Abstract
Background
Accumulation of aggregated α-synuclein from the enteric nervous system is believed to be involved in the pathogenesis of Parkinson’s disease (PD). The appendix contains abundant α-synuclein and lacks a blood–tissue barrier, suggesting that appendectomy might reduce α-synuclein aggregation, and therefore the risk of PD. Studies on this intriguing possibility have not come to consistent conclusions.
Methods
PubMed, Embase (via Ovid), and the Cochrane Controlled Register of Trials were searched for studies published through February 20, 2019 on the potential relationship between appendectomy and PD. Two reviewers independently screened literature, extracted data and evaluated the quality of included studies. Data were summarized as pooled effect sizes (RRs or SMDs) with 95% confidence intervals (CIs), which were calculated using the inverse variance method and a random-effects model. Heterogeneity was assessed using the I2 statistic and explored in subgroup analyses.
Results
Of the 408 references screened, six studies involving 3,554,540 people were included eventually. Appendectomy did not significantly affect PD risk (RR 1.02, 95% CI 0.87–1.20, I2 = 83.1%, P = 0.789) or delay its onset (SMD 0.21, 95% CI − 0.03 to 0.44, I2 = 43.4%, P = 0.083).
Conclusion
The available evidence suggests no protective effect of appendectomy against PD. Future studies should seek to clarify the role of inflammation, α-synuclein pathology and the gut–brain axis in PD pathogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease [1]: in 2016, it affected more than 6.1 million individuals globally, causing substantial burden to the health system [2]. Due to the progressive loss of midbrain dopaminergic neurons of the substantia nigra, PD patients present with motor symptoms of bradykinesia, rigidity, rest tremor, abnormal gait and posture [3]. Non-motor symptoms also occur in many PD patients, such as gastrointestinal dysfunction, and may precede motor symptoms by years [4]. The potential involvement of the gut–brain axis in PD is gaining increasing attention.
Braak and colleagues proposed that the protein α-synuclein, a key component in Lewy bodies and Lewy neurites and a pathological hallmark of PD, may move from the enteric nervous system to the brain via active retrograde transport along the vagal nerve, giving rise to idiopathic PD [5, 6]. The appendix is abundant in α-synuclein, and materials can move freely from that organ into the brain without passing through a barrier [7]. Thus, several studies have examined the possibility that appendectomy, a surgical procedure to remove the vermiform appendix [8], may affect the pathogenesis of PD.
Studies of this question have examined potential effects of appendectomy on age at PD onset, PD risk and PD severity [9,10,11,12,13,14], and they have come to conflicting conclusions. Therefore, we undertook the present systematic review and meta-analysis to gain a clear picture of the available evidence on this question.
Method
Search strategy
The PubMed, Embase (via Ovid), and Cochrane Controlled Register of Trials (CENTRAL) databases were systematically searched by two independent researchers (HTL and QYS) through February 20, 2019. The following search strategy was employed: “(Parkinsonian disorders OR Parkinson disease OR Parkinson OR Parkinson’s disease OR Idiopathic Parkinson disease OR Idiopathic Parkinson’s disease OR Paralysis agitans OR Parkinsonism) AND (Appendectomy OR Appendicectomy OR Ecphyadectomy OR Append*)”. All terms were searched as text words and subject headings (e.g., MeSH in PubMed) where available. Additional potential publications were identified by hand-searching reference lists of the included articles and relevant reviews.
Study selection
Two authors (HTL and QYS) independently screened all titles and abstracts to determine eligibility for our review. If these items did not present sufficient information to decide eligibility, the full text was evaluated. Disagreements were resolved through discussion or, when necessary, decided by a third expert (YMX).
Studies had to have an observational design and involve a control group of non-appendectomy subjects matched to appendectomy subjects for age, sex, lifestyle hobbies, comorbidity, etc. These control subjects had to have PD if the study examined age at PD onset or PD severity. Other inclusion criteria included: publication in English; confirmation of appendectomy history based on procedural codes or patient interviews and reporting of the surgical details; reporting numbers of PD cases, age at PD onset and standardized assessment of PD severity; follow-up lasting at least 10 years to ensure detection of outcomes; and reporting adjusted relative risk (RR), hazard ratio (HR) or odds ratio (OR) with corresponding 95% confidence intervals (CIs), or the corresponding original data to allow calculation of these values. If multiple studies reported data on overlapping populations, only the study with larger sample or longer follow-up was included.
Studies were excluded if they were editorials, letters, meta-analyses, reviews, meeting abstracts, experimental studies or case reports unsuitable for quantitative analysis; failed to define the study population or recruited one using an invalid method; did not include a suitable comparison or control group; did not report on any of the desired outcomes (PD risk, age at PD onset or PD severity); or reported on desired outcome(s) but not in sufficient detail to calculate adjusted risk estimates.
Data extraction
Two reviewers (HTL and QYS) independently extracted the following data from the included studies into a predesigned table: first author, year of publication, country, study design, population source, study period, sample size, appendectomy history and reason for surgery, number of individuals with or without PD and with or without appendectomy history, mean (± SD) age at PD onset, and adjusted risk estimates with corresponding 95% CIs. If risk estimates were not reported, an RR was calculated from the original data. The tables from the two reviewers were compared to correct any errors.
Quality assessment
The Newcastle–Ottawa Scale (NOS) was adopted to assess the quality of these non-randomized studies [15]. This scale assesses selection, comparability and outcome/exposure (in cohort/case–control studies, respectively). Based on previous literature, we defined studies that reached a total score ≥ 7 points out of a maximum 9 as high quality [16, 17].
Statistical analysis
Continuous data were transformed as described [18] to obtain means (± SD) for synthesis. Given the low incidence of PD, we assumed that adjusted HRs and ORs could be considered equivalent to the more conservative RR, and so, all risk estimates were treated as RR in our meta-analysis. Pooled RRs or standard mean differences (SMDs) with corresponding 95% CIs were calculated using a random-effects inverse variance method. Heterogeneity across studies was measured using the I2 statistic, with 25% ≤ I2 < 50% defined as low heterogeneity; 50% ≤ I2 < 75%, moderate heterogeneity; and ≥ 75%, high heterogeneity [19]. Sources of heterogeneity were investigated through subgroup analyses based on sex, study quality, sample size, geographical location and follow-up duration. Sensitivity analysis was conducted by removing each study individually and repeating the analysis. Publication bias was not assessed because too few studies were included in the meta-analysis [20].
All statistical analyses were undertaken using Stata/MP 14.0 (StataCorp LP, Texas, USA). All statistical tests were two-tailed, and P < 0.05 was considered significant.
Results
Search results and study characteristics
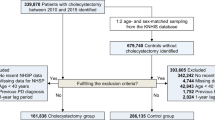
Our database searching yielded 408 potentially relevant articles. After removing duplicates, 302 were screened and six were included in the end (Fig. 1) [9,10,11,12,13,14]. The six studies were published in 2016 or later and involved a total of 3,554,540 individuals in Sweden, USA, Portugal, Canada, Denmark and Germany (Table 1). Four studies analyzed nation- or province-wide data on samples ranging from 85,994 to 1,698,000 people [9, 10, 12, 13], while two involved much smaller samples of 295 [11] and 1,625 people [14]. Three studies applied a data linkage method [9, 12, 13], while others were based on self-reported [10, 11] or chart review [14] appendectomy history. One study utilized a case–control design [14], while the other five studies employed a cohort design, three were prospective [10, 12, 13], one was retrospective [11], and the remaining one used both prospective and retrospective designs because the authors conducted two complementary epidemiological studies together [9].
Quality of included studies
Quality assessment of five of the included studies for PD risk analysis gave an average score of 7 points (range 5–8; Table S2), suggesting reasonably high quality. We did not determine the exact quality score for one study [11] and defined it’s low-quality because we considered that its cases did not adequately representative and there was a lack of comparable control, and it was only included in subsequent meta-analysis of appendectomy on age at PD onset.
Meta-analysis
Appendectomy and risk of PD
Data from five studies involving 3,553,396 people were meta-analyzed to assess the potential relationship between appendectomy and PD risk [9, 10, 12,13,14]. Risk did not vary significantly with previous appendectomy or not (RR 1.02, 95% CI 0.87–1.20, I2 = 83.1%, P = 0.789; Fig. 2).
Appendectomy and age at PD onset
Data from three studies involving 1983 PD patients were meta-analyzed to explore the potential correlation between appendectomy and age at PD onset [9, 11, 14]. Age at onset did not differ significantly between those with or without a history of appendectomy (SMD 0.21, 95% CI − 0.03 to 0.44, I2 = 43.4%, P = 0.083; Fig. 3).
Appendectomy and PD severity
Data from three studies involving 1983 PD patients were qualitatively assessed to examine the potential association between appendectomy and PD severity [9, 11, 14]. The data were not meta-analyzed because the studies used different methods to assess severity and report them, some of which were subjective that may induce considerable heterogeneity. Moreover, a scarce of available data made it impossible to quantify effects. All three studies concluded that appendectomy was not related to disease severity, based on the unified PD rating scale, the Hoehn and Yahr Scale score, levodopa equivalent daily dose or disease duration.
Subgroup analyses
We performed several subgroup analyses to explore whether certain factors may affect the potential relationship between appendectomy and PD risk (Table 2). The only significant effect that we observed was for follow-up duration: the one study that followed up longer than 35 years found that appendectomy was associated with reduced risk of PD; whereas, four studies that followed up for shorter periods found appendectomy to be associated with elevated PD risk. We did not perform subgroup analysis based on early or late PD onset because insufficient data were reported in two studies [12, 14].
Discussion
To our knowledge, this is the first systematic review and meta-analysis investigating the impact of appendectomy on PD. Our meta-analysis of all the included studies as well as subgroup analyses suggest that appendectomy does not significantly affect PD risk, age at onset or severity. Despite these negative findings, it remains possible that the appendix acts as a source of α-synuclein that can contribute to PD. Patients who undergo appendectomy later in life may already have accumulated sufficient α-synuclein originating from that organ in order for PD to occur. It is also possible that α-synuclein that contributes to PD originates not only from the appendix but also from the olfactory and gastrointestinal systems, and that these alternative sources continue to drive disease progression even after appendectomy [21, 22]. Further work is needed to determine conclusively whether α-synuclein from the appendix contributes to PD.
One of the difficulties in assessing the potential relationship between appendectomy and PD is the long follow-up needed to ensure that PD is detected. Insufficient follow-up may fail to detect PD in those who go on to develop the disease, leading to false-negative (type II) errors. The follow-up in the five studies whose quality we assessed ranged from 10 years to 52 years. Whether follow-up lasted longer or shorter than 35 years indeed led to opposite relationships between appendectomy and PD risk. The reason for this difference is unclear, since previous work suggests that 20 years is long enough to detect PD in patients who manifest a prodromal phase in the gastrointestinal tract [21]. It may be that appendectomy does reduce PD risk, but only over much longer time frames than have been followed up in the literature.
Another difficulty in assessing the potential relationship between appendectomy and PD is the variety of outcome measures for assessing PD, some of which may be more subjective than others, as well as the potential confounders that may be adjusted (Table 1). This and other factors likely contribute to the substantial heterogeneity among our included studies. For example, the appendectomy groups in some studies were relatively young, suggesting insufficient follow-up, and our meta-analysis did not adjust for several potential confounding variables, such as genetic polymorphism, smoking or medication [23]. We could eliminate the heterogeneity in our meta-analysis only by removing the largest study with the longest follow-up [9] (Fig. 4), which should arguably be the most reliable study. We conclude that exploring whether appendectomy or other factors affect PD involves inherent heterogeneity difficult to eliminate through statistical methods.
Some have suggested that because appendicitis and PD share common inflammatory factors, the inflammatory response associated with appendicitis may promote α-synuclein transmission to the brain [24,25,26]. Others have suggested that appendicitis may be caused by neurotrophic enteric pathogens that lead to PD [7]. However, the decreased PD risk resulting from appendectomy in individuals followed up longer than 35 years [9] argues against these ideas.
This meta-analysis was based on high-quality studies involving more than three million people, suggesting that it should be reliable and capable of demonstrating a relationship between appendectomy and PD risk if one exists. Nevertheless, there was substantial heterogeneity across the studies that we could not eliminate, primarily in the duration of follow-up, the methods used to identify cases and adjustment of different variables.
Despite these limitations, our meta-analysis of the available high-quality evidence suggests no association between appendectomy and PD risk, age at onset or severity. Prospective studies with long follow-up are warranted to (1) determine the sufficient observation time for credible PD diagnosis and to investigate the impact of appendectomy on prodromal gastrointestinal tract dysfunction, (2) develop a more sensitive algorithm for identifying PD or appendectomy history, and (3) explore whether the relationship between appendectomy and PD depends on the reasons for the appendectomy, the type of surgery or the age of the patient.
To conclude, the available evidence suggests no protective effect of appendectomy against PD. Future studies should seek to clarify the role of inflammation, α-synuclein pathology and the gut–brain axis in PD pathogenesis.
References
Hirtz D, Thurman DJ, Gwinn-Hardy K et al (2007) How common are the “common” neurologic disorders? Neurology 68:326–337. https://doi.org/10.1212/01.wnl.0000252807.38124.a3
GBD 2016 Parkinson’s Disease Collaborators (2018) Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17:939–953. https://doi.org/10.1016/s1474-4422(18)30295-3
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601. https://doi.org/10.1002/mds.26424
Chen H, Zhao EJ, Zhang W et al (2015) Meta-analyses on prevalence of selected Parkinson’s nonmotor symptoms before and after diagnosis. Transl Neurodegener 4:1. https://doi.org/10.1186/2047-9158-4-1
Braak H, Del Tredici K, Rub U et al (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Braak H, Rub U, Gai WP et al (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm (Vienna) 110:517–536. https://doi.org/10.1007/s00702-002-0808-2
Gray MT, Munoz DG, Gray DA et al (2014) Alpha-synuclein in the appendiceal mucosa of neurologically intact subjects. Mov Disord 29:991–998. https://doi.org/10.1002/mds.25779
Bhangu A, Soreide K, Di Saverio S et al (2015) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 386:1278–1287. https://doi.org/10.1016/s0140-6736(15)00275-5
Killinger BA, Madaj Z, Sikora JW et al (2018) The vermiform appendix impacts the risk of developing Parkinson’s disease. Sci Transl Med 10:eaar5280. https://doi.org/10.1126/scitranslmed.aar5280
Palacios N, Hughes KC, Cereda E et al (2018) Appendectomy and risk of Parkinson’s disease in two large prospective cohorts of men and women. Mov Disord 33:1492–1496. https://doi.org/10.1002/mds.109
Mendes A, Goncalves A, Vila-Cha N et al (2015) Appendectomy may delay Parkinson’s disease Onset. Mov Disord 30:1404–1407. https://doi.org/10.1002/mds.26311
Marras C, Lang AE, Austin PC et al (2016) Appendectomy in mid and later life and risk of Parkinson’s disease: a population-based study. Mov Disord 31:1243–1247. https://doi.org/10.1002/mds.26670
Svensson E, Horvath-Puho E, Stokholm MG et al (2016) Appendectomy and risk of Parkinson’s disease: a nationwide cohort study with more than 10 years of follow-up. Mov Disord 31:1918–1922. https://doi.org/10.1002/mds.26761
Yilmaz R, Bayram E, Ulukan C et al (2017) Appendectomy history is not related to Parkinson’s disease. J Parkinsons Dis 7:347–352. https://doi.org/10.3233/JPD-171071
Wells GA, Shea B, O’Connell D et al (2014) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, Ottawa. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Feb 2014
McPheeters ML, Kripalani S, Peterson NB et al (2012) Quality improvement interventions to address health disparities. Closing the quality gap: revisiting the state of the science. Agency for Healthcare Research and Quality, Rockville. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0049222/pdf/TOC.pdf
Geng J, Zhang J, Yao F et al (2019) A systematic review and meta-analysis of the associations of vitamin D receptor genetic variants with two types of most common neurodegenerative disorders. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01135-4
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Higgins JPT, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928. Accessed 20 June 2014
Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. http://handbook.cochrane.org. Updated Mar 2011
Stokholm MG, Danielsen EH, Hamilton-Dutoit SJ et al (2016) Pathological alpha-synuclein in gastrointestinal tissues from prodromal Parkinson disease patients. Ann Neurol 79:940–949. https://doi.org/10.1002/ana.24648
Hawkes CH, Del Tredici K, Braak H (2007) Parkinson’s disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol 33:599–614. https://doi.org/10.1111/j.1365-2990.2007.00874.x
Paul KC, Chuang YH, Shih IF et al (2019) The association between lifestyle factors and Parkinson’s disease progression and mortality. Mov Disord 34:58–66. https://doi.org/10.1002/mds.27577
Houser MC, Chang J, Factor SA et al (2018) Stool immune profiles evince gastrointestinal inflammation in Parkinson’s disease. Mov Disord 33:793–804. https://doi.org/10.1002/mds.27326
de Oliveira Machado SL, Bagatini MD, da Costa P et al (2016) Evaluation of mediators of oxidative stress and inflammation in patients with acute appendicitis. Biomarkers 21:530–537. https://doi.org/10.3109/1354750x.2016.1160426
Lema Tome CM, Tyson T, Rey NL et al (2013) Inflammation and alpha-synuclein’s prion-like behavior in Parkinson’s disease—is there a link? Mol Neurobiol 47:561–574. https://doi.org/10.1007/s12035-012-8267-8
Funding
This work was funded by the Basic Conditions Platform Construction Project of Sichuan Science and Technology Department (no. 2019JDPT0015) and the Major Clinical Disease Research Program from the Health and Family Planning Commission of Sichuan Province (no. 17ZD011).
Author information
Authors and Affiliations
Contributions
HTL wrote the main manuscript. YMX provided the study idea. HTL and QYS conducted article literature search, screening, and data extraction. DX and QZZ contributed to analyze and interpret the data. YMX made critical comments and revision for the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, Ht., Shen, Qy., Xie, D. et al. Lack of association between appendectomy and Parkinson’s disease: a systematic review and meta-analysis. Aging Clin Exp Res 32, 2201–2209 (2020). https://doi.org/10.1007/s40520-019-01354-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01354-9