Abstract
Background
Nurses have the key roles to detect delirium in hospitalized older patients but under-recognition of delirium among nurses is prevalent. The objectives of this study were to identify the under-recognition rate of delirium by intensive care nurses (ICU) using Confusion Assessment Method for the ICU (CAM–ICU) and factors associated with under-recognition.
Methods
Participants were older patients aged ≥65 years who were admitted to the ICU of Srinagarind Medical School, Khon Kaen, Thailand from May 2013 to August 2014. Baseline characteristics were collected. Delirium was rated by a trained clinical researcher using the CAM–ICU. Demographic data were analyzed using descriptive statistics. Univariate and multiple logistic regressions were used to analyze the outcomes.
Results
Delirium occurred in 44 of 99 patients (44.4 %). Nurses could not identify delirium in 29.6 % of patients compared with researchers. Pre-existing dementia and depression were found in 47.7 % of patients. Pneumonia or other causes of respiratory failure were the most common causes of admission to ICU (47.7 %). Independent factors associated with under-recognition by nurses were identified—heart failure [adjusted odds ratio (OR), 77.8; 95 % confidence interval (CI) 2.5–2,543, p = 0.01] and pre-existing taking treatment with benzodiazepines (adjusted OR, 22.6; 95 % CI 1.8–85, p = 0.01).
Discussion
Under-recognition of delirium is a frequent issue. New independent factors associated with under-recognition were identified. Awareness of delirium in the patients with these factors is recommended.
Conclusions
This study supports the finding of high under-recognition rates of delirium among hospitalized older adults in ICU. Patients with heart failure and receiving benzodiazepines were identified as barriers of recognition of delirium.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Delirium is a clinical syndrome, characterized by an acute change in consciousness, attention, cognition and perception and tends to fluctuate during the course of the day [1]. Delirium represents a medical emergency with serious complications among hospitalized elderly. Its prevalence on hospital admission varies from 11 to 33 %. The incidence rate during hospitalization in a general ward is 3–56 %. The prevalence and incidence of delirium in Thai medical wards were 40.4 and 8.4 %, which was quite high comparable to other reports [2]. Delirium tends to increase in patients at an age of 65 or over, male subjects, patients with cognitive impairment, patients in the postoperative phase (especially post-hip fracture and vascular surgery, and those in intensive care in which the incidence ranges from 19 to 87 % [3, 4]. It is associated with increased morbidity and mortality including short and long-term outcomes such as a longer length of hospital stay, a higher rate of nursing home placement, persistent functional decline, and increased healthcare costs [1, 5–7].
Although delirium is prevalent and leads to serious adverse outcomes, it is usually under-recognized [8–10]. Early detection of this condition is crucial as implementing early intervention to the patients could lessen unfavorable consequences of delirium [11]. Nurses play an important role to primarily detect delirium as nurses spend more time at the bedsides than other healthcare providers [9, 12]. A change in consciousness level and other components of delirium could be, therefore, discovered initially by nurses. Existing reviews show that the under-recognition rates of delirium among nurses are high, ranging from 23 to 75 % [9, 10, 13]. There was poor agreement between nurses and researchers from one study (kappa 0.34) [8]. The sensitivity of detecting delirium by nurses was low while the specificity was high [9]. The independent factors associated with poor recognition were aging, in particular age >80 years, length of stay, pre-existing dementia, baseline Barthel index, hypoactive delirium, and vision impairment [8, 9]. Additionally, greater numbers of these risk factors were associated with an increased risk of under-recognition of delirium [9]. A lack of awareness for delirium diagnosis was high and the use of validated screening tools was low [14]. A survey study among healthcare professionals in Italy reported that 84.5 % of physicians defined delirium correctly, compared with 49.8 % of nurses, 52.9 % of physiotherapists, and 76.7 % of psychologists; a delirium screening tool was only used by about 15 % of all participants [15]. The Confusion Assessment Method (CAM), a validated tool of detecting delirium [1], was used 27 % of the time by these Italian nurses and the majority of them did not use the correct method of CAM to detect delirium [15].
Routinely, CAM is not used in general wards and ICU settings of Thailand but given that the medical school hospital is a tertiary care hospital, there are likely to be more complicated cases in addition to greater risks for developing delirium than expected in general clinical practices. The under-recognition rate of delirium in the ICU was not yet known for Thai patients. In addition, the magnitude of factors associated with under-recognition in this setting has not been identified. Therefore, the primary objective of this study was to identify the under-recognition rate of delirium by ICU nurses using the CAM–ICU and the secondary objective was to identify factors associated with under-recognition.
Methods
Study participants
This study was a sub-study of the “Prevalence, incidence and related factors of delirium among medically-ill older adults in the intensive care unit of Srinagarind Hospital”. The setting was the intensive care unit (ICU) of the Internal Medicine Department, Srinagarind Medical School, Khon Kaen University, Khon Kaen, Thailand. Potential participants were Thai patients who were 65 years or over admitted to the ICU of the Medicine Department from 1 May 2013 to 31 August 2014. The patients were excluded if they were previously admitted to this ward during the same hospitalization, patients and/or their families were not willing to participate in this study, coma (Richmond Agitation Sedation Scale: RASS score <−3) [16], severe aphasia or severe hearing impairment. Termination of study criteria was fulfilled when patients were no longer classified as delirious, discharged to other settings, or dead.
Measurement
Delirium was defined by the Confusion Assessment Method (CAM) criteria which are composed of acute onset and fluctuating causes of symptoms, inattention, and either an altered level of consciousness or disorganized thinking. It is a short, accurate and widely used tool to detect delirium. It has been validated in many countries including Thailand with a sensitivity of 94–100 %, specificity of 90–100 % and high inter-rater reliability [17, 18]. As the setting was the ICU, we adopted the CAM for the intensive care unit (CAM–ICU) [19]. The CAM–ICU was adapted from the CAM to use in mechanically ventilated patients. It shows a high sensitivity (93 %) and specificity (89 %) in diagnosing delirium [20]. The Thai version of CAM–ICU (Thai CAM–ICU) was performed as forward and backward translations under the “Copyright © 2002, E. Wesley Ely, MD, MPH and Vanderbilt University, all rights reserved” from which the training manual for the Thai CAM–ICU is currently available from the website www.icudelirium.org. It is easy to administer and takes less than 2 min to complete and requires minimal training [21]. The performance of the Thai CAM–ICU shows good validity and reliability with its sensitivity of 92.3 % and specificity of 94.7 % [22].
We assessed the severity of illness with the Acute Physiology and Chronic Health Evaluation II (APACHE II), and baseline function of the patients with the Barthel activities of daily living (ADL) index, referring to the period prior to hospital admission [23].
Procedures
Baseline patient data were collected after informed consent by trained clinical researchers, and completed within 48 h of admission to the ICU. They included demographic information and the CAM–ICU rating for delirium. Demographic information consisted of age, sex, educational level, underlying disease, admitting diagnosis, self-reported baseline basic activities of daily living (ADLs) using Barthel ADLs index), APACHE II scores, length of stay in hospital, and medication review. For detection of delirium, the trained clinical researchers administered the CAM–ICU every 24 h until the patients were out of delirium, discharged from ICU or dead. The CAM–ICU evaluations of ICU nurses who had experience in nursing care of at least 5 years, ratings of delirium were collected at the same intervals at the same time. To avoid potential bias, the results of rating delirium by ICU nurses and trained clinical researchers were blinded to each other.
Statistical analyses
Inter-rater reliability of the trained clinical researchers to detect delirium by CAM–ICU was analyzed using kappa statistics, until kappa >0.8. For the APACHE II scores, the researchers analyzed intraclass correlation coefficients (ICC) until ICC >0.8. Then, they could collect the data in the main study. Demographic data and rating of delirium by the trained clinical researchers and the ICU nurses were analyzed using descriptive statistics, presentations in percentage, mean and standard deviation. If the distribution of these data was not a normal distribution, then medians, and inter-quartile ranges were used instead. The effects of factors associated with under-recognition of delirium were evaluated using univariate and multiple logistic regressions. For univariate analysis, the Chi square test or Fisher’s exact test was used to examine all categorically associated factors and Student t tests were used to compare all continuous variables. Factors with a P < 0.20 were then entered into a stepwise multiple logistic regression model. P < 0.05 was considered to indicate statistically significant differences and adjusted odds ratios (OR) and their 95 % confidence intervals (CI) were reported to consider the strength of association. All the data analyses were carried out using STATA version10.0 (StataCorp, College Station, Texas).
Ethics approval was provided by Ethics Committee of the Faculty of Medicine, Khon Kaen University as instituted by the Helsinki Declaration.
Results
There were 102 patients eligible for this study during the study period. Three cases were excluded due to their Richmond Agitation Sedation Scale (RASS) scores of less than −3. Therefore, there were 99 patients remaining in the study (Fig. 1). The researchers detected delirium in 44 of 99 patients (44.4 %) The demographic data of these patients are shown in Table 1. There were slightly more men than women. Most of them had 6 years or less of education. Pre-existing dementia and depression were evidenced in nearly a half of the delirious patients. Pneumonia or other causes of respiratory failure were the most common causes of admission to the ICU. Nurses under-recognized delirium in about a third (13 out of 44) of the patients as shown in Table 1. Most of them were older women who had a background of dementia. Heart failure and septicemia were the leading causes of being transferred to the ICU. Nearly half of them received benzodiazepines prior to the ICU admission.
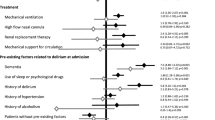
Possible variables associated with under-recognition of delirium by nurses in this setting are presented in Table 2. For multivariate analysis we selected sex, heart failure, pneumonia or other causes of respiratory failure, and pre-existing treatment with benzodiazepines on the basis of quantitative significance from Table 1; on the other hand, we selected age, sensory impairment, dementia, length of stay and presence of hypoactive components of delirium on the basis of literature review [8, 9]. After stepwise multivariate analysis, there were 5 factors remained in the analyses and there were 2 final variables that showed statistical significance—heart failure and pre-existing treatment with benzodiazepines (Table 2).
Discussion
Nurses play a key role for detecting delirium in hospitalized older adults as they are the direct healthcare providers that care for the patients for 24 h. This study investigated delirium in the ICU setting where the presence of delirium is usually higher, and is associated with greater morbidity and mortality [1, 7]. In this study, the under-recognition of delirium by the nurses’ ratings using the CAM–ICU was about a third in comparison to other studies where they used CAM to detect delirium in general care settings [8–10]. The diagnosis of delirium is based mainly on key clinical features, assessing core components of delirium, and therefore is crucial. Practically, existing studies show that the assessment of important features is usually lacking. Nurses usually identified symptoms of delirium as a part of medical conditions alone or therapeutic management alone rather than the diagnosing of delirium [9, 10]. Disorientation and patient’s behavior are usually features that nurses use to specify delirium though disorientation alone demonstrates a low sensitivity and specificity to detect delirium, and delirium in patients whose behavior was not an issue was overlooked [9, 10]. An Italian survey regarding recognition and management of delirium among healthcare professionals also showed that about half of nurses could not define delirium correctly and had modest knowledge about core features of delirium. Moreover, screening tools to detect delirium were not widely used among nurses [15] whereas the subjective clinical impression of delirium was used to detect delirium more than objective assessment [14].
Factors associated with under-recognition of delirium have been documented in prior studies including advanced age, baseline low functional status and sensory impairment, presence of hypoactive delirium, dementia and increased length of stay [8, 9]. The results of this study are inconsistent with the prior reports [8, 9]. The possible explanation is the limited sample size, the differences in clinical settings and study inclusion criteria; however, new independent factors identified from this study are the presence of heart failure and receiving benzodiazepines prior to ICU admission. These factors have been evidenced as either precipitating or predisposing factors of delirium [1, 11]. The potential reasons to explain both conditions are the failure of cognitive assessment, poor documentation of baseline cognitive status and function and difficulty to communicate to these patients. In addition, frustration in the communication with the physicians has been reported as one of the obstacles as physicians’ clinical orders are usually written without doing anything that alleviates patients’ discomfort [24]. Older patients who receive benzodiazepines usually have a hypoactive rather than hyperactive component of delirium [25]. Patients’ behavior such as physical restraint and being agitated that attracts the attention of the nurses is usually documented as delirium [9, 26]. Therefore, nurses tend to under detect the patients who are receiving benzodiazepines as having delirium.
The implications from this study support the previous literature that under-recognition of delirium is a frequent issue, and requires an urgent call for action. Firstly, a strategy to enhance education to nurses regarding the importance of delirium and how to early diagnose delirium using screening tools. There is a consensus that delirium screening in at-risk population is appropriate [13]. Furthermore, related healthcare providers such as physicians and physiotherapists should also be educated in this area because there apparently is a lack of competence in this area in a survey and delirium in older adults requires a multidisciplinary care team to be involved [15]. Secondly, the strategy to eradicate barriers to diagnosing delirium that this study demonstrates, is that novel factors different from prior reports are important, in that patients with heart failure or receiving benzodiazepines are at-risk populations and are under-recognized as delirium. Special attention in these populations is recommended. This is the first study in Thailand regarding the under-recognition of delirium in the acute care setting; however; it is not sufficient to know only the prevalence of this condition. Further research—especially a qualitative study—is essential to explain the barriers of under-recognition and to implement actions to overcome this challenge. Although there are some studies in this area, cultural differences might influence the results [15].
There are some limitations of this study. Firstly, the setting was the ICU of a tertiary care hospital where nursing staff’s turnover was low and the nurses were likely to have extensive experience in taking care of ICU patients. Thus, the results might not be generalized to different settings. Secondly, because the sample size was low, some factors that affect the under-recognition of delirium might not show statistical significance in this report. Additional studies are warranted regarding greater participation and improving the clinical decision process that nurses use to identify delirium.
In conclusion, under-recognition of delirium among older adults in the ICU setting was high, as enlightened by previous reports. Heart failure and prior treatment with benzodiazepines are some of the barriers that prevent nurses to detect delirium.
References
Inouye SK (2006) Delirium in older persons. N Engl J Med 354(11):1157–1165
Praditsuwan R, Limmathuroskul D, Assanasen J, Pakdeewongse S, Eiamjinnasuwat W, Sirisuwat A, Srinonprasert V (2012) Prevalence and incidence of delirium in Thai older patients: a study at general medical wards in Siriraj Hospital. J Med Assoc Thai 95(Suppl 2):S245–S250
Sharma A, Malhotra S, Grover S, Jindal SK (2012) Incidence, prevalence, risk factor and outcome of delirium in intensive care unit: a study from India. Gen Hosp Psychiatry 34(6):639–646
Fagundes JA, Tomasi CD, Giombelli VR, Alves SC, de Macedo RC, Topanotti MF, de Lourdes Ugioni Bristot M, do Brasil PE, Soares M, Salluh J, Dal-Pizzol F, Ritter C (2012) CAM-ICU and ICDSC agreement in medical and surgical ICU patients is influenced by disease severity. PLoS One 7(11):e51010
Leslie DL, Inouye SK (2011) The importance of delirium: economic and societal costs. J Am Geriatr Soc 59(Suppl 2):S241–S243
Limpawattana P, Sutra S, Thavornpitak Y, Sawanyawisuth K, Chindaprasirt J, Mairieng P (2012) Delirium in hospitalized elderly patients of Thailand; is the figure underrecognized? J Med Assoc Thai 95(Suppl 7):S224–S228
Young J, Inouye SK (2007) Delirium in older people. BMJ 334(7598):842–846
Rice KL, Bennett M, Gomez M, Theall KP, Knight M, Foreman MD (2011) Nurses’ recognition of delirium in the hospitalized older adult. Clin Nurse Spec 25(6):299–311
Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM Jr (2001) Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med 161(20):2467–2473
Rice KL, Bennett MJ, Clesi T, Linville L (2014) Mixed-methods approach to understanding nurses’ clinical reasoning in recognizing delirium in hospitalized older adults. J Contin Educ Nurs 45(3):136–148
Fong TG, Tulebaev SR, Inouye SK (2009) Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol 5(4):210–220
Rigney TS (2006) Delirium in the hospitalized elder and recommendations for practice. Geriatr Nurs 27(3):151–157
Teodorczuk A, Reynish E, Milisen K (2012) Improving recognition of delirium in clinical practice: a call for action. BMC Geriatr 12:55
Hussein EM, Hirst S, Salyers V (2014) Factors that contribute to underrecognition of delirium by registered nurses in acute care settings: a scoping review of the literature to explain this phenomenon. J Clin Nurs. doi:10.1111/jocn.12693
Bellelli G, Morandi A, Zanetti E, Bozzini M, Lucchi E, Terrasi M, Trabucchi M (2014) Recognition and management of delirium among doctors, nurses, physiotherapists, and psychologists: an Italian survey. Int Psychogeriatr 26(12):2093–2102
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR (2003) Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289(22):2983–2991
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the Confusion Assessment method. A new method for detection of delirium. Ann Intern Med 113(12):941–948
Wongpakaran N, Wongpakaran T, Bookamana P, Pinyopornpanish M, Maneeton B, Lerttrakarnnon P, Uttawichai K, Jiraniramai S (2011) Diagnosing delirium in elderly Thai patients: utilization of the CAM algorithm. BMC Fam Pract 12:65
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR, Dittus RS (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 291(14):1753–1762
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK (2001) Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 29(7):1370–1379
Vanderbilt University Medical Center (2011) Assessment resources for ICU delirium. http://www.mc.vanderbilt.edu/icudelirium/assessment.html. Accessed 7 Feb 2013
Pipanmekaporn T, Wongpakaran N, Mueankwan S, Dendumrongkul P, Chittawatanarat K, Khongpheng N, Duangsoy N (2014) Validity and reliability of the Thai version of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Clin Interv Aging 9:879–885
Jitapunkul S, Kamolratanakul P, Ebrahim S (1994) The meaning of activities of daily living in a Thai elderly population: development of a new index. Age Ageing 23(2):97–101
Eden BM, Foreman MD (1996) Problems associated with underrecognition of delirium in critical care: a case study. Heart Lung 25(5):388–400
Peterson JF, Pun BT, Dittus RS, Thomason JW, Jackson JC, Shintani AK, Ely EW (2006) Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc 54(3):479–484
Voyer P, Cole MG, McCusker J, St-Jacques S, Laplante J (2008) Accuracy of nurse documentation of delirium symptoms in medical charts. Int J Nurs Pract 14(2):165–177
Acknowledgments
We wish to acknowledge Professor James A. Will, University of Wisconsin-Madison, for editing the manuscript via the Faculty of Medicine Publication Clinic, Khon Kaen University, Thailand. This manuscript was funded by the Neuroscience Research and Development Group, Khon Kaen University, Thailand.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panitchote, A., Tangvoraphonkchai, K., Suebsoh, N. et al. Under-recognition of delirium in older adults by nurses in the intensive care unit setting. Aging Clin Exp Res 27, 735–740 (2015). https://doi.org/10.1007/s40520-015-0323-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0323-6