Abstract
Aim
To evaluate operative and prognostic parameters associated with elective versus emergency surgery in a retrospective cohort of elderly patients.
Methods
A total of 533 geriatric patients (aged ≥ 65 years, median age: 73.0 years, 50.7% were females) who underwent either elective surgery (n = 285) or emergency surgery (n = 248) were included in this study. Data on patient demographics, co-morbid disorders, type of surgery and anesthesia, American Society of Anesthesiologists (ASA) physical status (PS) classification, length of hospital stay, length of ICU stay, hospitalization outcome, prognosis (survivor, non-survivor) were obtained from medical records.
Results
Emergency surgery group was associated with higher prevalence of ASA-PS III (48.8 vs. 25.6%, p < 0.001) and ASA-PS IV (19.0 vs. 0.4%, p < 0.001) categories and higher mortality rates (20.6 vs. 4.9% vs. p < 0.001) when compared to the elective surgery group. ASA-PS IV category was associated with oldest patient age (median 82.0 vs. 71.0 years for ASA-PS I and II, p < 0.001 for each and versus 75.0 years for ASA-PS III, p < 0.05) and highest mortality rate (35.4 vs. 3.4% for ASA-PS I, 6.0% for ASA-PS II and 16.5% for ASA-PS III, p < 0.001) as compared with other categories.
Conclusion
In conclusion, our findings in a retrospective cohort of elderly surgical patients revealed high prevalence of co-morbidities, predominance of ASA-PS II or ASA-PS III classes and an overall in-hospital mortality rate of 12.2%. Emergency as compared with elective surgery seems to be associated with older age, male gender, ASA-PS III and IV classes, higher likelihood of postoperative ICU transfer and higher mortality rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to increase in longevity and advances in surgical and anesthetic techniques, the number of elderly patients presenting for surgery is increasing at a rate faster than the aging of the population [1,2,3,4,5,6].
Increased postoperative mortality, higher rates for in-hospital adverse events, prolonged length of hospital stay (LOS), and post-discharge institutionalization are amongst the poor surgical outcomes reported in elderly patients as compared to younger patients [4, 7, 8].
Given the high prevalence of co-morbidities, polypharmacy, functional and cognitive impairment, the recognition of poor prognostic factors for postoperative outcome via a multidisciplinary approach is considered of critical importance in the management of elderly surgical patients [1, 8, 9].
Elderly surgical patients are considered to be exposed to high risks of morbidity and mortality when undergoing both elective and emergency surgery [1, 2]. Anesthesia and perioperative care in elderly population has, therefore, become the main the focus of investigation in the past decade, in terms of preoperative assessment for identification of poor prognostic factors to enable optimal care and an improved clinical outcome [10, 11]. However, when compared to more extensive body of research available addressing the outcome of elective surgery, there are limited data on the outcome of emergency surgery among elderly population [4, 12].
This study was, therefore, designed to evaluate operative and prognostic parameters associated with elective versus emergency surgery in a retrospective cohort of elderly patients.
Methods
A total of 533 geriatric patients (aged ≥ 65 years, median age: 73.0 years, 50.7% were females) who underwent either elective surgery (n = 285) or emergency surgery (n = 248) in a tertiary care center between July 2016 and July 2017 were included in this retrospective study.
The study was conducted in full accordance with local Good Clinical Practice guideline and current legislations, while the permission was obtained from our institutional ethics committee for the use of patient data for publication purposes.
Study parameters
Data on patients demographics (age, gender), co-morbid disorders, type of surgery (elective, emergency, anatomical region) type of anesthesia (general anesthesia, central or peripheral nerve blockade), intraoperative needs for inotropic agents and blood products, American Society of Anesthesiologists (ASA) physical status (PS) classification category (ASA-PS I–IV), postoperative transfer unit (ward, ICU), length of hospital stay (LOS), length of ICU stay, hospitalization outcome (discharge, transfer to other ward, death), prognosis (survivor, non-survivor), were obtained from medical records. Study variables were compared in elective versus emergency surgery groups as well as with respect to ASA-PS categories.
ASA-PS classification
ASA-PS classification is a grading system based on a simple categorization of a patient’s preoperative physical physiological status to predict the operative risk before selecting the anesthetic or performing surgery. Physiological status is classified in six categories including ASA PS I (normal healthy patients with no organic, physiologic, or psychiatric disturbance), ASA PS II (patients with mild systemic disease with no functional limitations), ASA PS III (patients with severe systemic disease and some functional limitation), ASA PS 4 (patients with severe systemic disease that is a constant threat to life with at least one severe disease that is poorly controlled or at end stage), ASA PS 5 (moribund patients who are not expected to survive without the operation) and ASA PS 6 (a declared brain-dead patient whose organs are being removed for donor purposes) [13, 14].
Statistical analysis
Statistical analysis was made using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY). Pearson Chi-Square, Fisher Exact and Fisher–Freeman–Halton tests applied with Monte Carlo simulations were used for the comparison of categorical data, while numerical data were analyzed using Mann–Whitney U and Kruskal–Wallis tests together with Monte Carlo resampling procedures and post hoc Dunn’s test. Data were expressed as “mean (standard deviation; SD)”, median (minimum–maximum) and percent (%) where appropriate. p < 0.05 was considered statistically significant.
Results
Patient demographics and baseline characteristics in emergency versus elective surgery groups
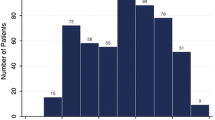
Median age was 73.0 years, while females comprised 50.7% of this retrospective cohort of operated geriatric patients. Hypertension (39.2%), cardiovascular disease (31.3%) and respiratory disease (30.4%) were the three most common co-morbidities in the overall study population. Most of patients were either in ASA-PS II (43.5%) or in ASA-PS III (36.4%) category (Table 1).
Overall, 53.5% of patients underwent elective surgery and 46.5% underwent emergency surgery. Considering demographic and baseline characteristics in emergency versus elective surgery groups, emergency surgery group was associated with older age (median(min–max) 77.0 (65.0–97.0) years versus 72.0 (65.0–100.0) years, p < 0.001), higher percentage of males (55.2 vs. 44.2%, p = 0.012), lesser likelihood of co-morbid hypertension (29.0 vs. 48.1%, p < 0.001), whereas higher likelihood of co-morbid renal (16.1 vs. 1.4%, p < 0.001) and respiratory (45.2 vs. 17.5%, p < 0.001) diseases as well as higher prevalence of ASA-PS III (48.8 vs. 25.6%, p < 0.001) and ASA-PS IV (19.0 vs. 0.4%, p < 0.001) categories as compared with elective surgery group (Table 1).
Operative and prognostic parameters in emergency versus elective surgery groups
Overall, the most common type of anesthesia was general anesthesia (75.4%) as followed by central nerve blockade (19.3%), while open abdominal surgery (33.6%) and extremity surgery (27.2%) were the most common operations. Median operative time was 100 min along with intraoperative need for inotropic support and blood product in 9.8 and 26.3% of patients, respectively. Postoperatively, 51.2% of patients were transferred to an ICU and 48.8% to a ward for a median 3.0 and 8.0 days, respectively. Overall survival rate was 87.8 and 79.5% of survivors were discharged with improvement (Table 2).
General anesthesia in the emergency surgery group (80.7 vs. 70.9%), whereas central nerve blockade in the elective surgery group (24.2 vs. 13.7%) were more commonly applied types of anesthesia (p = 0.009) (Table 2).
Open abdominal surgery (43.1 vs. 25.3%, p < 0.001), urogenital surgery (9.3 vs. 2.8%, p = 0.002) and neurosurgery (5.2 vs. 1.1%, p = 0.009) were more common in the emergency surgery group, whereas neck, thoracic and abdominal wall surgery (28.1 vs. 10.9%, p < 0.001) and thoracic and cardiac surgery (10.9 vs. 2.8%, p < 0.001) were more commonly performed under elective than emergency conditions (Table 2).
No significant difference was noted between emergency and elective surgery groups in terms of intraoperative need for inotropic support and blood products. Significantly higher percentage of patients in the emergency surgery group was transferred to ICU postoperatively as compared with those in the elective surgery group (62.9 vs. 41.1%, p < 0.001) (Table 2).
Emergency surgery was associated with significantly longer ICU stay [median(min–max) 4.0 (0.0–70.0) versus 1.0 (0.0–50.0) days, p < 0.001], shorter LOS [7.0 (0.0–80.0) versus 8.0 (1.0–54.0) days, p = 0.015] and shorter operative time [95.0 (5.0–750.0) min versus 110.0 (10.0–300.0) min, p = 0.023] when compared to elective surgery (Table 2).
Discharge rates were significantly higher (94.7 vs. 62.1%, p < 0.001) and mortality rates were significantly lower (4.9 vs. 20.6%, p < 0.001) in the elective surgery group as compared with the emergency surgery group (Table 2).
No significant difference was noted between survivors and non-survivors in terms of usage of general anesthesia (75.4% for each) or central nerve blockade (20.3 vs. 12.3%, respectively), whereas use of peripheral nerve blockade was significantly more common among non-survivors than in survivors (12.3 vs. 4.3%, p = 0.016) (Table 2).
Demographic, operative and prognostics characteristics according to ASA-PS categories
ASA-PS IV category was associated with oldest patient age (median 82.0 vs. 71.0 years for ASA-PS I and II, p < 0.001 for each, and versus 75.0 years for ASA-PS III, p < 0.05) and highest mortality rate (35.4 vs. 3.4% for ASA-PS I, 6.0% for ASA-PS II and 16.5% for ASA-PS III, p < 0.001) as compared with other categories. Both ASA-PS III and IV categories were associated with more frequent need for intraoperative inotropic support (19.1 and 18.8 vs. 2.6% for ASA-PS II, p < 0.001), higher rate of postoperative transfer to ICU (69.1 and 85.4 vs. 22.0% for ASA-PS I and 36.6% for ASA-PS II, p < 0.001) and longer ICU stay (median 4.0 vs. 0 days for ASA-PS I and II, p < 0.001), while ASA-PS III category was associated with longest LOS (10 vs. 6.0 days for AA-PS I) and 7.0 days for ASA-PS II and IV, p < 0.05 for each) and longest operative time (140.0 vs. 85 min for ASA-PS I, 90 min for ASA-PS II and 77.5 min for ASA-PS IV, p < 0.01 for each) as compared with other ASA-PS categories (Table 3).
Discussion
Our findings in a retrospective cohort of elderly surgical patients revealed high prevalence of co-morbidities, predominance of ASA-PS II or ASA-PS III classes, higher likelihood of receiving general anesthesia and undergoing open intraabdominal surgery along with an overall in-hospital mortality rate of 12.2%.
High prevalence of co-morbidities including hypertension, cardiovascular disease and respiratory disease and of ASA-PS III and IV classes in our cohort support the consideration of elderly people as a heterogeneous population at increased risk of functional limitations and with multiple co-morbidities (i.e., hypertension, respiratory disease, diabetes, hypothyroidism, and heart failure) superimposed on age-dependent anatomical and physiological alterations [12, 15,16,17].
Almost half of patients in our cohort underwent emergency surgery, supporting the growing increase in the number surgical emergency admissions among elderly patients due to demographic shift and drastic decrease in elective surgical interventions after the age of 75 years [15].
Open abdominal surgery was the most frequent type of surgery in our cohort of elderly patients, and more commonly performed under emergency than under elective conditions. This seems notable given the association of emergency gastrointestinal surgery with the highest complication and mortality rates in geriatric surgery patient population [1, 18].
Older age, male gender, presence of renal and respiratory co-morbidities and ASA-PS III and IV categories were associated with higher likelihood of undergoing emergency rather than elective surgery in our cohort. This seems also consistent with our findings on the association of emergency surgery with higher likelihood of postoperative ICU transfer, lower rate of hospital discharge and higher mortality rates (20.6 vs. 4.9%) as compared with elective surgery.
Past studies in elderly surgical patients revealed factors such as emergency operation, increased ASA classification and a increment of operative duration to predict increased risk of in-hospital mortality [4, 12], while postoperative morbidity and mortality were also shown to increase progressively with increasing age [2, 4].
Accordingly, in our cohort, ASA-PS IV class was associated with oldest age and highest mortality (35.4%); ASA-PS III class was associated with longest LOS and longest operative time, whereas both ASA-PS III and IV classes were associated with higher rate of postoperative transfer to ICU and longer ICU stay. This seems consistent with the data from past studies indicated poor functional status in older people to be associated with prolonged postoperative LOS, adverse postoperative outcomes and postoperative discharge to a higher level of care [1].
Hence, higher mortality rates in emergency than in elective surgery patients in our cohort seems to be associated with higher prevalence of ASA-PS III and IV categories in our emergency than in elective group of patients, emphasizing the role of existing functional limitations in the postoperative outcome in elderly patients.
ASA IV class was also shown to be associated with the highest mortality rate (33.0%) in a past study of elderly general surgery population, while evaluation of ASA class has been considered useful for surgeons to set realistic goals as well as to give estimates of morbidity and mortality to patients and their caregivers, preoperatively [12, 15].
Accordingly, our findings support the utility of ASA-PS classification system in elderly for preoperative risk stratification and management not only by anesthesia providers, but also by surgeons [1, 12]. This seems notable given that inability to perform preoperative interventions for identification of baseline health, mental and social status and co-morbidities and planning care accordingly in emergency conditions is considered to exacerbate the vulnerability of elderly patients undergoing emergency surgery [12, 18, 19].
Although physicians are considered likely to be reluctant to refer patients for surgical treatment due to risk of advanced age and co-morbidities, neither chronologic age nor the number of co-morbidities were shown to be associated with postoperative morbidity or mortality in elderly patients, suggesting that age per se should not be the limiting factor for surgical referral or treatment [12].
In our cohort, operative time and LOS were longer in patients undergoing elective surgery as compared with those in the emergency surgery group. This seems notable given that increased geriatric operative time (≥ 120 min) is considered to play a major role in the development of postoperative complications [20].
Although clinical perceptions and theoretic considerations suggest regional anesthesia should be safer than general anesthesia in elderly patients, current studies indicate no difference in outcomes [21]. Studies involving regional versus general anesthesia have demonstrated a significant impact on perioperative outcomes such as LOS and ICU utilization in patients receiving regional anesthesia [22]; however, randomized studies and a meta-analysis of several randomized clinical trials have shown little evidence of improved outcome and reduced post-operative morbidity and mortality via regional anesthesia [23, 24].
No significant difference was noted between ASA-PS classes in terms of selected anesthesia in our cohort, while use of general anesthesia was more common in the emergency versus elective group and peripheral nerve blockade was more commonly applied among non-survivor versus survivors.
Past studies among elderly surgical patients revealed no difference between peripheral nerve blocks and general anesthesia in terms of mortality and complication rates, while also emphasize a dramatic increase in implementation of peripheral nerve blocks among elderly patients with no additional increase in mortality, due to advances in anesthetic techniques as well as postoperative care over time [25].
Anesthesia choice and management is of critical importance among elderly surgical patients and based on the patient’s preference, co-morbidities, potential postoperative complications and the clinical experience of the anesthesiologist [22, 26]. Nonetheless, the overall therapeutic approach in elderly surgical patients has been suggested to be determined jointly by the surgeon, the geriatrician and the anesthesiologist through a multidisciplinary approach [27].
While the management of elderly patients undergoing surgery is challenging, the provision of proactive preoperative assessment coupled with patient-centered multidisciplinary targeted interventions has been shown to improve outcomes such as LOS, rates of institutionalization and readmission, and functional status in elective surgery [15, 17, 18, 28]. Although performing preoperative interventions is not possible in emergency conditions due to the urgent nature of operative intervention, early identification of patients at a high risk of developing adverse outcomes is considered to be associated with more appropriate allocation of resources in these patients [18].
Certain limitations to this study should be considered. First, due to retrospective single center design, establishing the temporality between cause and effect as well as generalizing our findings to overall elderly surgical population seems difficult. Second, lack of data on concomitant treatments and postoperative complications is another limitation which otherwise would extend the knowledge achieved in the current study. Nevertheless, despite these certain limitations, providing data on emergency versus elective surgery in relation to ASA-PS class in a large scale cohort of elderly surgical patients from a broad spectrum of disciplines, our findings represent a valuable contribution to the literature.
In conclusion, our findings in a retrospective cohort of elderly surgical patients revealed high prevalence of co-morbidities, predominance of ASA-PS II or ASA-PS III classes, higher likelihood of receiving general anesthesia and undergoing open intraabdominal surgery along with an overall in-hospital mortality rate of 12.2%. Emergency as compared with elective surgery seems to be associated with older age, male gender, ASA-PS III and IV classes, higher likelihood of postoperative ICU transfer, lower rate of hospital discharge and higher mortality rates. Our findings emphasize the utility of ASA classification system as an available and robust tool for estimating postoperative in-hospital mortality and setting realistic expectations in elderly patients. There is a need for future high quality prospective studies addressing the utility of risk stratification models in preoperative intervention for elderly surgical patients to be able to set realistic goals and to develop most effective strategies for optimization of postoperative outcome.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pearce L, Bunni J, McCarthy K et al (2016) Surgery in the older person: training needs for the provision of multidisciplinary care. Ann R Coll Surg Engl 98:367–370
McLean RC, McCallum IJ, Dixon S et al (2016) A 15-year retrospective analysis of the epidemiology and outcomes for elderly emergency general surgical admissions in the North East of England: a case for multidisciplinary geriatric input. Int J Surg 28:13–21
Benavides-Caro CA (2016) Anestesia y paciente anciano, en busca de mejores desenlaces neurológicos. Rev Colomb Anestesiol 44:128–133
Turrentine FE, Wang H, Simpson VB et al (2006) Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203:865–877
Klopfenstein CE, Herrmann FR, Michel JP et al (1998) The influence of an aging surgical population on the anesthesia workload: a ten-year survey. Anesth Analg 86:1165–1170
Etzioni DA, Liu JH, Maggard MA et al (2003) The aging population and its impact on the surgery workforce. Ann Surg 238:170–177
Hosking MP, Warner MA, Lobdell CM et al (1989) Outcomes of surgery in patients 90 years of age and older. JAMA 261:1909–1915
Kim KI, Park KH, Koo KH et al (2013) Comprehensive geriatric assessment can predict postoperative morbidity and mortality in elderly patients undergoing elective surgery. Arch Gerontol Geriatr 56:507–512
Shipway DJ, Partridge JS, Foxton CR et al (2015) Do surgical trainees believe they are adequately trained to manage the ageing population? A UK survey of knowledge and beliefs in surgical trainees. J Surg Educ 72:641–647
Murthy S, Hepner DL, Cooper Z et al (2015) Controversies in anaesthesia for noncardiac surgery in older adults. Br J Anaesth 115:15–25
Glance LG, Osler TM, Neuman MD (2014) Redesigning surgical decision making for high-risk patients. N Engl J Med 370:1379–1381
Merani S, Payne J, Padwal RS et al (2014) Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World J Emerg Surg 9:43
Saklad M (1941) Grading of patients for surgical procedures. Anesthesiologist 2:281–284
Dripps RD (1963) New classification of physical status. Anesthesiologist 24:111
Vilches-Moraga A, Fox J (2018) Geriatricians and the older emergency general surgical patient: proactive assessment and patient centred interventions. Salford-POP-GS. Aging Clin Exp Res. https://doi.org/10.1007/s40520-017-0886-5
Desserud KF, Veen T, Søreide K (2016) Emergency general surgery in the geriatric patient. Br J Surg 103:52–61
Torrance ADW, Powell SL, Griffiths EA (2015) Emergency surgery in the elderly: challenges and solutions. Open Access Emerg Med OAEM 7:55–68
Khan M, Azim A, O’Keeffe T et al (2018) Geriatric rescue after surgery (GRAS) score to predict failure-to-rescue in geriatric emergency general surgery patients. Am J Surg 215:53–57
Inouye SK (2000) Prevention of delirium in hospitalized older patients: risk factors and targeted intervention strategies. Ann Med 32:257–263
Saleh A, Thirukumaran C, Mesfin A et al (2017) Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2320 patients. Spine J 17:1106–1112
Roy RC (2000) Choosing general versus regional anesthesia for the elderly. Anesthesiol Clin N Am 18:91–104
Kim S, Brooks AK, Groban L (2014) Preoperative assessment of the older surgical patient: honing in on geriatric syndromes. Clin Interv Aging 10:13–27
Rigg JR, Jamrozik K, Myles PS et al (2002) Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet 359:1276–1282
Novak-Jankovic V (2013) Regional anaesthesia for the elderly patients. Periodicum Biologorum 115:119–123
Liu JL, Wang XL, Gong MW et al (2014) Comparative outcomes of peripheral nerve blocks versus general anesthesia for hip fractures in geriatric Chinese patients. Patient Prefer Adherence 8:651–659
Luger TJ, Kammerlander C, Gosch M et al (2010) Neuroaxial versus general anaesthesia in geriatric patients for hip fracture surgery: does it matter? Osteoporos Int 21(Suppl 4):555–572
Harari D, Hopper A, Dhesi J et al (2007) Proactive care of older people undergoing surgery (‘POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing 36:190–196
Dhesi J (2013) Setting up a proactive service to make surgery safer for older people. The Health Foundation. http://patientsafety.health.org.uk/resources/setting-proactive-service-make-surgery-safer-older-people. Accessed 10 Feb 2018
Funding
No financial support or funding was received for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The design and protocol of this retrospective study were approved by our institutional review board (Date: 19 July 2017, Decision Number: 01).
Informed consent
All patients provided consent for their medical records to be used in a scientific study.
Rights and permissions
About this article
Cite this article
Soyalp, C., Yuzkat, N., Kilic, M. et al. Operative and prognostic parameters associated with elective versus emergency surgery in a retrospective cohort of elderly patients. Aging Clin Exp Res 31, 403–410 (2019). https://doi.org/10.1007/s40520-018-0976-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0976-z