Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) is the liver manifestation of metabolic syndrome, a risk factor for mortality and cardiovascular morbidity, but we ignore the role of steatosis per se in survival, and there is very little information about this condition in the geriatric patient.
Aims
With the present study, we investigated the independent prognostic value of NAFLD on overall mortality in the elderly.
Methods
Within the Pianoro Project, involving people ≥ 65 years, anamnestic, clinical and laboratoristic data related to NAFLD, insulin resistance, diabetes/hyperglycemia, hypertension, obesity and dyslipidemia were collected in 804 subjects (403 male, 401 female). These subjects were followed up for mortality for a median time of 12.6 years. A multivariate analysis was performed to evaluate the prognostic value of the covariates.
Results
At Kaplan–Meier estimator the presence of NAFLD seems to be associated to a lower mortality, and survival tends to increase with the increasing of steatosis grade. Cox’s analysis found that survival is increased for subjects having hypercholesterolemia (RR = 0.565), NAFLD (RR = 0.777), hypertension (RR = 0.711) and in female (RR = 0.741), while it is decreased for the older subjects (RR = 3.046), in patients with hypertriglyceridemia (RR = 1.699) and for diabetics (RR = 1.797). The variables BMI and HDL-cholesterol have no role.
Conclusion
The data obtained in our study show that NAFLD is not associated to overall mortality in the elderly population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is characterised by excessive hepatic fat accumulation, associated with insulin resistance. NAFLD includes two distinct conditions: non-alcoholic fatty liver (NAFL) and non-alcoholic steatohepatitis (NASH), with an increased risk of fibrosis progression, cirrhosis and possibly hepatic comorbidities such as hepatocellular carcinoma (HCC) [1, 2]. NAFLD is the most common liver disorder in Western countries, affecting 17–46% of adults [3, 4] and in these countries NAFLD has reached epidemic proportions [5, 6]. There is a strong correlation between NAFLD and metabolic syndrome (MS). NAFLD might represent an additional characteristic, or the hepatic manifestation, of MS [7, 8].
Some studies have recently evaluated NAFLD in the elderly population. An association between sarcopenia in the elderly and hepatic steatosis has been documented. There is an inverse correlation between insulin resistance and muscle mass, and a direct association between insulin resistance and steatosis [9, 10]. A potential common mechanism between sarcopenia and NAFLD is the chronic low-grade inflammation that characterizes aging, commonly called "inflammaging" [11, 12].
Some studies showed that NAFLD might represent a risk factor for the development of dementia. This association could be linked to the increased cerebrovascular risk (increased incidence of atherosclerotic carotid plaques in subjects with NAFLD), but hormonal factors may also play a role [13,14,15].
The aim of the present study was to evaluate the epidemiological features of NAFLD in the elderly population and its relationship with MS. We also evaluated, in this age group, the independent prognostic relevance of NAFLD on overall mortality, to consider the opportunity to treat this common condition in geriatric patients, which have peculiarities in terms of limitation in physical activity, higher risk of drug interactions and adverse reactions.
Materials and methods
Study setting and study design
Our study is part of a larger cross-sectional and prospective study about the promotion of physical activity in the elderly population called “The Pianoro Study”.
The study started in November 2003 and recruited 3255 subjects, aged over 65 years, of both sexes, resident in Pianoro, who received a postal questionnaire to evaluate: the presence of risk factors for atherosclerosis, their quality of life, the previous or actual cardiovascular diseases, their degree of autonomy, prescribed medications and the amount of physical activity performed in the last week. There were no exclusion criteria apart from age.
Two thousand twenty-three subjects (62% of the population) filled in the questionnaire and sent it back by ordinary mail. All the subjects over 65 resident in Pianoro, whether they had answered the questionnaire, were invited to their general practitioner’s office, where gave written informed consent to take part in the study, had a check of the previously filled questionnaire, received a paperpencil cognitive test (Mini Mental State Examination) and a weight, height and blood pressure evaluation.
Between January 2004 and January 2005 they were also invited to come to our hospital division, where we collected anthropometric parameters, fasting blood samples, an electrocardiogram, an abdominal ultrasound scan and a sub-maximal step test.
In all, 1144 subjects, 550 men and 594 women, aged 65–91 years (median 71), performed all clinical steps of the study without missing data.
Fourteen years after the study start (between December 2016 and March 2018), we tried to evaluate the outcome of these subjects (death or survival) deducing information from their accesses to the National Health Service. In this way, we found data of 804 of them.
Variables examined
Age, gender and anthropometry
Age, gender, weight, height and waist circumference (measured in centimeters with the patient standing at the umbilicus level) were assessed. BMI was calculated as the ratio between weight (kg) and the square of height (m). According to the BMI [16] we classified the population in class 0 (BMI < 25 kg/m2), class 1 (BMI 25–29,9 kg/m2), class 2 (BMI 30–35 kg/m2) and class 3 (BMI > 35 kg/m2). Class 0 corresponds to normal weight or underweight; class 1 corresponds to overwight, class 2 or 3 to obesity.
Four skinfolds were measured: biceps skinfold, triceps skinfold, subscapular skinfold and suprailiac skinfold.
According to the age, the population of our study was divided into two subgroups: between 65 to 74 years old (young old) and over 74 years old (old old and oldest old, not further subdivided due to the small number of people over 85 years).
Laboratory assays
Blood glucose, creatinine, total cholesterol, HDL-cholesterol and triglycerides were assayed with enzymatic methods. Also insulin was measured with an analytical sensitivity of 0.2 mU/l.
Lifestyle, diseases and multimorbidity
Variables evaluated were:
-
Alcohol intake: defined as the daily use of at least one alcoholic unit (a glass of wine or a pint of beer or a small glass of spirit).
-
Diabetes: subjects with a history of diabetes according to the American Diabetes Association Criteria, and/or on anti-diabetes drugs and/or with blood glucose > 126 mg/dl were considered diabetic.
-
Impaired fasting glucose (IFG): subjects with blood glucose > 100 mg/dl but not diabetic.
-
Hypertension: subjects with a history of hypertension, those with systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg and those on current therapy with anti-hypertensive drugs.
-
Dyslipidemia: were considered as independent variables hypertriglyceridemia (triglycerides > 150 mg/dl) or current treatment, pathological levels of HDL cholesterol (< 40 mg/dl in men or < 50 mg/dl in women) or current treatment with statins and hypercholesterolemia (total cholesterol ≥ 200 mg/dl) or current therapy.
-
Insulin resistance: insulin resistance was estimated, according to the homeostasis model assessment (HOMA), with the formula: (fasting insulin [mU/l] × fasting glucose [mmol/l])/22.5 [17]. In a previous study concerning an Italian population, the cut-off of HOMA values indicative of insulin resistance (above the 75th percentile) was set at 2.7 [18, 19].
-
MS: the presence of MS, according to the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III rev. 2004), occurs when at least three of the following five criteria are fulfilled: waist circumference > 102 cm in men or > 88 cm in women; blood glucose ≥ 100 mg/dl (5.6 mmol/l) or current treatment with hypoglycaemic drugs; triglycerides ≥ 150 mg/dl (1.7 mmol/l) or current treatment; HDL cholesterol < 40 mg/dl (1.0 mmol/l) in men or < 50 mg/dl (1.3 mmol/l) in women; systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg or current treatment with antihypertensive drugs.
-
Charlson comorbidity index: multimorbidity was assessed using the Charlson comorbidity index, a scoring system including 19 categories of comorbid conditions and commonly used as prognostic tool for mortality [20].
Abdominal ultrasound scan for evaluating fatty liver, subcutaneous and visceral fat.
The abdominal ultrasound (US) scan was performed using an Esaote-Ansaldo Technos echograph with a 3.5–5 MHz convex US probe. Diagnosis of fatty liver was based on the increased echogenicity of the liver parenchyma. Two physicians with extensive US experience performed each exam. If present, steatosis was classified into three degrees:
-
Mild: slightly brighter liver as compared to the renal cortex, clear visualization of diaphragm.
-
Moderate: brighter liver with attenuation of the ultrasound beam.
-
Severe: very bright liver, severe ultrasound beam attenuation with a marked attenuation of the ultrasound beam, such as not to make visible the portal bifurcation.
With transversal scan in epigastrium/mesogastrium we also evaluated subcutaneus fat (distance between the anterior abdominal wall and the parietal peritoneum) and visceral fat (distance between the anterior abdominal wall and the anterior border of the abdominal aorta, subtracting the subcutaneous fat).
Fat mass percentages
To determine this value it was used the formula of the Siri equation [21]:
Body density was calculated considering the four skinfolds using the formula:
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Science (SPSS version 23 for Windows).
Before running the statistical analysis, continuous parametric variables were tested to check the presence of a normal distribution. Descriptive data are presented as mean value ± standard deviation (SD) or median (range) for continuous variables, and as frequencies and percentages for discrete variables.
The Chi square test (χ2) was used to evaluate differences between groups in discrete variables. The Mann–Whitney’s U test was used to compare continuous variables between groups.
To evaluate the prognostic value of NAFLD, Kaplan–Meier survival curves were performed.
We also evaluated prognostic significance, for survival, of other clinical/laboratoristic/anamnestic variables transformed into dichotomic or category parameters, for example presence or absence of diabetes, presence ore absence of hypertriglyceridemia etc.
All variables that were significant or nearly significant at univariate time-dependent analysis were considered for multivariate time-dependent analysis according to Cox’s Model.
For each variable the adjusted relative risk (RR) and 95% confidence interval (CI) were also computed.
For all tests two-tailed p values are reported, and the level of significance was set at p < 0.05.
Results
Description of the population
We recruited 804 subjects (403 males and 401 female) in our study. The median age was 72.7 years (65.5–93.6) with 64% of subjects < 75 years (young old) and 36% ≥ 75 years.
Their outcomes were evaluated after a median follow-up of 12.6 years (22 days–14 years); 401 of them are still alive, while 403 are dead.
At the end of the follow up the median age was 83.3 years (67.5–99.8 years). Regarding lifestyle, 10% of the population at the time of enrolment was an active smoker, while 48% were ex-smokers; 63% of subjects reported consuming alcoholic beverages, but only 53 subjects (about 6.6% of the population) said they consume more than three alcoholic units for day.
We evaluated our subjects for their comorbidities with the Charlson Comorbidity Index: the median value was 1 (0–10). These data are summarized in Table 1.
Considering the prevalence of the features included in MS definition, according to NCEP-ATP III criteria, we found that the 44.4%, at first examination, had IFG, while the 12.9% had diabetes; the 70.4% was hypertensive; the 30.3% had hypertriglyceridemia; the 38.1% had low HDL cholesterol; the 52.3% had pathological waist circumference. There are no significant differences in the distribution of these criteria between the two age classes (< and ≥ 75 years).
The prevalence of MS in our population, according to the same criteria, was 44.6%, without significant age-related differences.
Considering our subjects’ BMI, we found that the 38.8% was normal or under-weight, the 44.1% over-weight and the 17.1% obese. There is significant difference (p < 0,001) between the two age classes in BMI distribution, with a higher prevalence of lower BMI classes in older subjects, likely representative of malnutrition. The average BMI of the whole population is 26.5 ± 4.0 kg/m2, while it is 27.1 ± 4.2 kg/m2 in the young olds and 25.4 ± 3.4 kg/m2 in people over 75.
Additional anthropometric and metabolic features of the enrolled subjects were evaluated. There are significant age-dependent differences in BMI, fat mass percentage, subcutaneous and visceral fat, while there is no difference in the prevalence of insulin-resistance, diabetes and hypercholesterolemia.
All the variables analysed and their differences between the two age classes are reported in Table 2.
Prevalence of hepatic steatosis in the elderly
In our population we found a prevalence of US-diagnosed hepatic steatosis of 42.7%; 26.6% of these subjects had mild steatosis, 13.7% moderate, 2.4% severe. The grade of steatosis tends to decrease moving from the younger age class to the older one with a statistically significant difference (Table 3).
We found a negligible prevalence of drinkers; for this reason, we avoided excluding from our sample this small group of subjects (only 53 subjects), and we considered all the individuals with US-diagnosed steatosis as having NAFLD.
Relationship between NAFLD and MS in the elderly
As a first purpose, we evaluated if NAFLD and MS have in the elderly the same tight association as widely confirmed in the adults. We studied if the single features of MS had a different distribution in subjects with and without NAFLD; all comparisons show wide and statistically significant differences (Table 4).
We also found significant differences in the distribution of hepatic steatosis between the different BMI classes (Table 5).
This data show, in the elderly as in adult subjects, a strong relationship between NAFLD, MS, and associated conditions, such as diabetes and obesity.
Univariate analysis
Survival curves of subjects with hepatic steatosis, diabetes, insulin resistance, hypercholesterolemia, MS and all parameters included in the definition of MS according to the NCEP-ATP III criteria were estimated with Kaplan–Meier analysis. These survival curves were compared with those of subjects not affected by these conditions.
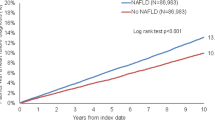
Evaluating the survival curves of subjects with and without hepatic steatosis at the first visit (Fig. 1) we observed that survival is greater in affected subjects, compared to those not affected (χ2 = 5.441; p = 0.020); furthermore, distinguishing survival curves for hepatic steatosis degree, we observed a survival decrease with the reduction of steatosis degree (χ2 = 9.427; p = 0.024), as shown in Fig. 2.
At Kaplan–Meier estimate, as expected, survival was increased in younger subjects compared to the older ones (χ2 = 98.739; p < 0.001). Sex is a relevant feature too: survival was increased in females compared to males (χ2 = 5.551; p = 0.018). BMI is not a significant feature (χ2 = 3.270; p = 0.071), although there’s a trend to a higher survival for the overweight subjects compared with the subjects under or normal-weight.
We analysed the role of single components of MS on survival. The role of waist circumference is not significant (χ2 = 0.212; p = 0.645), and neither is hyperglycaemia (χ2 = 2.533; p = 0.111); hypertriglyceridemia is associated with a lower survival (χ2 = 6.002; p = 0.014); paradoxically, hypertension (χ2 = 12,959; p < 0,001) and low HDL cholesterol (χ2 = 7.349; p = 0.007) seem to be related to a higher survival. The role of MS itself seems not to be relevant in our population (χ2 = 0.001; p = 0.982).
Survival was decreased for diabetics (χ2 = 9.349; p = 0.002), while hypercholesterolemia is associated to a higher survival (χ2 = 10.862; p = 0.001). Finally the insulin-resistance was evaluated: about survival no difference between people with insulin-resistance and without insulin-resistance was found (χ2 = 0.018; p = 0.893).
The results shown above are summarized in Table 6.
Multivariate analysis
The main aim of our study was the evaluation of NAFLD prognostic significance in old people.
For the purpose to evaluate the independent prognostic value of NAFLD in our population, a backward logistic regression analysis was performed considering in the Cox’s model as variables the ones significantly associated to survival at univariate analysis, in a positive or negative way (Table 7).
Cox’s analysis result showed that the variables independently associated to survival are:
-
1.
NAFLD: after a median follow up of 12.6 years, the death risk is 22% lower in subjects with NAFLD than without NAFLD;
-
2.
Female sex: the death risk is 26% lower in women than in men;
-
3.
Hypertension: the subjects having a systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg, or being on anti-hypertensive therapy, have a death risk 29% lower than the ones not fulfilling these criteria;
-
4.
Hypercholesterolemia: the death risk is almost halved in hypercholesterolemic subjects.
The variables negatively associated to survival, representing risk factors for overall mortality, apart from obviously age, are:
-
1.
Diabetes: the death risk, after a follow up of 12.6 years, is 80% higher in diabetics;
-
2.
Hypertriglyceridemia: the death risk is 70% higher in subjects having hypertriglyceridemia.
The contribution of the variables BMI and low HDL-cholesterol seems not to be relevant.
Discussion
Several studies showed an increased mortality in subjects with NAFLD [22, 23], but studies investigating the independent prognostic value of NAFLD in the elderly population have never been performed.
In our study the median value of Charlson Comorbidity Index was low; it means that, as we expected, our sample is not exactly representative of the whole old population, but it’s made of fitter subjects, as the result of a voluntary enrolment which required a certain degree of autonomy to attend the medical examinations, and so a relatively good health.
This is, in our opinion, not so much a limitation of this study, because it is precisely in this population the doubt arises whether to treat or not to treat NAFLD, and not in multi-pathological or institutionalized subjects.
A relevant information of our study is that MS and all its components, diabetes and insulin-resistance, show high prevalence in old people, with no distribution differences between the two age classes that we considered (< or ≥ 75 years).
On the contrary, according to previous observations, we found significant distribution differences in BMI, fat mass percentage, and subcutaneous and visceral fat: all these variables show higher average values in younger subjects. These differences are an expression of the changes in body composition old people undergo in different phases of aging, differences that have to be considered in therapeutic and nutritional approach to geriatric patient [24].
NAFLD shows a prevalence of 42.7% in the old population recruited in our study, that is definitely higher than reported by other authors for adult subjects [25].
As other metabolic features, according to literature [13], the distribution of NAFLD prevalence in old people show a decreasing trend, with higher average values in younger subjects than in older people.
This trend, similar to the ones of BMI, fat mass percentage, visceral and subcutaneous fat, may suggest that changes in the prevalence of hepatic steatosis in the elderly are part of changes in the body composition, and would not be caused by differences in the prevalence of insulin resistance and MS, which show a similar distribution in different age groups.
However, this does not stand for a weaker relationship between NAFLD, MS and its single components in the elderly population: this association, according to our results, is important and statistically significant, contrary to other authors’ thesis [26].
Other groups [27] suggest that the reducing prevalence of NAFLD in the older people might be an expression of a negative selection of subjects with NAFLD, but this hypothesis seems to be denied by our study, too.
The main purpose of our study was to investigate the independent prognostic value of NAFLD in the elderly. We also evaluated the prognostic significance of all components of the MS. Cox’s analysis show that modifiable risk factors for overall mortality in the elderly are diabetes and hypertriglyceridemia, while NAFLD, hypercholesterolemia and elevated blood pressure have no association with overall mortality. Although these results seem to be paradoxical, it must be considered that “traditional” risk factors, in the elderly, often tend to lose their prognostic value, and sometimes to revert it.
With regard to the "hypertension" parameter, probably this paradoxical result is caused, at least in part, to the fact that we considered hypertensive people not only those with high blood pressure but also those in anti-hypertensive therapy (regardless of blood pressure values).
Furthermore, according to recent raccomandations on cardiovascular risk in the elderly population [28], the correction of hypertension should not be "aggressive”.
The role of hypercholesterolemia should be carefully evaluated in the geriatric patients, too: a slightly increased cholesterolemia may be considered an indirect sign of good nutritional status and has a good prognostic significance in elderly subjects [29]. This data is confirmed by our study, too.
Evaluating the independent prognostic significance of NAFLD our study shows that, in the old population, NAFLD is not associated with an increased overall mortality, differently from studies in adult population suggest.
Some limitations in our study have to be acknowledged: NAFLD was diagnosed just by the US finding of a “bright liver”, although its diagnosis would require the exclusion of drinkers and people suffering from other chronic liver diseases. We did not exclude the first ones as subjects exceeding the daily alcohol intake limits were a small group in our population, and there were no significant differences between the ones having NAFLD or not. Instead, we unfortunately did not have information about the prevalence of other chronic liver diseases in our subjects, and we have to underline that HCV infection has a non-negligible prevalence in old population.
Conclusion
The results of our study show, in the old population, no association between NAFLD and overall mortality. On an institutional level, this result can be a cause for reflection in health organizative matter, in particular in terms of allocating resources to treat or to follow up a so common condition in this age class.
Moreover, on a biological level, our data suggest a possible different “biological significance” of NAFLD in the geriatric patients: an indirect marker of good nutritional status.
Anyway, we still must repeat that, in the elderly as in the adult, there is a tight association between NAFLD and MS and, more important than MS in old subjects, a tight association with diabetes. Although NAFLD does not seem to be a risk factor for overall mortality in the elderly, it must be considered an alert for the presence of metabolic comorbidities. These ones, especially diabetes, will possibly deserve a therapy, but not NAFLD per se.
References
Marchesini G, Day CP, Dufour JF et al (2016) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. https://doi.org/10.1016/j.jhep.2015.11.004
McCullough AJ (2006) Pathophysiology of nonalcoholic steatohepatitis. J Clin Gastroenterol. https://doi.org/10.1097/01.mcg.0000168645.86658.22
Vernon G, Baranova A, Younossi ZM (2011) Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Pharmacol Ther Aliment. https://doi.org/10.1111/j.1365-2036.2011.04724.x
Neuschwander-Tetri BA (2005) Nonalcoholic steatohepatitis and the metabolic syndrome. BMC Med. https://doi.org/10.1186/s12916-017-0806-8
Adams LA, Angulo P (2005) Recent concepts in non-alcoholic fatty liver disease. Med Diabet. https://doi.org/10.1111/j.1464-5491.2005.01748.x
Marchesini G, Bugianesi E, Forlani G et al (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. https://doi.org/10.1053/jhep.2003.50161
Lonardo A, Ballestri S, Marchesini G et al (2015) Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis. https://doi.org/10.1016/j.dld.2014.09.020
Frith J, Day CP, Robinson L et al (2010) Potential strategies to improve uptake of exercise interventions in non-alcoholic fatty liver disease. J Hepatol. https://doi.org/10.1016/j.jhep.2009.10.010
Hong HC, Hwang SY, Choi HY et al (2014) Relationship between sarcopenia and nonalcoholic fatty liver disease: The Korean Sarcopenic Obesity Study. Hepatology. https://doi.org/10.1002/hep.26716
Kitajima Y, Eguchi Y, Ishibashi E et al (2010) Age-related fat deposition in multifidus muscle could be a marker for nonalcoholic fatty liver disease. J Gastroenterol. https://doi.org/10.1007/s00535-009-0147-2
Franceschi C, Campisi J (2014) Chronic inflammation (Inflammaging) and its potential contribution to age-associated diseases. Gerontol A Biol Sci Med Sci. https://doi.org/10.1093/gerona/glu057
Beyer I, Mets T, Bautmans I (2012) Chronic low-grade inflammation and age-related sarcopenia. Opin Clin Nutr Metab Care Curr. https://doi.org/10.1097/MCO.0b013e32834dd297
Bertolotti M, Lonardo A, Mussi C et al (2014) Nonalcoholic fatty liver disease and aging: epidemiology to management. Gastroenterol World J. https://doi.org/10.3748/wjg.v20.i39.14185
Brea A, Mosquera D, Martín E et al (2005) Nonalcoholic fatty liver disease is associated with carotid atherosclerosis: a case-control study. Arterioscler Thromb Vasc Biol. https://doi.org/10.1161/01.ATV.0000160613.57985.18
Abbatecola AM, Ferrucci L, Marfella R, Paolisso G (2007) Insulin resistance and cognitive decline may be common soil for frailty syndrome. Intern Med Arch. https://doi.org/10.1001/archinte.167.19.2145-b
Pi-Sunyer FX, Becker DM, Bouchard C et al (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. https://doi.org/10.1093/ajcn/68.4.899
Haffner SM, Miettinen H, Stern MP (1997) The homeostasis model in the San Antonio Heart Study. Diabetes Care. https://doi.org/10.2337/diacare.20.7.1087
Bugianesi E, Gastaldelli A, Vanni E et al (2005) Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. https://doi.org/10.1007/s00125-005-1682-x
Bugianesi E, Pagotto U, Manini R et al (2005) Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2004-2240
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. https://doi.org/10.1016/0021-9681(87)90171-8
Siri WE (1993) Body composition from fluid spaces and density: analysis of methods. 1961. Nutrition 9:480–491
Ekstedt M, Franzén LE, Mathiesen UL et al (2006) Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. https://doi.org/10.1002/hep.21327
Zeb I, Li D, Budoff MJ et al (2016) Nonalcoholic fatty liver disease and incident cardiac events the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2016.01.07
Agricola E, Bove T, Oppizzi M et al (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695. https://doi.org/10.1378/chest.127.5.1690
Bedogni G, Miglioli L, Masutti F et al (2005) Prevalence of and risk factors for nonalcoholic fatty liver disease: the dionysos nutrition and liver study. Hepatology. https://doi.org/10.1002/hep.20734
Kagansky N, Levy S, Keter D et al (2004) Non-alcoholic fatty liver disease—a common and benign finding in octogenarian patients. Liver Int. https://doi.org/10.1111/j.1478-3231.2004.0969.x
Koehler EM, Schouten JNL, Hansen BE et al (2012) Prevalence and risk factors of non-alcoholic fatty liver disease in the elderly: results from the Rotterdam study. J Hepatol. https://doi.org/10.1016/j.jhep.2012.07.028
Bangalore S, Gong Y, Cooper-Dehoff RM et al (2014) 2014 eighth joint national committee panel recommendation for blood pressure targets revisited: results from the invest study. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2014.05.044
Schatz IJ, Masaki K, Yano K et al (2001) Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet. https://doi.org/10.1016/S0140-6736(01)05553-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
All procedures and the research protocol have been approved by the locally appointed ethics committee of the University of Bologna. The experimental protocol was designed in accordance with the Declaration of Helsinki (1964).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tallarico, V., Recinella, G., Magalotti, D. et al. Prognostic value of non-alcoholic fatty liver disease in the elderly patients. Aging Clin Exp Res 32, 2657–2665 (2020). https://doi.org/10.1007/s40520-020-01487-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01487-2