Abstract
Objective
With the development of online learning, communication, and entertainment, the Internet has become an indispensable tool for university students. Internet addiction (IA) has emerged as a health problem and the prevalence of IA varies from country to country. To date, the global prevalence of IA in medical students remains unknown. The objective of this meta-analysis was to establish precise estimates of the prevalence of IA among medical students in different countries.
Methods
The pooled prevalence of IA among medical students was determined by the random-effects model. Meta-regression and subgroup analysis were performed to identify potential factors that could contribute to heterogeneity.
Results
The pooled prevalence of IA among 3651 medical students is 30.1% (95% confidence interval (CI) 28.5–31.8%, Z = −20.66, df = 9, τ 2 = 0.90) with significant heterogeneity (I 2 = 98.12). Subgroup analysis shows the pooled prevalence of IA diagnosed by the Chen’s Internet Addiction Scale (CIAS) (5.2, 95% CI 3.4–8.0%) is significantly lower than Young’s Internet Addiction Test (YIAT) (32.2, 95% CI 20.9–45.9%) (p < 0.0001). Meta-regression analyses show that the mean age of medical students, gender proportion and the severity of IA are not significant moderators.
Conclusions
In conclusion, this meta-analysis identified the pooled prevalence of IA among medical students is approximately five times than that of the general population. Age, gender, and severity of IA did not account for high heterogeneity in prevalence, but IA assessment questionnaire was a potential source of heterogeneity. Given the high prevalence of IA, medical teachers and medical school administrators should identify medical students who suffer from IA and refer them for intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With the rapid advance in technologies over the past decade, the Internet has become an integral part of the lives of many individuals. Widespread Internet access has benefited people by improving access to online information and providing new opportunities for social communication and entertainment [1]. Although the Internet has offered advantages, excessive usage of the Internet is associated with a psychiatric condition known as Internet addiction (IA) [2, 3]. IA mimics other forms of addiction and is characterized by an inability to inhibit Internet use despite negative impact on physical health and psychosocial functioning [4,5,6,7].
Previous studies have highlighted the importance of studying IA in university students because they are more likely than the general population to use the Internet [1] and vulnerable to develop IA [8]. Additionally, university students have an immediate desire to engage in online activities because the Internet is readily available on laptop computers and smartphone devices [1]. Previous studies report the prevalence of IA among university students to vary between 4% in the USA [9] and 16.8% in Italy [10].
Meta-analysis is a statistical procedure used for combining the results of a number of studies in order to estimate a pooled effect size [11, 12]. Although previous meta-analysis studied the pooled prevalence of depression among medical students in different countries [13, 14], the pooled prevalence of IA remains unknown. In more recent work, IA was found to be associated with atrophy in the prefrontal cortex and cognitive impairment [4]. Such cognitive impairment could significantly affect the academic performance of medical students and fitness to practice after graduation. For this purpose, the current meta-analysis aimed to establish the pooled prevalence of IA among medical students in different countries.
Methods
A comprehensive search was conducted from January 1, 2017, to February 20, 2017. The following databases were searched: PubMed (since 1966), Embase (since 1980), PsychINFO (since 1806), BIOSIS (since 1926), Science Direct (since 2006), and Cochrane CENTRAL (since 1993). The search terminologies included permutations of the keywords for IA (e.g., Internet addiction, problematic internet use) and medical students, medical undergraduates.
The inclusion criteria for this meta-analysis were as follows: (a) undergraduate medical students formed the main cohort of the study population, (b) the severity of IA was measured by a validated questionnaire, and (c) prevalence of IA was the primary outcome of the study population. The exclusion criteria were as follows: (a) a study without an abstract written in English and (b) insufficient information to compute the pooled prevalence of IA.
Articles were de-identified (author(s), year of publication, and journal name) before data extraction [15]. Selection of the relevant publications was conducted independently by two authors, namely that of MWBZ and RL. In the first phase, articles were screened based on their titles and abstracts. The shortlisted articles were then evaluated against the aforementioned inclusion and exclusion criteria. In the event of any disagreement between two authors, it was resolved by discussion with the last author, RCMH. All procedures conformed to the guidelines for meta-analysis of observational studies in epidemiology and preferred reporting items for systematic reviews and meta-analyses where appropriate [16, 17].
The following information was extracted from each of the article, cross-checked by the second author and the last author, and recorded on a standardized electronic data collation form: (a) publication details (names of the authors and year of publication), (b) the number of medical students diagnosed with IA, (c) the total sample size for each study, (d) the mean age of participants, (e) the proportion of male and female participants, and (f) the name of assessment questionnaire used to assess IA, and (g) the mean IA score of all participants.
All statistical analysis was performed using the Comprehensive Meta-Analysis Version 2.0 based on random-effects model and methods established by previous studies [18,19,20]. The random-effect model was used because it assumes varying effect sizes between studies, because of differing study design and study population [21]. The assumption of homogeneity of effect sizes, that is, τ 2 = 0, can be tested by a chi-square statistic which is usually known as the Q statistic [22]. Between-study heterogeneity was assessed with the I 2 statistic, which describes the percentage of variability among effect estimates beyond that expected by chance [23]. As a reference, I 2 values of 25% are considered low, 50% moderate, and 75% high heterogeneity [24].
Meta-regression was performed to identify demographic and disease-related factors that might contribute to the heterogeneity [25] and predict the effective size [26]. The regression coefficients and the associated z values and p values were reported in the meta-regression analysis [27]. Subgroup analysis was undertaken to investigate the effects of categorical variables on the pooled prevalence of IA. We compared the prevalence of IA between subgroups based on the questionnaires used to assess IA.
Egger’s regression test was conducted to determine if publication bias was present [28]. If significant publication bias was present, the classic fail-safe test was performed to determine the number of missing studies that are required in order for the p value of the publication bias among the observed studies to be higher than 0.05.
Results
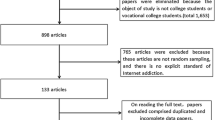
A cumulative total of 129 citations were identified using the search strategy and screened. One hundred fourteen articles were excluded because these studies recruited non-medical university students or failed to provide sufficient data to calculate effect size. Fifteen articles were further reviewed based on inclusion and exclusion criteria. One article was excluded because it did not provide access to the full text. Three studies were excluded because they included subjects who were studying in basic medical science but not medicine. One study was excluded because it included postgraduate students. The final data set consisted of 10 studies with a total of 3651 participants. The characteristics of studies included are described in Table 1.
The pooled prevalence of IA among 3651 medical students is 30.1% (95% confidence interval 28.5–31.8%, Z = −20.66, df = 9, τ 2 = 0.90, I 2 = 98.12). This meta-analysis demonstrates significant heterogeneity across studies (p < 0.0001). Figure 1 shows the forest plot generated for the pooled prevalence of IA among medical students. The meta-regression analyses show that the mean age of the medical students (β = 0.13, 95% CI = −0.94–1.21, Z = 0.24, p = 0.81), gender proportion of male medical students (β = 0.0091, 95% CI = −0,084–0.10, Z = −0.19, p = 0.85), and severity of IA (β = 0.13, 95% CI = −0.036–030, Z = 1.53, p = 0.12) are not significant moderators accounting for heterogeneity. Based on the subgroup analysis, the pooled prevalence of IA diagnosed using the CIAS (5.2, 95% CI 3.4–8.0%) is significantly lower than YIAT (32.2, 95% CI 20.9−45.9%) (p < 0.0001). For publication bias, the Egger’s regression test shows that publication bias is not significant in this meta-analysis (intercept = −3.55, 95% CI−21.4–14.25, t = 0.46, df = 8, p = 0.657).
Discussion
To our knowledge, this is the first meta-analysis that examined the prevalence of IA among medical students in different countries. Our most important result is that the prevalence of IA among 3651 medical students is 30.1%. In one meta-analysis, the global prevalence of IA among the general population was found to be 6% in 31 different countries [4]. In another study, the prevalence of IA among adolescents assessed by the YIAT was found to be 5% in six different Asian countries [38]. This meta-analysis highlights that the prevalence rate of IA among medical students was almost five times higher than that of the general population. The prevalence of IA was higher than global prevalence of depression in medical students which is 28.0% [14]. The high prevalence rate of IA is a major concern because medical students are trained to become health professionals. IA may affect patient safety [10] because it is associated with cognitive impairment [4]. Such impairment can affect medical student’s abilities to concentrate during academic study or clinical placement [39]. Furthermore, IA is associated with poor quality of life [40]. There are several reasons that account for higher prevalence of IA among medical students. First, the accessibility hypothesis suggests that medical students are more vulnerable to IA due to frequent use of the Internet to search for medical information as well as participating in online learning and assessment [8]. Second, medical students may immerse themselves into the virtual reality of the Internet to escape from academic stress [41]. Third, the use of the Internet as a coping strategy for negative psychological states (e.g., stress or depression) may perpetuate IA because students suffering from IA often avoid socialization with other people [1].
Meta-regression analyses demonstrate that continuous variables such as mean age, proportion of gender, and severity of IA are not significant moderators and do not account for the heterogeneity in the pooled prevalence of IA among medical students. Our findings suggest that gender may not play a key role in IA. This can be an emerging trend when both genders have equal access to the Internet [40], especially for medical students. The subgroup analysis demonstrates that there is a significant difference in the prevalence of IA between participants assessed by YIAT and CIAS; therefore, the questionnaires assessing IA is a potential source of heterogeneity. Previous study advised researchers to interpret the prevalence of IA assessed by the CIAS with caution because it was validated in Chinese population but not in other populations [38, 43]. In this meta-analysis, the study which used CIAS was conducted in Iran.
This meta-analysis has several limitations. First, we did not have information on other factors including the purpose of using the Internet (e.g., playing online games, usage of social media), the percentage of individuals who have access to the Internet in each country of study, quality of life of participants, family history of addiction, and academic performance [4, 44]. These factors could influence the pooled prevalence of IA. Second, this meta-analysis is based on six different countries (3 studies from Iran, 2 studies from India, 2 studies from Malaysia, 1 study from Chile, 1 study from Greece and 1 study from Thailand). We could not locate studies conducted in Australia, East Asia, Europe, and North America during our search. This limitation is noteworthy because it limits the generalizability of results. Further studies focusing on the prevalence of IA among medical students are required from these continents. Third, the studies included in this meta-analysis are cross-sectional and this meta-analysis is not able to demonstrate causality or temporal association between IA and undergraduate medical studies. Fourth, we could not perform subgroup analysis to compare the prevalence of IA between medical students from junior and senior years.
Our results have implications for administrators and medical teachers in medical schools. The high prevalence of IA among medical students suggest that medical teachers should be able to recognize signs of IA including inability to reduce internet use, psychological dependency, and withdrawal symptoms [1]. Prompt recognition of IA will facilitate referral for early intervention by mental health professionals. Early intervention can prevent further deterioration of IA and potential negative impact on quality of life [40]. Given the association between IA and other psychiatric disorders, it is of importance to screen for other psychiatric comorbidity including depression and sleep deprivation when assessing medical students suffering from IA. University students found IA as key factor for sleep deprivation [1] because students stay awake during late night hours to surf the Internet [42]. For medical students, the lack of sleep may lead to lack of concentration in lectures, tutorials, and bedside teaching. In addition, sleep deprivation is associated with impairment in executive functioning [45]. Such impairment is detrimental to medical students and junior doctors because it affects decision-making ability and patient safety [10]. Medical educators should increase the awareness of IA among medical students by teaching about IA in undergraduate psychiatry courses. Mental health professionals can offer motivational interviewing, cognitive behaviour therapy, virtual-reality therapy [46] and psychotropic medications to treat psychiatric comorbidity associated with IA.
In conclusion, this meta-analysis reports that the pooled prevalence of IA among medical students from different countries is 30.1%, which is approximately five times than that of the general population. Age, gender, and severity of IA cannot explain high heterogeneity in prevalence, but IA assessment questionnaire are a potential source of heterogeneity. Given the high prevalence of IA, medical teachers and medical school administrators should identify medical students suffering from IA and refer them for intervention. The undergraduate psychiatric curriculum should cover IA and increase the awareness of IA among medical students.
References
Li W, O’Brien JE, Snyder SM, Howard MO. Characteristics of internet addiction/pathological internet use in U.S. university students: a qualitative-method investigation. PLoS One. 2015;10(2):e0117372. doi:10.1371/journal.pone.0117372.
Should PR. DSM-V Designate “Internet Addiction” a mental disorder? Psychiatry (Edgmont). 2009;6(2):31–7.
Widyanto L, Griffiths MD. “Internet Addiction”: a critical review. Int J Ment Heal Addict. 2006;4:31–51. doi:10.1007/s11469-006-9009-9.
Cheng C, Li AY. Internet addiction prevalence and quality of (real) life: a meta-analysis of 31 nations across seven world regions. Cyberpsychol Behav Soc Netw. 2014;17(12):755–60. doi:10.1089/cyber.2014.0317.
Ho RC, Zhang MW, Tsang TY, Toh AH, Pan F, Lu Y, et al. The association between internet addiction and psychiatric co-morbidity: a meta-analysis. BMC Psychiatry. 2014;14:183. doi:10.1186/1471-244X-14-183.
Kawabe K, Horiuchi F, Ochi M, Oka Y, Ueno S. Internet addiction: prevalence and relation with mental states in adolescents. Psychiatry Clin Neurosci. 2016;70(9):405–12. doi:10.1111/pcn.12402.
Bhandari PM, Neupane D, Rijal S, Thapa K, Mishra SR, Poudyal AK. Sleep quality, internet addiction and depressive symptoms among undergraduate students in Nepal. BMC Psychiatry. 2017;17(1):106. doi:10.1186/s12888-017-1275-5.9.
Fatehi F, Monajemi A, Sadeghi A, Mojtahedzadeh R, Mirzazadeh A. Quality of life in medical students with Internet addiction. Acta Med Iran. 2016;54(10):662–6. doi:10.4103/0253-7176.92068.
Christakis DA, Moreno MM, Jelenchick L, Myaing MT, Zhou C. Problematic internet usage in US college students: a pilot study. BMC Med. 2011;9:77. doi:10.1186/1741-7015-9-77.
Younes F, Halawi G, Jabbour H, El Osta N, Karam L, Hajj A, et al. Internet addiction and relationships with insomnia, anxiety, depression, stress and self-esteem in university students: a cross-sectional designed study. PLoS One. 2016;11(9):e0161126. doi:10.1371/journal.pone.0161126.
Ho RC, Ong HS, Kudva KG, Cheung MW, Mak A. How to critically appraise and apply meta-analyses in clinical practice. Int J Rheum Dis. 2010;13(4):294–9. doi:10.1111/j.1756-185X.2010.01560.x.
Mak A, Cheung MW, Fu EH, Ho RC. Meta-analysis in medicine: an introduction. Int J Rheum Dis. 2010;13(2):101–4. doi:10.1111/j.1756-185X.2010.01471.x.
Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000–2015]. Ann Transl Med. 2016;4(4):72. doi:10.3978/j.issn.2305-5839.2016.02.07.
Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016 Apr;50(4):456–68. doi:10.1111/medu.12962.
Ho RC, Cheung MW, Fu E, Win HH, Zaw MH, Ng A, et al. Is high homocysteine level a risk factor for cognitive decline in elderly? A systematic review, meta-analysis, and meta-regression. Am J Geriatr Psychiatry. 2011;19(7):607–17. doi:10.1097/JGP.0b013e3181f17eed.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Mak A, Cheung MW, Chiew HJ, Liu Y, Ho RC. Global trend of survival and damage of systemic lupus erythematosus: meta-analysis and meta-regression of observational studies from the 1950s to 2000s. Semin Arthritis Rheum. 2012;41(6):830–9. doi:10.1016/j.semarthrit.2011.11.002.
Zhang MW, Ho RC, Cheung MW, Fu E, Mak A. Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry. 2011;33(3):217–23. doi:10.1016/j.genhosppsych.2011.03.009.
Lu Y, Mak KK, van Bever HP, Ng TP, Mak A, Ho RC. Prevalence of anxiety and depressive symptoms in adolescents with asthma: a meta-analysis and meta-regression. Pediatr Allergy Immunol. 2012;23(8):707–15. doi:10.1111/pai.12000.
Loh AZ, Tan JS, Zhang MW, Ho RC. The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J Am Med Dir Assoc. 2017;18(2):111–6. doi:10.1016/j.jamda.2016.08.014.
Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. 2017;18(7):742–54. doi:10.1111/obr.12535.
Cheung MW, Ho RC, Lim Y, Mak A. Conducting a meta-analysis: basics and good practices. Int J Rheum Dis. 2012 Apr;15(2):129–35. doi:10.1111/j.1756-185X.2012.01712.x.
Yeo LL, Ho R, Paliwal P, Rathakrishnan R, Sharma VK. Intravenously administered tissue plasminogen activator useful in milder strokes? A meta-analysis. J Stroke Cerebrovasc Dis. 2014;23(8):2156–62. doi:10.1016/j.jstrokecerebrovasdis.2014.04.008.
Mak KK, Kong WY, Mak A, Sharma VK, Ho RC. Polymorphisms of the serotonin transporter gene and post-stroke depression: a meta-analysis. J Neurol Neurosurg Psychiatry. 2013;84(3):322–8. doi:10.1136/jnnp-2012-303791.
Mak A, Liu Y, Ho RC. Endothelium-dependent but not endothelium-independent flow-mediated dilation is significantly reduced in patients with systemic lupus erythematosus without vascular events: a meta-analysis and meta-regression. J Rheumatol. 2011;38(7):1296–303. doi:10.3899/jrheum.101182.
Mak A, Cheung MW, Cheak AA, Ho RC. Combination of heparin and aspirin is superior to aspirin alone in enhancing live births in patients with recurrent pregnancy loss and positive anti-phospholipid antibodies: a meta-analysis of randomized controlled trials and meta-regression. Rheumatology (Oxford). 2010;49(2):281–8. doi:10.1093/rheumatology/kep373.
Ho RC, Thiaghu C, Ong H, Lu Y, Ho CS, Tam WW, et al. A meta-analysis of serum and cerebrospinal fluid autoantibodies in neuropsychiatric systemic lupus erythematosus. Autoimmun Rev. 2016 Feb;15(2):124–38. doi:10.1016/j.autrev.2015.10.003.
Ho RC, Ong H, Thiaghu C, Lu Y, Ho CS, Zhang MW. Genetic variants that are associated with neuropsychiatric systemic lupus erythematosus. J Rheumatol. 2016;43(3):541–51. doi:10.3899/jrheum.150884.
Nath K, Naskar S, Victor R. A CrossSectional Study on the Prevalence, Risk Factors, and Ill Effects of Internet Addiction Among MedicalStudents in Northeastern India. Prim Care Companion CNS Disord. 2016;18(2). doi:10.4088/PCC.15m01909.
Berner JE, Santander J, Contreras AM, Gómez T. Description of internet addiction among Chilean medical students: a crosssectional study. Acad Psychiatry. 2014;38(1):114. doi:10.1007/s4059601300226.
Tsimtsiou Z, Haidich AB, Spachos D, Kokkali S, Bamidis P, Dardavesis T, Arvanitidou M. Internet addiction in Greek medical students: an online survey. Acad Psychiatry. 2015;39(3):3004. doi:10.1007/s405960140273x.
Chaudhari B, Menon P, Saldanha D, Tewari A, Bhattacharya L. Internet addiction and its determinants among medical students. Ind Psychiatry J. 2015;24(2):15862. doi:10.4103/09726748.181729.
Ghamari F, Mohammadbeigi A, Mohammadsalehi N, Hashiani AA. Internet addiction and modeling its risk factors in medical students, iran. Indian J Psychol Med. 2011;33(2):15862. doi:10.4103/02537176.92068.
Salehi M, Norozi Khalili M, Hojjat SK, Salehi M, Danesh A. Prevalence of internet addiction and associated factors among medical students from mashhad, iran in2013. Iran Red Crescent Med J. 2014;16(5):e17256. doi:10.5812/ircmj.17256.
Haque M, Rahman NA, Majumder MA, Haque SZ, Kamal ZM, Islam Z, Haque AE, Rahman NI, Alattraqchi AG. Internet use and addiction among medical students of Universiti Sultan Zainal Abidin, Malaysia. Psychol Res Behav Manag. 2016;14(9):297-307. eCollection 2016.
Ching SM, Hamidin A, Vasudevan R, Sazlyna MS, Wan Aliaa WS, Foo YL, Yee A, Hoo FK. " Prevalence and factors associated with internet addiction among medical students - A cross-sectional study in Malaysia. Med J Malaysia. 2017;72(1):7-11.
Boonvisudhi T, Kuladee S. A ssociation between Internet addiction and depression in Thai medical students at Faculty of Medicine, Ramathibodi Hospital. PLoS One. 2017 Mar 20;12(3):e0174209. doi:10.1371/journal.pone.0174209.
Mak KK, Lai CM, Watanabe H, Kim DI, Bahar N, Ramos M, et al. Epidemiology of Internet behaviors and addiction among adolescents in six Asian countries. Cyberpsychol Behav Soc Netw. 2014;17(11):720–8. doi:10.1089/cyber.2014.0139.
Carr N. The shallows: what the internet is doing to our brains. New York: W.W. Norton & Company; 2011.
Tran BX, Huong LT, Hinh ND, Nguyen LH, Le BN, Nong VM, et al. A study on the influence of internet addiction and online interpersonal influences on health-related quality of life in young Vietnamese. BMC Public Health. 2017;17(1):138. doi:10.1186/s12889-016-3983-z.
Zhang MW, Ho RC. Smartphone applications for immersive virtual reality therapy for internet addiction and internet gaming disorder. Technol Health Care. 2017;25(2):367–72. doi:10.3233/THC-161282.
Frangos CC, Frangos CC, Sotiropoulos I. Problematic Internet use among Greek university students: an ordinal logistic regression with risk factors of negative psychological beliefs, pornographic sites, and online games. Cyberpsychol Behav Soc Netw. 2011;14(1–2):51–8. doi:10.1089/cyber.2009.0306.
Lai CM, Mak KK, Watanabe H, Ang RP, Pang JS, Ho RC. Psychometric properties of the internet addiction test in Chinese adolescents. J Pediatr Psychol. 2013;38(7):794–807. doi:10.1093/jpepsy/jst022.
Lam LT. Risk factors of Internet addiction and the health effect of internet addiction on adolescents: a systematic review of longitudinal and prospective studies. Curr Psychiatry Rep. 2014;16(11):508. doi:10.1007/s11920-014-0508-2.
Ling A, Lim ML, Gwee X, Ho RC, Collinson SL, Ng TP. Insomnia and daytime neuropsychological test performance in older adults. Sleep Med. 2016;17:7–12. doi:10.1016/j.sleep.2015.07.037.
Lam LT, Lam MK. Health Intervention for problematic internet use (PIU). Curr Psychiatry Rep. 2016;18(12):107. doi:10.1007/s11920-016-0747-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, M.W.B., Lim, R.B.C., Lee, C. et al. Prevalence of Internet Addiction in Medical Students: a Meta-analysis. Acad Psychiatry 42, 88–93 (2018). https://doi.org/10.1007/s40596-017-0794-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40596-017-0794-1