Abstract
Background
Dizziness is one of the most prevalent symptoms in old age and tends to increase with age.
Aims
To report physical functioning, health-related aspects and gender differences in elderly persons with and without dizziness in a population-based sample of 75-year-olds.
Methods
A cross-sectional sample of 75-year-olds from Gothenburg, Sweden (n = 675, 398 women and 277 men) was examined by means of questionnaires and functional tests. The questions concerned dizziness/imbalance, physical activity level, walking habits, falls efficacy, number of falls, subjective health or general fatigue and medication. The tests included were self-selected and maximum gait speed, stair climbing capacity, one leg stance and grip strength.
Results
More women than men reported dizziness/imbalance (40 vs 30 %, p < 0.001). Persons with dizziness, compared to those without dizziness, less often regularly exercised at a moderate intensity level (summer: 62 vs 74 %, p < 0.001; winter: 41 vs 51 %, p < 0.001), less often took a daily walk (p < 0.05), had lower scores on the FES(S) (p < 0.001), more often reported general fatigue (p < 0.001), more often had fallen in the previous year (40 vs 23 %, p < 0.001) and had a higher intake of medical drugs (4.6 vs 3.3, p < 0.001). They also performed worse regarding gait speed, stair climbing and one leg stance (p < 0.001), but there was no difference in grip strength.
Conclusion
Older persons with dizziness are less physically active, have worse lower extremity function, are more often fallers and report lower self-rated health than persons without dizziness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dizziness is a subjective sensation of disorientation or involuntary motion that can be caused by several factors [1]. Maintaining balance is a complex ability that is dependent on the integrity of visual, vestibular, and somatosensory information. Such signals are continuously processed in the central nervous system [2, 3]. Dizziness is among the most prevalent symptoms in older persons [1]. Dizziness is also a strong predictor of falls and recurrent falls [4]. Older persons who suffer from dizziness exhibit a decrease in daily activities and a reduced quality of life [5, 6]. Women have been reported to have a higher lifetime prevalence of moderate or severe dizziness or vertigo than men (36 vs 22 %) [7]. The prevalence of dizziness in a Swedish population of 70–75-year-olds was 40 % for women and 30 % for men [8]. Dizziness is a problem that may increase with age [6]. Severe vestibular vertigo leading to the interruption of daily activities has been reported in 8.4 % of women and 3.4 % of men [7]. Grimby et al. [5] showed that dizziness was significantly correlated with nervousness and depression in men. Gazzola et al. [9], who studied elderly people with chronic vestibular dysfunction, found that females displayed higher levels of depressive symptoms than males.
There is evidence that balance training can decrease elderly persons’ dizziness and improve their balance [10, 11]. It is important to use good clinical instruments to detect the problem of poor balance, which can be one cause of dizziness. Dizziness and poor balance in elderly persons has been associated not only with low physical activity levels but also with falls [6] and reduced grip strength, which is an indicator of overall muscle strength [12].
The Falls Efficacy Scale (FES) measures a person’s degree of self-confidence in performing common daily activities without falling. The instrument has been reported to be associated with functional ability, and individuals with low levels of self-efficacy tend to reduce their physical and social activities [13].
In a previous population-based study of 75-year-olds, 36 % experienced dizziness, especially unsteadiness, when walking outdoors. Furthermore, 11 % had undiagnosed but treatable benign paroxysmal positional vertigo (BPPV). Persons who tested positive for BPPV had worse results on tests of static balance and walking speed compared to those without BPPV [14]. The present study further investigates health-related aspects among elderly persons with and without dizziness.
The purpose of this study was to report physical functioning, health-related aspects and gender differences among elderly persons, with and without dizziness, in a population-based sample of 75-year-olds.
Methods
Participants
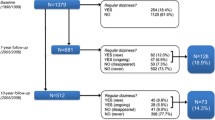
The study comprised the fifth cohort of the longitudinal, cross-sectional, gerontological and geriatric population studies in Gothenburg, Sweden (H70) [15]. The persons were selected from an urban population aged 75 years through systematic sampling based on date of birth, and 1332 persons were invited to participate. Six hundred and seventy-five persons (398 women and 277 men) agreed to participate; of these persons, 571 (337 women and 234 men) took part in the functional tests. Six hundred and fifty-seven persons did not participate in the study; the reasons for not participating in the functional tests were, e.g., arthritis, back pain or joint problems in the lower extremities.
Data based on interviews and tests conducted by physiotherapists
Dizziness
The question concerning dizziness was as follows: “Do you have any problems with dizziness or impaired balance?” The response alternatives were yes/no [14].
Physical activity level
Regarding walking habits, the questions were as follows: “Do you generally take a daily walk?” (response alternatives: yes or no.) “How long does your walk generally last?” (five response alternatives: 0–15, 15–30, 30–60 min, 1–2 h, >2 h) [16].
Participants rated their physical activity level, including household activities, for the summer and winter seasons separately using a six-grade scale ranging from hardly any physical activity to hard or very hard exercise regularly and several times/week where the physical exertion is great [16].
Falls efficacy
Falls efficacy was estimated according to the Falls Efficacy Scale Swedish version (FES)(S), which includes 13 items [17]. The respondents rated their confidence on a 0–10-point scale (0 = not confident at all and 10 = completely confident). The scale includes three parts: six items measure personal activities of daily living (ADLs), walking up and walking down stairs and six items measure instrumental ADLs. The maximum score is 130 points. The reliability of the Swedish version of the scale was found to be acceptable [17]. Furthermore, falls efficacy has recently been found to be a reliable and valid tool for measuring persons with dizziness and imbalance [18].
Additional questions
The following questions were asked: “Have you fallen during the last year (yes/no)?”, “Do you generally feel healthy (yes/no)?”, and “Do you generally feel tired (yes/no)?” [19].
Additionally, medication (number of drugs) was registered.
Functional performance
Chair stand was used to test the ability to rise from a chair 45 cm high without support.
The participants performed the test as quickly as possible five times in a row. The total time (s) was used as the outcome [20].
Stair climbing was utilized to test the ability to climb onto boxes of varying heights (10, 20, 30, 40 and 50 cm) without the use of a handrail [21], and the ability to climb >40 cm was used for the analyses.
Grip strength was tested with a JAMAR Dynamometer, Sammons Preston 503IJI. The test was repeated three times for each hand, and the highest value for the best hand was used for the analyses. This method has been shown to have high intra- and inter-test reliability [22] and validity [23].
Walking speed was tested for 20 m at both self-selected and maximum speed, and there was no acceleration or deceleration phase [21]. Walking speed is a highly valid and reliable test [24]. In addition, walking 10 m at a self-selected speed while repeatedly turning the head to the left and right was tested. In addition, the number of steps taken was registered [14].
Balance function was tested using the sharpened Romberg test with eyes open and closed and without shoes. The tests were performed with the heel of the dominant foot directly in front of the toe of the non-dominant foot. The tests were terminated when the person lost balance by moving one foot or both feet. The best result of three trials was recorded, and the maximum time was 30 s [14]. Kammerlind et al. [25] showed that the static balance test is a reliable test that can be administered to persons with dizziness.
One leg stance with eyes open was performed while standing on one leg without shoes for a maximum of 30 s. Participants’ hip joint of their non-weight-bearing leg was in a neutral position, knee was flexed to approximately 90°, and hands were behind their back while they looked straight ahead. The test was interrupted if the person moved from the standardized position. Three trials for each leg were allowed, and the best result was used for the analyses [26].
Statistical analysis
The software used for the statistical analysis was a statistics program package developed at the Department of Geriatrics at Gothenburg University (GIDSS for Windows).
Tests of the differences between two groups in variables measured on a linear scale were done with t test for each sex and with linear regression with sex as a covariate for the total group. Tests of the differences in dichotomized variables were calculated by logistic regression with sex as a covariate for the total group. Significance is reported for two-tailed tests, and the significance level used is 5 %.
Ethics
The study was approved by the Research Ethics Committee of Gothenburg University (Dnr S 227-00).
Results
More women than men reported dizziness/impaired balance (40 versus 30 %, p < 0.01).
Persons with dizziness were less likely to take daily walks than persons without dizziness (p < 0.05). However, fewer women than men with dizziness walked >30 min (p < 0.05) (Table 1). Regarding physical activity level, persons who had a low level of physical activity (1–3) suffered from dizziness to a greater extent than persons who were more physically active (levels 4–5) (p > 0.001). For the summer season, 62 % of the persons with dizziness reported level-4 physical activity compared to 74 % of those without dizziness (p < 0.001) (Fig. 1), and for the winter season, 40 % of persons with dizziness compared to 51 % of those without dizziness reported level-4 activity (p < 0.001) (Fig. 2). The proportion of men with dizziness engaging in level-5 physical activity was small compared to men without dizziness for both the summer and winter seasons (p < 0.05).
Regarding falls efficacy, the majority had maximum scores for all 13 variables, which indicates high confidence in performing common daily activities without falling. However, the proportion with maximum scores was significantly lower among persons with dizziness than those without dizziness. The lowest falls efficacy confidence among those with dizziness was found for “Get up and down stairs” (75 versus 92 %) and “answer the telephone” (79 versus 95 %). This difference was significantly greater among women (Table 1).
Persons with dizziness had, compared to those without dizziness, more often fallen during the past year (40 versus 23 %, p < 0.001). Those with dizziness also took more medications [mean number of drugs among those without dizziness = 3.3, compared to those with dizziness = 4.6 (p < 0.001)], and 30.5 % of persons with dizziness reported fatigue compared to 11.5 % of those without dizziness (p > 0.001). Of the persons with dizziness, 20.1 % did not feel healthy, compared to 8.2 % of those without dizziness (p > 0.001) (Table 2).
For the chair stand test, persons with dizziness displayed worse results than persons without dizziness (p < 0.001). The same result was found for stair climbing capacity (48.1 versus 76.3 %, p < 0.001). Regarding grip strength, there was no difference between the two groups (Table 3).
Persons with dizziness had slower self-selected and maximum walking speeds compared to those without dizziness (p < 0.001). Regarding walking while turning their head, persons with dizziness performed this activity slower (p < 0.05). They also performed significantly worse on the standing on one leg with eyes open test and the Sharpened Romberg Test with eyes close or open compared to those without dizziness (p < 0.001). Both women and men with dizziness showed worse results for both the walking and static balance tests compared to those without dizziness (p < 0.001) (Table 3).
Discussion
The study investigates the health-related aspects and gender differences among older persons with and without dizziness. Compared to those without dizziness, persons with dizziness less regularly exercised at a moderate intensity level. Those with dizziness had lower scores on the FES(S), more often reported general fatigue, more often had fallen in the previous year and took a greater number of drugs. The physical functioning of persons with dizziness was significantly worse than that of those without dizziness, but there was no difference in grip strength. The old persons with dizziness had significantly more problems with strength in the lower extremities. There were gender differences; women with dizziness walked less than men but had significantly greater scores in terms of activity scale, FES, and feeling healthy. However, there was no gender difference in feeling fatigue or in physical functional tests.
The higher prevalence of dizziness among older persons has been reported by others [8, 14]. Dizziness is sometimes viewed as a geriatric syndrome, i.e., a condition caused by the decline of several bodily functions in old age [3], and sometimes overlooked because of its complex and multifactorial etiology. However, a correct diagnosis and treatment may reduce the loss of health in this population. The reason why more women felt dizziness compared to men is unclear. Other authors have suggested that the higher prevalence in women may be attributed to factors such as hormonal cycle variety, higher prevalence of migraine or more medical care seeking behaviours [27]. There was a high prevalence of persons with dizziness in this study; however, the actual prevalence may be even higher because we may have missed the sickest persons, as they may find it difficult to participate in research.
However, the physical activity levels of persons with dizziness were lower (level 3) than of persons without dizziness (level 4). This trend was stronger in women than in men and in winter compared to summer. In winter, the risk of falling due to icy roads can be one cause of lower activity levels. Another factor can be fewer hours of daylight in winter. Ekwall et al. [6] reported that light exercise seems to be beneficial in terms of both improving quality of life and decreasing the risk of falling. These authors used an age-stratified, randomized (different between those with and without dizziness) sample of persons aged 75 or older (n = 4360).
Due to the finding of reduced physical activity during the winter, it is important to encourage any type of reasonable indoor physical activity. The current study showed that those with dizziness had significantly lower scores on the FES compare to those without dizziness. This result is line with the findings of Olsson Möller et al. [28]. In addition, a study by Moraes et al. [29] showed that a higher proportion of elderly persons <80 years old with dizziness feared falling.
Our study reported that the significantly lowest scores on the FES for persons with dizziness were found for “Get up and down stairs” and “Answer the telephone”. These activities involve movements and stimulate the vestibular system. Recently, a report found that signs of vestibular asymmetry among elderly persons (median age = 80 years) could predict falls [30]. A study by Morgon et al. [18] found that FES-I is a reliable and valid tool for measuring an individual’s concern about falling in a sample of persons with dizziness.
Those with dizziness had more often fallen in the past year than those without dizziness, and there was no difference between the genders. This result is in line with several studies [6, 29]. Dizziness is an important risk factor for falls, and studies have shown that the prevalence of falls increases with age [3]. Persons with dizziness who fall might suffer from fear of falling, which might initiate a vicious cycle of avoidance of activities, reduced mobility, functional decline and loss of self-confidence, as discussed by Zijlstra et al. [31].
However, a feeling of general fatigue was more common among those with dizziness compared to those without dizziness (30.5 versus 11.7 %). Fatigue was common to both women and men who experienced dizziness. Olsson, Moller et al. [28] found that fatigue showed a high prevalence rate (61 %) in persons with dizziness under 80 years of age (n = 531) after a 6-year follow-up. They also found that a history of falling or dizziness was a strong predictor of dependency in instrumental ADLs [28].
Another study by de Moraes et al. [29] examined community-dwelling individuals aged 65 years and older (n = 391) and found that 45 % reported dizziness and that 41.5 % of persons with dizziness complained about feeling fatigue. Bronstein et al. [32] discussed fatigue as a secondary problem among patients with vestibular pathology together with muscular pain, increased muscle tension and chronic anxiety. For self-report, fatigue is a broad term that might included both physical and physiological aspects.
In the current study, persons with dizziness took significantly more medication (p < 0.001), and there was no difference between the genders. Grassmann and Rupprecht also highlighted that persons with dizziness take more medication than persons without dizziness [3]. A study by Olsson Möller et al. [28] reported that among persons under 80 years, the consumption of neuroleptic medication was a predictor of falls. In a large Swedish epidemiology study specific medication and diseases were associated with dizziness and faintness [33].
Regarding the current chair standing and stair climbing tests, the results were worse for those with dizziness, but those with and those without dizziness showed no difference in grip strength. Olsson Möller and colleagues found reduced grip strength in persons with dizziness, younger than 80 years of age, but in their study only the right hand was measured [28]. It has recently been reported by Maarsingh et al. [34], who found that impaired function of the lower extremities is an important predictor of regular dizziness in older adults at 7- and 10-year follow–ups.
Impaired function of the lower extremities can affect the dynamic balance tests, and those with dizziness displayed poorer performance on these tests. Poor dynamic balance is a disabling factor in terms of daily life activities. A recent study conducted by Rossi-Izquierdo et al. [35] showed that nearly half of the falls that elderly persons experience occur when they are walking. Grassman et al. [3] found that the majority of their elderly participants (>65-year-olds) with dizziness described a feeling of losing their balance (64.5 %), which was associated with gait disturbance and the risk of falls.
In a previous study, we found that the strongest dizziness experience was unsteadiness while standing and walking [14]. The experience of feeling unsteady while standing and walking may lead to greater tension in the muscles because of the fear of falling. Greater tension in the muscles also costs a substantial amount of energy, and this could be one cause of increased fatigue, as previously discussed.
Our study showed that grip strength was reduced in persons with dizziness. Why is there a difference between grip strength and functional tests of the lower extremities? Together with physical functional tests of the lower extremities, grip strength is a common measure of general health and function in older persons [26]. Grip strength can depend on several factors.
One factor is clinical experience; persons with dizziness, especially old persons, fear falling or losing their balance. Thus, older persons use their hands more to avoid falling. Furthermore, persons with dizziness may sit more and, thus, use their hands more than their lower extremities. Ekwall et al. [6] study showed that elderly persons with dizziness who perform light exercise reduced their risk of falling and depression.
Another study examined persons over 70 years with symptoms of dizziness and no documented vestibular deficits. In that study, the addition of standard balance rehabilitation with exercises related to vestibular-specific gaze stability and lower limb muscle strength resulted in a greater reduction of falls risk [36].
The current study is the first to report the physical activity level and physical functional fitness of persons with dizziness. The results have important clinical implications for the design of rehabilitation programs, which should focus on dynamic activities such as gait and lower limb strength.
Limitations
This study also has several limitations. First, drop-out was especially prominent among men, which might affect the study’s external validity and reduce the overall generalizability. Second, we likely met the healthiest persons, which can also reduce the generalizability of the findings.
Third, there was a discrepancy between those who only completed the questionnaire and those who underwent the clinical tests and also answered the questionnaire (675/571), potentially leading to the underestimation of the prevalence of dizziness. This difference was primarily due to immobility and tiredness. Another limitation may be the use of dizziness or imbalance as an umbrella term. However, this study had a cross-sectional design, making it difficult to assess the direction of casualty. The reason why questionnaires that have been tested for reliability and validity were not used was the cross-sectional nature of the original study, which does not allow the opportunity to change to new instruments. Fifth, it might be hard to retrospectively recall falls over a period of 1 year.
Conclusion
Persons with dizziness are less physically active, have worse lower extremity function, are more often fallers, and report lower self-rated health than persons without dizziness. These are important clinical implications when designing rehabilitation programs, which should have a clear focus on dynamic activities such as gait and strength training for the lower extremities. Considering the high costs of falls and dizziness for society and the individual suffering from these issues, it is necessary to focus on interventions that address falls and dizziness.
References
Baloh RW (1992) Dizziness in older people. J Am Geriatr Soc 40:713–721
Konrad HR, Girardi M, Helfert R (1999) Balance and aging. Laryngoscope 109:1454–1460
Gassmann KG, Rupprecht R (2009) Dizziness in an older community dwelling population: a multifactorial syndrome. J Nutr Health Aging 13:278–282
Gassmann KG, Rupprecht R, Freiberger E (2009) Predictors for occasional and recurrent falls in community-dwelling older people. Z Gerontol Geriatr 42:3–10
Grimby A, Rosenhall U (1995) Health-related quality of life and dizziness in old age. Gerontology 41:286–298
Ekwall A, Lindberg A, Magnusson M (2009) Dizzy—why not take a walk? Low level physical activity improves quality of life among elderly with dizziness. Gerontology 55:652–659
Neuhauser HK, von Brevern M, Radtke A et al (2005) Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology 65:898–904
Jonsson R, Sixt E, Landahl S et al (2004) Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res 14:47–52
Gazzola JM, Aratani MC, Dona F et al (2009) Factors relating to depressive symptoms among elderly people with chronic vestibular dysfunction. Arq Neuropsiquiatr 67:416–422
Kammerlind AS, Hakansson JK, Skogsberg MC (2001) Effects of balance training in elderly people with nonperipheral vertigo and unsteadiness. Clin Rehabil 15:463–470
Jung JY, Kim JS, Chung PS, Woo SH et al (2009) Effect of vestibular rehabilitation on dizziness in the elderly. Am J Otolaryngol 30:295–299
Rantanen T, Era P, Heikkinen E (1994) Maximal isometric strength and mobility among 75-year-old men and women. Age Ageing 23:132–137
Tinetti ME, Mendes de Leon CF, Doucette JT et al (1994) Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol 49:M140–M147
Kollén L, Frändin K, Möller M et al (2012) Benign paroxysmal positional vertigo is a common cause of dizziness and unsteadiness in a large population of 75-year-olds. Aging Clin Exp Res 24:317–323
Rinder L, Roupe S, Steen B et al (1975) Seventy-year-old people in Gothenburg. A population study in an industrialized Swedish city. Acta Med Scand 198:397–407
Frändin K, Grimby G, Mellström D et al (1991) Walking habits and health-related factors in a 70-year-old population. Gerontology 37:281–288
Hellstrom K, Lindmark B, Fugl-Meyer A (2002) The Falls-Efficacy Scale, Swedish version: does it reflect clinically meaningful changes after stroke? Disabil Rehabil 24:471–481
Morgan MT, Friscia LA, Whitney SL et al (2013) Reliability and validity of the Falls Efficacy Scale-International (FES-I) in individuals with dizziness and imbalance. Otol Neurotol 34:1104–1108
Mattiasson-Nilo I, Sonn U, Johannesson K et al (1990) Domestic activities and walking in the elderly: evaluation from a 30-hour heart rate recording. Aging (Milano) 2:191–198
Guralnik JM, Seeman TE, Tinetti ME et al (1994) Validation and use of performance measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano) 6:410–419
Frändin K, Mellström D, Svanborg A (1994) Assessment of physical activity, fitness and performance in 76-years olds. Scand J Med Sci Sports 4:41–46
Bellace JV, Healy D, Besser MP et al (2000) Validity of the Dexter Evaluation System’s Jamar dynamometer attachment for assessment of hand grip strength in a normal population. J Hand Ther 13:46–51
Peolsson A, Hedlund R, Oberg B (2001) Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med 33:36–41
Rydwik E, Bergland A, Forsen L et al (2011) Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: a systematic review. Physiother Theory Pract 28:238–256
Kammerlind A-S, Bergquist Larsson P, Ledin T et al (2005) Reliability of clincal balance tests and subjective ratings in dizziness and disequilibrium. Adv Physiother 7:96–107
Frändin K, Sonn U, Svantesson U et al (1995) Functional balance tests in 76-year-olds in relation to performance, activities of daily living and platform tests. Scand J Rehabil Med 27:231–241
Bittar RS, Oiticica J, Bottino MA et al (2013) Population epidemiological study on the prevalence of dizziness in the city of Sao Paulo. Braz J Otorhinolaryngol 79:688–698
Olsson Moller U, Midlov P, Kristensson J et al (2012) Prevalence and predictors of falls and dizziness in people younger and older than 80 years of age—a longitudinal cohort study. Arch Gerontol Geriatr 56:160–168
de Moraes SA, Soares WJ, Ferriolli E et al (2013) Prevalence and correlates of dizziness in community-dwelling older people: a cross sectional population based study. BMC Geriatr 13:4
Ekvall Hansson E, Magnusson M (2013) Vestibular asymmetry predicts falls among elderly patients with multi-sensory dizziness. BMC Geriatr 13:77
Zijlstra GA, van Haastregt JC, van Eijk JT et al (2007) Prevalence and correlates of fear of falling, and ssociated avoidance of activity in the general population of community-living older people. Age Ageing 36:304–309
Bronstein AM, Lempert T (2010) Management of the patient with chronic dizziness. Restor Neurol Neurosci 28:83–90
Tamber AL, Bruusgaard D (2009) Self-reported faintness or dizziness—comorbidity and use of medicines. An epidemiological study. Scand J Public Health 37:613–620
Maarsingh OR, Stam H, van de Ven PM et al (2014) Predictors of dizziness in older persons: a 10-year prospective cohort study in the community. BMC Geriatr 14:133
Rossi-Izquierdo M, Santos-Perez S, Del-Rio-Valeiras M et al (2015) Is there a relationship between objective and subjective assessment of balance in elderly patients with instability? Eur Arch Otorhinolaryngol 272:2201–2206
Hall CD, Heusel-Gillig L, Tusa RJ et al (2010) Efficacy of gaze stability exercises in older adults with dizziness. J Neurol Phys Ther 34:64–69
Acknowledgments
This study was supported by grants from the Research and Development Council for Southern Gothenburg and Bohuslän. We are very grateful to the persons who agreed to participate in this study. The authors also thank Valter Sundh for providing statistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts interest.
Statement of human and animal rights
All procedures performed in this study involving human participants were accordance with the ethical standards of the institutional and national research committee and with the 1964 declaration of Helsinki. Procedures performed in this study did not involve animals.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kollén, L., Hörder, H., Möller, C. et al. Physical functioning in older persons with dizziness: a population-based study. Aging Clin Exp Res 29, 197–205 (2017). https://doi.org/10.1007/s40520-016-0567-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0567-9