Abstract
Background
Compared to non-Hispanic whites, African-American women tend to be diagnosed with breast cancer at an earlier age, to have less favorable tumor characteristics, and to have poorer outcomes from breast cancer. The extent to which differences in clinical characteristics account for the black/white disparity in breast cancer mortality is unclear. The purpose of this investigation was to examine the association of clinical, demographic, and treatment variables with total mortality and breast cancer recurrence by race/ethnicity in a cohort of women diagnosed with invasive breast cancer.
Methods
To this end, we used data on 3890 invasive breast cancer cases diagnosed at a single medical center. Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (95% CI) for the association of tumor characteristics and treatment variables with mortality and recurrence.
Results
Compared to white women, black women with breast cancer presented with tumors that had worse prognostic factors, particularly higher stage, lower frequency of hormone-receptor positive tumors, and higher frequency of comorbidities. Hispanics also generally had less favorable prognostic factors compared to non-Hispanic whites. Among estrogen receptor-positive cases, blacks had roughly a two-fold increased risk of recurrence compared to non-Hispanic whites. However, ethnicity/race was not associated with total mortality. Tumor stage, tumor size, and Charlson comorbidity index were positively associated with mortality, and mammography and chemotherapy and hormone therapy were inversely associated with mortality.
Conclusion
In spite of poorer prognostic factors among blacks compared whites, race/ethnicity was not associated with total mortality in our study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In spite of African-American women having a lower incidence of invasive breast cancer compared to white women, mortality from breast cancer is 42% higher among African-American women [1]. Compared to whites, black women are more likely to be diagnosed with breast cancer at an early age and to present with a higher tumor stage and a more aggressive phenotype (e.g., ER-negative/HER2-positive and triple-negative breast cancer) [2–5] and to have poorer outcome from breast cancer [3, 6]. Extensive evidence points to differences in the biology of breast cancer in African-Americans compared to whites [7, 8]. However, even after controlling for biologic factors such as age and cancer phenotype, racial differences in survival/mortality appear to persist [4, 9]. Studies point to the existence of racial disparities in receipt of treatment and adherence to treatment schedules [10, 11], barriers to accessing care influenced by socioeconomic factors [12–14], and poorer general health [15], all of which may affect outcomes in breast cancer patients. Thus, the extent to which biological factors (molecular characteristics of the tumor, menopausal status, reproductive history, exogenous hormone use) and non-biological factors (e.g., socioeconomic status) either contribute independently or through interaction with each other to ethnic/racial disparities in breast cancer survival is unclear [7, 8].
Reducing cancer disparities is a major public health objective of the National Cancer Institute and the Centers for Disease Control and Prevention [16]. We report here on disparities between black, white, and Hispanic women regarding breast cancer recurrence and survival in a cohort of Bronx women receiving care at the Montefiore Medical Center (MMC). The Bronx population is uniquely suited to this objective as it has a high proportion of minority groups, allowing for detailed evaluation of ethnicity/race and race-specific factors related to outcomes following breast cancer diagnosis. Analysis of the MMC cancer registry data provides an opportunity to identify factors that may influence the observed differences in breast cancer recurrence and mortality in minority populations.
Methods
Study Population
Montefiore Medical Center is the largest health care provider in the Bronx, NY, and is the teaching hospital for the Albert Einstein College of Medicine. The Montefiore Medical Center Tumor Registry maintains a registry of cancer patients receiving care at MMC. All cancer-related data are initially assembled by the Montefiore Einstein Medical Center Tumor Registry. These data are provided nightly to Montefiore’s Clinical Looking Glass System (CLG). Looking Glass™ Clinical Analytics (Streamline Health, Atlanta, Georgia) is a user-friendly interactive software application for the evaluation of health care quality, effectiveness, and efficiency [17]. The CLG has reliable data on cancer patients diagnosed from 2004 up until 2013.
The cohort used in this study was defined as those CLG patients with an initial diagnosis date of invasive breast cancer between 7/1/2004 and 12/31/2013, as determined on 2/11/2014 (N = 3890).
Clinical Data
For each individual with breast cancer in the CLG system, data are reported on breast cancer characteristics including stage, grade, tumor size, receptor status (ER, PR, HER2), and histology, and, if it has occurred, recurrence (local, regional, distant). Demographic information is also reported, including sex, ethnicity/race, age, tobacco use, and pre-diagnosis and post-diagnosis BMI (however, the latter variables were only available on 34.4 and 77.0% of the study population, respectively). In addition, information on socioeconomic status can be derived from the census tract of each individual [18]. Tumor treatment data are obtained from a separate file, outside of the CLG system (but provided by CLG personnel), that contains detailed information on treatment start date, treatment course, and treatment type (modality). Both breast cancer recurrence and all-cause mortality are also reported to CLG.
To assess overall health, the Charlson comorbidity index [19] was computed by summing the number of chronic conditions reported in the hospital chart, including diabetes, myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, mild liver disease, hemiplegia or paraplegia, renal disease, and malignancy.
Because women of Asian background constituted only 1.6% of invasive cases (63 out of 3890), we combined Asians with women of “other race/ethnicity.”
Mortality Data
Mortality data to 12/31/2013 were obtained by linkage of the cohort to the National Death Index. Additional follow-up data on the cohort, including vital status, were obtained via the CLG system through 04/06/15.
Statistical Analysis
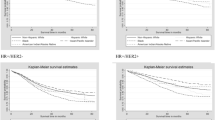
Cox proportional hazard models were used to estimate hazard ratios and 95% confidence intervals for the association of each clinical and treatment variable with patient vital status and recurrence. The associations of race/ethnicity with recurrence and vital status were also evaluated. Study participants were considered to be at risk starting from the date of first diagnosis of invasive breast cancer and ending at the date of termination of follow-up (04/06/ 2015), breast cancer recurrence (for recurrence analysis only), or death, whichever occurred first. All 3890 cases were included in the analyses with mortality as the outcome. Risk of recurrence was assessed in 2657 cases who were classifiable as to whether they had a recurrence. This analysis excluded 1233 women, 418 of whom were classified as “never disease-free” and 815 cases who were classified as “unknown if recurrence, or patient ever disease-free.” Of the 2657 women classifiable as to recurrence, 209 had evidence of recurrence and 2448 were free of disease following treatment. Among those with evidence of recurrence, 19.1% had local, 16.7% had regional, and 64.1% had distant recurrence. All analyses were adjusted for age at diagnosis and AJCC stage, and fully adjusted models included age at diagnosis, AJCC stage, tumor phenotype, other tumor characteristics, mammography screening, and treatment variables. Inclusion of a derived variable for SES based on census tract information did not alter the results and therefore was not included in the final multivariable model. All statistical tests were two-sided and all analyses were conducted using SAS version 9.4 (Cary NC).
Results
Clinical and treatment characteristics of invasive breast cancer cases are presented in Table 1. Non-Hispanic whites were older than other ethnic groups (mean age 65.8 years vs. 61.1 years [African-Americans], 59.6 years [Hispanics], and 59.8 years [“other ethnicity/race”]). The proportion of stage I tumors was highest in non-Hispanic whites and lowest in African-American cases (55.5 vs. 42.5%), while the reverse obtained for higher stage tumors. Hispanics also tended to be diagnosed at more advanced stages compared to non-Hispanic whites. The proportion of cases with ER-positive and PR-positive tumors was greatest in non-Hispanic whites and lowest in African-American cases, whereas the proportion of HER2-positive cases varied little by race/ethnicity (a substantial proportion of cases had unknown HER2 status). The proportion of cases with triple-negative breast cancer was higher in African-American than non-Hispanic white cases (11.3% vs. 4.9%). The distribution by tumor grade and tumor size was also most favorable in non-Hispanic whites and least favorable in African-Americans (42.4% of African-Americans had poorly-differentiated tumors as opposed to 27.6% of non-Hispanic whites). In general, aside from tumor stage, the pattern of tumor markers among Hispanics was intermediate between that of blacks and whites. Hispanics and African-Americans had somewhat lower proportions of cases with no comorbid conditions compared to other groups. Fewer African-Americans and Hispanics had breast-conserving surgery compared to non-Hispanic whites, and correspondingly greater proportions of African-American and Hispanic cases had a mastectomy. Greater proportions of African-Americans, Hispanics, and “other race/ethnicity” received chemotherapy compared to non-Hispanic whites, and somewhat greater proportions of African-Americans, Hispanics, and “other ethnicity/race” received radiation therapy. With regard to neighborhood level SES, 59.1% of whites were in the two highest quintiles compared to 29.1% of blacks, 16.5% of Hispanics, and 37.6% of “other race/ethnicity.”
Median follow-up of the cohort was 3.73 years (5th percentile, 0.59 years; 95th percentile, 8.60 years; mean = 4.6 years). In analyses adjusting only for age at diagnosis and stage, ER status (ER-negative), PR status (PR-negative), tumor grade (higher grade), tumor size (larger size), and Charlson comorbidity index were positively associated with mortality, whereas having had a screening mammogram in the 3 years prior to diagnosis, and radiation therapy and chemotherapy were inversely associated with mortality (Table 2). In model 2, in which all variables were examined simultaneously, higher tumor stage, greater tumor size, and higher Charlson comorbidity index were positively associated with mortality, and prior screening mammogram, radiation therapy, and hormone therapy were inversely associated with mortality. When dummy variables for ethnicity/race were added as covariates, risk estimates were unchanged, and no ethnic/race group was at increased (or decreased) risk of mortality. The small number of cases who had no surgery had roughly a 3-fold increased risk of dying.
There was a significant inverse association between “other ethnicity/race” and mortality in both the minimally- and fully-adjusted models in the analysis including all cases and in those restricted to ER-positive and ER-negative breast cancer (Table 3). There were no other associations between race and mortality.
The median time to recurrence, among cases suitable for assessing recurrence, was 2.00 years (5th percentile 0.55; 95th percentile 5.26 years; mean = 2.4 years). After adjustment for age at diagnosis and tumor stage, African-Americans were at increased risk of recurrence compared to non-Hispanic white cases (referent group) (Table 4). However, this association was no longer significant after controlling for clinical and treatment variables. When the sample was restricted the ER-positive cases, in both models African-Americans had roughly a two-fold increased risk of recurrence compared to non-Hispanic whites (model 2 HR 1.84, 95% CI 1.03–3.29). Among ER-negative cases, compared to white women, Hispanic women and women of “other race/ethnicity” had reduced risk of recurrence. Among the 1233 cases who were lacking recurrence information, the stage distribution was similar to that among cases who went on to have a recurrence (data not shown).
Only 44 deaths were attributed to breast cancer. After adjustment for age and stage, blacks had significantly increased breast cancer-specific mortality relative to whites. However, in the full model, the excess risk among blacks was no longer statistically significant (Supplementary Table).
Discussion
In this analysis of clinical and treatment characteristics, recurrence, and mortality among cases with invasive breast cancer diagnosed at a single medical center in the Bronx, African-American women presented with tumors that had worse prognostic factors compared to those of tumors in non-Hispanic white cases. These included more advanced stage and grade, greater tumor size, lower proportions of estrogen-receptor positive and progesterone-receptor positive tumors, and a higher frequency of triple-negative tumors. Hispanics also generally had less favorable prognostic factors compared to non-Hispanic whites. Among ER-positive cases, African-Americans had roughly a two-fold increased risk of recurrence compared to non-Hispanic whites. However, ethnicity/race was not associated with total mortality. Tumor stage, tumor size, and Charlson comorbidity index were positively associated with mortality, and mammography and chemotherapy and hormone therapy were inversely associated with mortality.
Our analysis is based on women who have already sought treatment at a major tertiary care medical center. The differences in clinical and treatment characteristics observed in the MMC breast cancer population are consistent with the results of a recent analysis of the SEER data on invasive breast cancer cases [4]. For example, in the SEER data, the proportion of stage I cases among non-Hispanic whites, African-Americans, and Hispanics was 50.8%, 37.0%, and 40.1%, respectively, compared to 55.5%, 42.5%, and 44.9% in our study. Similarly, 82.1% of non-Hispanic white cases, 66.3% of African-American cases, and 76.0% of Hispanic cases in SEER had ER-positive tumors, compared to 81.7, 65.4, and 72.8%, respectively, in our study. Among invasive breast cancer cases from the California Cancer Registry, 48.5% of non-Hispanic white cases vs. 36.4% of African-American cases were classified as stage I [9].
While the evidence regarding worse tumor characteristics among blacks compared to non-Hispanic whites is consistent in different study populations, it is unclear to what extent these differences in tumor characteristics influence recurrence and mortality. In our analysis, ethnicity/race was not associated with overall mortality in the full multivariable model including clinical factors and treatment. However, the duration of follow-up was relatively short, particularly to allow for outcomes in women with hormone-positive disease. Our finding that blacks had a two-fold increased risk of recurrence compared to whites is consistent with that from a clinical trial in which black patients with hormone receptor-positive HER2-negative disease had worse disease-free survival compared to non-black patients [20].
There is also inconsistency in the literature regarding whether, compared to whites, blacks have a poorer outcome from breast cancer after accounting for sociodemographic factors. A meta-analysis including 20 studies up to 2005 [6] found African-American ethnicity was associated with worse overall survival (HR 1.27, 95% CI 1.18–1.38) and breast cancer-specific survival (HR 1.19, 95% CI 1.10–1.29). The African-American disparity in survival remained after adjustment for SES, whereas no ethnic differences in outcome were detected in a SEER-Medicare analysis that controlled for SES and comorbidities [21]. In a review of medical records from one medical center, no difference in overall survival was seen after adjustment for sociodemographic factors, but the risk of recurrence was non-significantly increased among blacks (HR = 1.3, p = 0.11) [22]. Some studies have found that differences in mortality are limited to certain stages and tumor markers [9, 14, 23]. This suggests that there may be disparities in access to adjuvant or neo-adjuvant treatments or in other factors that affect mortality [24].
Breast cancer mortality rates have decreased since 1990 in both blacks and whites; however, they have remained higher and have decreased at a slower rate in black women [25, 26]. Before the 1980s, breast cancer mortality rates differed little between blacks and whites after adjustment for incidence [27]. At that time, radical surgery was the predominant treatment available. The appearance of a disparity between black and white breast cancer mortality starting in the late 1980s coincided with the introduction of adjuvant systemic treatments and mammography. This suggests that differences in treatment may contribute to the black-white breast cancer mortality difference. While differences in treatment by race/ethnicity observed in the present study were consistent with differences in clinical factors at diagnosis, since available data in the CLG system were limited and pertained only to the first line of treatment, we cannot rule out differences in subsequent treatment and/or compliance by race/ethnicity.
There is compelling evidence that both biological and non-biological factors play a role in the black-white breast cancer mortality differential [7, 8]. Factors other than the inherent biological nature of the tumor, including reproductive history, other comorbidities, and socioeconomic status and attitudes toward treatment which affect access to, and compliance with, medical care, also appear to contribute to the black-white disparity [10–14]. As has been pointed out [13], many of these factors are correlated through their association with SES, and they may interact to influence prognosis by multiple pathways [3]. Since the black-white mortality gap has widened over time, one or more factors associated with increased mortality must have increased among blacks relative to whites. Although obesity, which can influence the prognosis of breast cancer [28], has increased in the U.S. in the past 3 decades, and the increase has been greatest in black women and those with less than a high school education [29], one study found that obesity did not explain the black/white disparity in breast cancer mortality [30]. Another possibility is that higher rates of comorbidity among blacks contribute to the disparity [15].
Strengths of the present study include the availability of uniform clinical and treatment information on a large multi-ethnic population at a single medical center. Limitations include the unavailability of information on reproductive history, diet, hormone use, or individual-level socioeconomic status, and the relatively short follow-up. Information on pre-diagnosis body mass index was only available for a one-third of patients, and post-diagnosis BMI was available for three-quarters of cases. In a sensitivity analysis, post-diagnosis BMI, which was strongly correlated with pre-diagnosis BMI [Pearson r = 0.93] was not associated with overall mortality when added to the full model presented in Table 2. Furthermore, as mentioned earlier, treatment information was limited to the first course of treatment with a given modality (yes, no), and information on the type and dose of chemotherapy was not available. In addition, the follow-up period was relatively short, and the relatively small number of recurrences and deaths in our study did not permit analyses to be stratified by stage or other tumor characteristics. The fact that adjustment for neighborhood level SES did not affect the association of study factors with mortality may reflect the relative homogeneity of the population in terms of SES. Alternatively, neighborhood-level SES may be weakly correlated with factors affecting mortality.
In conclusion, compared to white women diagnosed with breast cancer, black women with breast cancer had a worse profile with respect to clinical factors, particularly higher stage and higher frequency of comorbidities. Among women with ER-positive tumors, blacks had an increased risk of recurrence, but ethnicity/race was not associated with overall mortality.
References
DeSantis C, Fedewa SA, Sauer AG, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66:31–42.
Cunningham JE, Butler WM. Racial disparities in female breast cancer in South Carolina: clinical evidence for a biological basis. Breast Cancer Res Treat. 2004;88:161–76.
Maskarinec G, Sen C, Koga K, Conroy SM. Ethnic differences in breast cancer survival: status and determinants. Women’s Health (Lond Engl). 2011;7(6):677–87. doi:10.2217/whe.11.67.
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015;313(2):165–73.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MCU, Nielsen TO, Moorman PG, Earp HS, Millikan RC. Race, breast cancer subtypes, and survival in the Carolina breast cancer study. JAMA. 2006;295(21):2492–502.
Newman LA, Griffith KA, Jatoi I, Simon MS, Crowe JP, Colditz GA. Meta-analysis of survival in African-American and white American patients with breast cancer: ethnicity compared with socioeconomic status. J Clin Oncol. 2006;24(9):1342–9.
Keenan T, Moy B, Mroz EA, Ross K, Niemierko A, Rocco JW, Isakoff S, Ellisen LW, Bardia A. Comparison of the genomic landscape between primary breast cancer in African American versus white women and the association of racial difference with tumor recurrence. J Clin Oncol. 2015;33(31):3621–7.
Danforth DN. Disparities in breast cancer outcomes between Caucasians and African American women: a model for describing the relationship of biological and nonbiological factors. Breast Cancer Res. 2013;15:208.
Tao L, Gomez SL, Keegan THM, Kurian AW, Clarke CA. Breast cancer mortality in African-American and non-Hispanic white women by molecular subtype and stage at diagnosis: a population-based study. Cancer Epidemiol Biomark Prev. 2015;24(7):1039–45.
Breen N, Wesley MN, Merrill RM, et al. The relationship of socioeconomic status and access to minimum expected therapy among female breast cancer patients in the National Cancer Institute black-white cancer survival study. Ethn Dis. 1999;9:111–25.
Samson ME, Porter NG, Hurley DM, Adams SA, Eberth JM. Disparities in breast cancer incidence, mortality, and quality of care among African American and European American women in South Carolina. South Med J. 2016;109(1):24–30. doi:10.14423/SMJ.
Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Int Med. 2006;166:2244–52.
Vona-Davis L, Rose DP. The influence of socioeconomic disparities on breast cancer tumor biology and progrosis: a review. J Women’s Health. 2009;18(6):883–93.
Parise CA, Caggiano V. Disparities in race/ethnicity and socioeconomic status: risk of mortality of breast cancer patients in the California cancer registry, 2000-2010. BMC Cancer. 2013;13:449.
Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D. Comorbidity and survival disparities among black and white patients with breast cancer. JAMA. 2005;294(14):1765–72.
Kohler BA, Sherman RL, Howlander N, et al. Annual report to the nation on the status of cancer 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107(6):djv048.
Bellin E, Fletcher DD, Geberer N, Islam S, Srivastava N. Democratizing information creation from health care data for quality improvement, research, and education – the Montefiore medical center experience. Acad Med. 2010;85(8):1362–8. doi:10.1097/ACM.0b013e3181df0feb.
Roux AVD, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:100.
Molto A, Dougados M. Comorbidity indices. Clin Exp Rheumatol. 2014;32(Suppl. 85):S131–4.
Sparano JA, Wang M, Zhao F, Stearns V, Martino S, Ligibel JA, Perez EA, Saphner T, Wolff AC, Sledge Jr GW, Wood WC, Davidson NE. Race and hormone receptor-positive breast cancer outcomes in a randomized chemotherapy trial. J Natl Cancer Inst. 2012;104:406–14.
Curtis E, Quale C, Haggstrom D, Smith-Bindman R. Racial and ethnic differences in breast cancer survival: how much is explained by screening, tumor severity, biology, treatment, comorbidities, and demographics. Cancer. 2008;112(1):171–80.
Komenaka IK, Martinez ME, Pennington Jr RE, et al. Race and ethnicity and breast cancer outcomes in an underinsured population. J Natl Cancer Inst. 2010;102(15):1178–87.
Albain KS, Unger JM, Crowley JJ, Coltman CA, Hershman DL. Racial disparities in cancer survival among randomized clinical trial patients of the southwest oncology group. J Natl Cancer Inst. 2009;101:984–92.
Daly B, Olopade OI. Race, ethnicity, and the diagnosis of breast cancer (editorial). JAMA. 2015;313:141–2.
Menashe I, Anderson WF, Jatoi I, Rosenberg PS. Underlying causes of the black-white racial disparity in breast cancer mortality: a population-based analysis. J Natl Cancer Inst. 2009;101:993–1000.
DeSantis C, Jemal A, Ward E, Thun MJ. Temporal trends in breast cancer mortality by state and race. Cancer Causes Control. 2008;19:537–45.
Mandelblatt JS, Sheppard VB, Neugut AI. Black-white differences in breast cancer outcomes among older Medicare beneficiaries (editorial). JAMA. 2013;310(4):376–7.
Carmichael AR. Obesity and prognosis of breast cancer. Obes Rev. 2006;7(4):333–40.
Krishna A, Razak F, Lebel A, Smith GD, Subramanian SV. Trends in group inequalities and interindividual inequalities in BMI in the United States, 1993-2012. Am J Clin Nutr. 2015;101:598–605.
Lu Y, Ma H, Malone KE, Norman SA, Sullivan-Halley J, Strom BL, Marchbanks PA, Spirtas R, Burkman RT, Deapen D, Folger SG, Simon MS, Press MF, McDonald JA, Bernstein L. Obesity and survival among black women and white women 35 to 64 years of age at diagnosis with invasive breast cancer. J Clin Oncol. 2011;29:3358–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure of Potential Conflicts of Interest
The authors declare that they have no competing interests.
Research Involving Human Participants
This study was approved the Institutional Review Board of the Albert Einstein College of Medicine. No animal subjects were included in this study.
Funding
This work was supported by institutional funds from the Albert Einstein College of Medicine.
Dr. Rohan receives support from the Breast Cancer Research Foundation.
We thank Dr. Chelsea Catsburg for her help in developing the breast cancer cohort.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Kabat, G.C., Ginsberg, M., Sparano, J.A. et al. Risk of Recurrence and Mortality in a Multi-Ethnic Breast Cancer Population. J. Racial and Ethnic Health Disparities 4, 1181–1188 (2017). https://doi.org/10.1007/s40615-016-0324-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-016-0324-y