Abstract
Population aging is a worldwide phenomenon with significant and manifold impacts on society. Advanced age correlates with the onset of frailty. In this vulnerable state, the immune response is weakened and a higher susceptibility to infectious diseases is observed. The present narrative review aims to cover the topic of herpes zoster (HZ) and its complications in frail populations. The lifetime risk of developing HZ is estimated at about 20–30%, and the risk increases with age. In older people, HZ can lead to the inability to recover the lifestyle, the interests, and the level of activity that existed before its development. Severity of the disease at presentation and depression are the major correlates of pain burden in patients with acute HZ and postherpetic neuralgia (PHN). The frail elderly need careful assessment prior to treatment initiation and could be affected to a greater extent by treatment-related adverse events. In light of the significant burden caused by HZ and its complications in the frail elderly, the adoption of a preventive strategy appears to be promising, particularly using vaccination in appropriate age- and risk-groups. Although very few vaccine studies consider explicitly the frail elderly as their study population, there is evidence that the live, attenuated vaccine induces significant immunological responses. An adjuvanted recombinant subunit vaccine has recently been approved in Canada, in the United States, in the European Union, and in Japan, and will likely provide additional opportunities for prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Population aging is a worldwide phenomenon with significant and manifold impacts on society.
In 2017, 13% of the global population was represented by people over 60 years old. Current estimates indicate that, in 2050, in most of the world’s regions, with the exception of the African continent, about a quarter of the population will be aged ≥ 60 years and the ≥ 80-year-old population will treble [1].
Advanced age correlates with the onset of frailty: a condition that still lacks a standard definition. Frailty is commonly defined as a clinically identifiable state of vulnerability associated with the age-related decline of the functions and reserves of various physiological systems. It is important to highlight at this point that co/multi-morbidity and disability, though related to frailty and sometimes overlapping with it, represent distinct concepts [2]. There are currently two general models that try to describe and explain the features of frailty: the phenotype model [3] and the cumulative deficit model [4].
In the phenotype model, frailty is defined according to clinically observable traits that, if present, are predictive of a poorer outcome; specifically, the frailty syndrome (phenotype) is established when ≥ 3 of these criteria are fulfilled: unintentional weight loss (> 4.5 Kg in the previous year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity [3].
In the cumulative deficit model, the clinical deficits associated with aging (which can be symptoms, signs, abnormal test results, or diseases) are counted for an individual. More commonly in clinical practice, a concise Clinical Frailty Scale is constructed (ranging for example from Very Fit to Severely Frail), that allows for the existence of frailty over a spectrum, which is more in line with common clinical experience [4,5,6].
According to a holistic view of the individual, frailty is “a dynamic state affecting an individual who experiences losses in one or more domains of human functioning (physical, psychological, and social), which is caused by the influence of a range of variables and which increases the risk of adverse outcomes” [7].
As previously mentioned, the prevalence of frailty increases with age and, according to a recent study, is about 10% in people aged > 65 years, reaching between 25 and 50% in persons aged > 85 years [8].
Among the several avenues of research in this area, one of particular interest is the potential role of age-induced modifications of the immune-endocrine axis in determining frailty. Studies have investigated the interlinked phenomena of sarcopenia, immune senescence, and chronic inflammation in aging (“inflammageing”), finding alterations in blood hormone concentrations [for example, lower levels of dehydroepiandrosterone sulphate (DHEAS) and a higher cortisol:DHEAS ratio] and in both the innate and adaptive branches of the immune system at cellular and molecular (cytokines) levels [9,10,11].
This state of immunosenescence causes a higher susceptibility to infectious diseases [12].
Therefore, it is not surprising to find that the association between infectious agents and frailty has been investigated in several studies. In particular, herpesviruses, with their ability to establish lifelong latent infections with possible reactivations [13], have been studied for possible associations with frailty. Such studies have yielded conflicting results, with associations sometimes found between cytomegalovirus (CMV) antibodies and frailty, whereas antibodies against varicella zoster virus (VZV), Epstein–Barr Virus (EBV), and herpes simplex virus 1 and 2 (HSV-1 and HSV-2) were not associated with risks of incident frailty [14,15,16]. Considering the relevance of cell-mediated immunity (CMI) in the immune response to these viruses, measurement of antibodies might not be the most appropriate marker for investigating such associations [17, 18].
The drop in CMI that occurs with advancing age correlates with the incidence/onset of herpes zoster (HZ) and, especially in the over 50 s, with both incidence and severity of HZ [19, 20].
In light of the above considerations, the occurrence of HZ in frail elderly individuals will become more prevalent in the future with its attendant problems of care, long-term complications, and prevention [21, 22].
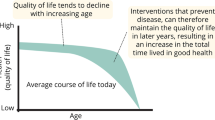
The World Health Organization (WHO) promotes active aging as a way to optimize opportunities for health, participation, and security, in order to improve the quality of life of the elderly [23].
Among currently available preventive measures, vaccination certainly plays an important role in promoting active and healthy aging [24].
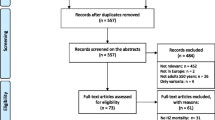
In the present narrative review, we aim to cover the topic of HZ (and its complications) in frail populations in terms of epidemiology, impact, clinical management, and preventive measures.
Varicella zoster virus (VZV) is an alpha herpesvirus, with human hosts as its exclusive reservoir, transmitted through the airborne route and through direct contact with lesions. Primary VZV infection causes varicella (chickenpox) following which the virus remains in a latent state within cranial or spinal nervous ganglia for years/decades [25].
HZ is a disorder involving the sensory ganglion, nerves, and skin, that is caused by the reactivation of VZV [26, 27].
HZ appears in the form of an often severe and painful rash, which typically resolves within 1 month of presentation. However, about 20% of the affected individuals will continue to experience pain in the area of the rash, also after resolution, developing postherpetic neuralgia (PHN) [28].
PHN is a common and much feared complication of HZ, usually defined as pain that persists for over 90 days following the onset of the herpetic rash. PHN can last for months or years, and have a significant impact on the quality of life of affected individuals [29]. In a study performed in Italy on immune competent individuals 50 years and older diagnosed with HZ, 89.6% of patients reported HZ-associated pain at the first medical examination [30]. Following a systematic review, the risk of developing PHN is variable (5–30%) due to different study design, definition of PHN, and population age. According to some studies, about 30–50% of patients that develop PHN will experience pain for more than a year [31].
Pain intensity at the rash onset, age, rash severity, length of prodromal pain, and cranial localization are more frequently reported as predictors of PHN, although it is unclear whether one or all of these factors are equally relevant [28, 32,33,34,35]. PHN can become a severe and debilitating condition affecting all aspects of a patient’s life and placing an economic and social burden on patients’ caregivers [36, 37].
Epidemiology and impact
In the prevaccine era, in temperate-climate regions, fewer than 5% of adults were still susceptible to primary infection with VZV (varicella), that was usually acquired before adolescence. In tropical-climate regions, VZV is more commonly acquired among adolescents and adults [38].
The lifetime risk of developing HZ is estimated at about 20–30% [39] and increases with age, such that 50% of the 85 years old population is expected to develop an episode of HZ [38]. Despite the fact that age is the most important risk factor for the occurrence of HZ and that 90% of affected patients are immunocompetent [30], disease- or treatment-related immunodepression can increase the risk of developing HZ [39].
Incidence rates of HZ in Europe, Asia-Pacific, and North America vary between 3 and 5/1000 person-years. At 60 years of age, the incidence rates are between 6 and 8/1000 person-years and reach up to 8–12/1000 person-years at 80 years of age. Available data for Asia, Africa, and Latin America are limited; it is likely that HZ is not currently perceived as a health priority in these regions, but, in the future, the proportion of elderly people living in those areas will increase with a concomitant increase of HZ cases [31].
In Europe, 1.7 ± 0.1 million new cases are estimated to occur every year. Considering different age groups, the following incidence rates can be observed: 1/1000 in children under 10 years, 2/1000 in adults under 40 years, 1–4/1000 in adults between 40 and 50 years, up to 7–8/1000 after 50 years, and 10/1000 in the over 80 years [40].
A recent study performed in the Japanese population, which has the highest percentage of elderly individuals in the world, showed that the incidence rate in individuals over 60 years and in the over 80 years is comparable to the worldwide rate in the same age groups and that women are affected to a higher extent (60.2% of cases) [41].
Recent Italian data show an overall population rate of 6.4 cases/1000 person-years and a rising incidence rate with advancing age [42], thus confirming the observations from the previous studies [43].
The HEROES study analyzed the onset and persistence of pain in 413 immunocompetent patients over 50 years of age with a new diagnosis of HZ. Pain was reported by patients (89.6%) and then measured with a Visual Analog Scale (VAS) score (mean score 5.8). Among patients who completed the 3-month visit, 20.6% showed pain, thus fulfilling all the criteria that define PHN (mean VAS score 3.7). The percentage of patients with PHN increases with age. Predictive factors for the development of PHN were found to be the presence of a high number of vesicles (≥ 50), male sex, and a VAS score ≥ 3 [30]. Such a level of pain intensity is considered to be related to interference in Activities of Daily Life (ADLs). A subsequent analysis of the whole sample, showed that 73% of patients with a new diagnosis of HZ had comorbidities and 69% were over 65 years of age. The most frequent comorbidities were cardiovascular diseases (75%), diabetes (24%), and respiratory diseases (17%). The presence of pain at 3-month visit was significantly higher in patients with underlying conditions. Allodynia, paresthesia, pruritus, and VAS ≥ 3 were also more common in these patients [44].
Possible risks for people with HZ are ischemic events such as Transient Ischemic Attacks (TIAs), stroke, and myocardial infarction; these conditions are related to the systemic inflammatory state triggered by the virus, which also affects vascular structures with the possibility of inducing endothelial damage and thrombosis [45].
The risk of stroke is higher in the first month after the episode of HZ [relative risk RR = 1.78 (95% CI 1.70–1.88)] and tends to diminish with time. It is higher in cases of herpes zoster ophthalmicus (HZO) [RR = 2.05 (95% CI 1.82–2.31)] in the first month after the episode), since ocular involvement is more frequently associated with inflammation of cerebral blood vessels [46].
In older people, HZ can lead to a permanent drop of the ability to be independent and to the inability to recover preHZ lifestyle, interests, and level of activity. When pain persists in the form of PHN, the negative effect on the life of patients affects not only the physical, but also the social and psychological domains with an impact on spouses and relatives [37]. The most frequently affected daily activity in patients with HZ or PHN is sleep, whereas psychological manifestations include stress, anxiety, and depressive symptoms. Consequences in the family environment and in the social sphere affect over 50% of individuals with HZ and 81% of individuals with PHN [47]. A study showed that 20% of people surveyed claimed to be isolated from their family and friends, while they were affected with HZ or PHN, with a resultant reduction in communication in 19 and 27% of cases, respectively [48].
Besides affecting the quality of life of patients, HZ also has a strong impact on health care systems.
Hospitalization rates for HZ, considering the overall population, vary between 2 and 25/100,000 person-years [31].
Hospitalization rates are higher in the older age groups; in USA, the rate varies from 10.2/100,000 in the 60–69 age group to 65.1/100,000 in the over 80 s [49].
Following a systematic review of the relevant literature, the costs per hospitalized HZ case in Europe, USA, and Asia were estimated at 774.66-31,026.22 €, 9,041.36-23,219.82 €, and 118.13-707.23 €, respectively; a hospitalized PHN case in Europe has an average cost of 4,026.05 €, whereas in USA, the cost is estimated to be between 1,538.17 € and 3,130.88 €. The observed variation between different world areas is not due to epidemiological differences but to factors such as the socioeconomic development level and the type of health care system of the selected country [50].
Data from England from 2004 to 2013 report a yearly average rate of 8.8/100,000 hospital admissions and confirm a high prevalence (71.5%) in individuals ≥ 60 years old (incidence of 28.4/100,000). Overall, 82% of cases occur in immunocompetent people and hospitalizations are more common in women. The yearly average number of days of hospitalization and the related cost stand at 41,780 days and 13 million £, respectively [51].
A recent Italian study analyzed data about hospital admissions from the period 2001–2013. The general hospitalization rate was 12.1/100,000 inhabitants/year with a decreasing temporal trend, from 16.5/100,000 in 2001 to 8.9/100,000 in 2013. The number of hospitalization increased with age [52]. For more details, see Table 1. The total economic impact of HZ and PHN in immunocompetent individuals > 50 years of age in Italy amounted to 41.2 million euros, of which at least a third was attributable to indirect costs related to productivity loss [43].
Management
Severity of the disease at presentation and depression are the major correlates of pain burden in patients with acute HZ and PHN [33, 34, 53].
The duration of HZ pain varies considerably, ranging from no pain or pain that lasts for only a few days after rash onset to pain that lasts for years after rash healing [26].
It is important to note that the frail elderly need careful assessment prior to treatment initiation and that they could be affected to a greater extent than “normal” adults by treatment-related adverse events, both in terms of frequency and in the possible severity of outcomes. More specifically, in the event of renal impairment, which is a frequent occurrence in the frail elderly, dosage has to be adjusted depending on creatinine clearance and adequate hydration needs to be ensured (another common problem in the frail elderly whose thirst reflex is diminished). The risk of neurological adverse events (such as headache, dizziness, confusion, tremor, convulsions, etc.) is also increased and their consequences can be serious, leading, for example, to falls with a high risk of fractures potentially leading to a vicious cycle of worsening frailty [54].
Acute phase management of HZ
Antiviral treatment
In HZ patients, antiviral drugs accelerate the resolution of skin lesions and acute pain, and reduce the duration of chronic pain. Table 2 summarizes the doses, side effects, and contraindications of the drugs currently available for the management of acute HZ in adults. Acyclovir was the first oral antiviral therapy to be investigated for treatment; it decreases virus shedding and new lesion formation, accelerates healing, and decreases acute pain if started within 48–72 h of rash onset and given for 7 days. Valacyclovir, famciclovir, and brivudin are superior to acyclovir for the treatment of HZ, and have the advantage of simpler dosing regimens. The latter is not licensed in North America and its use requires caution as it is contraindicated in patients treated with 5-fluoropyrimidines (5-FPs) and substances that are converted by the body to 5-FPs (such as, for example, cancer treatment regimens with 5-fluorouracil or substances converted to 5-fluorouracil). Famciclovir is comparable with valacyclovir, but the suggested doses vary widely in different countries [55].
Analgesic treatment
There is no published evidence base for the optimal treatment of acute pain in HZ, but combining antiviral therapy with additional effective relief of acute pain is indicated from a clinical viewpoint (Table 3).
Selected Complications other than PHN
The most frequent complications of HZ are listed in Table 4 [56]. The incidence and burden of complications other than PHN have not been widely studied, but ocular diseases and facial palsy seem to be the most frequent HZ-related complications in several studies worldwide, although with different frequencies [57, 58].
Treatment of postherpetic neuralgia (PHN)
PHN can be difficult to treat. It requires a thorough evaluation of the characteristics of the symptoms and sensory findings, as well as of the extent to which everyday living activities are affected. Since treatments also have side effects, careful counselling with frequent reviews and a willingness to adjust doses is essential. After an appropriate trial of the first-line therapy, it may be necessary to progress to alternative treatments on more than one occasion.
There is evidence that tricyclic antidepressants (TCAs), gabapentinoids, opioids, and topical capsaicin are effective in PHN [59]. Topical lidocaine gel (5%) or topical lidocaine patch (5%) also showed efficacy for PHN [59]. A guidance for the use of drugs for PHN is shown in Table 5 [60].
Prevention
In light of the significant burden caused by HZ and its complications (mainly PHN), the adoption of a preventive strategy appears to be particularly promising. In this respect, two main forms of prevention can be envisaged:
-
Prevention of HZ itself, and thus of its complications, using vaccination in appropriate age groups (primary prevention), Table 6.
-
Prevention of complications of HZ (mainly PHN) as soon as the disease has manifested itself by early and aggressive treatment (in essence a form of secondary prevention), although only supported by relatively weak evidence.
In the following sections, we will focus on the former, given that the latter has been covered in the “Management” section. It is sufficient to highlight here that the early and aggressive treatment option suffers from drawbacks, as alluded to earlier. From a pathophysiological stand point, in many cases, damage has already occurred before treatment initiation and from a “practical”/clinical stand point, the requirement for antiviral treatment to start within 72 h after HZ onset to be effective can prove difficult to fulfill in practice.
The live-attenuated Oka vaccine strain of VZV
The currently licensed vaccine is a live-attenuated Oka vaccine strain of VZV (OkaV); in this respect, it is identical to the varicella vaccine, but contains an approximately 14-fold higher concentration of OkaV virus than the varicella vaccine [61, 62].
The OkaV vaccine has been available both in USA and in the EU since 2006 and substantial knowledge on its efficacy, safety, and effectiveness has been accumulated. The main outstanding issue with the OkaV vaccine is related to the fact that it is a live-attenuated vaccine, which, in spite of it being the most attenuated of live viral vaccines [63], is currently contraindicated in immunocompromised individuals (immunodeficient or immunosuppressed), in line with other live-attenuated viral vaccines [61, 62]. This contraindication renders its use in immunocompromised individuals to be problematic. Since, as outlined in the introduction, the immune-endocrine axis is one of the body systems involved in the occurrence of frailty in the elderly, the above contraindication could represent a concern in HZ prevention in this special population, though it is by no means established that the immune system alterations associated with frailty confer an increased risk of adverse events upon OkaV vaccine administration [10]. On the other hand, many of the frail elderly also suffer from comorbidities that increase their likelihood of developing HZ and its attendant complications, and they would benefit from HZ prevention. The choice of vaccination in the elderly is, therefore, a delicate balancing act between safety and efficacy of vaccines and the risks of developing infectious diseases and their complications [64]. Most available studies of the use of OkaV vaccine in the elderly with comorbidities and/or varying degrees of immunocompromised conditions have not considered explicitly frailty criteria in the selection of the sample, although their findings could be applied with caution to the frail elderly who share many of the same conditions.
In a very recent study, however, the immunogenicity of OkaV vaccine and immunologic markers of VZV-specific T-cell-mediated immunity (as an interferon-gamma ELISPOT assay) associated with a response to OkaV vaccine and cellular markers of immune senescence were evaluated specifically in the frail elderly. The study was performed in a cohort of 190 frail nursing home residents with a mean age of 89 years (range 80–102 years) and at least one comorbidity, and in a cohort of 50 community-dwelling seniors, used as a comparison group, with a mean age of 67 years (range 60–75 years) and a maximum of one comorbidity. Frailty was assessed with a validated 70-item (variables) frailty index score based on the cumulative deficit model, and calculated as the ratio between the number of deficits and the total number of items. The two groups were given OkaV vaccine and had blood samples taken at the same visit the vaccine was administered and 6 weeks later. Results showed that, as foreseen, the frail elderly exhibited higher levels of immunosenescence at baseline, but interestingly, they were still able to respond to OkaV vaccine by mounting potentially protective responses. Clearly, as acknowledged by the authors, a limitation of the study is the limited time frame and the lack of direct information on protective clinical efficacy [65].
Another outstanding issue with the OkaV vaccine is related to the duration of protection, which has been shown to wane over time and which has not been established beyond 5 year postvaccination [62].
Other vaccines derived from the Oka vaccine strain of VZV
Heat-inactivated Zoster vaccine
To have a vaccine that could be safely administered to immune compromised individuals, attempts have been made to develop a heat-inactivated OkaV zoster vaccine. Some trials have been performed in different groups of immune compromised individuals, with mixed results but, at the time of writing, the heat-inactivated vaccine has not been licensed [66,67,68].
Adjuvanted VZV subunit vaccine
The sequencing of the VZV genome and the identification of the role of specific genes encoding specific viral components and of their function has made it possible to select candidates suitable for inclusion in a vaccine. The development of an adjuvanted VZV subunit vaccine, named Adjuvanted Recombinant Zoster Vaccine (RZV), therefore, represents a new approach to the problem of varicella and HZ prevention [63].
The RZV is based, on one hand, on the recombinant VZV glycoprotein E as the target epitope and, on the other hand, on a liposome-based adjuvant system (AS01B). Studies have shown that a two-dose schedule can induce robust VZV-specific T-cell responses that last for at least 6 years after vaccination [63].
Two international phase III randomized, double-blind, placebo-controlled clinical trials were conducted concurrently at the same study sites and using the same methods to assess the efficacy and safety of RZV in preventing HZ in two different populations. The ZOE-50 study (NCT01165177) included adults ≥ 50 years of age [69] and ZOE-70 (NCT01165229) included adults ≥ 70 years of age [70]. In the ZOE-50 study, the incidence of HZ was 0.3/1,000 person-years (PY) in the RZV group and 9.1/1,000 PY in the placebo group with an estimated overall vaccine efficacy (VE) in preventing HZ of 97.2% [69]. In a pooled analysis of over 70 years old from both ZOE 50 and ZOE-70, the HZ incidence in the RZV group was 0.9/1,000 PY and 9.2/1,000 in the placebo group and the estimated overall VE against HZ was 91.3% [70].
If adult HZ vaccination was to be globally adopted, it could lead to a dramatic reduction in the incidence of PHN. Combining this with the long-term effect (40 + years) of childhood varicella vaccination, future generations might be largely immune to PHN.
According to available information, the protection is maintained for up to 4 year postvaccination and the duration of protection beyond 4 years is under investigation [71].
The vaccine has first been approved in Canada and in the United States, and more recently in Japan and in the European Union [72].
Conclusions
The concept of frailty has become an important tool in geriatric practice but, as is often the case with the elderly population, specific clinical studies are very few or unavailable. In the case of HZ prevention, to our knowledge, only two published studies were performed in a population of nursing home residents. It is very often the case that treatment (and prevention) decisions have to be extrapolated from data collected in other population groups, which requires caution given the propensity of the frail elderly to experience more frequent and more severe adverse effects to treatment, with outcomes that can lead to worsening degrees of frailty and higher mortality. Though not easy to perform, further research would be needed in this special and numerically growing population.
References
United Nations, Department of Economic and Social Affairs, Population Division (2017) World population prospects: The 2017 revision, key findings and advance tables. Working paper no. ESA/P/WP/248. https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf. Accessed 10 July 2017
Fried LP, Ferrucci L, Darer J et al. (2004) Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 59:255–263
Fried LP, Tangen CM, Walston J et al (2001) Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-56
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173:489–495
British Geriatrics Society (2014) Fit for Frailty—consensus best practice guidance for the care of older people living in community and outpatient settings—a report from the British Geriatrics Society
Rockwood K, Mitnitski A, MacKnight C (2002) Some mathematical models of frailty and their clinical implications. Rev Clin Gerontol 12:109–117
Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT et al. (2010) In search of an integral conceptual definition of frailty: opinions of experts. J Am Med Dir Assoc 11:338–343
Clegg A, Young J, Iliffe S et al. (2013) Frailty in elderly people. Lancet 381 868:752–762
Wilson D, Jackson T, Sapey E et al. (2017) Frailty and sarcopenia: the potential role of an aged immune system. Ageing Res Rev 36:1–10
Baylis D, Bartlett DB, Syddall HE et al (2013) Immune-endocrine biomarkers as predictors of frailty and mortality: a 10-year longitudinal study in community-dwelling older people. Age (Dordr) 35:963–971
Wang GC, Casolaro V (2014) Immunologic changes in frail older adults. Transl Med UniSa 24:1–6
Caruso C, Buffa S, Candore G et al (2009) Mechanisms of immunosenescence. Immun Ageing 6:10
Cohen JI (2014) Introduction to Herpesviridae. In: Mandell GL, Bennett JE, Dolin R (eds) Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 8th edn. Elsevier, Philadelphia
Wang GC, Han C, Detrick B et al (2016) Herpesvirus infections and risk of frailty and mortality in older women: Women’s Health and Aging Studies. J Am Geriatr Soc 64:998–1005
Haeseker MB, Pijpers E, Dukers-Muijrers NH et al (2013) Association of cytomegalovirus and other pathogens with frailty and diabetes mellitus, but not with cardiovascular disease and mortality in psycho-geriatric patients; a prospective cohort study. Immun Ageing 10:30
Goldeck D, Pawelec G, Norman K et al (2016) No strong correlations between serum cytokine levels, CMV serostatus and hand-grip strength in older subjects in the Berlin BASE-II cohort. Biogerontology 17:189–198
Levin MJ (2012) Immune senescence and vaccines to prevent herpes zoster in older persons. Curr Opin Immunol 24:494–500
Weinberg A, Zhang JH, Oxman MN et al (2009) US Department of Veterans Affairs (VA) Cooperative Studies Program Shingles Prevention Study Investigators. Varicella-zoster virus-specific immune responses to herpes zoster in elderly participants in a trial of a clinically effective zoster vaccine. J Infect Dis 200:1068–1077
SAGE Working Group on Varicella and Herpes Zoster Vaccines. Background paper on Herpes zoster vaccines. 2014 Mar. http://www.who.int/immunization/sage/meetings/2014/april/2_Background_document_Herpes_Zoster.pdf?ua=1. Accessed 10 July 2017
Franco E, Zorzoli E, Valente N et al. (2016) Aspetti epidemiologici dell’Herpes zoster e della nevralgia post-erpetica [Epidemiological aspects of Herpes zoster and post-herpetic neuralgia]. In: Gabutti G (ed) Herpes zoster e nevralgia post-erpetica. Edizioni Minerva medica, Torino, pp 17–26 (Italian)
Varghese L, Standaert B, Olivieri A et al. (2017) The temporal impact of aging on the burden of herpes zoster. BMC Geriatr 17:30
Maggi S, Gabutti G, Franco E et al (2015) Preventing and managing herpes zoster: key actions to foster healthy aging. Aging Clin Exp Res 27:5–11
WHO. Active ageing: a policy framework. WHO/NMH/NPH/02.8. 2002. http://apps.who.int/iris/bitstream/10665/67215/1/WHO_NMH_NPH_02.8.pdf. Accessed 10 July 2017
Gabutti G, Bonanni P, Conversano M et al (2017) Prevention of Herpes Zoster and its complications: from clinical evidence to real life experience. Hum Vaccin Immunother 13:391–398
Stefanati A, Kuhdari P, Bertoni L et al. (2016) Storia naturale e risposta immunitaria nell’infezione da Varicella-zoster virus: varicella ed Herpes zoster [Natural history and immune response in Varicella-zoster virus infection: varicella and herpes zoster]. In: Gabutti G (ed) Herpes zoster e nevralgia post-erpetica. Edizioni Minerva medica, Torino, pp 9–16 Italian.
Dworkin RH, Schmader KE (2001) The epidemiology and natural history of herpes zoster and post-herpetic neuralgia. In: Watson CP, Gershon AA (eds) Herpes zoster and post-herpetic neuralgia, 2nd edn. Elsevier Press, New York, pp 39–64
Gershon AA, Gershon MD, Breuer J et al (2010) Advances in the understanding of the pathogenesis and epidemiology of herpes zoster. J Clin Virol 48:S2–S7
Opstelten W, Mauritz JW, de Wit NJ, et al (2002) Herpes zoster and postherpetic neuralgia: incidence and risk indicators using a general practice research database. Fam Pract 19:471–475
Cohen JI (2013) Clinical practice: Herpes zoster. N Engl J Med 369:255–263
Bricout H, Perinetti E, Marchettini P et al (2014) Burden of herpes zoster-associated chronic pain in Italian patients aged 50 years and over (2009–2010): a GP-based prospective cohort study. BMC Infect Dis 14:637
Kawai K, Gebremeskel BG, Acosta CJ (2014) Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open 4:e004833
Jung BF, Johnson RW, Griffin DRJ, et al (2004) Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology 62:1545–1551
Volpi A, Gatti A, Serafini G et al (2007) Clinical and psychosocial correlates of acute pain in herpes zoster. J Clin Virol 38:275–279
Volpi A, Gatti A, Pica F et al (2008) Clinical and psychosocial correlates of post-herpetic neuralgia. J Med Virol 80:1646–1652
Gatti A, Pica F, Boccia MT et al (2010) No evidence of family history as a risk factor for herpes zoster in patients with post-herpetic neuralgia. J Med Virol 82:1007–1011
Pica F, Gatti A, Divizia M et al (2014) One-year follow-up of patients with long-lasting post-herpetic neuralgia. BMC Infect Dis 14:556
Johnson RW, Bouhassira D, Kassianos G et al. (2010) The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 8:37
WHO (2014) Varicella and herpes zoster vaccines: WHO position paper, June 2014. Wkly Epidemiol Rec 89:265–288 (English, French)
Johnson RW, Wasner G, Saddier P et al (2008) Herpes Zoster and postherpetic neuralgia: optimizing management in the elderly patient. Drugs Aging 25:991–1006
Pinchinat S, Cebrián-Cuenca AM, Bricout H et al (2013) Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis 13:170
Sato K, Adachi K, Nakamura H et al (2017) Burden of herpes zoster and postherpetic neuralgia in Japanese adults 60 years of age or older: Results from an observational, prospective, physician practice-based cohort study. J Dermatol 44:414–422
Alicino C, Trucchi C, Paganino C et al (2017) Incidence of herpes zoster and post-herpetic neuralgia in Italy: Results from a 3-years population-based study. Hum Vaccin Immunother 13:399–404
Gialloreti LE, Merito M, Pezzotti P et al (2010) Epidemiology and economic burden of herpes zoster and post-herpetic neuralgia in Italy: a retrospective, population-based study. BMC Infect Dis 10:230
Torcel-Pagnon L, Bricout H, Bertrand I et al (2017) Impact of underlying conditions on Zoster-related pain and on quality of life following Zoster. J Gerontol A Biol Sci Med Sci 72:1091–1097
Nagel MA, Jones D, Wyborny A (2017) Varicella zoster virus vasculopathy: The expanding clinical spectrum and pathogenesis. J Neuroimmunol 308:112–117
Marra F, Ruckenstein J, Richardson K (2017) A meta-analysis of stroke risk following herpes zoster infection. BMC Infect Dis 17:198
Gater A, Uhart M, McCool R et al. 2015) The humanistic, economic and societal burden of herpes zoster in Europe: a critical review. BMC Public Health 15:193
Lukas K, Edte A, Bertrand I (2012) The impact of herpes zoster and post-herpetic neuralgia on quality of life: patient-reported outcomes in six European countries. Z Gesundh Wiss 20:441–451
Jackson LA, Reynolds MA, Harpaz R (2008) Hospitalizations to treat herpes zoster in older adults: causes and validated rates. Clin Infect Dis 47:754–759
Panatto D, Bragazzi NL, Rizzitelli E et al (2015) Evaluation of the economic burden of Herpes Zoster (HZ) infection. Hum Vaccin Immunother 11:245–262
Hobbelen PH, Stowe J, Amirthalingam G et al. (2016) The burden of hospitalisation for varicella and herpes zoster in England from 2004 to 2013. J Infect 73:241–253
Valente N, Cocchio S, Stefanati A et al (2017) Temporal trends in herpes zoster-related hospitalizations in Italy, 2001–2013: differences between regions that have or have not implemented varicella vaccination. Aging Clin Exp Res 29:771–779
Schmader K (2016) Herpes zoster. Clin Geriatr Med 32:539–553
Kaye AD, Baluch A, Scott JT (2010) Pain management in the elderly population: a review. Ochsner J 10:179–187
Gnann J (2006) Antiviral therapy for herpes zoster. Herpes 13:16A-20A
Volpi A (2007) Severe complications of herpes zoster. Herpes 14 :35–39
di Luzio PU, Arpinelli F, Visonà G (1999) Herpes zoster and its complications in Italy: an observational survey. J Infect 38:116–120
Oxman MN (2000) Clinical manifestations of herpes zoster. In: Arvin AM, Gershon AA (ed) Varicella-zoster virus: virology and clinical management. Cambridge University Press, Cambridge, pp 246–275
Haanpää M, Rice ASC, Rowbotham MC (2015) Treating herpes zoster and postherpetic neuralgia. PAIN Clin Updates 23:1–8
Hempenstall K, Nurmikko TJ, Johnson RW et al. (2005) Analgesic therapy in postherpetic neuralgia: a quantitative systematic review. PLoS Med 2:e164
VARIVAX Summary of Product Characteristics. https://www.medicines.org.uk/emc/medicine/15264. Accessed 12 July 2017
ZOSTAVAX Summary of Product Characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000674/WC500053462.pdf. Accessed 12 July 2017
Watson CPN et al (2017) Herpes zoster: postherpetic neuralgia and other complications. Springer, Switzerland
Amanna IJ (2012) Balancing the Efficacy and Safety of vaccines in the elderly. Open Longev Sci 6:64–72
Lelic A, Verschoor CP, Lau VW et al (2016) Immunogenicity of varicella vaccine and immunologic predictors of response in a cohort of elderly nursing home residents. J Infect Dis 214:1905–1910
Redman RL, Nader S, Zerboni L et al (1997) Early reconstitution of immunity and decreased severity of herpes zoster in bone marrow transplant recipients immunized with inactivated varicella vaccine. J Infect Dis 176:578–585
Hata A, Asanuma H, Rinki M et al (2002) Use of an inactivated varicella vaccine in recipients of hematopoietic-cell transplants. N Engl J Med 347:26–34
Mullane KM, Winston DJ, Wertheim MS et al (2013) Safety and immunogenicity of heat-treated zoster vaccine (ZVHT) in immunocompromised adults. J Infect Dis 208:1375–1385
Lal H, Cunningham AL, Godeaux O et al (2015) Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Eng J Med 372:2087–2096
Cunningham AL, Lal H, Kovac M et al (2016) Impact of the herpes zoster subunit vaccine in adults 70 years of age or older. N Eng J Med 375:1019–1032
SHINGRIX Product Monograph (Approved 13 October 2017). https://pdf.hres.ca/dpd_pm/00041658.PDF Accessed 20 Dec 2017
European Commission (2018) Community register of medicinal products for human use. http://ec.europa.eu/health/documents/community-register/html/h1272.htm#EndOfPage Accessed 26 Mar 2018
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ermanno Zorzoli Congress attendance sponsored by Sanofi. Francesca Pica has no conflict of interest. Giulia Masetti has no conflict of interest. Elisabetta Franco had scientific collaboration with GSK, Merck, Pfizer and Sanofi, and reimbursement for participation to meetings and advisory boards without personal fees. Antonio Volpi was involved in clinical trials for GSK and Achaogen, and participated to advisory board meetings for GSK and Sanofi Pasteur MSD. Giovanni Gabutti has received grants from GlaxoSmithKline Biologicals SA, Sanofi Pasteur MSD, Novartis,Crucell/Janssen, Seqirus, Sanofi Pasteur, Merck Italy, and Pfizer for being consultant or taking part in advisory board, expert meetings, being a speaker or an organizer of congresses/conferences, and acting as investigator in clinical trials.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Zorzoli, E., Pica, F., Masetti, G. et al. Herpes zoster in frail elderly patients: prevalence, impact, management, and preventive strategies. Aging Clin Exp Res 30, 693–702 (2018). https://doi.org/10.1007/s40520-018-0956-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0956-3