditure Panel Survey. J. Racial and Ethnic Health Disparities 6, 1011–1020 (2019). https://doi.org/10.1007/s40615-019-00602-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-019-00602-y