Abstract
Background
Sedentary behavior is a significant health risk. Emerging research suggests that mentally active sedentary behaviors (e.g., computer use and reading) are associated with better health than mentally passive sedentary behaviors (e.g., watching TV). However, these relationships are not well established in the literature, and little is known about the oldest old (age ≥ 80).
Aims
The aims of this study were to (1) identify distinct subgroups of oldest old adults based on six domains of sedentary behavior (watching TV, using a computer/tablet, talking to friends or family members, doing hobby or other activities, transportation, and resting/napping); and (2) compare health-related outcomes across identified subgroups, using the National Health and Aging Trends Study (NHATS) dataset.
Methods
Latent profile analysis was used to identify distinct profiles of sedentary behavior. Design-based linear and logistic regressions were used to examine associations between different profiles and health outcomes, accounting for socio-demographic characteristics.
Results
A total of 852 participants were included. We identified four profiles and named them based on total sedentary time (ST) and passive/active pattern: “Medium-passive”, “High-passive”, “Low”, “High-mentally active”. Compared to the “High-passive” group, “Low” group and “High-mentally active” group were associated with fewer difficulties with activities of daily living, fewer problems limiting activities and higher cognitive function.
Conclusion
This study, with a national representative sample of the oldest old population, suggests that both total ST and sedentary behavior pattern matter when evaluating health outcomes of being sedentary. Interventions should encourage oldest old adults to reduce ST and especially target mentally passive ST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Higher sedentary time is associated with poor health outcomes, including cardiovascular disease, cancer, all-cause mortality, cognitive decline, frailty, and poorer physical function [1,2,3,4]. Sedentary behavior is defined as any behavior in a sitting or lying position with an energy expenditure ≤ 1.5 metabolic equivalents [5]. Adults aged 80 and older, referred to as the oldest old, tend to spend large amounts of time in sedentary behaviors [6]. Recent studies have explored the health effects of different types of sedentary behavior in older adults (≥ 60 years) [7, 8], however, these relationships are not well established and little is known about the patterns of sedentary behavior among oldest old adults.
Some sedentary behaviors involve cognitive engagement and can be classified as mentally active, while other sedentary behaviors are mentally passive [9, 10]. Mentally passive sedentary behaviors include watching television (TV), sitting around, and listening or talking while sitting [11]. Mentally active sedentary behaviors include using a computer and hobbies such as reading, playing games, or doing crafts [11]. Evidence suggests that mentally passive sedentary behaviors are associated with more depressive symptoms in adults and worse cognitive function and higher psychological distress in older adults, while mentally active sedentary behaviors may reduce depression and improve cognitive performance [11,12,13]. Higher TV viewing time has been associated with worse cardiometabolic outcomes in older adults [7, 11, 14, 15]. In these studies, mentally active sedentary behavior was either not associated with cardiometabolic outcomes or was associated with better outcomes (lower BMI) [7, 11, 14, 15] although the association with weight may change when mentally active sedentary behavior exceeds 3 h per day [11]. In addition, less time spent watching TV and more time in mentally active sedentary behaviors may contribute to successful aging (fewer health deficits) [16]. Only one known study has examined specific domains of sedentary behavior in an oldest old population, this study focused solely on the outcome of psychological distress [17].
Understanding how different types of sedentary behavior cluster and how different profiles are related to socio-demographic characteristics and health outcomes beyond psychological distress in oldest old adults could have important implications for designing interventions to reduce specific types of sedentary behavior associated with harmful health effects. The aims of this study were to (1) use latent profile analysis to identify distinct groups of older adults (≥ 80 years) with similar sedentary behavior based on time spent in six domains of sedentary behavior (watching TV, using a computer/tablet, talking to friends or family members, doing hobbies or other activities, transportation, and resting/napping); and (2) compare socio-demographic characteristics and health-related outcomes across identified groups, using the nationally representative National Health and Aging Trends Study (NHATS) dataset.
Methods
Data sources and study population
The NHATS dataset is a national longitudinal cohort study with annual survey waves of Medicare beneficiaries aged 65 and older living in the community, residential care, and nursing homes [18]. Data have been collected since 2011 from a sample of respondents (Round 1), and in 2015, the sample was replenished (Round 5). In both Rounds 1 and 5, participants were selected using a stratified three-stage sample design with oversampling of older persons (aged 90 and older) and Black non-Hispanic individuals [18]. In each round, an analytic weight was calculated by the NHATS leadership which accounted for differential probabilities of selection and adjusted for potential bias related to unit nonresponse. The weighted response rate at each round ranged from 71.5 to 96% [18].
The current study analyzed data from Round 6 of the NHATS which was collected in 2016. In Round 6, 7276 interviews were completed. A random subset comprising one-third of participants were asked questions about sedentary behavior (n = 2141). Participants who were at least 80 years old in Round 6 and had complete data on six domains of sedentary behavior were eligible for inclusion. A total of 1289 were excluded from the 2141 respondents: 1158 were younger than 80 years old and 131 did not have complete information about sedentary behaviors, leaving a study sample of 852 participants.
Measures
Sedentary behaviors were assessed using questionnaire items modeled after existing instruments [19], Dori E. [20]. These items measured time spent on six types of sedentary behavior, including (1) sitting or lying down to watch TV, (2) sitting and using a computer or tablet, (3) sitting and talking to friends or family members, (4) sitting to do hobbies or other activities such as reading, playing cards, puzzles, or crafts, (5) driving or riding somewhere as a passenger, and (6) laying down to rest or take a nap. Participants were asked “how many of the last 7 days”, “how many hours on a typical day” and “how many minutes on a typical day (if less than 1 h)” they spent in each sedentary behavior. For each sedentary behavior, sedentary time was computed as number of days/week multiplied by number of h/day. Total sedentary time was calculated as the sum of time spent on all six types of sedentary behavior per week. Some of the six sedentary behaviors have been characterized in the literature as mentally passive (watching TV, talking, resting/napping) or mentally active (computer use, hobbies), while other sedentary behaviors are not as well defined [11].
We analyzed five socio-demographic characteristics including: (1) age (measured in 5-year bands), (2) sex, (3) race/ethnicity, (4) educational level, and (5) marital status. We analyzed seven health-related outcomes. Self-rated health was rated as excellent, very good, good, fair, or poor. Body mass index (BMI) (calculated based on self-reported height and weight) was used both as a continuous measure and to categorize participants as underweight, normal, overweight, or obese. Number of chronic conditions was based on self-reports of the following chronic conditions: heart attack, heart disease, blood pressure, arthritis, osteoporosis, diabetes, lung, stroke, dementia and cancer. Number of difficulties in activities of daily living (ADL) was based on validated items assessing difficulty with the following activities: eating, showering or bathing, using the toilet, getting dressed, getting out of bed, and getting around inside the home [21]. Number of problems limiting activities was based on self-reports of the following problems: pain, breathing, upper body strength, lower body strength, low energy, and balance coordination problems. A depression and anxiety score was obtained by summing responses for the two items in Patient Health Questionnaire-2 and two items in the Generalized Anxiety Disorder-2 scale [22, 23]. The total depression and anxiety score ranged from 4 to 16, with a higher score indicating poorer mental health. Cognitive function was assessed using immediate word recall score, which ranged from 0 to 10 with a higher score indicating better cognitive function [24].
Statistical analysis
The final sample included 852 participants (≥ 80 years) who had complete data on all six types of sedentary behaviors. To identify profiles/groups of people with similar patterns of sedentary behavior, we conducted an exploratory (with no covariates) Latent Profile Analysis (LPA) using Mplus version 8.0. To select an optimal number of profiles/groups, the model fit was assessed using the Bayesian Information Criterion (BIC), Vuong–Lo–Mendell–Rubin Likelihood Ratio Test (VLMR), Lo–Mendell–Rubin adjusted likelihood ratio test (LRT), and entropy measures. The best fit was determined by a low BIC to indicate a good fit and high entropy to indicate a good separation of the latent profiles/groups; significant VLMR and LRT tests were also assessed to compare adjacent lower and higher order class solutions (e.g., 3-class solution versus 2-class solution) to determine the optimal number of groups [25, 26, 26, 27, 27]. The resulting groups were then profiled and defined based on their overall level of sedentary time and the types of sedentary behavior where they spent the most time.
Once the profiles were defined, we used Stata/SE 17.0 software to compare the sedentary time, socio-demographic, and health-related outcomes across the identified subgroups of sedentary behavior. The complex sample design (stratification and primary sampling units) and sampling weights in Round 6 were accounted for in the analyses. Taylor series linearization methods were used for variance estimation. A subpopulation of participants who were aged ≥ 80 and who had completed all six sedentary behavior items was created (n = 852), while accounting for the full sample design. Descriptive statistics (percentages for categorical variables, means and standard errors for continuous variables) were calculated to summarize the sedentary time, socio-demographic, and health-related outcomes. Bivariate analyses were used to compare the socio-demographic and health-related outcomes of different groups; bivariate differences were assessed with Rao–Scott Chi-square tests for categorical variables and design-based F-tests for continuous variables. To control for socio-demographic characteristics (age, sex, race/ethnicity, educational level, marital status), we conducted design-based linear regression analyses to determine whether BMI, the number of chronic conditions, number of difficulties in ADL, number of problems limiting activities, anxiety and depression, and word recall were different among groups. The adjusted coefficients and 95% confidence intervals (95% CI) were provided. We also conducted design-based logistic regression analyses to determine whether the self-rated health (excellent or not) was different among groups, controlling for socio-demographic characteristics. The adjusted odds ratios (aOR) and 95% CI were calculated.
Results
Characteristics of study population
Fifty percent of the participants were 80–84 years old. Most were female (59.68%), Non-Hispanic White (83.76%), single/divorced/widowed (58.17%), overweight/obese (57.31%), reported excellent/very good/good health (72.34%), and did not obtain college degree (78.38%). They reported an average of 2.77 chronic conditions, 0.96 difficulties with ADL, and 1.48 problems limiting activities. Their average depression and anxiety score was 6.04 (score range 4–16) and average word recall was 4.01 (score range 0–10) (see Table 1).
Identified groups
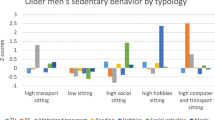
Overall, individuals reported a total of 46.86 ± 1.07 h/week sedentary time (TV = 16.91 ± 0.57; talking = 8.66 ± 0.33; computer = 3.68 ± 0.32; hobbies = 8.65 ± 0.38; transportation = 4.17 ± 0.19; resting = 4.77 ± 0.33). The results of the LPA indicated that a four-class solution provided both optimal fit and an interpretable number of distinct groups/profiles based on the six different types of sedentary behavior (see Supplemental Table 1 for detail). Figures 1 and 2 show group profiles based on the composite sedentary behavior score and the six different types of sedentary behavior. In terms of total sedentary time, Group 2 and Group 4 were high (74–84 h/week), Group 1 was medium (62.5 h/week), and Group 3 was low (34 h/week). In terms of sedentary behavior pattern (mentally active/passive), Group 1 was high in passive sedentary behavior (TV), Group 2 was high in passive sedentary behavior (TV, talking, resting), Group 3 was low in all sedentary behavior, and Group 4 was high in mentally active sedentary time (computer, hobbies). Based on the total sedentary time and sedentary behavior pattern, Group 1 was named “medium-passive”, Group 2 was named “high-passive”, Group 3 was named “low”, and Group 4 was named “high-mentally active”.
Differences in socio-demographic and health-related outcomes across subgroups
Table 1 compares socio-demographic and health-related outcomes across the four subgroups. Compared to Group 3 “low” and 4 “high-mentally active”, individuals in Group 1 “medium-passive” and 2 “high-passive” were older, had lower education levels, were more likely to report poor health, report more difficulties with ADL, report more problems limiting activities, and had lower cognitive function (recalled fewer words). In addition, individuals in Group 1 “medium-passive” reported more chronic conditions compared to Group 3 “low”; Individuals in Group 1 “medium-passive” and 2 “high-passive” had higher depression and anxiety scores compared to Group 4 “high-mentally active”.
Table 2 and Supplemental Table 2 show the relationships between identified subgroups and health-related outcomes, controlling for socio-demographic characteristics. Linear regression models showed that membership in Group 3 “low” and 4 “high-mentally active” were associated with fewer difficulties with ADL, fewer problems limiting activities, and better cognitive function/higher word recall, compared to Group 2 “high-passive”. In addition, membership in Group 4 “high-mentally active” was associated with lower depression and anxiety scores compared to Group 2 “high-passive”. Identified subgroups were not associated with BMI or number of chronic conditions. Logistic regression model showed that individuals in Group 3 “low” and 4 “high-mentally active” were more likely to report excellent health, compared to Group 2 “high-passive”.
Discussion
We identified four subgroups of oldest old adults based on their different levels and types of sedentary behavior (mentally active vs. passive). We demonstrated that both total sedentary time and the type of sedentary behavior matter when evaluating health outcomes of sedentary behavior in the oldest older adults. For example, individuals with high total sedentary time but a mentally active pattern may have fewer difficulties with ADLs, fewer problems limiting activities, lower anxiety and depression and higher cognitive function, compared to individuals with high total sedentary time but a passive pattern. Based on our review of published literature, this is the first analysis to examine associations between different sedentary profiles (total sedentary time and passive/mentally active pattern) and health-related outcomes in a nationally representative sample of the oldest old population.
We found that individuals with low total sedentary time reported better physical and cognitive outcomes. This confirms findings from previous studies, and it is well established that low sedentary time is protective [28, 29]. Total sedentary time in the oldest old was lower in this study compared to other studies with objective measures. A recent meta-analysis found that oldest old adults are sedentary for an average of 10.6 h/day when sedentary behavior is measured with objective devices [6]. This is not surprising considering underestimation of self-reported sedentary time is common [30], and sedentary behaviors may go beyond the six sedentary behaviors measured in this study, such as time on telephone or public transport.
In addition to total sedentary time, our study also supported the relationships between sedentary pattern (passive versus mentally active) and three health outcomes, cognitive performance, mental health, and physical performance. These relationships are not well established in the literature; this study confirms the relationship using a nationally representative dataset and extends findings from general older adults to the oldest old. Given the cross-sectional nature of analysis, we could not clarify the direction of these relationships. Better cognitive or physical function and mental health could increase the ability or willingness to engage in mentally active sedentary behaviors [16, 31]. Conversely, mentally active sedentary pattern could contribute to better cognitive, mental, and physical health outcomes, as discussed below.
First, we found that a mentally active sedentary pattern was associated with better cognitive performance, which is consistent with a prior study in general older adults [13]. The cognitive stimulation required by mentally active sedentary activities may reduce cognitive decline, potentially by building cognitive reserve [7, 13]. Second, we observed that a mentally active sedentary pattern was associated with lower anxiety and depression compared to a passive pattern. This result is in line with prior studies in adults and older adults which found that passive sedentary behavior is associated with depression and lower mental health-related quality of life [7, 9, 9, 10, 10]. Common passive sedentary behaviors such as TV watching may be more socially isolating and contribute to negative ruminations more than mentally active sedentary behaviors [9, 10].
In addition, we found that a passive sedentary pattern was associated with more difficulty with ADLs and problems limiting activities. Prior research regarding the relationship between passive sedentary time and physical function has been inconsistent. Some reported that higher passive sedentary behaviors were associated with worse physical performance (e.g., grip strength, walking, agility) and frailty in older adults, while mentally active sedentary behaviors were associated with better physical function [7, 32] or had no relationship with physical function [33], D. E. [34]. Higher passive sedentary behaviors in adults 60 and older contributes to accelerated accumulation of functional and mental health deficits, an indicator of less successful aging [16]. In contrast, one study found that measures of physical performance were not associated with different types of sedentary behaviors in adults 65 and older [35] and another study found that not watching TV was associated with disability [36]. It is not well understood why different types of sedentary behavior may differentially affect physical health and function because all sedentary behaviors involve muscular inactivity. One explanation is that TV viewing may be more harmful to physical health than other sedentary behaviors because it is associated with unhealthy eating habits [7].
In our study, those with higher educational level tended to spend more time in mentally activity sedentary behavior. This is in line with previous research indicating that TV viewing time is greater in adults with lower education, while higher education is associated with increased computer use (a mentally active sedentary behavior) [37].
We are not aware of other studies reporting sedentary times within different domains for oldest old adults, but studies of adults aged 60 and older have reported similar amounts of time spent watching TV, using a computer, reading/doing hobbies, and in transportation as we found here in adults aged 80 and older. [7, 11, 13, 14, 38]. TV watching time is typically the most prevalent sedentary behavior in older adults and this is consistent with our findings in the oldest old [7, 11, 13, 38, 39]. In our analysis, time spent talking was higher than previous studies that reported time socializing in adults aged 60 and older (1.24 vs. 0.5–0.8 h/day) [7, 14].
The above findings highlight the importance of assessing various domains of sedentary behavior in addition to overall sedentary time in research and practice. Future research may consider measuring total sedentary time with objective measures and sedentary context with self-reported measures. Future research is needed to establish differential health effects of various sedentary activities in oldest old adults and establish directions of causality.
In terms of practical implementation, more harmful types of sedentary behavior such as TV watching could be specifically targeted through interventions, e.g., using TV control devices to restrict access to TV [40]. TV watching presents an important opportunity for reducing sedentary time as it is often the most common sedentary behavior and has been consistently associated with worse health outcomes. Interventions also could be tailored for individuals according to their baseline patterns of sedentary behavior, such as the types of subgroups identified in this analysis. Future policies could encourage oldest old adults to reduce sedentary time and especially target mentally passive sedentary time.
This study had some strengths and limitations. The use of a nationally representative dataset was a major strength as the results are generalizable to the oldest old adults in the United States. As mentioned above, the cross-sectional analysis prevents us from drawing conclusions about the direction of the relationships between domains of sedentary behavior and the health-related outcomes. In addition, the self-report measures of sedentary behavior are not as accurate as objectively measured sedentary behavior, although necessary for assessing specific domains of sedentary behavior. Cognitive function may have also influenced the accuracy of self-reported sedentary behavior.
Conclusion
Despite the limitations, this study is the first to identify subgroups of the oldest old adults based on distinct sedentary behavior profiles using a nationally representative sample. Individuals with higher sedentary time and a passive sedentary behavior pattern tend to report worse health, more difficulty with ADLs, more problems limiting activities, higher anxiety, and depression and fewer word recall. Our study suggests that interventions may focus on overall sedentary time reduction, as well as target more harmful sedentary behaviors (e.g., TV viewing) to promote healthier aging.
Data availability
The NHATS data analyzed in the current study are publicly available for research purposes at www.nhats.org.
References
Biswas A, Oh PI, Faulkner GE et al (2015) Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 162:123–132. https://doi.org/10.7326/M14-1651
Mañas A, del Pozo-Cruz B, García-García FJ et al (2017) Role of objectively measured sedentary behaviour in physical performance, frailty and mortality among older adults: a short systematic review. Eur J Sport Sci 17:940–953. https://doi.org/10.1080/17461391.2017.1327983
Mañas A, Del Pozo-Cruz B, Rodríguez-Gómez I et al (2019) Dose-response association between physical activity and sedentary time categories on ageing biomarkers. BMC Geriatr 19:270. https://doi.org/10.1186/s12877-019-1284-y
Rojer AGM, Reijnierse EM, Trappenburg MC et al (2018) Instrumented assessment of physical activity is associated with muscle function but not with muscle mass in a general population. J Aging Health 30:1462–1481. https://doi.org/10.1177/0898264317721554
Tremblay MS, Aubert S, Barnes JD et al (2017) Sedentary behavior research network (SBRN)—terminology consensus project process and outcome. Int J Behav Nutr Phys Act 14:1–17. https://doi.org/10.1186/s12966-017-0525-8
Webster KE, Zhou W, Gallagher NA et al (2021) Device-measured sedentary behavior in oldest old adults: a systematic review and meta-analysis. Prev Med Rep 23:101405. https://doi.org/10.1016/j.pmedr.2021.101405
Compernolle S, De Bourdeaudhuij I, Cardon G et al (2021) Sex-specific typologies of older adults’ sedentary behaviors and their associations with health-related and socio-demographic factors: a latent profile analysis. BMC Geriatr 21:66. https://doi.org/10.1186/s12877-021-02011-5
Taylor WC (2022) Understanding variations in the health consequences of sedentary behavior: a taxonomy of social interaction, novelty, choice, and cognition. J Aging Phys Act 30:153–161. https://doi.org/10.1123/japa.2020-0360
Hallgren M, Dunstan DW, Owen N (2020) Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev 48:20–27. https://doi.org/10.1249/jes.0000000000000211
Hallgren M, Nguyen TT, Owen N et al (2020) Cross-sectional and prospective relationships of passive and mentally active sedentary behaviours and physical activity with depression. Br J Psychiatry 217:413–419. https://doi.org/10.1192/bjp.2019.60
Kikuchi H, Inoue S, Sugiyama T et al (2014) Distinct associations of different sedentary behaviors with health-related attributes among older adults. Prev Med 67:335–339. https://doi.org/10.1016/j.ypmed.2014.08.011
Huang Y, Li L, Gan Y et al (2020) Sedentary behaviors and risk of depression: a meta-analysis of prospective studies. Transl Psychiatry 10:26. https://doi.org/10.1038/s41398-020-0715-z
Kesse-Guyot E, Charreire H, Andreeva VA et al (2012) Cross-sectional and longitudinal associations of different sedentary behaviors with cognitive performance in older adults. PLoS One 7:e47831. https://doi.org/10.1371/journal.pone.0047831
Hsueh MC, Liao Y, Chang SH (2015) Are total and domain-specific sedentary time associated with overweight in older Taiwanese adults? Int J Environ Res Public Health 12:12697–12705. https://doi.org/10.3390/ijerph121012697
Hsueh MC, Liao Y, Chang SH (2016) Associations of total and domain-specific sedentary time with type 2 diabetes in Taiwanese older adults. J Epidemiol 26:348–354. https://doi.org/10.2188/jea.JE20150095
García-Esquinas E, Ortolá R, Martínez-Gómez D et al (2021) Causal effects of physical activity and sedentary behaviour on health deficits accumulation in older adults. Int J Epidemiol 50:852–865. https://doi.org/10.1093/ije/dyaa228
Štefan L, Baić M, Sporiš G et al (2019) Domain-specific and total sedentary behaviors associated with psychological distress in older adults. Psychol Res Behav Manag 12:219–228. https://doi.org/10.2147/prbm.S197283
Kasper JD, Freedman VA (2020) National Health and Aging Trends Study User Guide: rounds 1–9 beta release. Johns Hopkins University School of Public Health, Baltimore
Gardiner PA, Clark BK, Healy GN et al (2011) Measuring older adults’ sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc 43:2127–2133
Rosenberg DE, Norman GJ, Wagner N et al (2010) Reliability and validity of the sedentary behavior questionnaire (SBQ) for adults. J Phys Act Health 7:697–705. https://doi.org/10.1123/jpah.7.6.697
Freedman VA, Kasper JD, Cornman JC et al (2011) Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J Gerontol A Biol Sci Med Sci 66:1013–1021. https://doi.org/10.1093/gerona/glr087
Kroenke K, Spitzer RL, Williams JBW (2003) The patient health questionnaire-2: validity of a two-item depression screener. Med Care 41:1284–1292
Seo JG, Park SP (2015) Validation of the generalized anxiety disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain 16:97. https://doi.org/10.1186/s10194-015-0583-8
Shankle WR, Romney AK, Hara J et al (2005) Methods to improve the detection of mild cognitive impairment. PNAS 102:4919–4924
Collins LM, Lanza ST (2009) Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences, vol 718. Wiley
McCabe SE, Veliz P, Wilens TE et al (2019) Sources of nonmedical prescription drug misuse among US high school seniors: differences in motives and substance use behaviors. J Am Acad Child Adolesc Psychiatry 58:681–691
McCabe SE, Veliz PT, Dickinson K et al (2019) Trajectories of prescription drug misuse during the transition from late adolescence into adulthood in the USA: a national longitudinal multicohort study. Lancet Psychiatry 6:840–850
Amaral Gomes ES, Ramsey KA, Rojer AGM et al (2021) The association of objectively measured physical activity and sedentary behavior with (instrumental) activities of daily living in community-dwelling older adults: a systematic review. Clin Interv Aging 16:1877–1915. https://doi.org/10.2147/cia.S326686
Rojer AGM, Ramsey KA, Amaral Gomes ES et al (2021) Objectively assessed physical activity and sedentary behavior and global cognitive function in older adults: a systematic review. Mech Ageing Dev 198:111524. https://doi.org/10.1016/j.mad.2021.111524
Dall PM, Coulter EH, Fitzsimons CF et al (2017) TAxonomy of self-reported sedentary behaviour tools (TASST) framework for development, comparison and evaluation of self-report tools: content analysis and systematic review. BMJ Open 7:e013844. https://doi.org/10.1136/bmjopen-2016-013844
Kaye J, Mattek N, Dodge HH et al (2014) Unobtrusive measurement of daily computer use to detect mild cognitive impairment. Alzheimers Dement 10:10
Hamer M, Stamatakis E (2013) Screen-based sedentary behavior, physical activity, and muscle strength in the English longitudinal study of ageing. PLoS One 8:e66222. https://doi.org/10.1371/journal.pone.0066222
García-Esquinas E, Andrade E, Martínez-Gómez D et al (2017) Television viewing time as a risk factor for frailty and functional limitations in older adults: results from 2 European prospective cohorts. Int J Behav Nutr Phys Act 14:54. https://doi.org/10.1186/s12966-017-0511-1
Rosenberg DE, Bellettiere J, Gardiner PA et al (2016) Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. J Gerontol A Biol Sci Med Sci 71:78–83. https://doi.org/10.1093/gerona/glv103
Busschaert C, Scherrens AL, De Bourdeaudhuij I et al (2016) Socio-ecological variables associated with context-specific sitting time in Belgian older adults: a one-year follow-up study. PLoS One 11:e0167881. https://doi.org/10.1371/journal.pone.0167881
Liang Y, Xu X, Yin M et al (2018) A more comprehensive investigation of disability and associated factors among older adults receiving home-based care in rural Dongguan, China. BMC Geriatr 18:158. https://doi.org/10.1186/s12877-018-0852-x
Andrade-Gómez E, García-Esquinas E, Ortolá R et al (2017) Watching TV has a distinct sociodemographic and lifestyle profile compared with other sedentary behaviors: a nationwide population-based study. PLoS One 12:e0188836. https://doi.org/10.1371/journal.pone.0188836
Shibata A, Oka K, Ishii K et al (2019) Objectively-assessed patterns and reported domains of sedentary behavior among Japanese older adults. J Epidemiol 29:334–339. https://doi.org/10.2188/jea.JE20180041
Kasović M, Štefan L, Zvonař M (2020) More time spent in sedentary behaviors is associated with higher plantar pressures in older women. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17062089
Shrestha N, Grgic J, Wiesner G et al (2019) Effectiveness of interventions for reducing non-occupational sedentary behaviour in adults and older adults: a systematic review and meta-analysis. Br J Sports Med 53:1206–1213
Acknowledgements
K. W. is supported by T32NR018407.
Funding
None.
Author information
Authors and Affiliations
Contributions
WZ, KW and JL contributed to the study conception and design. WZ and PL contributed to the data analysis. WZ, KW, PL and JL contributed to the preparation and revision of the manuscript. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
NHATS was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. Informed consent was obtained from the NHATS participants. This current study was exempt from an institutional ethical review because it involved a publicly available, de-identified dataset.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, W., Webster, K.E., Veliz, P.T. et al. Profiles of sedentary behaviors in the oldest old: findings from the National Health and Aging Trends Study. Aging Clin Exp Res 34, 2071–2079 (2022). https://doi.org/10.1007/s40520-022-02157-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02157-1