Abstract
Background
Mild cognitive impairment (MCI) is a cognitive state falling between normal aging and dementia. The relation between alcohol intake and risk of MCI as well as progression to dementia in people with MCI (PDM) remained unclear.
Objective
To synthesize available evidence and clarify the relation between alcohol intake and risk of MCI as well as PDM.
Method
We searched electronic databases consisting of PubMed, EMBASE, Cochrane Library, and China Biology Medicine disc (CBM) from inception to October 1, 2019. Prospective studies reporting at least three levels of alcohol exposure were included. Categorical meta-analysis was used for quantitative synthesis of the relation between light, moderate and heavy alcohol intake with risk of MCI and PDM. Restricted cubic spline and fixed-effects dose–response models were used for dose–response analysis.
Result
Six cohort studies including 4244 individuals were finally included. We observed an unstable linear relation between alcohol intake (drinks/week) and risk of MCI (P linear = 0.0396). It suggested that a one-drink increment per week of alcohol intake was associated with an increased risk of 3.8% for MCI (RR, 1.038; 95% CI 1.002–1.075). Heavy alcohol intake (> 14 drinks/week) was associated with higher risk of PDM (RR = 1.76; 95% CI 1.10–2.82). And we found a nonlinear relation between alcohol intake and risk of PDM. Drinking more than 16 drinks/week (P nonlinear = 0.0038, HR = 1.42; 95% CI 1.00–2.02), or 27.5 g/day (P nonlinear = 0.0047, HR = 1.46; 95% CI 1.00–2.11) would elevate the risk of PDM.
Conclusion
There was a nonlinear dose–response relation between alcohol intake and risk of PDM. Excessive alcohol intake would elevate the risk of PDM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mild cognitive impairment (MCI) is a cognitive state falling between normal aging and dementia [1]. An estimated prevalence of MCI was 6.7–25.2% for ages 60–84 [2]. And progression to dementia in people with MCI (PDM) was conservatively estimated at 5–10% per year in a systematic review and meta-analysis [3]. As no evidence existed to support effective intervention or pharmacologic treatments for MCI [2, 4] and dementia [5, 6], finding the modifying factors of MCI and PDM might be a significant approach for prevention of cognitive dysfunction and dementia.
As a globally consumed beverage, alcohol intake was proved of a modifying factor of dementia in a dose–response meta-analysis [7]. The study found that modest alcohol intake (≤ 12.5 g/day) was associated with a reduced risk of dementia, while heavy drinking (≥ 23 drinks/week or ≥ 38 g/day) would significantly elevate the risk. However, whether it provided an appropriate alcohol intake of lower risk of MCI or PDM was far from clear. Although some studies explored the relation between alcohol intake and risk of MCI [8,9,10], and PDM [9, 11, 12], these studies should be interpreted more cautiously because of heterogeneous alcohol categories and units. And the results were not always consistent. For instance, Anttila found that participants drinking no alcohol or drinking frequently (> 1 time/month) at midlife were both twice as likely to have MCI in old age as those who drank infrequently (< 1 times/month) [8]. But Solfrizzi found no significant association between any levels of alcohol intake (< 1 drinks/day, 1–2 drinks/day, > 2 drinks/day) and risk of MCI versus abstainers [9]. And Koch found no significant association of any level (none, 0.1–0.9 drinks/week, 1.0–7.0 drinks/week, 7.1–14.0 drinks/week, > 14.0 drinks/week) of alcohol intake (drinks/week) and risk of PDM [12]. However, Solfrizzi suggested that up to 1 drink/day of alcohol or wine may decrease the risk of PDM [9]. Additionally, whether there was a dose–response relation between alcohol intake and risk of MCI or PDM remained unclear.
Therefore, we conducted this dose–response meta-analysis for comprehensively synthesizing available evidence, and the objectives of this meta-analysis were: (1) quantifying the relation between alcohol intake and risk of MCI; (2) quantifying the relation between alcohol intake and risk of PDM.
Method
We had prospectively registered the protocols of this systematic review into two parts in PROSPERO (www.crd.york.ac.uk/prospero/): Part 1, association between alcohol intake and risk of MCI (CRD42019127261); part 2, association between alcohol intake and risk of PDM (CRD42019127367). We conducted the two part at the same time and reported in this systematic review and meta-analysis based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) [13].
Search strategy
We searched electronic databases [PubMed, EMBASE, Cochrane Library, and China Biology Medicine disc (CBM)] from inception to October 1, 2019 using the following key terms: ethanol, alcohol, drinking, mild cognitive impairment, preclinical dementia, etc. (full search strategy was available in Supplementary Text 1). No restrictions were imposed.
Eligibility criteria
Studies were included if the following criteria were met simultaneously: (1) was prospective cohort study; (2) the association between alcohol intake and risk of MCI or PDM had been investigated, and there was no restriction on the comorbidity at the baseline; (3) alcohol exposure was categorized into at least three levels which could be quantitated with no restriction on alcohol unit (frequency or quantity); (4) level-specific hazard ratio (HR) or relative risk (RR) associated with 95% confidence interval (CI) were reported. In addition, if multiple articles were published based on the same cohort, we chose that with a larger sample size or longer follow-up time. Studies were excluded if the full-text could not be obtained after we contacted the corresponding authors.
Study selection
Two reviewers independently examined all the titles and abstracts for preliminary inclusion based on pre-set eligibility criteria. Literatures that did not meet the inclusion criteria were excluded at this stage. Then, full-text of literatures left over were checked for final inclusion by two reviewers independently. Any dispute arising in the pairing process were resolved by consensus.
Data extraction and quality evaluation
Two reviewers extracted information into a standardized form independently. For each study, we extracted: (1) study characteristics: first author, publication year, study design, study area, duration of follow-up, loss to follow-up rate, sample size; (2) participants details: diagnostic criteria, age, gender; (3) details of exposure: method of assessing alcohol intake, alcohol categories and unit; (4) outcomes of each alcohol categories: number of events, adjusted confounders, effect size (RR, or HR with 95% CI). The extracted data were cross-checked by the two reviewers. The Newcastle-Ottawa Scale (NOS) tool [14] was used for risk of bias assessment of cohort studies by two review authors independently too. The NOS contains eight items, categorized into 3 dimensions consisting of selection (4 items, 1 star each), comparability (1 item, up to 2 stars), and outcome (3 items, 1 star each) for cohort studies. We regarded research with scores of “0–3”, “4–6” and “7–9” as “low”, “medium”, and “high” quality, respectively [15]. Any dispute arising in the pairing process were resolved by consensus.
Data analysis
Firstly, we conducted categorical meta-analysis with the same alcohol category. Specifically, we combined the risk estimates reflective of the same category in the same study using fixed-effect model and then those in different studies using random-effect model. The alcohol intake was predefined qualitatively as light (< 7 drinks/week), moderate (7–14 drinks/week), and heavy (> 14 drinks/week) based on previous study [7, 16]. The combined results for qualitative categories were compared to observe the variation trend of dementia risk based on alcohol dose.
Then, to conducted dose–response analysis, we assigned the median or mean alcohol intake for alcohol category to each corresponding RR/HR. When the median or mean intake was not reported, we assigned the midpoint of the upper and lower boundaries in each category as the median intake [17, 18]. As previous study reported, when the lowest or upper category was open-ended, we set the lower boundary to zero and assumed that the boundary had the same amplitude as the adjacent category [17, 18].
Since alcohol units used in included studies were unified, we used different pooled units for meta-analysis. We assumed that one drink contains 12 g as used in previous studies if studies did not report specific conversion criteria [7, 18, 19]. And according to previous study, the median frequency for individuals drinking at least 12 g/day was about five times a week [20]. Thus, we could mutually transform alcohol unit from frequency into quantity. Furthermore, one unit was regarded as 8 g and 0.67 drinks as previous study [21, 22].
Restricted cubic spline and fixed-effects dose–response models were used for dose–response meta-analysis [23, 24]. Sensitivity analyses were performed to estimate the influence of alcohol unit transformation from frequency to quantity as well as the choice of statistic index between “HR” and “RR” on the synthesis results. Furthermore, we conducted sensitivity analysis by excluding one study at a time and to assess the influence of individual studies on the pooled estimate [18]. Egger test was used to assess publication bias if included studies were more than ten [25, 26]. The I2 statistic was used to measure the heterogeneity among each studies [27]. I2 > 50% and p < 0.05 was defined as a significant heterogeneity. All statistical analyses were conducted in Stata version 15.0 (Stata Corp, College Station, TX, USA), with two-tailed p < 0.05 for statistical significance.
Result
Literature search
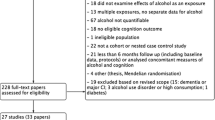
The results of studies selection process were presented in a flow diagram (Fig. 1). We identified 3699 articles during initial electronic search, of which 2816 records were left after removing duplication. 2753 records were excluded after reviewing titles and abstracts, leaving 63 papers with full-text available. Finally, 57 papers were further excluded and a total of six studies were included [8,9,10,11,12, 28]. Titles of articles excluded after screen of the full-text were provided in supplement materials (Supplementary Table 1).
Study characteristics
In the included six studies, two studies explored the relation between alcohol intake and risk of MCI as well as PDM [9, 10]. Additionally, one studies were about alcohol intake and risk of MCI [8]. Three studies explored the relation between alcohol intake and risk of PDM [11, 12, 28]. Six studies were both prospective cohort studies published in English [8,9,10,11,12, 28]. In total, 2883 individuals with normal cognition and 260 incident MCI cases were included in Part 1, 1361 individuals with MCI and 430 incident dementia cases were included in Part 2. Diagnostic criteria to identify MCI and detailed operational procedures of included studies were different from each other. We summarized detailed criteria items and diagnostic procedures in Supplementary Table 2. Two studies did not report clear diagnostic procedures [11, 28]. One study [28] selected MCI individuals from two different cohort [29, 30] which used different diagnostic criteria for MCI, thus, we presented them separately. Three studies were conducted in the Europe [8, 9, 28], one study was conducted in China [11], one study was conducted in America [12] and one study was conducted in Australia [10]. Studies included in Part 1 were regarded as high quality (NOS score ≥ 7), while two studies [10, 11] were regarded as medium quality (scored 6) in Part 2. The characteristics of include studies were presented in Table 1. Specific scores for each item of NOS can be found in the supplement material (Supplementary Table 3).
Part 1: alcohol intake and risk of MCI
Categorical meta-analysis
Among the three included studies, two studies [9, 10] used drinks/day, and one used times/month [8] as alcohol unit. When manually converted units of frequency (times/week) into quantity (drinks/week), the pooled results showed no significant association between risk of MCI and light alcohol intake (RR = 0.79; 95% CI 0.56–1.11; I2 = 0%) or moderate alcohol intake (RR = 1.43; 95% CI 0.85–2.42; I2 = 0%) (Fig. 2). Result was similar when not convert “times/week” into “drinks/week”. As included studies were less than ten, we didn’t perform analysis of publication bias.
Dose–response meta-analysis
We found a linear dose–response relation between alcohol intake (drinks/week) and risk of MCI when transforming alcohol unit from frequency into quantity [8,9,10] (P linear = 0.0396, Fig. 3a). It suggested that a one-drink increment per week in alcohol intake was associated with an increased risk of 3.8% for MCI (RR = 1.038; 95% CI 1.002–1.075). Sensitivity analysis showed that unit transformation from frequency into quantity did not influence the result. But we could not observe the relation when grams/day was used as pooled unit (P linear = 0.0521, Fig. 3b).
Part 2: Alcohol intake and risk of PDM
Categorical meta-analysis
The pooled RRs of risk of PDM for light, moderate, and heavy alcohol intake were 0.74 (95% CI 0.28–1.95; I2 = 63.4%), 0.85 (95% CI 0.51–1.41; I2 = 0%), and 1.76 (95% CI 1.10–2.82; I2 = 0%), respectively (Fig. 4). Only heavy alcohol intake seemed a significant risky association with PDM. Since included studies were less than ten, we did not perform analysis of publication bias.
Dose–response meta-analysis
Among five studies included in the dose–response analysis, three studies used drinks/day [9,10,11], one study used drinks/week [12], and one study used units/week [28] as alcohol unit. Two study reported specific conversion criteria for drink and gram [9, 11]. Thus, we used drinks/week and gram/day as pooled alcohol unit. We observed a nonlinear association between alcohol intake (drinks/week) and risk of PDM when pooling four studies using “HR” as statistic index [9, 11, 12, 28] (P nonlinear = 0.0038, Fig. 5a). We found that drinking more than 16 drinks/week (HR = 1.42; 95% CI 1.00–2.02) would increase the risk of PDM. When pooled in grams/day, we also found a non-linear association between alcohol intake (grams/day) and risk of PDM (P nonlinear = 0.0047, Fig. 5b). We found that drinking more than 27.5 grams/day (HR = 1.46; 95% CI 1.00–2.11) would increase the risk of PDM.
Non-linear association of alcohol intake and risk of PDM (a using “drinks/week” as alcohol unit and “hazard ratio” as statistic index; b using “grams/day” as alcohol unit and “hazard ration” as statistic index; c sensitivity analysis when unsing “drinks/week” as alcohol unit; d sensitivity analysis when using “grams/day” as alcohol unit)
Sensitivity analysis
We conducted sensitivity analysis by adding another one study using “RR” as statistic index to the model. We still observed a nonlinear associated between alcohol intake and risk of PDM. It suggested that drinking more than 17.5 drinks/week (RR = 1.42; 95% CI 1.00–2.05) would increase the risk of PDM (P nonlinear = 0.0061, Fig. 5c). When pooled in grams/day, it still suggested a risky threshold that was 30 g/day (RR = 1.47; 95% CI 1.00–2.16) (P nonlinear = 0.0059, Fig. 5d). Another sensitivity analysis suggested that when excluded Xu [11] or Koch [12], we could not observed a potential dose–response relation. Details of this sensitivity analysis was presented in supplement material (Supplementary Table 4).
Discussion
In this meta-analysis, we systematically evaluated the relation between alcohol intake and the risk of MCI and PDM for the first time. We found a potential linear relation that alcohol drinking might increase the risk of MCI although the association seemed to be instable. Furthermore, it suggested that there was also a potential nonlinear relation between alcohol intake and risk of PDM. Excessive alcohol intake (more than 16 drinks/week or 27.5 g/day) would elevate the risk of PDM. But the relation was not robust too.
Earlier studies about alcohol drinking and cognition defined cognitive impairment in terms of performance in a variety of neuropsychological tests and did not validate it by any clinical or diagnostic concepts [31]. The different measures of cognitive impairment defined based on psychometric made it difficult to compare different studies and to determine the relevance of cognitive impairment in participants’ lives [8]. For instance, some prospective studies found that alcohol intake may improve the cognitive performance measured by Cognitive Abilities Screening Instrument (CASI) [32], the modified Telephone Interview for Cognitive Status (TICS-m) [33], and psychomotor speed and flexibility tests [34]. Furthermore, one study reported a U shape association that nondrinkers and heavy drinkers had the lowest CASI scores, while moderate drinkers had better cognitive performance [35] which was consistent with Launer 1998 based on Mini-Mental State Examination (MMSE) [36]. Nevertheless, one study found that alcohol intake was related to lower cognitive performance in a dose–response manner, even at low levels [37]. The concept of MCI takes into account both psychometric and clinical aspects, and so it may be considered to signify a clinically relevant entity itself [8, 38]. Identifying MCI could well be to help engage people in clinical research and offer pragmatic advice on life style and health modifications, which undoubtedly have a beneficial effect on cognitive performance and prevention of dementia.
A significant number of studies have considered the relation between alcohol intake and risk of MCI and PDM. However, the results might be confused. Some prospective studies found that alcohol intake was associated with a reduced risk for MCI [39, 40]. In the contrast, other studies did not find a protective effect of alcohol for MCI [9, 10, 41]. One study found alcohol drinking was not related to risk of PDM [42]. However, another research revealed that light–moderate alcohol drinker (defined as consuming no more than two drinks a day for at least 6 months) was a risk factor for PDM [43]. As noticed in the above studies, alcohol drinking was often used as a confounding factor when the researchers explored another target potential factor. And then alcohol drinking was always defined in different variable forms artificially. And the most common is the dichotomous variable as far as we know. However, a more detailed relations might be obscured due to an artificially inappropriate definition of alcohol drinking. Heterogeneity of alcohol exposure definition in primary studies made it more difficult to explore the relation of alcohol and risk of MCI or PDM. Based on the above considerations, and to meet the applicable scope of the dose effect meta-analysis model, we only included the primary studies with at least three levels of alcohol exposure.
Primary studies eligible to Part 1 of this study seemed few apparently. We found no significant relation between any alcohol intake categories and risk of MCI in categorical meta-analysis. To our knowledge, none of exiting study had reported the dose–response relation between alcohol intake and risk of MCI clearly. However, a potential weak relation could be found when pooled in drinks/week, but it disappeared when pooled in grams/day. We could not exclude the potential bias of defining the transfer criteria artificially, although researchers always did so based on previous study [7, 18,19,20]. As there was significant clinical uncertainty of the same drinking frequency, and heterogeneous amounts of alcohol was contained in one drink in different areas, the finding should be interpreted with a high degree of caution. All in all, the circumstantial results seemed far from robust and needs to be further verified by future research.
We found a potential nonlinear relation between alcohol intake and risk of PDM in this meta-analysis for the first time. Of the included five studies, only one study reported a significant relation in a certain dose (< 1 drinks/day, HR = 0.15; 95% CI 0.03- 0.78) [9]. Only heavy alcohol intake was found significant associated with risk of PDM in categorical meta-analysis. The results in dose–response meta-analysis corroborated. We revealed a risky alcohol intake dose (> 16 drinks/week, or 27.5 g/day) for PDM. Sensitivity analysis when adding another prospective study using “RR” as statistic index showed higher thresholds for safe alcohol intake. However, this relation was influenced by Xu [11] and Koch [12]. The relation seemed to be not robust enough. It might be due to some eligible studies were not high-quality [10, 11] and the larger effect size contributed by Xu [11] and Koch [12]. Thus, it should be confirmed by more study in the future. And relation between risk of PDM and alcohol intake that was less than the threshold or severe high intake need to be more clarified.
Many studies explored the association between alcohol intake and risk of dementia. One meta-analysis found a significant dose–response relation between alcohol intake and risk of dementia [7]. It revealed that modest alcohol intake (≥ 12.5 g/day) was associated with a reduced risk of dementia with 6 g/day of alcohol conferring a lowest risk, while heavy drinking (≥ 23 drinks/week or ≥ 38 g/day) would significantly elevate the risk. Our results provided a smaller threshold (16 drinks/week or 27.5 g/day) for safe alcohol intake dose for preventing dementia. Alcohol drinking might be more dangerous to cognitive function when taking MCI into consideration. Ding found that increased alcohol intake was associated with brain atrophy [44]. In the contrast, Gu found light to moderate alcohol intake was associated with larger total brain volume and was potentially beneficial for brain aging [45]. Furthermore, Chen highlighted the dose-dependent effects of vascular risk factors (VRF) on bilateral dorsolateral prefrontal cortex (DLPFC) in MCI individuals, and the dynamic compensatory neural processes that fluctuated along with variations of VRF loading could be key role in the progression of MCI [46]. These findings indicated complex neurophysiological mechanism explaining such clinical feature.
As noticed, though no significant statistical heterogeneity was found between included studies, heterogeneous diagnostic criteria and procedures for MCI in primary studies might lead to potential bias. It may be because that the concept of MCI continued to evolve and improve during the past decades even based on observation on different populations [38]. Additionally, the fact that studies originated from different countries or continents might bring about potential clinical heterogeneity too. To be specific, different regions often signified heterogeneous ethnicity, alcohol measurement, drinking preferences and so on which might contribute to different results finally [47]. However, we couldn’t conduct further exploration based on above considerations due to data limitation, which could rely on more detailed reported data for resolution in the future.
The primary strength of our study was that it was the first dose–response meta-analysis to assess the relation between alcohol intake and MCI as well as PDM. And the dose–response design which could better assess the strength of causal relation [48]. Another significant strength of our study was the prospective design of included studies. Furthermore, we had used “hazard ratio” as an index to explain our results. There were also some limitations to this study. Firstly, the included study and pooled sample size were limited. It explained the instability of our results to some extent. Secondly, we could not conduct more subgroup exploration due to the restriction of data about the influence of type of alcohol [45, 49], gender [50], apolipoprotein E4 status [51] etc. Thirdly, we couldn’t avoid possible misclassification of alcohol intake when considering that alcohol dose consumed was always self-reported in primary studies. Fourthly, we cannot exclude the potentially spurious association caused by some confounders as adjusted confounders were inconsistent in different studies. Lastly, we could not explore more about the influence of different originated regions of included studies as well as heterogeneous diagnostic criteria and procedures for MCI on pooled results due to data limitation.
Conclusion
There was a nonlinear dose–response relation between alcohol intake and risk of PDM. Excessive alcohol intake (> 16 drinks/week, or 27.5 g/day) was associated with higher risk of PDM. And there was a potential unstable linear dose–response relation between alcohol intake and risk of MCI. High quality studies should be conducted to exam our preliminary results.
References
Petersen RC, Smith GE, Ivnik RJ et al (1995) Apolipoprotein E status as a predictor of the development of Alzheimer’s disease in memory-impaired individuals. JAMA 273:1274–1278
Petersen RC, Lopez O, Armstrong MJ et al (2018) Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology 90:126–135. https://doi.org/10.1212/wnl.0000000000004826
Mitchell AJ, Shiri-Feshki M (2009) Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand 119:252–265. https://doi.org/10.1111/j.1600-0447.2008.01326.x
Cooper C, Li R, Lyketsos C, Livingston G (2013) Treatment for mild cognitive impairment: systematic review. Br J Psych J Mental Sci 203:255–264. https://doi.org/10.1192/bjp.bp.113.127811
Hugo J, Ganguli M (2014) Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin Geriatr Med 30:421–442. https://doi.org/10.1016/j.cger.2014.04.001
Pink J, O'Brien J, Robinson L et al (2018) Dementia: assessment, management and support: summary of updated NICE guidance. BMJ (Clin Res) 361:k2438–k2444. https://doi.org/10.1136/bmj.k2438
Xu W, Wang H, Wan Y et al (2017) Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 32:31–42. https://doi.org/10.1007/s10654-017-0225-3
Anttila T, Helkala EL, Viitanen M et al (2004) Alcohol drinking in middle age and subsequent risk of mild cognitive impairment and dementia in old age: a prospective population based study. BMJ (Clin Res) 329:539–545. https://doi.org/10.1136/bmj.38181.418958.BE
Solfrizzi V, D’Introno A, Colacicco AM et al (2007) Alcohol consumption, mild cognitive impairment, and progression to dementia. Neurology 68:1790–1799. https://doi.org/10.1212/01.wnl.0000262035.87304.89
Lipnicki DM, Crawford J, Kochan NA et al (2017) Risk factors for mild cognitive impairment, dementia and mortality: the Sydney memory and ageing study. J Am Med Dir Assoc 18:388–395. https://doi.org/10.1016/j.jamda.2016.10.014
Xu G, Liu X, Yin Q et al (2009) Alcohol consumption and transition of mild cognitive impairment to dementia. Psychiatry Clin Neurosci 63:43–49. https://doi.org/10.1111/j.1440-1819.2008.01904.x
Koch M, Fitzpatrick AL, Rapp SR et al (2019) Alcohol consumption and risk of dementia and cognitive decline among older adults with or without mild cognitive impairment. JAMA Netw Open 2:e1910319–e1910332. https://doi.org/10.1001/jamanetworkopen.2019.10319
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097–e1000104. https://doi.org/10.1371/journal.pmed.1000097
GA Wells, B Shea, D O’Connell, et al. (2011) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on 20 Mar 2020
Huang Y, Cai X, Mai W et al (2016) Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ (Clin Res) 355:i5953–i5964. https://doi.org/10.1136/bmj.i5953
Li XH, Yu FF, Zhou YH et al (2016) Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Am J Clin Nutr 103:818–829. https://doi.org/10.3945/ajcn.115.114389
Threapleton DE, Greenwood DC, Evans CE et al (2013) Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clin Res) 347:f6879–f6891. https://doi.org/10.1136/bmj.f6879
Larsson SC, Orsini N, Wolk A (2015) Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. Eur J Heart Fail 17:367–373. https://doi.org/10.1002/ejhf.228
Wang YT, Gou YW, Jin WW et al (2016) Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC cancer 16:212–223. https://doi.org/10.1186/s12885-016-2241-1
Handing EP, Andel R, Kadlecova P et al (2015) Midlife alcohol consumption and risk of dementia over 43 years of follow-up: a population-based study from the Swedish twin registry. J Gerontol Ser A Biol Sci Med Sci 70:1248–1254. https://doi.org/10.1093/gerona/glv038
Sabia S, Fayosse A, Dumurgier J et al (2018) Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ (Clin Res) 362:k2927–k2938. https://doi.org/10.1136/bmj.k2927
Deng J, Zhou DH, Li J et al (2006) A 2-year follow-up study of alcohol consumption and risk of dementia. Clin Neurol Neurosurg 108:378–383. https://doi.org/10.1016/j.clineuro.2005.06.005
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose–response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309. https://doi.org/10.1093/oxfordjournals.aje.a116237
Orsini N, Li R, Wolk A et al (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73. https://doi.org/10.1093/aje/kwr265
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res) 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Higgins JPT TJ, Chandler J, Cumpston M, et al. (Eds) (2019) Cochrane handbook for systematic reviews of interventions version 6.0 (Updated July 2019) Cochrane. www.training.cochrane.org/handbook. Accessed on 20 Mar 2020
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ (Clin Res) 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Reijs BLR, Vos SJB, Soininen H et al (2017) Association between later life lifestyle factors and Alzheimer’s disease biomarkers in non-demented individuals: a longitudinal descriptive cohort study. J Alzheimer’s Dis JAD 60:1387–1395. https://doi.org/10.3233/jad-170039
Visser PJ, Verhey FR, Boada M et al (2008) Development of screening guidelines and clinical criteria for predementia Alzheimer’s disease. DESCR Study Neuroepidemiol 30:254–265. https://doi.org/10.1159/000135644
Hall A, Munoz-Ruiz M, Mattila J et al (2015) Generalizability of the disease state index prediction model for identifying patients progressing from mild cognitive impairment to Alzheimer’s disease. J Alzheimer’s Dis JAD 44:79–92. https://doi.org/10.3233/jad-140942
Petersen RC, Doody R, Kurz A et al (2001) Current concepts in mild cognitive impairment. Arch Neurol 58:1985–1992. https://doi.org/10.1001/archneur.58.12.1985
Bond GE, Burr R, McCurry SM et al (2004) Alcohol, gender, and cognitive performance: a longitudinal study comparing older Japanese and non-Hispanic white Americans. J Aging Health 16:615–640. https://doi.org/10.1177/0898264304268587
Wright CB, Elkind MS, Luo X et al (2006) Reported alcohol consumption and cognitive decline: the northern Manhattan study. Neuroepidemiology 27:201–207. https://doi.org/10.1159/000096300
Kalmijn S, van Boxtel MP, Verschuren MW et al (2002) Cigarette smoking and alcohol consumption in relation to cognitive performance in middle age. Am J Epidemiol 156:936–944. https://doi.org/10.1093/aje/kwf135
Galanis DJ, Joseph C, Masaki KH et al (2000) A longitudinal study of drinking and cognitive performance in elderly Japanese American men: the Honolulu-Asia aging study. Am J Publ Health 90:1254–1259. https://doi.org/10.2105/ajph.90.8.1254
Launer LJ, Feskens EJ, Kalmijn S et al (1996) Smoking, drinking, and thinking. The zutphen elderly study. Am J Epidemiol 143:219–227. https://doi.org/10.1093/oxfordjournals.aje.a008732
Hassing LB (2018) Light alcohol consumption does not protect cognitive function: a longitudinal prospective study. Front Aging Neurosci 10:81–89. https://doi.org/10.3389/fnagi.2018.00081
Petersen RC, Caracciolo B, Brayne C et al (2014) Mild cognitive impairment: a concept in evolution. J Intern Med 275:214–228. https://doi.org/10.1111/joim.12190
DeCarli C, Miller BL, Swan GE et al (2001) Cerebrovascular and brain morphologic correlates of mild cognitive impairment in the national heart, lung, and blood institute twin study. Arch Neurol 58:643–647. https://doi.org/10.1001/archneur.58.4.643
Ganguli M, Fu B, Snitz BE et al (2013) Mild cognitive impairment: incidence and vascular risk factors in a population-based cohort. Neurology 80:2112–2120. https://doi.org/10.1212/WNL.0b013e318295d776
Wang T, Xiao S, Chen K et al (2017) Prevalence, incidence, risk and protective factors of amnestic mild cognitive impairment in the elderly in Shanghai. Curr Alzheimer Res 14:460–466. https://doi.org/10.2174/1567205013666161122094208
Li J, Wang YJ, Zhang M et al (2011) Vascular risk factors promote conversion from mild cognitive impairment to Alzheimer disease. Neurology 76:1485–1491. https://doi.org/10.1212/WNL.0b013e318217e7a4
Xue H, Sun Q, Liu L et al (2017) Risk factors of transition from mild cognitive impairment to Alzheimer’s disease and death: a cohort study. Compr Psychiatry 78:91–97. https://doi.org/10.1016/j.comppsych.2017.07.003
Ding J, Eigenbrodt ML, Mosley TH et al (2004) Alcohol intake and cerebral abnormalities on magnetic resonance imaging in a community-based population of middle-aged adults: the atherosclerosis risk in communities (ARIC) study. Stroke 35:16–21. https://doi.org/10.1161/01.Str.0000105929.88691.8e
Gu Y, Scarmeas N, Short EE et al (2014) Alcohol intake and brain structure in a multiethnic elderly cohort. Clin Nutr (Edinb, Scotl) 33:662–667. https://doi.org/10.1016/j.clnu.2013.08.004
Chen H, Su F, Ye Q et al (2018) The dose-dependent effects of vascular risk factors on dynamic compensatory neural processes in mild cognitive impairment. Front Aging Neurosci 10:131–142. https://doi.org/10.3389/fnagi.2018.00131
Gagnier JJ, Moher D, Boon H et al (2012) Investigating clinical heterogeneity in systematic reviews: a methodologic review of guidance in the literature. BMC Med Res Methodol 12:111. https://doi.org/10.1186/1471-2288-12-111
Guyatt GH, Oxman AD, Kunz R et al (2008) What is “quality of evidence” and why is it important to clinicians? BMJ (Clin Res) 336:995–998. https://doi.org/10.1136/bmj.39490.551019.BE
Truelsen T, Thudium D, Gronbaek M (2002) Amount and type of alcohol and risk of dementia: the Copenhagen city heart study. Neurology 59:1313–1319. https://doi.org/10.1212/01.wnl.0000031421.50369.e7
Wang X, Zhou W, Ye T et al (2019) Sex Difference in the association of APOE4 with memory decline in mild cognitive impairment. J Alzheimer’s Dis JAD 69:1161–1169. https://doi.org/10.3233/jad-181234
Ruitenberg A, van Swieten JC, Witteman JC et al (2002) Alcohol consumption and risk of dementia: the Rotterdam study. Lancet (Lond, Engl) 359:281–286. https://doi.org/10.1016/s0140-6736(02)07493-7
Funding
This work was supported by the National Social Science Fund of China (Grant No. 19ZDA142), the Fundamental Research Funds for the Central Universities (Grant No. 18LZUJBWZX006 and Grant No. 2019jbkyzy002): Evidence-based Social Science Research, and the National Innovation and Entrepreneurship Training Program for Undergraduate (Grant No. 201910730215). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
KY, PY were responsible for the conception and design of the study. YL and LH were in charge literature search data acquisition. YL, LH, JL and XH selected eligible studies, and extracted the data. YL and PY analyzed and interpreted the data. YL wrote the first draft of the manuscript. Other co-authors had given critical advice to the manuscript. All authors read and approved the final manuscript. We sincerely thanked XZ, YG, JF and XH for important help in getting the full articles though they could not be identified as co-authors. And we would like to thank the authors of the article "Risk Factors for Mild Cognitive Impairment, Dementia and Mortality: The Sydney Memory and Ageing Study" [10] for providing us with the extra data we requested.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Human and animal rights
As this study was a meta-analysis based on published studies, as such, did not involve human or animal participants. And there is no need for an ethical approval or informed consent requested by animal and human experiments.
Informed consent
For this type of study: a systematic review based on published studies, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lao, Y., Hou, L., Li, J. et al. Association between alcohol intake, mild cognitive impairment and progression to dementia: a dose–response meta-analysis. Aging Clin Exp Res 33, 1175–1185 (2021). https://doi.org/10.1007/s40520-020-01605-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01605-0