Abstract
Background
The elderly often complain of faintness, lightheadedness, dizziness, and unsteadiness, which may be associated with the orthostatic hypotension (OH), but most of them are subclinical. The pathogenic mechanism of subjective symptoms in the elderly with OH is controversial.
Aims
The aim of this study was to assess the involvement of the irregularity of the vertical perception in the dizzy elderly with OH.
Methods
This study consisted of 403 patients seeking treatment for dizziness in our hospital. The neurotological examinations include the subjective visual vertical (SVV) test and the bithermal caloric test. The self-perceived handicapping effects imposed by dizziness were assessed by the dizziness handicap inventory (DHI). The variability (standard deviation) and the average deviation of eight trials (four trials in each direction) were calculated. In addition, they underwent the orthostatic Schellong test for the diagnosis of the OH. They were separated into three groups, including patients aged ≥65 years, patients aged 50–64 years, and patients aged <50 years.
Results
The variability of the SVV in the patients aged ≥65 years with OH was significantly larger than that in the patients aged ≥65 years without OH. There was no significant difference in the average deviation of the SVV, the canal paresis % by the bithermal caloric test, and the DHI score among groups.
Conclusions
The result suggests that the elderly patients with OH have subclinical impairment in the perception of the verticality independent of the peripheral vestibular function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The elderly often complain of symptoms associated with orthostatic hypotension (OH) which has been explained by a decline of venous return associated with muscle weakness, the decrease in fluid volume, the increase of venous compliance, dysfunction of the baroreflex, and the degradation of cardiac performance [1]. Symptoms of dizziness, faintness, or lightheadedness on standing occur in 5.8 % of the elderly >70 years old, and thus, orthostatic dizziness is not uncommon [2]. The compensatory mechanisms that regulate blood pressure upon standing are dysfunctional in subjects with OH, and the condition may lead to inadequate cerebral perfusion with accompanying symptoms of dizziness, falls, and fractures. However, the pathogenic mechanism of dizziness and unsteadiness in the elderly with OH has not been understood.
Clinical studies emphasize that the subjective visual vertical (SVV) is a sensitive tool for detecting an imbalance in otolith function [3]. Normal subjects can adjust an illuminated rod in an otherwise totally dark room to approximate real vertical. The ability depends primarily on proprioceptive and vestibular cues, the latter usually equated with the tonic afferent input from otolith organs and central graviceptive pathways [4], and a large intra-individual variability of the SVV indicates abnormal subjective perception of verticality independent of the peripheral vestibular function [5].
Various studies have also shown that assessing SVV along with other clinical indicators can allow accurate localization of lesions in the central nervous system involved in the vestibular system (e.g., pontomedullary lesions, pontomesencephalic lesions, thalamic lesions, and parietoinsular vestibular cortex) [6, 7]. The certainty in the perception of the verticality decreases with age, and especially, very old subjects show high uncertainty in determining with their body against the internal vertical [8].
Hypothetically, the elderly with the OH, even if it is asymptomatic, may show the uncertainty in the perception of the verticality, resulting in inducing dizziness or increasing the risk of falls. However, few studies have examined the relationship between the perception of the verticality and the presence of OH in the elderly. The aim of this study was to assess the involvement of the irregularity of the vertical perception in the dizzy elderly with OH.
Materials and methods
Subjects and ethical considerations
This study consisted of 403 patients seeking treatment for dizziness in our hospital. We separated the participants into three groups and analyzed the data of 115 patients aged ≥65 years (male: 64, female: 51, range of age: 65–80 years), 129 patients aged 50–64 years (male: 57, female: 72), and 159 patients aged <50 years (male: 64, female: 95). They routinely underwent the SVV test, bithermal caloric test, and orthostatic Schellong test on the same day within 1 week from the first visit to our hospital. The local Ethics Committee of Gifu University Graduate School of Medicine approved this study. After a complete description of the study, written informed consent was obtained from all patients.
Subjective visual vertical testing
Each subject was seated in an upright position with their head held in place by a chin rest. A 15-cm-long rod of charged fluorescent tape 5-mm wide was placed in front of the subjects at a distance of 1 m. The rod was positioned at eye level in complete darkness (i.e., no frame, no disc) and its starting position was tilted to either the left or the right (approximately 40°). Without time constraints, the subjects were required to adjust the rod to gravitational vertical by rotating the handle of a potentiometer [9]. Eight trials (four trials in each direction) were performed for each subject. The subjects’ performance of SVV adjustment was expressed as a deviation from gravitational vertical (0°) measured in degrees of deviation. Deviations to the left (counter clockwise) were counted as negative, and deviations to the right (clockwise) were counted as positive. The mean as an average deviation and the standard deviation as variability using the absolute value of the deviations to both sides of eight trials were calculated. The greater deviation of SVV indicates an imbalance in otolith function, and the larger variability of SVV may be associated with an abnormal subjective perception of verticality independent of the peripheral vestibular function [5].
Bithermal caloric testing
The bithermal caloric test is a useful clinical test to assess the semicircular canal function. Surface electrodes were placed beside the lateral angle of both eyes and frontal region of the head to detect eye movements as electronystagmography (ENG). The signal was amplified, monitored, and recorded continuously at a rate of 120 Hz using an analog-to-digital converter with programming software (CHARTR VNG/ENG, LCS Medical, Schaumburg, IL, USA). The ENG data were passed a low-pass filter with a high cut-off frequency of 30 Hz. The amplitude was calibrated with the angle of the eye movement in advance. Subjects were shielded light using goggle and positioned in supine with head inclined 30 deg up from horizontal. The external auditory canals were alternately irrigated with warm air (50 °C) for 60 s, and then, after a recovery period, cool air (24 °C) for 60 s using the air caloric stimulator (CHARTR NCA 200, LCS Medical, Schaumburg, IL, USA). The maximal slow phase eye velocity (MSPV) of nystagmus was calculated following each irrigation. Jongkees’s formula was used to determine the semicircular canal paresis (CP) using the MSPV (with a 25 % difference in the CP being considered significant) [10]. The bilateral hypofunction (MSPV of nystagmus for cold and warm caloric stimulus: <10°/s) was defined as 100 % in CP.
The orthostatic Schellong test
The orthostatic Schellong test was performed in the mid-morning and the blood pressure (BP) and heart rate (HR) were automatically assessed with Automated Blood Pressure Monitor (Colin Corporation) with subjects in the supine position for 10 min. After that, the patients were asked to get up from the bed and stand up naturally without support or any standing device, such as forearm crutches or leg braces. All patients stood up within 20 s, and their systolic blood pressure (SBP), diastolic blood pressure (DBP), and HR were measured at approximately 1 min after actively changing from the supine position to the upright position. Following that, they were asked to maintain an upright posture quietly for 3 min and their SBP, DBP, and HR were monitored at 1-min intervals.
The changes in the SBP, DBP, and HR after standing up in comparison to the average data for the 10 min in the supine position were calculated at 1, 2, and 3 min after standing up. We adopted the criteria for OH based on the American Autonomic Society (AAS), which define the OH as an SBP decrease of at least 20 mm Hg or a DBP decrease of at least 10 mm Hg within 3 min of standing up [11].
Dizziness handicap inventory questionnaire
The dizziness handicap inventory includes 25 questions designed to assess a patient’s physical (seven questions), emotional (nine questions), and functional (nine questions) limitations. Each question provides a choice of three replies: “yes” (4 points), “sometimes” (2 points), and “no” (0 points). A maximum score of 100 points indicates the greatest possible disturbance to the patient, and the minimum score of 0 points indicates a lack of any handicap [12]. The dizziness handicap inventory assesses the precipitating physical factors associated with dizziness/unsteadiness and the functional/emotional consequences of symptoms as measures of disability in patients with dizziness and unsteadiness. The patients were asked to answer each question, as it pertains to dizziness or disequilibrium problems during the last month. The score on the DHI has been thought to reflect the impact on quality-of-life in patients with dizziness [13].
Statistical analysis
Mann–Whitney U-test was used to compare the parameters of the above examinations between groups due to unequal variances in the data among groups evaluated in this study. The level of significance of the two-tailed p < 0.05 was adopted throughout the study. The data in this text and table represent means (95 % confidence intervals).
Results
The OH was diagnosed in 16.5 % of all patients in this study and the positive rate of the OH in patients aged ≥65 years (31.3 %) was much higher than that in patients aged <50 years old (12.0 %) and patients aged 50–64 years (11.0 %). There was no significant difference in mean age between patients with OH and without OH in each group (p > 0.05, Table 1). The average SBP and average DBP for supine position in the patients aged ≥65 years with OH were significantly higher than those in the patients aged ≥65 years without OH (p < 0.01, Table 1). The average SBP and average DBP at 1 min after standing in the patients aged ≥65 years with OH were significantly lower than those in the patients aged ≥65 years without OH (p < 0.01, Table 1). The average DBP at 1 min after standing in the patients aged 50–64 years with OH was significantly lower than that in the patients aged 50–64 years without OH (p < 0.01, Table 1).
In this study, the peripheral causes of dizziness were the most common in all groups and they included benign paroxysmal positional vertigo (BPPV), vestibular neuritis, labyrinthitis, and Meniere’s disease (Table 2). The medical causes of dizziness (hypotension, low blood sugar, and anemia) were found in 30.6 % of the patients aged ≥65 years with OH, and most of them were attributed to medications for hypertension, prostatic hypertrophy, or insomnia. Depression, hyperventilation, panic disorder, and phobic postural vertigo were classified into the category of psychogenic dizziness. Central causes of dizziness were migraine, brain tumor, meningitis, and vertebral artery insufficiency. Post-traumatic vertigo, non-specific, or unlocalized dizziness was classified into others (Table 2).
The highest prevalence of the dizziness in all groups was peripheral causes, which was followed by the central and medical causes of dizziness. The disease distribution may be due to referral bias, because the population in this study was the patients sent to the otolaryngology department. Dizziness in patients aged more than 65 years was less likely to be due to the psychogenic cause regardless of the presence or absence of the OH. In patients with the OH, the medical causes of dizziness in patients aged more than 65 years were much common in comparison with other groups (Table 2). Most of dizzy patients in this study were managed with symptomatic therapy, and patients with BPPV were treated with the Epley maneuver or repositioning maneuver.
The ratios of patients with the treatment of antihypertensive drugs in patients aged more than 50 years with OH and patients aged more than 65 years without OH were the highest, more than 35 % (Table 2). They were treated with different antihypertensive regimens which were comprehensive (e.g., angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, beta blockers, and calcium channel blockers). The relative higher prevalent comorbidity in the dizzy patients aged more than 50 years was diabetes, followed by hyperlipidemia and hyperuricemia.
The CP% of patients with OH were not significantly different from those of patients without OH in each group (p > 0.05, Table 3). There was no significant difference in the score on the DHI among groups (p > 0.05, Table 3).
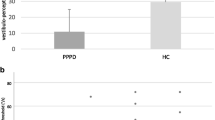
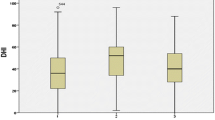
No age-related difference in the variability of the SVV was found in patients without OH (p > 0.05). The patients aged ≥65 years with OH showed the larger variability of the SVV than the patients aged <50 years with OH (p < 0.05, Fig. 1); however, no significant difference in the variability of the SVV was found between the patients aged ≥65 years with OH and patients aged 50–64 years with OH (p > 0.05, Fig. 1). There was no age-related difference in the average deviation of the SVV as well as the variability of the SVV (p > 0.05, Fig. 2).
The patients aged ≥65 years with OH showed a significantly larger variation of the SVV (mean 1.36, 95 % CI 1.14–1.57 degree) than the patients aged ≥65 years without OH (mean: 1.10, 95 % CI 0.96–1.24 degree, p < 0.05, Table 3, Fig. 1). No significant difference in the variability of the SVV was found between patients aged 50–64 years with OH (mean: 1.26, 95 % CI 0.86–1.65 degree, p > 0.05, Table 3, Fig. 1) and the patients aged 50–64 years without OH (mean: 0.91, 95 % CI 0.84–0.99 degree, p > 0.05, Table 3, Fig. 1). In patients aged <50 years, no significant difference in the variability of the SVV was found regardless of the presence or absence of the OH (p > 0.05, Table 3; Fig. 1).
There was no significant difference in the average deviation of the SVV among each group (p > 0.05, Table 3; Fig. 2). No significant difference in the average deviation of the SVV was found regardless of the presence or absence of the OH (p > 0.05, Table 3; Fig. 2).
Discussion
The OH occurs in about 20 % of the elderly and the morbidity of the OH increases with aging [14]. The elderly with dizziness are prone to move more slowly to avoid transient positional vertigo, and they are in physical deconditioning. It may aggravate the recovery of the graviceptive responses to the changes of gravitational acceleration, resulting in being predisposed to develop the OH. Our study showed that the ratio of the OH in dizzy patients aged ≥65 years was 31 %, which was much higher than that in the healthy elderly in a previous study [15]. If the orthostatic Schellong test is normal in patients with orthostatic symptoms, further examination by head-up tilt (HUT) test may be required, because the sensitivity of the orthostatic Schellong test is lower to detect postural tachycardia syndrome (POTS) and neutrally mediated syncope (NCS) rather than the HUT test [16, 17]. The POTS and NCS are more frequent in young people than the elderly [18, 19]. In addition, the ideal orthostatic test should be similar to real-life situations; however, the HUT test is far from a representation of the real-life situation. Therefore, we applied the orthostatic Schellong test as a screening test for the diagnosis of the OH in this study.
The larger variation of the SVV in the patients aged ≥65 years with OH in this study never seems to be induced by only the distress due to dizziness, because there was no significant difference in the CP%, the average deviation of the SVV, and the DHI score among all groups. The DHI, which reflects the self-perceived handicapping effects imposed by dizziness, has become crucial to diagnose the severity of handicap in the elderly, because elderly patients >65 years have balance affections due to dizziness. However, the previous study reported that the DHI score in the elderly with dizziness showed lower levels of self-perceived handicap [20]. Although the DHI is the most popular index of self-perceived handicap due to dizziness in clinical practice, the frequency of dizziness attacks is not always correlated with the perceived severity of the handicap. Patients with fewer dizziness attacks would report that they were severely handicapped and those that had many attacks of dizziness did not necessarily report being severely handicapped [13]. Therefore, the larger variability of the SVV in the elderly patients with OH may be associated with the subclinical impairment of the subjective perception of the verticality independent of the peripheral function and the severity due to dizziness.
Most of the patients who met the criteria for OH showed asymptomatic OH and non-pharmacologic treatment were offered to patients with OH initially. They were instructed to drink enough fluids, such as water, drink little to no alcohol, avoid walking during hot weather, elevate the head of your bed, and stand up slowly. The exercise programs to strengthen your leg muscles were recommended. The change of medications for hypertension and prostatic hypertrophy was required in 5 of 11 patients with medical dizziness among patients aged ≥65 years with OH. However, no patients aged ≥65 years were treated with additional pharmacological management for the OH.
The otolith organs related with the SVV are vulnerable to degradation due to aging, and the vestibular-cardiovascular response may be diminished with age [21, 22]. In this study, the elderly patients with OH showed normal average deviation, but the abnormal variability of the SVV. The SVV depends primarily on proprioceptive and vestibular cues, and the average deviation is usually equated with the tonic afferent input from otolith organs and central graviceptive pathways [4]. The large variability of the SVV indicates abnormal subjective perception of verticality independent of the peripheral vestibular function [5]. Our results may indicate an association between the impairment of central graviceptive pathways and the development of the OH in the elderly.
The postural cerebral hypoperfusion in frontal and parietal cortices has been found in patients with OH [23], which is conversely implicated in cerebral hypoperfusion among the elderly [24]. The cerebral hypoperfusion also occurs with age, especially in the periventricular white matter region, basal ganglia, hippocampus, and the regions of the brain with more than one source of blood supply [25]. The OH possibly contributes to significant declines in sustained attention, visual memory, and visual perception [26]. These brain regions overlap regions in the inferior parietal cortex and parietoinsular cortex, in which the vestibular, sensory, and visual inputs for the construction of the gravitational referential are integrated [7, 27]. Acute cerebral hemispheric stroke with lesions involved in visuospatial disturbance exacerbated both the deviation and the variability of the SVV [5]. Another study demonstrated that right hemispheric lesion patients, in particular, exhibit larger variability in the SVV than age-matched healthy subjects and patients with left hemispheric lesions, not a deviation of SVV [9]. Our previous study found a significant correlation between the variability of the SVV and the white matter regions on the MRI in dizzy elderly patients [28]. The greater variability of SVV in the elderly with OH in this study may, therefore, be induced by a disturbance at the level of polymodal sensory integration, resulting in inducing subjective dizzy symptoms.
The vertical perception may be dissociated from tilt perception identified by the deviation of the SVV [29]. The tilt perception may be compensated by other regions associated with the vestibular network. This phenomenon is caused by a probable dependence on non-vestibular information, such as proprioception, which may facilitate the compensation of static vestibular deficits. One study reported that the OH possibly contributes to significant declines in sustained attention, visual memory, and visual perception [25]. Therefore, the development of the OH may aggravate the sense of the verticality, independent of the tilt perception. The orthostatic test has not been routinely performed in clinical practice in the elderly patients suffering from dizziness. Furthermore, the OH diagnosed in the elderly may be asymptomatic OH, because the OH was gradually developed with age. Our results suggest that the OH in the elderly, even if the OH is asymptomatic, may be related to the impairment of the subjective perception of the verticality, and the subjective dizziness in the elderly may be consequently developed with the OH. It may indicate an efficiency of the orthostatic test, because OH is one of the main causes of chronic intolerance and falls, which lead to bone fractures and head injuries in the elderly [30].
This potential dysregulated blood pressure mechanism may be associated with latent neurobehavioral dysfunction as well as a silent cerebrovascular disease [31]. Subjects with asymptomatic OH showed poorer scoring on neurobehavioral function tests and more advanced leukoaraiosis than subjects without OH in the community-dwelling elderly population [32]. This result may support our result that less accuracy was found in vertical perception among elderly patients with OH than elderly patients without OH. However, the association between the variability of the SVV and the subjective symptoms in the elderly with the OH remains unclear. Additional research on the relating the OH to the impaired vertical perception in the elderly provides valuable information for treatment of elderly patients with dizziness and disequilibrium.
Conclusions
The pathogenic mechanism of dizziness and unsteadiness in the elderly is often controversial. Especially, many of the elderly suffering from dizziness have OH, of which the morbidity increases with age. In this study, the elderly with OH showed the larger variability of the SVV which indicates the impaired perception of the verticality. Although further study needs to evaluate the mechanism, the result may provide efficient information for treatment of dizzy elderly patients.
Abbreviations
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- OH:
-
Orthostatic hypotension
- SVV:
-
Subjective visual vertical
References
Rutan GH, Hermanson B, Bild DE et al (1992) Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 19:508–519
Wu JS, Yang YC, Lu FH et al (2008) Population-based study on the prevalence and correlates of orthostatic hypotension/hypertension and orthostatic dizziness. Hypertens Res 31:897–904. doi:10.1291/hypres.31.897
Gresty MA, Bronstein AM, Brandt T et al (1992) Neurology of otolith function. Peripheral and central disorders. Brain 115(Pt 3):647–673
Brandt T, Dieterich M (1994) Vestibular syndromes in the roll plane: topographic diagnosis from brainstem to cortex. Ann Neurol 36:337–347. doi:10.1002/ana.410360304
Yelnik AP, Lebreton FO, Bonan IV et al (2002) Perception of verticality after recent cerebral hemispheric stroke. Stroke 33:2247–2253
Dieterich M, Brandt T (1993) Ocular torsion and tilt of subjective visual vertical are sensitive brainstem signs. Ann Neurol 33:292–299. doi:10.1002/ana.410330311
Brandt T, Dieterich M, Danek A (1994) Vestibular cortex lesions affect the perception of verticality. Ann Neurol 35:403–412. doi:10.1002/ana.410350406
Barbieri G, Gissot AS, Perennou D (2010) Ageing of the postural vertical. Age 32:51–60. doi:10.1007/s11357-009-9112-5
Asai M, Aoki M, Hayashi H et al (2009) Subclinical deviation of the subjective visual vertical in patients affected by a primary headache. Acta Otolaryngol 129:30–35. doi:10.1080/00016480802032785
Lee IS, Park HJ, Shin JE et al (2009) Results of air caloric and other vestibular tests in patients with chronic otitis media. Clin Exp Otorhinolaryngol 2:145–150. doi:10.3342/ceo.2009.2.3.145
Freeman R, Wieling W, Axelrod FB et al (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci 161:46–48. doi:10.1016/j.autneu.2011.02.004
Newman CW, Weinstein BE, Jacobson GP et al (1990) The Hearing Handicap Inventory for Adults: psychometric adequacy and audiometric correlates. Ear Hear 11:430–433
Jacobson GP, Newman CW (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116:424–427
Low P (1997) The effect of aging on the autonomic nervous system. In: Low P (ed) Clinical autonomic disorders, 2nd edn. Lippincott-Raven Publishers, Philadelphia, pp 161–175
Raiha I, Luutonen S, Piha J et al (1995) Prevalence, predisposing factors, and prognostic importance of postural hypotension. Arch Intern Med 155:930–935
Winker R, Prager W, Haider A et al (2005) Schellong test in orthostatic dysregulation: a comparison with tilt-table testing. Wien Klin Wochenschr 117:36–41
Horrocks PM, FitzGerald MG, Wright AD et al (1987) The time course and diurnal variation of postural hypotension in diabetic autonomic neuropathy. Diabet Med 4:307–310
Singer W, Sletten DM, Opfer-Gehrking TL et al (2012) Postural tachycardia in children and adolescents: What is abnormal? J Pediatr 160:222–226. doi:10.1016/j.jpeds.2011.08.054
Low PA, Opfer-Gehrking TL, Textor SC et al (1995) Postural tachycardia syndrome (POTS). Neurology 45:S19–S25
Hansson EE, Mansson NO, Hakansson A (2005) Balance performance and self-perceived handicap among dizzy patients in primary health care. Scand J Prim Health Care 23:215–220. doi:10.1080/02813430500287299
Ray CA, Monahan KD (2002) Aging attenuates the vestibulosympathetic reflex in humans. Circulation 105:956–961
Tanaka K, Abe C, Awazu C et al (2009) Vestibular system plays a significant role in arterial pressure control during head-up tilt in young subjects. Auton Neurosci 148:90–96. doi:10.1016/j.autneu.2009.03.007
Hayashida K, Nishiooeda Y, Hirose Y et al (1996) Maladaptation of vascular response in frontal area of patients with orthostatic hypotension. J Nucl Med 37:1–4
Roman GC (2004) Brain hypoperfusion: a critical factor in vascular dementia. Neurol Res 26:454–458. doi:10.1179/016164104225017686
Allcock LM, Kenny RA, Mosimann UP et al (2006) Orthostatic hypotension in Parkinson’s disease: association with cognitive decline? Int J Geriatr Psychiatry 21:778–783. doi:10.1002/gps.1562
Aoki M, Tokita T, Kuze B et al (2014) A characteristic pattern in the postural sway of unilateral vestibular impaired patients. Gait Posture 40:435–440. doi:10.1016/j.gaitpost.2014.05.013
Barra J, Marquer A, Joassin R et al (2010) Humans use internal models to construct and update a sense of verticality. Brain 133:3552–3563. doi:10.1093/brain/awq311
Aoki M, Tanaka K, Wakaoka T et al (2013) The association between impaired perception of verticality and cerebral white matter lesions in the elderly patients with orthostatic hypotension. J Vestib Res 23:85–93. doi:10.3233/VES-130479
Perennou DA, Leblond C, Amblard B et al (2000) The polymodal sensory cortex is crucial for controlling lateral postural stability: evidence from stroke patients. Brain Res Bull 53:359–365
Shibao C, Grijalva CG, Raj SR et al (2007) Orthostatic hypotension-related hospitalizations in the United States. Am J Med 120:975–980. doi:10.1016/j.amjmed.2007.05.009
Eguchi K, Kario K, Hoshide S et al (2004) Greater change of orthostatic blood pressure is related to silent cerebral infarct and cardiac overload in hypertensive subjects. Hypertens Res 27:235–241
Passant U, Warkentin S, Gustafson L (1997) Orthostatic hypotension and low blood pressure in organic dementia: a study of prevalence and related clinical characteristics. Int J Geriatr Psychiatry 12:395–403
Acknowledgments
This research was supported by the Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science, a Grant from the intractable diseases fund (vestibular disorders) of the Ministry of Health and Welfare, Japan, and a Grant-in-Aid from the Gifu University School of Medicine for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments. No studies with animals were performed.
Informed consent
Informed consent was obtained from all participants in this study.
Rights and permissions
About this article
Cite this article
Aoki, M. The impaired subjective perception of verticality independent of peripheral vestibular function in dizzy elderly with orthostatic hypotension. Aging Clin Exp Res 29, 647–653 (2017). https://doi.org/10.1007/s40520-016-0624-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0624-4