Abstract
Purpose
This study aimed to examine the psychometric properties of the Chinese version of the modified Yale Food Addiction Scale 2.0 (C-mYFAS 2.0) and to analyze the prevalence of food addiction among Chinese college students and its relationship with resilience and social support.
Methods
A total of 1132 Chinese college students completed the C-mYFAS 2.0, BES, EAT-26, PHQ-9, GAD-7, TFEQ-18, CD-RISC-10, and PSSS. Confirmatory factor analysis was used to evaluate the factor structure of the C-mYFAS 2.0 and psychometric properties were assessed. Test–retest reliability was evaluated in a sub-sample (n = 62). Spearman correlation and logistic regression were used to examine the relationship between resilience, social support, and food addiction.
Results
The prevalence of food addiction according to the C-mYFAS 2.0 was 6.2%. Confirmatory factor analyses suggested a single-factor structure (comparative fit index = 0.961). The C-mYFAS 2.0 had good test–retest reliability and internal consistency (Kuder–Richardson’s α = 0.824). Good convergent validity was indicated by correlations with binge eating, eating disorder symptoms, depressive symptoms, generalized anxiety symptoms, uncontrolled eating, emotional eating, and BMI (ps < 0.001). Appropriate divergent validity was reflected by no association with cognitive restraint. Finally, binge eating was significantly predicted by C-mYFAS 2.0, depressive symptoms, and eating disorder symptoms (ps < 0.001), confirming incremental validity. In addition, our study found that poorer resilience and social support were related to food addiction (ps < .001).
Conclusions
The C-mYFAS 2.0 is a brief but reliable and valid screening instrument for food addiction among Chinese college students. In addition, we found that resilience and social support were negatively associated with food addiction.
Level of Evidence: Level V, cross-sectional descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Addictive disorders refer to a behavioral phenotype characterized in part by a recurrent failure to control consumption/use and continuation of the behavior despite substantial harmful consequences [1]. Addictive disorders are predominantly divided into two categories: substance-use disorders (e.g., tobacco, alcohol) and behavioral addictions (e.g., gambling disorder and the proposed Internet gaming disorder) [2]. In recent years, food addiction (FA) has attracted increasing attention and discussion as a potential addictive disorder, conceptualized as a substance-use disorder in relation to certain foods [3]. It is important to note that the validity and clinical utility of FA is has been debated in the literature [4], including whether it is more appropriate to conceptualize FA as a substance-use disorder or a behavioral addiction [5]. Common controversies of FA include the lack of studies examining neural changes associated with prolonged consumption of highly processed foods in humans [6], the overlap between FA and binge eating disorder [7], and the issue of the biological equivalence between those struggling to control their food and individuals with substance-use disorders [5]. However, while this research area remains in its nascent stages, studies in the past decade have provided compelling evidence for conceptualizing FA as a substance-use disorder to ultra-processed foods (e.g., pizza, chocolate, potato chips) [3].
The proportion of non-clinical samples of different ages and nationalities that meet FA diagnostic criteria range from 2.8% [8] to 38.6% [9]. With the rapid increase of ultra-processed, industry-made foods has led individuals to eat to not only to meet the homeostatic needs of bodily function but also to experience hedonic reward [10]. Notably, symptoms of FA seem to occur uniquely with these ultra-processed foods and not with foods in a natural state. For example, animal studies have found that rats with a high intake of processed foods or intermittent intake of sugar can develop symptoms of FA, including tolerance, overeating, and withdrawal [11]. In addition, studies with humans have found that ultra-processed foods, but not naturally occurring foods, are associated with behavioral indicators of FA and self-reported symptoms of addictive eating [9, 12, 13].
The study of FA is important because the increased availability of ultra-processed foods in the food environment has occurred in line with a rise in the global rates of obesity [14]. Furthermore, the prevalence of binge eating has increased among adolescents over the past several decades [15]. Binge eating has many of the characteristics of addictive behavior, such as reduced control and continued consumption despite adverse consequences [16]; however, it presents theoretical differences when compared with addiction perspectives [17] and is defined by time-restricted binge episodes that may not reflect the full phenotype of addictive-like eating behavior. Importantly, previous studies have found that FA appears to be associated with both obesity and binge eating disorder [18], suggesting that this phenotype may have clinical utility for understanding overweight and overeating disorders.
While FA exhibits some shared features with clinically recognized eating disorders like bulimia nervosa and binge eating disorder [19, 20], it is operationalized as a distinct phenotype. Although FA is not yet considered a clinical diagnosis, it is most commonly defined based on the criteria for substance-use disorders listed in the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM), namely the DSM-5 [21], such as craving, tolerance, and withdrawal symptoms. These shared criteria with addictive disorders have been adapted to refer to addictive consumption of ultra-processed foods and can be assessed using the Yale Food Addiction Scale (YFAS) [22]. The YFAS was originally developed by Gearhardt et al. [23] in 2009 as a 25-item self-report measure assessing the seven criteria for diagnosing substance-use disorders listed in the DSM-IV-TR plus clinically significant impairment and distress [24]. A “diagnostic” score on the YFAS is provided when an individual meets three or more of the seven criteria and either impairment or distress [23]. The YFAS was translated into Chinese by Xiao et al. [25] and introduced into China in 2015.
In 2013, the American Psychiatric Association revised the DSM-5 diagnostic criteria for substance dependence [21]. To maintain consistency with the DSM-5, Gearhardt et al. formally revised and published the new Yale Food Addiction Scale (YFAS 2.0) in 2016, comprising 35 self-report items that assess the 11 diagnostic DSM indicators of substance-use disorders plus clinically significant impairment and distress [26]. The YFAS 2.0 has been translated into French [27], German [28], Italian [29], Spanish [30], and Japanese [31], and exhibited good measurement invariance across genders and racial groups [32].
In 2017, Schulte and Gearhardt [33] developed the modified YFAS 2.0 (mYFAS 2.0), a briefer measure of FA (only comprises 13 items), optimal for use in large-scale epidemiological investigations or simple screening for FA symptoms. While the mYFAS 2.0 performs similarly as the YFAS 2.0, it may underestimate FA symptoms and prevalence in clinical samples compared to the full YFAS 2.0 [34]. The mYFAS 2.0 has also been translated into Italian [35], Arabic [36], and other languages, showing good psychometric characteristics. In both the original study and other language versions [37, 38], the mYFAS 2.0 demonstrated a single-factor structure and exhibited good internal consistency, convergent validity with binge eating, and discriminant validity with substance use measures. In addition, the mYFAS 2.0 has shown incremental validity in predicting binge eating behavior [39].
At present, many studies have explored FA in Western countries. However, there is scarce information about FA in the Chinese population, which may be related to the lack of effective assessment tools for FA in mainland China. A previous survey with 584 Chinese female college students (with a prevalence of obesity of 1.54%) found that 9.4% met the FA diagnostic criteria [25]. In addition, a survey with 608 Chinese adolescents aged 13–17 years found that the prevalence of FA was 6.91% [40]. However, it must be noted that these two Chinese studies used the original version of YFAS, reflecting the seven DSM-IV-TR criteria, instead of the YFAS 2.0, reflecting the current 11 DSM-5 criteria. Using the original YFAS to assess FA in the Chinese population may affect the accuracy and authenticity of FA measurements and research results (e.g., by underestimating the prevalence of FA). Further, the use of a dated instrument is not conducive to enabling other scholars to refer to or integrate the research evidence regarding FA in China; therefore, it is important to use the latest version of the FA measurement tool based on DSM-5 criteria. However, to the best of our knowledge, there is no Chinese version of the YFAS 2.0 or mYFAS 2.0. Based on its convenience with large samples and as a brief screening measure, we chose to first verify the Chinese version of mYFAS 2.0 (C-mYFAS 2.0), though future studies should extend this research to validate a Chinese version of the complete YFAS 2.0.
At present, many studies have found that FA has been associated with psychological and health-related problems. For example, studies with international samples have confirmed that FA is closely related to depression [41], anxiety [42], sleep quality [43], and poor quality of life [44]. However, few studies have considered the relationship between individual positive psychosocial factors and FA. In recent years, numerous studies have assessed individual addictive behaviors from the perspective of positive psychology, with the goal of informing related intervention programs [45]. As an important part of the individual’s positive psychological traits, resilience refers to the ability to adapt to adversity, traumatic events, tragedies, threats, and other stresses [46]. Thus, individuals with high resilience are more likely to cope with difficulties or pressures with courage, optimism, and a positive attitude [47]. This means that higher resilience may also help to reduce the risk of addiction. Previous study suggested that greater resilience may be a protective factor against eating disorders [48]. Therefore, resilience may be also associated with FA. However, no previous research has investigated the relationship between college students’ resilience and FA, let alone within a Chinese sample. Therefore, exploring the relationship between resilience and FA will help to fill the gaps in the literature and provide preliminary evidence for college health educators to understand how fostering resilience may protect against FA.
Another positive psychosocial factor that may be related to FA among Chinese students is social support. China is a collectivist society, and seeking social support reflects this collectivist tendency [49]. Under the influence of collectivism, social eating is one of the social communication methods commonly used by Chinese people to enhance social support [50]. Many studies in China have shown that the social support generated by social eating helps to encourage individuals to follow healthy eating guidelines and actively understand and improve their healthy eating behavior [51,52,53]. Previous studies have also found that social support is closely related to eating disorders, with poor social support being a risk factor [54]. Considering that FA is closely related to eating disorders, it is plausible that social support is also related to FA. Since no prior research has investigated this association, it is important to explore the impact of social support on FA to help inform psychosocial intervention strategies.
Based on the aforementioned gaps in the literature, this study had three objectives. The first was to develop and examine the psychometric properties of the C-mYFAS 2.0 in a non-clinical sample of Chinese college students, to be used for screening for FA. The second objective was to study the prevalence of FA in Chinese college students. The third objective was to study the correlation of FA with resilience and social support.
Methods
Study participants
This study was conducted with undergraduate students from two medical universities in Shandong province using convenience sampling. The inclusion criteria were age ≥ 18 years and having no clinically diagnosed diseases, such as affective, metabolic, substance dependence and addictive disorders (based on the participants’ self-report). Senior students were not considered because they were engaged in internships off-site. We contacted teachers and students at the two universities by email to brief them on the purpose and content of the study. With the help of teachers, each school recruited 600 college students, making a total of 1200 students. After excluding the questionnaires with obvious logical errors (e.g., age < 10 years, attention check questions were filled out incorrectly), 1132 valid questionnaires were recovered. All the participants were concentrated in the classroom to participate in the survey, and uniformly trained investigators guided participants to complete paper questionnaires within 30 min.
In addition, 62 participants (18 men and 44 women) were selected from one of the two medical universities to complete the C-mYFAS 2.0 again 2 weeks later, to enable us to evaluate the test–retest reliability of the scale. Unless otherwise specified, all other reliability and validity indicators used the complete sample (N = 1132). All participants voluntarily participated in the study and they did not receive any payment. Students who did not participate in the study were not subject to any consequences to their academic performance. The study was approved by the Medical Ethics Committee of Xiangya School of Public Health, Central South University (No. XYGW-2017–16). All participants signed an informed consent form.
Translation procedure
We obtained permission from Drs. Schulte and Gearhardt to translate and validate the mYFAS 2.0. The original mYFAS 2.0 in English was translated into Chinese by the three Chinese authors (G.C., Z.L., and Z.C.) and back-translated into English by two graduates majoring in English who had no previous knowledge of the mYFAS 2.0. Three translators and a professor with expertise in social medicine reviewed the differences between the back-translation and the original to produce a final version. Given that eating habits and food preferences in China are different from those in Western countries, we replaced some food examples in the introduction section of the scale. For example, “sweets” included additions like Chinese cakes (red bean cakes, moon cakes, etc.) and jelly. “Starches” included steamed buns, deep-fried dough sticks, noodles, and dumplings, and white bread and rolls were combined into bread. “Salty snacks” included spicy dry tofu, pickles; “fatty foods” included fried food (e.g., fried meat), pork feet, sausage, and potato chips; and “sugary drinks” included soda, coke, milk tea, and fruit tea.
Measurements
mYFAS 2.0
The mYFAS 2.0, the brief version of the YFAS 2.0, was developed by Schulte and Gearhardt [33]. It is a 13-item scale designed to assess FA behaviors during the previous 12 months: 11 items assess symptoms of FA, and 2 items assess diet-related impairment and distress. All items are rated on an 8-point Likert scale (0–7 points). According to the FA diagnostic thresholds, the dichotomous score conversion (0 = did not meet criterion, 1 = met criterion) is performed on each item. If any item that corresponds to the diagnostic criteria or diet-related impairment and distress meets the clinical threshold, this criterion is endorsed. The 13 items were translated into 11 FA diagnostic criteria and 2 clinically impairment or distress criteria. There are two scoring options for the mYFAS 2.0. One is the symptom count scoring method (scores range from 0 to 11), which adds up the diagnostic criteria that the subject meets. The other is a categorical diagnostic method based on the DSM-5 criteria (mild = 2–3 symptoms plus impairment or distress, moderate = 4–5 symptoms plus impairment or distress, severe = 6 or more symptoms plus impairment or distress). We used both scoring methods in the present study.
Binge eating scale
The Binge Eating Scale (BES) is a 16-item scale developed by Gormally et al. [55] to measure binge eating severity. Each item has three to four scoring options, with a range of 0–3. The scores of the 16 items are summed to generate the total BES score; the greater the total score, the more severe the degree of binge eating. According to the scoring method of Marcus et al. [56], a score greater than 17 indicates binge eating symptoms. In this study, we used a Chinese translation version previously used in research [57].
26-Item eating attitude test
The 26-item Eating Attitude Test (EAT-26) was developed by Garner et al. [58] to measure eating disorder behaviors and psychological characteristics. Each item is rated on a 6-point Likert scale ranging from 1 (never) to 6 (always), with total scores ranging from 26 to 156. The higher the score, the greater the tendency toward eating disorder symptoms. In this study, the Chinese version, which was validated by Kang et al. [59], was used.
Patient health questionnaire depression scale
The Patient Health Questionnaire Depression Scale (PHQ-9) was used to assess depressive symptoms during the prior 2 weeks [60]. The scale consists of nine items, each of which is scored from 0 to 3 points (0 = not at all, 1 = a few days, 2 = more than half, 3 = almost every day), with total scores ranging from 0 to 27. The higher the score, the more serious the depressive symptoms. In this study, we used a Chinese version, which was validated in the general population [61].
Generalized anxiety disorder scale
The Generalized Anxiety Disorder Scale (GAD-7), which is based on DSM-IV criteria, was used to evaluate the generalized anxiety symptoms of individuals over a 2-week period approximately [62]. The scale comprises seven items, each of which is scored from 0 to 3 points (0 = not at all, 1 = a few days, 2 = more than half, 3 = almost every day), with total scores ranging from 0 to 21 points. The higher the score, the more serious the generalized anxiety symptoms. We used the Chinese version of GAD-7 [63] in this study.
Revised three factor eating questionnaire
The Revised Three Factor Eating Questionnaire (TFEQ-18) was used to assess three eating behaviors: cognitive restraint, uncontrolled eating, and emotional eating. The original 51-item scale was developed by Stunkard and Messick in 1985 [64], and was simplified to 18 items (TFEQ-18) by Karlsson et al. in 2000 [65]. Each item is rated on a 4-point Likert scale, with a scoring range of 1–4. The higher the score, the greater the tendencies toward cognitive restraint, uncontrolled eating, and emotional eating. In this study, the Chinese version, which was translated and validated by Shi et al. [66], was used.
10-Item connor–davidson resilience scale
The 10-item Connor–Davidson Resilience Scale (CD-RISC-10) was developed by Campbell et al. [67]. as a simplification of the 25-item Connor–Davidson Resilience Scale [46], which is used widely to evaluate respondents’ resilience during the prior month. The scale presents a single factor structure with a total of 10 items. Each item is rated on a 5-point Likert scale ranging from 0 (never) to 4 (almost always), with total scores ranging from 0 to 40. A higher total score indicates greater resilience. In this study, we used a Chinese version, which was validated in the college students [68].
Perceived social support scale
The Perceived Social Support Scale (PSSS) was developed by Zimet et al. [69] to measure subjectively perceived social support. This scale includes 3 dimensions, namely family support (4 items), friend support (4 items), and other support (4 items), with a total of 12 items. Each item rating is rated on a 7-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree), with total scores ranging from 12 to 84 points. A higher total score indicates a higher degree of perceived social support. In this study, we used the Chinese translation version previously used in college students [70].
Demographic information
Demographic information collected included participants’ age, gender, grade, major, and self-reported height and weight. Body mass index (BMI) was calculated using self-reported height and weight. The classification of BMI was determined by the BMI reference norms for screening overweight/obesity in Chinese children and adolescents [71]: lean (< 18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24.0–27.9 kg/m2), obese (≥ 28.0 kg/m2).
Data analysis
All analyses were performed using IBM SPSS version 25.0 (SPSS Inc., Chicago, IL, USA) and Mplus version 7 [72]. All statistical tests were two-tailed and statistical significance for all analyses was set at 0.05. Data were summarized as n (%) for categorical variables and mean ± SD for numerical variables.
The confirmatory factor analysis (CFA) for dichotomous data with weighted least square means and variance adjusted estimation was used to evaluate the factor structure of the C-mYFAS 2.0 11 diagnostic criteria by Mplus. The model fit in CFA was assessed using the root mean square error of approximation (RMSEA), comparative fit index (CFI), Tucker–Lewis index (TLI), and standardized root mean square residual (SRMR). In general, an acceptable fit is denoted by RMSEA values lower than 0.08, CFI and TLI values of 0.90 or greater, and SRMR values below 0.08 [73]. Convergent validity was assessed by inspecting the correlations between the C-mYFAS 2.0 symptom count and FA diagnosis, BES, EAT-26, TFEQ-18, and BMI. The relationships between C-mYFAS 2.0 symptom count and other continuous variables were assessed using Spearman correlation. The relationships between FA diagnostic scoring and other continuous variables were assessed by Kruskal–Wallis H test. We selected 62 participants to complete the C-mYFAS 2.0 again 2 weeks after initial completion and evaluated test–retest reliability by comparing correlations between initial and retest scores of the original 13 items and 11 FA diagnostic criteria.
Previous studies have found the mYFAS 2.0 scores are not significantly associated with the TFEQ cognitive restraint subscale [33]. Therefore, the association between FA and the TFEQ cognitive restraint score was examined to assess discriminant validity. Kuder–Richardson’s α (KR-20) was used to assess the internal consistency of the 11 C-mYFAS 2.0 diagnostic criteria. Hierarchical linear regression analysis was used to assess the incremental validity of the C-mYFAS 2.0 in predicting binge eating according to eating disorder symptoms and depressive symptoms scores. Logistic regression was conducted to analyze the relationship resilience, social support, and FA.
Results
Descriptive statistics
The descriptive statistics for the study sample are presented in Table 1.
FA symptoms and FA diagnosis prevalence
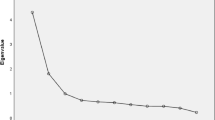
The number of FA symptoms reported by study participants ranged from 0 to 11 (mean = 1.42; SD = 2.19; median = 0). The FA prevalence among the complete sample, men, and women was 6.2% (70/1132), 4.6% (20/435), and 7.2% (50/697), respectively. In addition, the prevalence of mild, moderate, and severe FA according to the C-mYFAS 2.0 was 1.4%, 1.7%, and 3.1%, respectively.
Construct validity and internal consistency
The CFA results showed that the single-factor model for the 11 FA criteria had an acceptable fit to the data (RMSEA = 0.069, 90% confidence interval (CI): 0.061–0.077; CFI = 0.961; TLI = 0.945; SRMR = 0.078). Table 2 shows the factor loadings and proportions of participants who met FA criteria. The KR-20 internal reliability coefficient was 0.824 for the 11 FA criteria. Besides, in this study, the internal consistency coefficients of the BES, EAT-26, PHQ-9, GAD-7, cognitive restraint, uncontrolled eating, and emotional eating, CD-RISC-10, and PSSS were 0.856, 0.799, 0.854, 0.910, 0.807, 0.728, 0.704, 0.923, and 0.939, respectively.
Test–retest reliability
The test–retest correlations were significant for the total scores of the original 13 items (r = 0.759 in all 62 participants, r = 0.812 in 18 men, r = 0.644 in 44 women) and the number of FA symptoms (r = 0.878 in 62 participants, r = 0.887 in 18 men, r = 0.867 in 44 women).
Convergent and discriminant validity
Spearman correlations and Kruskal–Wallis H tests showed that the C-mYFAS 2.0 symptom count and FA diagnosis were positively associated with BES (r = 0.518, H = 103.249, p < 0.001), EAT-26 (r = 0.465, H = 83.309, p < 0.001), depressive symptoms (r = 0.404, H = 57.827, p < 0.001), generalized anxiety symptoms (r = 0.366, H = 48.265, p < 0.001), TFEQ uncontrolled eating (r = 0.407, H = 92.480, p < 0.001), TFEQ emotional eating (r = 0.417, H = 93.926, p < 0.001), and BMI (r = 0.223, H = 138.918, p < 0.001). This indicates that the C-mYFAS 2.0 had good convergent validity. Additionally, TFEQ cognitive restraint (r = 0.057, H = 4.849, p > 0.05) was not associated with the C-mYFAS 2.0 symptom count or FA diagnosis, demonstrating good discriminant validity.
Incremental validity
We used hierarchical liner regression models with the BES total score as the dependent variable, and the PHQ-9, EAT-26, and C-mYFAS 2.0 scores as independent variables to investigate the incremental validity of the C-mYFAS 2.0 (Table 3). Particularly, PHQ-9 and EAT-26 scores were entered in step 1 of the regression model, and the C-mYFAS 2.0 symptom count was entered in step 2. In the first model, depressive symptoms and eating disorder symptoms were significantly and positively associated with binge eating, explaining 38.2% of the variance in the BES total score. In the second model, in which the C-mYFAS 2.0 symptom count was entered, a significant incremental change was observed (R2 change = 0.065, F change = 131.423, p < 0.001).
Relationship of C-mYFAS 2.0 symptom count and FA diagnosis with resilience and social support
The result of Spearman correlation and Kruskal–Wallis H test shows that the C-mYFAS 2.0 symptom count and FA diagnosis were negatively correlated with resilience (r = −0.246, H = 24.332, p < 0.001) and social support (r = − 0.221, H = 15.242, p < 0.001). In addition, we constructed a logistic regression model with the presence or absence of FA (0 = FA absent, 1 = FA present) as the dependent variable, and resilience, social support, and gender as the independent variables. The results showed that resilience and social support were associated with FA (Table 4).
Discussion
To the best of our knowledge, no FA screening tool had yet been assessed for use with Chinese populations that is based on DSM-5 substance-use disorder criteria. This study was the first to investigate the reliability and validity of the C-mYFAS 2.0 with Chinese college students. Our results provide preliminarily evidence on the psychometric properties of the C-mYFAS 2.0 that is suggestive of appropriate reliability and validity within a sample of college students in China.
In this study, 6.18% of the college students exhibited FA, which is comparable to a previous Chinese study using the original version of the YFAS (6.91%) [40], and an Italian study (5.7%) [35]. All three studies may have reported similar percentages because they all involved college students, most of whom were of normal weight. This is a lower prevalence compared with prior results from Europe (e.g., 8.2% in French college students and their families, 10% in German university students) [27, 28] and the United States (e.g., 18.8% in college students) [32], and higher than the results of Japanese undergraduate students (3.3%) [31]. These cultural differences may be related to the low rate of obesity among Chinese college students; indeed, a survey of 11,673 Chinese college students found that the prevalence of obesity was 2.2% [74].
CFA indicated that the single-factor structure had an acceptable fit, with all factor loadings being greater than 0.637, which suggests an acceptable construct validity of the C-mYFAS 2.0. This result is consistent with the single-factor original scale [33]. Our results showed that the internal consistency and test–retest reliability of the C-mYFAS 2.0 were good, consistent with the original, Italian, and Brazilian versions of the mYFAS 2.0 [33, 35, 38]. This provides support for the cross-cultural psychometric properties of the mYFAS 2.0 as a global assessment tool for FA. We also assessed convergent validity by measuring the relationship between the C-mYFAS 2.0 symptom count, FA diagnosis, and scores on each of the BES, EAT-26, PHQ-9, GAD-7, BMI, TFEQ uncontrolled eating, and TFEQ emotional eating. As expected, the number of FA symptoms was significantly correlated with scores on BES, EAT-26, PHQ-9, GAD-7, and BMI. There were also strong correlations with TFEQ uncontrolled eating and TFEQ emotional eating scores. These correlations support the convergent validity of the C-mYFAS 2.0. Furthermore, the C-mYFAS 2.0 symptom count and FA diagnosis were not associated with TFEQ cognitive restraint, which indicates that the C-mYFAS 2.0 has good discriminant validity. Notably, the lack of associations between FA and cognitive restraint were demonstrated in the original scale validation study [26] but has not been replicated in all cultural contexts, such as Japan [31] and Italy [29]. This may be related to the presence of patients with anorexia nervosa in their study sample. Studies in Italy have shown that people with anorexia can have symptoms of both FA and restricting food consumption [29]. Therefore, the relationship between FA and cognitive restriction may be different between non-clinical samples and clinical samples, which warrant empirical investigation. Finally, binge eating was significantly predicted by C-mYFAS 2.0, depressive symptoms, and eating disorder symptoms, confirming incremental validity. Therefore, the C-mYFAS 2.0 showed sufficient reliability and validity to be used among college students in China. This scale may help school doctors to detect early symptoms of FA in this population and facilitate future research on interventions for college students with FA.
Our study also found that resilience and social support were negatively correlated with C-mYFAS 2.0 symptom count, with poor resilience and social support being related to FA. This provides preliminary support to the relationship between positive psychological and social factors and FA. Previous research has shown that interventions related to resilience and social support can help reduce tobacco-use and other substance-use disorders [75,76,77,78]. Based on these findings, resilience and social support interventions should also be examined for potential utility in reducing FA through future longitudinal studies or intervention studies. For example, the resilience of individuals with FA could be enhanced through mindfulness training and music therapy. Alternatively, it would be possible to establish a peer support group for individuals with FA, so that they could support each other to process and manage their shared experiences regarding addictive-like eating. In addition, psychological health education courses and daily extracurricular activities could be used among college students for early prevention of FA. For example, positive psychological training could be added to college students’ mental health education courses to improve their ability to manage stress and prevent them from using food consumption to relieve stress. Schools could also provide teamwork-based extracurricular activities related to healthy eating knowledge, attitudes, and behaviors. These activities could encourage a peer effect among college students and help them to develop healthy eating habits.
Our research had several limitations. First, we recruited college students from two medical schools, which may underestimate FA among college students in China in general, as medical college students generally have high health literacy. In the future, students from comprehensive universities should be selected for further verification. In addition, the C-mYFAS 2.0 should be tested with populations in China who may be most vulnerable to FA, such as individuals with obesity and patients with clinical eating disorders, to verify its psychometric soundness. Second, we used self-reported height and weight to calculate BMI, which may have led to underestimation. In the future, it will be necessary to use objective measures of participants’ height and weight. Finally, this was a cross-sectional study, which prevented us from inferring causal relationships between resilience, social support, and FA. Causality could be verified through longitudinal or interventional studies in the future, which will be important for determining the clinical utility of targeting these constructs in interventions for FA.
Conclusions
The C-mYFAS 2.0 showed a single-factor structure and sufficient test–retest reliability, internal consistency, and convergent and incremental validity in this study; thus, it is suitable for use among Chinese college students. In addition, the prevalence of FA among Chinese college students was 6.2%, and poorer resilience and social support were associated with FA.
What is already known on this subject?
The mYFAS 2.0 is a self-report assessment for food addiction based on DSM-5 criteria. Although there are already many language versions of mYFAS2.0, no previous studies have validated its Chinese version.
What does this study add?
The C-mYFAS 2.0 demonstrated good psychometric properties, and is an appropriate food addiction screening tool for a Chinese college student population. This study suggests that C-mYFAS 2.0 showed a single-factor structure with good psychometric properties. Poorer resilience and social support were also related to food addiction, which provides preliminarily insight into the relationship between positive psychological and social factors and food addiction.
References
Hagedorn WB (2009) The call for a new diagnostic and statistical manual of mental disorders diagnosis: Addictive disorders. J Addict Offender Couns 29(2):110–127. https://doi.org/10.1002/j.2161-1874.2009.tb00049.x
Alavi SS, Ferdosi M, Jannatifard F, Eslami M, Alaghemandan H, Setare M (2012) Behavioral addiction versus substance addiction: Correspondence of psychiatric and psychological views. Int J Prev Med 3 (4):290–294. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354400/
Gearhardt AN, Davis C, Kuschner R, Brownell KD (2011) The addiction potential of hyperpalatable foods. Curr Drug Abuse Rev 4(3):140–145. https://doi.org/10.2174/1874473711104030140
Fletcher PC, Kenny PJ (2018) Food addiction: a valid concept? Neuropsychopharmacol 43(13):2506–2513. https://doi.org/10.1038/s41386-018-0203-9
Hebebrand J, Gearhardt AN (2021) The concept of “food addiction” helps inform the understanding of overeating and obesity: NO. Am J Clin Nutr 113(2):268–273. https://doi.org/10.1093/ajcn/nqaa344
Volkow ND, Wang GJ, Tomasi D, Baler RD (2013) Obesity and addiction: neurobiological overlaps. Obes Rev 14(1):2–18. https://doi.org/10.1111/j.1467-789X.2012.01031.x
Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, Grilo CM (2012) An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord 45(5):657–663. https://doi.org/10.1002/eat.20957
Steward T, Mestre-Bach G, Vintró-Alcaraz C, Lozano-Madrid M, Agüera Z, Fernández-Formoso JA, Granero R, Jiménez-Murcia S, Vilarrasa N, García-Ruiz-de-Gordejuela A, de Las V, Heras M, Custal N, Virgili N, López-Urdiales R, Gearhardt AN, Menchón JM, Soriano-Mas C, Fernández-Aranda F (2018) Food addiction and impaired executive functions in women with obesity. Eur Eat Disord Rev 26(6):574–584. https://doi.org/10.1002/erv.2636
Schulte EM, Sonneville KR, Gearhardt AN (2019) Subjective experiences of highly processed food consumption in individuals with food addiction. Psychol Addict Behav 33(2):144–153. https://doi.org/10.1037/adb0000441
Cawley J (2004) An economic framework for understanding physical activity and eating behaviors. Am J Prev Med 27(3):117–125. https://doi.org/10.1016/j.amepre.2004.06.012
Avena NM, Rada P, Hoebel BG (2008) Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev 32(1):20–39. https://doi.org/10.1016/j.neubiorev.2007.04.019
Schulte EM, Avena NM, Gearhardt AN (2015) Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS ONE 10(2):e0117959. https://doi.org/10.1371/journal.pone.0117959
Pursey KM, Collins CE, Stanwell P, Burrows TL (2015) Foods and dietary profiles associated with “food addiction” in young adults. Addict Behav Rep 2:41–48. https://doi.org/10.1016/j.abrep.2015.05.007
Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes AC, Bes-Rastrollo M (2016) Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr 104(5):1433–1440. https://doi.org/10.3945/ajcn.116.135004
He J, Cai Z, Fan X (2017) Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. Int J Eat Disord 50(2):91–103. https://doi.org/10.1002/eat.22661
Gearhardt A, White M, Potenza M (2011) Binge eating disorder and food addiction. Curr Drug Abuse Rev 4(3):201–207. https://doi.org/10.2174/1874473711104030201
Schulte EM, Grilo CM, Gearhardt AN (2016) Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev 44:125–139. https://doi.org/10.1016/j.cpr.2016.02.001
Smith DG, Robbins TW (2013) The neurobiological underpinnings of obesity and binge eating: a rationale for adopting the food addiction model. Biol Psychiatry 73(9):804–810. https://doi.org/10.1016/j.biopsych.2012.08.026
Meule A, von Rezori V, Blechert J (2014) Food addiction and bulimia nervosa. Eur Eat Disord Rev 22(5):331–337. https://doi.org/10.1002/erv.2306
Burrows T, Skinner J, McKenna R, Rollo M (2017) Food addiction, binge eating disorder, and obesity: is there a relationship? Behav Sci (Basel) 7(3):54. https://doi.org/10.3390/bs7030054
Association AP (2013) Diagnostic and statistical manual of mental disorders—DSM-5. 5th edn edn. American Psychiatric Publishing, Arlington
Davis C (2014) Evolutionary and neuropsychological perspectives on addictive behaviors and addictive substances: relevance to the “food addiction” construct. Subst Abuse Rehabil 5:129–137. https://doi.org/10.2147/SAR.S56835
Gearhardt A, Corbin W, Brownell K (2009) Preliminary validation of the Yale Food Addiction Scale. Appetite 52(2):430–436. https://doi.org/10.1016/j.appet.2008.12.003
Association AP (2000) Diagnostic and statistical manual of mental disorders—DSMIV-TR. 4th edn edn. American Psychiatric Publishing, Washington, DC
Chen G, Tang Z, Guo G, Liu X, Xiao S (2015) The Chinese version of the yale food addiction scale: An examination of its validation in a sample of female adolescents. Eat Behav 18:97–102. https://doi.org/10.1016/j.eatbeh.2015.05.002
Gearhardt AN, Corbin WR, Brownell KD (2016) Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav 30(1):113. https://doi.org/10.1037/adb0000136
Brunault P, Courtois R, Gearhardt AN, Gaillard P, Journiac K, Cathelain S, Réveillère C, Ballon N (2017) Validation of the French version of the DSM-5 yale food addiction scale in a nonclinical sample. Can J Psychiatry 62(3):199–210. https://doi.org/10.1177/0706743716673320
Meule A, Müller A, Gearhardt AN, Blechert J (2017) German version of the Yale food addiction scale 2.0: prevalence and correlates of ‘food addiction’in students and obese individuals. Appetite 115:54–61. https://doi.org/10.1016/j.appet.2016.10.003
Aloi M, Rania M, Muñoz RCR, Murcia SJ, Fernández-Aranda F, De Fazio P, Segura-Garcia C (2017) Validation of the Italian version of the Yale Food Addiction Scale 2.0 (I-YFAS 2.0) in a sample of undergraduate students. Eat Weight Disord 22(3):527–533. https://doi.org/10.1007/s40519-017-0421-x
Granero R, Jiménez-Murcia S, Gearhardt AN, Agüera Z, Aymamí N, Gómez-Peña M, Lozano-Madrid M, Mallorquí-Bagué N, Mestre-Bach G, Neto-Antao MI (2018) Validation of the Spanish version of the Yale Food Addiction Scale 2.0 (YFAS 2.0) and clinical correlates in a sample of eating disorder, gambling disorder, and healthy control participants. Front Psychiatry 9:208. https://doi.org/10.3389/fpsyt.2018.00208
Khine MT, Ota A, Gearhardt AN, Fujisawa A, Morita M, Minagawa A, Li Y, Naito H, Yatsuya H (2019) Validation of the japanese version of the yale food addiction scale 2.0 (J-YFAS 2.0). Nutrients 11(3):687. https://doi.org/10.3390/nu11030687
Carr MM, Catak PD, PejsaReitz MC, Saules KK, Gearhardt AN (2017) Measurement invariance of the Yale Food Addiction Scale 2.0 across gender and racial groups. Psychol Assess 29(8):1044–1052. https://doi.org/10.1037/pas0000403
Schulte EM, Gearhardt AN (2017) Development of the modified Yale food addiction scale version 2.0. Eur Eat Disord Rev 25(4):302–308. https://doi.org/10.1002/erv.2515
Brunault P, Berthoz S, Gearhardt AN, Gierski F, Kaladjian A, Bertin E, Tchernof A, Biertho L, deLuca A, Hankard R (2020) The Modified Yale Food Addiction Scale 2.0: Validation among non-clinical and clinical french-speaking samples and comparison with the full Yale Food Addiction Scale 2.0. Front Psychiatry. https://doi.org/10.3389/fpsyt.2020.480671
Imperatori C, Fabbricatore M, Lester D, Manzoni GM, Castelnuovo G, Raimondi G, Innamorati M (2019) Psychometric properties of the modified Yale Food Addiction Scale Version 2.0 in an Italian non-clinical sample. Eat Weight Disord 24(1):37–45. https://doi.org/10.1007/s40519-018-0607-x
Mobarak EI, Eldeeb D, El-Weshahi H (2019) Reliability of an Arabic version of the Short Form Modified Yale Food Addiction Scale. J High Inst Public Health 49(3):168–174. https://doi.org/10.21608/JHIPH.2019.60843
Carr MM, Schulte EM, Saules KK, Gearhardt AN (2020) Measurement invariance of the Modified yale food addiction scale 2.0 across gender and racial groups. Assessment 27(2):356–364. https://doi.org/10.1177/1073191118786576
Nunes-Neto P, Köhler C, Schuch F, Quevedo J, Solmi M, Murru A, Vieta E, Maes M, Stubbs B, Carvalho AF (2018) Psychometric properties of the modified Yale Food Addiction Scale 2.0 in a large Brazilian sample. Braz J Psychiatry 40(4):444–448. https://doi.org/10.1590/1516-4446-2017-2432
Meule A, Gearhardt AN (2019) Ten years of the Yale Food Addiction Scale: a review of version 2.0. Curr Addict Rep 6(3):218–228. https://doi.org/10.1007/s40429-019-00261-3
Zhao Z, Ma Y, Han Y, Liu Y, Yang K, Zhen S, Wen D (2018) Psychosocial correlates of food addiction and its association with quality of life in a non-clinical adolescent sample. Nutrients 10(7):837. https://doi.org/10.3390/nu10070837
Şanlier N, Türközü D, Toka O (2016) Body image, food addiction, depression, and body mass index in university students. Ecol Food Nutr 55(6):491–507. https://doi.org/10.1080/03670244.2016.1219951
Ahmed AY, Sayed AM, Mostafa KM, Abdelaziz EA (2016) Food addiction relations to depression and anxiety in Egyptian adolescents. Egypt Pediatr Assoc Gaz 64(4):149–153. https://doi.org/10.1016/j.epag.2016.09.002
Najem J, Saber M, Aoun C, El Osta N, Papazian T, Khabbaz LR (2020) Prevalence of food addiction and association with stress, sleep quality and chronotype: A cross-sectional survey among university students. Clin Nutr 39(2):533–539. https://doi.org/10.1016/j.clnu.2019.02.038
Nunes-Neto PR, Köhler CA, Schuch FB, Solmi M, Quevedo J, Maes M, Murru A, Vieta E, McIntyre RS, McElroy SL (2018) Food addiction: Prevalence, psychopathological correlates and associations with quality of life in a large sample. J Psychiatr Res 96:145–152. https://doi.org/10.1016/j.jpsychires.2017.10.003
Krentzman AR (2013) Review of the application of positive psychology to substance use, addiction, and recovery research. Psychol Addict Behav 27(1):151. https://doi.org/10.1037/a0029897
Connor KM, Davidson JR (2003) Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety 18(2):76–82. https://doi.org/10.1002/da.10113
Park JA, Lee EK (2011) Influence of ego-resilience and stress coping styles on college adaptation in nursing students. J Korean Acad Nurs 17(3):267–276. https://doi.org/10.11111/jkana.2011.17.3.267
Las Hayas C, Padierna JA, Muñoz P, Aguirre M, Gomez del Barrio A, Beato-Fernández L, Calvete E (2016) Resilience in eating disorders: a qualitative study. Women health 56(5):576–594. https://doi.org/10.1080/03630242.2015.1101744
Cao C, Zhu C, Meng Q (2021) Chinese international students’ coping strategies, social support resources in response to academic stressors: does heritage culture or host context matter? Curr Psychol 40:242–252. https://doi.org/10.1007/s12144-018-9929-0
Bian Y, Liu C, Lin J (2004) Relationship capital and social eating in Chinese cities: theoretical model and empirical analysis. Open Times 2:93–107. https://doi.org/10.3969/j.issn.1004-2938.2004.02.010
Fang M, Xu L, Huang X, Gu F, Qu X, Xu M, Luo X (2015) Effects of family and peer support upon the stages of health-related behavior in adolescent. Chin J Prev Med 49(9):810–816. https://doi.org/10.3760/cma.j.issn.0253-9624.2015.09.009
Chen M, Fang M, Du Y, Xie W, Zhu Q, Xu L (2017) Phase change behaviors on dietary lipid intake among teenagers:a structural equation modeling analysis. Chin J Sch Health 38(2):169–172. https://doi.org/10.16835/j.cnki.1000-9817.2017.02.004
Zhu X, Sai X, Geng Y, Yang M, Zhao F (2019) Health behaviors and psychosocial determinants among primary and middle school students in Henan province. Chin J Sch Health 40(8):1162–1165. https://doi.org/10.16835/j.cnki.1000-9817.2019.08.012
Limbert C (2010) Perceptions of social support and eating disorder characteristics. Health Care Women Int 31(2):170–178. https://doi.org/10.1080/07399330902893846
Gormally J, Black S, Daston S, Rardin D (1982) The assessment of binge eating severity among obese persons. Addict Behav 7(1):47–55. https://doi.org/10.1016/0306-4603(82)90024-7
Marcus MD, Wing RR, Hopkins J (1988) Obese binge eaters: Affect, cognitions, and response to behavioral weight control. J Consult Clin Psychol 56(3):433. https://doi.org/10.1037//0022-006x.56.3.433
Yan W-S, Zhang R-R, Lan Y, Li Z-M, Li Y-H (2018) Questionnaire-based maladaptive decision-coping patterns involved in binge eating among 1013 college students. Front Psychol 9:609. https://doi.org/10.3389/fpsyg.2018.00609
Garner DM, Olmsted MP, Bohr Y, Garfinkel PE (1982) The eating attitudes test: psychometric features and clinical correlates. Psychol Med 12(4):871–878. https://doi.org/10.1017/s0033291700049163
Kang Q, Chan RCK, Li X, Arcelus J, Yue L, Huang J, Gu L, Fan Q, Zhang H, Xiao Z, Chen J (2017) Psychometric properties of the Chinese version of the eating attitudes test in young female patients with eating disorders in mainland China. Eur Eat Disord Rev 25(6):613–617. https://doi.org/10.1002/erv.2560
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, Zhang G, Zhou Q, Zhao M (2014) Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 36(5):539–544. https://doi.org/10.1016/j.genhosppsych.2014.05.021
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Li C, Qian J, Cui H, Wu W (2010) Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry 22(4):200–203. https://doi.org/10.3969/j.issn.1002-0829.2010.04.002
Stunkard AJ, Messick S (1985) The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 29(1):71–83. https://doi.org/10.1016/0022-3999(85)90010-8
Karlsson J, Persson LO, Sjöström L, Sullivan M (2000) Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women Results from the Swedish Obese Subjects (SOS) study. Int J Obes Relat Metab Disord 24(12):1715–1725. https://doi.org/10.1038/sj.ijo.0801442
Shi M, Kong F, Chen H, Cheng D (2011) Applicability of three fator eating questionaire among Chinese women undergraduates. Chin J J Clin Psychol 19(6):737–739. https://doi.org/10.16128/j.cnki.1005-3611.2011.06.007
Campbell-Sills L, Stein MB (2007) Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress 20(6):1019–1028. https://doi.org/10.1002/jts.20271
Cheng C, Dong D, He J, Zhong X, Yao S (2020) Psychometric properties of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) in Chinese undergraduates and depressive patients. J Affect Disord 261:211–220. https://doi.org/10.1016/j.jad.2019.10.018
Zimet GD, Dahlem NW, Zimet SG, Farley GK (1988) The multidimensional scale of perceived social support. J Pers Assess 52(1):30–41. https://doi.org/10.1207/s15327752jpa5201_2
Kong F, Ding K, Zhao J (2015) The relationships among gratitude, self-esteem, social support and life satisfaction among undergraduate students. J Happiness Stud 16:477–489. https://doi.org/10.1007/s10902-014-9519-2
Group of China Obesity Task Force (2004) Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Chin J Epidemiol, 25 (2):97. https://pubmed.ncbi.nlm.nih.gov/15132858/
Muthén LK, Muthén BO (1998) Mplus user’s guide (Version 7). Los Angeles
Carrión G.C., Nitzl C., Roldán J.L (2017) Mediation Analyses in Partial Least Squares Structural Equation Modeling: Guidelines and Empirical Examples. In: Latan H., Noonan R. (eds) Partial Least Squares Path Modeling. Springer, Cham. Doi: https://doi.org/10.1007/978-3-319-64069-3_8
Jiang S, Peng S, Yang T, Cottrell RR, Li L (2018) Overweight and obesity among Chinese college students: An exploration of gender as related to external environmental influences. Am J Mens Health 12(4):926–934. https://doi.org/10.1177/1557988317750990
Hodder RK, Freund M, Wolfenden L, Bowman J, Nepal S, Dray J, Kingsland M, Yoong SL, Wiggers J (2017) Systematic review of universal school-based ‘resilience’ interventions targeting adolescent tobacco, alcohol or illicit substance use: A meta-analysis. Prev Med 100:248–268. https://doi.org/10.1016/j.ypmed.2017.04.003
Kim HS, Hodgins DC (2018) Component model of addiction treatment: A pragmatic transdiagnostic treatment model of behavioral and substance addictions. Front Psychiatry 9:406. https://doi.org/10.3389/fpsyt.2018.00406
Ford P, Clifford A, Gussy K, Gartner C (2013) A systematic review of peer-support programs for smoking cessation in disadvantaged groups. Int J Environ Res Public Health 10(11):5507–5522. https://doi.org/10.3390/ijerph10115507
Kim SJ, Marsch LA, Brunette MF, Dallery J (2017) Harnessing Facebook for Smoking Reduction and Cessation Interventions: Facebook User Engagement and Social Support Predict Smoking Reduction. J Med Internet Res 19(5):e168. https://doi.org/10.2196/jmir.6681
Acknowledgments
Thank all participants recruited in this study. We also want to thank Dr. Gearhardt for allowing us to translate and use mYFAS2.0.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, S.-J.L., E. -M.S., G.-H.C., Z.-H.L., Z.-M.C. and H.-L.X.; data curation, S.-J.L. and G.-H.C.; formal analysis, S.-J.L.; investigation, S.-J.L., G.-H.C.; methodology, S.-J.L. and Z.-H.L.; software, S.-J.L. and Z.-M.C; validation, S.-J.L.; writing—original draft, S.-J.L. and G.-H.C.; writing—review & editing, E. -M.S. and H.-L.X. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no conflicts of interest.
Ethical approval
The study was approved by the Medical Ethics Committee of Xiangya School of Public Health, Central South University.
Informed consent
All participants signed and approved an informed consent form before participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, S., Schulte, E.M., Cui, G. et al. Psychometric properties of the Chinese version of the modified Yale Food Addiction Scale version 2.0 (C-mYFAS 2.0): Prevalence of food addiction and relationship with resilience and social support. Eat Weight Disord 27, 273–284 (2022). https://doi.org/10.1007/s40519-021-01174-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01174-9