Abstract
Purpose
Obesity among adolescents is becoming increasingly prevalent and “food addiction” (addiction-like attraction to foods with high content of fat and refined carbohydrates) may be a potential contributor to this development. This study aimed to investigate the psychometric properties of the dimensional Yale Food Addiction Scale for Children version 2.0 (dYFAS-C 2.0) and to estimate the weighted mean score on the dYFAS-C 2.0 (as a measure of food addiction symptom load) among adolescents from the general Danish population.
Methods
A total of 3,750 adolescents aged 13–17 were randomly drawn from the general Danish population and invited to participate in a web-based survey. Data on health and socioeconomic factors from the Danish registers were linked to both respondents and non-respondents, which allowed for analysis of attrition. The total- and sex-stratified weighted mean dYFAS-C 2.0 scores were estimated using augmented inverse probability weighted estimation.
Results
A total of n = 576 (15.4%) adolescents participated in survey of whom 55.6% were female. The confirmatory factor analysis of the dYFAS-C 2.0 supported a one-factor model. The dYFAS-C 2.0 total score was associated with eating pathology, BMI z-scores, and ADHD symptomatology. The weighted mean dYFAS-C 2.0 score was 12.1 (95% CI: 11.2;12.9), 15.0 (95% CI: 13.9;16.2) for females and 9.5 (95% CI: 8.3;10.6) for males.
Conclusions
The dYFAS-C 2.0 appears to be a psychometrically valid tool to assess symptoms of food addiction among adolescents. Food addiction symptom severity correlated positively with eating pathology (including restrained eating), BMI z-scores, and ADHD symptomatology.
Level IV, observational cross-sectional descriptive study combined with retrospective register data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity among adolescents is becoming increasingly prevalent [1] and food addiction—i.e., addiction-like attraction to highly processed foods with high levels of saturated fat and refined carbohydrates—has been proposed as a potential mechanism underlying this development [2,3,4]. Highly processed foods (e.g., chocolate, chips, cookies, pizza and other fast foods) are more effective in triggering reward-related neural responses than minimally processed foods (e.g., fruits, vegetables) and are, therefore, often implicated in addictive patterns of consumptions (e.g., loss of control, cravings, continued use despite negative consequences) [3, 5]. Adolescence is a particularly high-risk period for problematic consumption of addictive substances due to a heightened reward drive combined with a relatively less developed inhibitory control system [6]. Thus, the increasing availability of highly processed foods may contribute to excessive intake and contribute to the surge in obesity rates observed among adolescents [7].
Food addiction was first operationalized by the Yale Food Addiction Scale (YFAS) [8], which was based on the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) criteria for substance dependence. The YFAS has since been adapted for use in children and adolescents, resulting in the development of the YFAS for children (YFAS-C) [9]. With the release of the DSM-5 [10], symptoms related to abuse and dependence were merged into one-dimensional measure of substance use disorder including more problem-focused symptoms from the abuse criteria; e.g., “interpersonal problems” and “failure to fulfill role obligations”. These problem-focused criteria are reflected in the updated version of the adult version of the YFAS (the YFAS 2.0) [11], which has shown good psychometric properties in both clinical and non-clinical samples of adults [11,12,13,14]. However, the psychometric properties of the full YFAS-C 2.0 adapted for use in children and adolescents were shown to be suboptimal [16]—mainly due to a low endorsement rate of problem-focused items. Compared to adults, children and adolescents experience fewer responsibilities, and may, therefore, be less likely to experience failure in fulfilling them [15]. Further, the substance misuse may not yet have developed into a dependence disorder, and children and adolescents are therefore less likely to endorse all syndrome criteria including those for impairment and distress [16]. For these reasons, the problem-focused criteria from the adult YFAS 2–0 were omitted in the updated YFAS for children (dYFAS-C 2.0), which focuses exclusively on the 16 items that reflect the remaining core diagnostic criteria for substance use disorders (e.g., loss of control, cravings, continued use despite negative consequences, withdrawal, etc.). Furthermore, the dYFAS-C 2.0 is based on a dimensional approach (not requiring clinical cut-offs), which appears to be more sensitive in detecting emerging addictive-like eating in children and adolescents [17].
In the study by Schiestl & Gearhardt from 2018 [17], the dYFAS-C 2.0 showed promising psychometric properties. For instance, higher dYFAS-C 2.0 scores were associated with higher BMI z-scores, which is in accordance with several other studies finding an association between food addiction and increasing BMI/obesity [18, 19]. Also, high scores on the dYFAS-C 2.0 were associated with more eating pathology (as measured by the Dutch Eating Behavior Questionnaire) [17], and the dYFAS-C 2.0 score was significantly higher among females compared to males, confirming observations from studies among adults [11, 19,20,21,22].
However, the study by Schiestl & Gearhardt remains the only study that has been published using the dYFAS-C 2.0, and the sample was relatively restrictive with exclusion of adolescents with a history of mental disorders (including eating disorders). In fact, the lack of studies with representative random samples also applies for most studies using the first version of the YFAS-C [9, 23,24,25]. Consequently, data on food addiction in adolescents from general populations are sparse.
Denmark has a wide range of nationwide registers, which contain individual-level demographic, socioeconomic, and health-care data for all Danish residents [26]. The nationwide registers have given rise to a longstanding tradition for register-based research and conduction of large-scale nationwide surveys. Denmark is, therefore, well suited for an examination of food addiction in a more representative sample of adolescents. For this reason, we conducted a combined survey and register-based study in Denmark with the following aims:
-
(I)
To investigate the psychometric properties of the dYFAS-C 2.0, including the internal reliability, factor structure, and convergent, discriminant and incremental validity, in a random sample of adolescents from the general population.
-
(II)
To assess the generalizability of the results based on attrition analysis using demographic, socioeconomic and health-care data on both respondents and non-respondents from Danish registers.
-
(III)
To estimate the median and range of the dYFAS-C 2.0 score and the weighted mean dYFAS-C 2.0 score in a general population of adolescents in Denmark (informed by the results of the attrition analysis), and to determine whether the well-known female preponderance in food addiction is also present among Danish adolescents.
Materials and methods
Study design and setting
The data for this study stem from the Food Addiction Denmark Project [27], a nationwide survey conducted in 2018. The survey was linked to data from Danish national registers on demographics, socioeconomics and health-care (see “Register data used for the attrition analyses” below). An in-depth description of the Food Addiction Denmark Project is provided in Horsager et al. [27].
Participants
A total of 3,750 adolescents aged 13–17 years were randomly drawn from the Danish Civil Registration System (DCRS) [28]. All Danish citizens are registered in the DCRS by a personal registration number, which enables linkage of data between the Danish registers and survey data on an individual and de-identified level [28]. For this study, the DCRS also allowed for linkage of the survey invitees to their parents. To be invited, the adolescents had to i) be born in Denmark, ii) have Danish-born parents and iii) have a valid Danish postal address. Adolescents living in an institution or who were otherwise in the care of the authorities were not eligible. Adolescents with parents who were legally incapacitated or if the parents had protected address/name were also not eligible. If siblings were randomly drawn, they were all invited to participate.
Survey procedure
Adolescents were invited via their cohabiting parents, if living together, or via the primary cohabiting parent, if the parents did not live together. The invited adolescents were informed to fill in the questionnaire themselves. The invitation included a personal link to the web-based questionnaire. The initial invitation was sent by an electronic secure mail system (eBoks) [29] used by Danish public authorities. A reminder was sent via surface mail if the invitees had not filled out the questionnaire six weeks after receiving the invitation.
Measures
The measures chosen for the survey represent constructs that are considered to be either convergent with- or discriminant against food addiction, as such measures are required for psychometric validation. This approach is analog to that used in our validation of the adult version of the YFAS 2.0 [12].
The dimensional Yale Food Addiction Scale for Children 2.0 (dYFAS-C 2.0): The dYFAS-C 2.0 contains 16 items and allows for a continuous/dimensional scoring of food addiction with a total score ranging from 0 to 64 [17]. Symptoms are reported for the past twelve months. The full YFAS-C 2.0 was translated into Danish in accordance with the WHO back-translation procedure [30]. The back-translated version of the scale was evaluated by Dr. A. Gearhardt, to ensure agreement with the original version.
The Eating Disorder Examination Questionnaire (EDE-Q): The EDE-Q is based on the Eating Disorder Examination (EDE) clinical interview [31]. The subscales on eating, weight, and shape concern as well as the total score were used in the analysis of convergent validity [13, 20]. Binge eating frequency was used for the incremental and convergent validity analyses, and the subscale on restrained eating was used in the analysis of discriminant validity [11, 13, 20].
The ADHD subscale of the Symptom Checklist-92 (SCL-92): The SCL-92 examines a broad range of psychopathology [32] including ADHD. In the context of this study, the ADHD subscale was used as a measure of impulsivity and attention deficit in the analysis of convergent validity, since impulsivity and ADHD symptoms have been reported to be associated with food addiction [33, 34].
The Alcohol Use Disorder Test (AUDIT): The AUDIT was developed to detect alcohol dependence and problematic use of alcohol, and is considered to be valid for use in adolescence [35]. Alcohol dependence has been shown to correlate inversely (or not at all) with food addiction, and was, therefore, used as a discriminant construct in the validity analysis [21].
Weight and height: Weight and height were self-reported. Body Mass Index (BMI) varies with sex and age in growing children and adolescents; therefore, we computed the BMI z-score, taking the common growth according to age and sex into account [36]. The BMI z-score was categorized according to the WHO definitions of underweight/thinness < − 2 SD, normal weight − 2 SD > + 1 SD, overweight + 1 SD < + 2 SD, and obesity > + 2 SD [36]. BMI z-scores > + 5.5 and < − 4.5 were considered biologically implausible, and we, therefore, intended to exclude individuals with such values from the analyses. However, all BMI z-scores were within the biologically plausible range.
Definition of complete response to the dYFAS-C 2.0
Complete response to the dYFAS-C 2.0 was defined as having answered all 16 questions, and the psychometric validation analyses were based only on data from those with complete response to the dYFAS-C 2.0. There were only few who did not complete the dYFAS-C 2.0 among those who began responding to the survey (YFAS-C 2.0 was the first questionnaire in the battery). For this reason, we considered partial responders to the dYFAS-C 2.0 (e.g., only answered three out of 16 items) to be non-respondents.
Register data used for the attrition analyses
For both respondents and non-respondents, data on demographics (age, sex, parental marital status, urbanization, geography/region of residence), socioeconomics (parental highest educational level, parental highest occupation status and the family’s equivalised disposable income), and health-care (adolescent and parental prior somatic illness operationalized by the Charlson Comorbidity Index [37], adolescent and parental prior mental disorders, and finally adolescent and parental prior use of psychotropic medication) were obtained from the following Danish registers: the DCRS [28], the registers on personal level of education [26], the registers on personal labor market affiliation [26], the Income Statistics Register [26], the Danish National Patient Register [38], the Psychiatric Central Research Register [39], and the National Prescription Register [40], respectively. A thorough description of the demographic, socioeconomic, and health-care variables is provided in Supplement S1.
Ethics
The included adolescents were invited via their parents (legal guardians) to ensure that the parents were informed on the purpose of the study. This procedure ensured that the parents were able to decide whether their child should have the opportunity to participate in the survey, and that it was the parents who provided informed consent. The parents (and the adolescents) were informed that participation in the survey was voluntary and that the consent to participate could be withdrawn at any time. The study was, therefore, performed in accordance with the principles of the Declaration of Helsinki. The questionnaire and survey methodology were approved by the Danish Health Data Authority, and approval of the use of data from the Danish registers was granted by Statistics Denmark and the Danish Health Data Authority. In Denmark, ethical review board approval is not required for survey and register-based studies if they do not include collection of biological material. Data obtained from the survey and data from the Danish registers were de-identified by Statistics Denmark before being made available to the authors of this study. The project was registered with the Danish Data Protection Agency (record number 2008-58-0028).
Statistics
Before running the statistical analyses, the underlying model assumptions were checked, and if the assumptions were not met, alternative non-parametric analyses were chosen. Specific details on model assumptions are provided for each analysis in the section below. All analyses were conducted using STATA version 15.1.
We deliberately chose only to include complete responses of the dYFAS-C 2.0 in the confirmatory factor analysis. Therefore, imputation of missing values was not required. The same applied for analyses of the construct validity, which included other measures than the dYFAS-C 2.0, here both the dYFAS-C 2.0 and the other scale/subscale of interest should be complete to be included. The number of included responses, therefore, differs from analysis to analysis (specified in the tables and figures in the results section).
Attrition analyses: The respondents (complete response to the dYFAS-C 2.0) and non-respondents were characterized using descriptive statistics, i.e., means and standard deviations (SDs) for continuous variables, and relative frequencies for categorical variables. Comparisons between respondents and non-respondents were conducted using Chi2 test/Fishers exact test and student’s simple t-test, with the significance level set at p < 0.05.
Factor structure and reliability of the dYFAS-C 2.0: The psychometric validity was tested in accordance with the original work on the dYFAS-C 2.0 [17] including an examination of the internal consistency using Cronbach’s alpha, and a confirmatory factor analyses for a one-factor model with calculation of the following fit indices; comparative fit index (CFI), Tucker–Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). The fit indices were considered as adequate according to Barrett [41] with: CFI ≥ 0.90–0.95, TLI ≥ 0.90–0.95, RMSEA ≤ 0.06–0.08, and Cronbach’s alpha > 0.80 [42]. Furthermore, the model fit indices were also compared against obtained in the original dYFAS-C 2.0 study [17]. Due to the relatively large sample size, the assumption regarding multivariate normality for the CFA analysis was assessed via Q–Q plots only. All of the dYFAS-C 2.0 item scores were non-normally distributed. Therefore, robust maximum likelihood estimation (MLR) was applied to the CFA model [43].
The crude dYFAS-C 2.0 total score and weighted dYFAS-C 2.0 total score estimate: The crude mean dYFAS-C 2.0 total score was reported for all respondents and stratified on sex (scores of males and females compared using simple t-test). Because model assumptions were violated (the dYFAS-C 2.0 total score was not normally distributed), bootstrapping with 1000 replications was used to estimate the 95%CI for the mean values. Additionally, informed by the attrition analyses, weighted estimates of the mean dYFAS-C 2.0 score were computed using augmented inverse probability weighted estimation (AIPW) [44]. The assumptions for the AIPW model, namely” stable unit treatment value” and “strong ignorability” were met. In the AIPW model, the variables were included in the following order: age, sex, parental marital status, parental socioeconomic factors (highest educational level, highest occupational status and family’s equivalised disposable income), urbanization, geography/region of residence, adolescent prior somatic illness (the Charlson Comorbidity Index) [37], adolescent prior mental disorders and finally adolescent prior use of psychotropic medication (the latter as yes/no).
Convergent and discriminant validity of the dYFAS-C 2.0: The convergent and the discriminant validity [8, 9, 11, 17] were evaluated using Pearson’s correlation coefficient comparing the dYFAS-C 2.0 total score and scores for the theoretically convergent and discriminant constructs mentioned in the section on measures above. In addition, the correlation of the dYFAS-C 2.0 total score with age and BMI z-score, respectively, was evaluated. Only complete responses on the included measures of interest were used for the correlation analyses. A Pearson’s correlation coefficient (|r|) ≥ 0.30 was considered a relevant association [45] and the cut-off for statistical significance was set at p < 0.05.
Incremental validity of the dYFAS-C 2.0: Multiple hierarchical regression analysis was used to examine incremental validity [11, 17]. Specifically, the predictive effect of binge eating frequency and the dYFAS-C 2.0 total score on the BMI z-score was estimated. In the first model, binge eating frequency was entered as the only explanatory variable for the BMI Z-score. In the second model, the dYFAS-C 2.0 total score was entered along with binge eating frequency to evaluate the unique variance in the BMI Z-score accounted for by each of the two measures.
Results
In total, n = 576 of the 3750 invitees filled in the full 16-item dYFAS-C 2.0 questionnaire, corresponding to a response rate of 15.4%.
Attrition analysis: The results of the attrition analysis are presented in Table 1. The respondents, compared to the non-respondents, were more likely to be female (55.6% vs. 47.4%, p < 0.001) and slightly younger (14.8 years vs. 15.1 years, p = 0.001). The parents of the respondents more often (i) had a higher education (both medium-cycle and long-cycle higher education) (p < 0.001), (ii) were in the labor force (p = 0.034), and (iii) were in the higher income quintiles (p = 0.003). The respondents more often lived in densely populated areas and less often in intermediately populated areas compared to non-respondents (p = 0.025), and they were more likely to come from the capital or Central Jutland and less likely to residence in Southern Jutland and Zealand (p = 0.042). No difference was observed with regard to the lifetime somatic illness load (i.e., the Charlson Comorbidity Index), among the respondents vs. the non-respondents (p = 0.342 for the adolescents and p = 0.599 for the parents, respectively). Non-respondents were more likely to be registered with a mental disorder (lifetime) compared to the respondents (p = 0.032) and were more likely to be registered with prior use (lifetime) of psychotropic medication than were the respondents (p = 0.007). Mental disorder (lifetime status) was also more prevalent among the parents of the non-respondents compared to the parents of the respondents (p = 0.032), The same was the case regarding prior use (lifetime) of psychotropic medication (p < 0.001).
Factor structure and reliability of the dYFAS-C 2.0: Factor loadings for each of the 16 items of the dYFAS-C 2.0 are provided in Table 2. The confirmatory factor analyses for the single factor model showed factor loadings in the range from 0.38 (“I ate certain food all day long”) up to 0.83 (“I really wanted to cut down or stop eating certain kinds of foods, but I just couldn’t.”), both with p-values < 0.001. The fit indices were as follows: the CFI = 0.86, the TLI = 0.84, the RMSEA = 0.099, and the SRMR = 0.06. The Cronbach’s alpha (internal consistency) was 0.92.
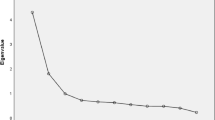
Crude and weighted estimates of dYFAS-C 2.0 total score: The median dYFAS-C 2.0 total score was 10.0 (min:0 and max:44), and the crude mean dYFAS-C 2.0 total score was 11.9 (95% CI: 11.1;12.7) for the total sample, and 14.2 (95% CI: 13.1;15.3) for females and 9.1 (95% CI: 8.1;10.1) for males, respectively. The female–male difference in the crude mean dYFAS-C total score was statistically significant (5.1, p < 0.001). In Fig. 1, a graphical illustration of the stepwise weighting of the mean dYFAS-C 2.0 total score is shown. The weighted mean total score was 12.1 (95% CI: 11.2;12.9) for the total sample, and 15.0 (95% CI: 13.9;16.2) for females and 9.5 (95% CI: 8.3;10.6) for males.
Figure 2 shows the relationship between the mean dYFAS-C 2.0 score and weight categories based on BMI z-scores. Among the respondents, 8.2% (n = 45) were overweight and 2.7% (n = 15) were obese.
Convergent and discriminant validity of the dYFAS-C 2.0
The results of the analyses of convergent and discriminant validity of the dYFAS-C 2.0 are shown in Table 3. Eating pathology correlated moderately to strongly with the dYFAS-C 2.0 total score. This applied for the global score of the EDE-Q (r = 0.56, p < 0.05) as well as for all of its subscales (eating concern (r = 0.55, p < 0.05), shape concern (r = 0.56, p < 0.05), binge eating frequency (r = 0.46, p < 0.05) and restrained eating (r = 0.41, p < 0.05)). The ADHD subscale also correlated moderately with the dYFAS-C 2.0 total score (r = 0.47, p < 0.05). The correlation coefficients for the dYFAS-C 2.0 total score and the BMI z-score and the AUDIT score were r = 0.29 (p < 0.05) and r = 0.14 (p < 0.05), respectively.
Incremental validity of the dYFAS-C 2.0: The first model was based on data from 542 respondents with data on binge eating frequency and BMI z-score. Here, binge eating frequency was examined as explanatory variable in relation to the BMI z-score. The results showed that binge eating frequency was a significant predictor of BMI z-score (t = 5.01, coeff. = 0.36 [0.22;0.50], p < 0.001) explaining 4.4% of the variance in the model. When adding the dYFAS-C 2.0 total score to the model (based on data from the same 542 respondents), the association between binge eating frequency and the BMI z-score weakened (t = 2.11, coeff. = 0.17 [0.01;0.32], p = 0.036), and the dYFAS-C 2.0 total score was more strongly associated with the BMI z-score (t = 5.35, coeff. = 0.027 [0.02;0.04], p < 0.001), accounting for additional 4.8% of the variance in the BMI z-score.
Discussion
In this study, we evaluated the psychometric validity of the Danish version of the dYFAS-C 2.0 in a random sample of adolescents from the general Danish population. Furthermore, we conducted comprehensive attrition analyses based on demographic, socioeconomic and health-care data from both respondents and non-respondents to assess the generalizability of the results. Based on the results from the attrition analyses, the weighted mean dYFAS-C 2.0 total score for Danish adolescents was estimated. Despite a relatively low response rate, the crude and the weighted mean dYFAS-C 2.0 total scores were very similar (difference not statistically significant), suggesting that selection bias had no considerable impact on the dYFAS-C 2.0 score.
The weighted dYFAS-C 2.0 total scores found in this study (15.0 for females and 9.5 for males, respectively) were much lower compared to those reported in the only other study of the dYFAS-C 2.0 (30.0 for females and 25.0 for males, respectively), which was conducted in the United States [17]. The most likely explanation for this difference is that more participants were overweight and obese in the US sample (mean BMI z-score 0.95, SD = 0.89) compared to respondents in the present study from Denmark (mean BMI z-score − 0.20, SD = 1.07). Even though the sample in the study by Schiestl et al. may not be representative of the American population, the higher prevalence of overweight and obesity in their sample compared to those reported for our Danish sample is compatible with the fact that rates of overweight and obesity among adolescents are substantially higher in the US (20.6% in the age group 14–19 years with obesity) [46] compared to Denmark; (in 2016, 15% were overweight and 4% obese among the 14–16-year-olds [47]. Similarly, in 2017 among the 16–24-year-olds, 21.0% of the males and 15.6% of the females were overweight, while 6.6% of the males and 8.1% of the females were obese [48]). There are many potential underlying reasons for this difference—one probably being a more “toxic” food environment in the US with easier access to highly processed foods [49]. The finding of different levels of food addiction symptomatology among adolescents across countries has important implications, as it may help identifying risk/protective factors with regard to development of food addiction.
The dYFAS-C 2.0 was developed as a tool for assessing indicators of food addiction in adolescence—a phase of life characterized by high incidence of addiction disorders [6, 50]. The study by Schiestl et al. showed that its psychometric properties were promising [17]. Compared to Schiestl et al., the factor loadings for the one-factor structure at the item level are somewhat higher in the present study (in the range 0.38 to 0.83). The same is the case for the internal consistency (Cronbach alpha 0.92). These findings lend further support to the validity of the dYFAS-C 2.0 and its applicability across cultures and languages.
The dYFAS-C 2.0 score correlated with the BMI z-score, although the correlation was rather weak (r = 0.29, p < 0.05). However, when examining the incremental validity, the dYFAS-C 2.0 predicted the BMI z-score over and above binge eating frequency, accounting for 4.4% of the variance in the BMI z-score. This is well in line with findings from our validation of the Danish version of the adult YFAS 2.0 in which 4.7% of the variance in the BMI was explained by the YFAS 2.0 [12] and also in accordance with the original study on dYFAS-C 2.0 where 3.4% of the variance in the BMI z-score was explained by the dYFAS-C 2.0 [17]). Taken together, these results suggest the dYFAS-C 2.0 is also able to capture food addiction symptoms in more lean populations (the sample in the present study).
For the evaluation of the construct validity, we used hypothesis testing with theoretically convergent and discriminant measures. The results presented in the correlation matrix (Table 3) followed the same pattern as most other validation studies on the YFAS 2.0 [11, 17, 20], including our recent validation of the YFAS 2.0 in the adult Danish general population [12]. Among the theoretically convergent food addiction measures, the dYFAS-C 2.0 score correlated moderately to strongly with all measures of eating pathology. Eating and shape concern and the global EDE-Q score (measure of total eating pathology) were the eating-pathology measures that correlated most strongly with the dYFAS-C 2.0. This corresponds well with validation studies on the adult YFAS 2.0 [11, 14] and with the quite consistent findings of high prevalence of food addiction (or high YFAS symptom scores) in populations with eating disorders [51, 52].
Restrained eating was hypothesized to be a discriminant construct in the context of food addiction. However, we found a moderately strong positive correlation between food addiction and restrained eating. While more studies have found restrained eating to be discriminant in the context of food addiction [11, 13], there is a growing body of evidence suggesting a positive association between restrained eating and food addiction also among adolescents [17]. This somewhat counterintuitive finding could be explained by the subjective feeling of control loss that individuals with anorexia nervosa experience or other restrictive eating patterns experience when eating even objectively small portions of food [18]. Another explanation could be that restrictive behavior could play a significant role in the food addiction pathophysiology, contributing to the development and maintenance of it. Indeed, dietary restriction has been identified as a potential positive predictor of BMI [53]—possibly due to the fact that it is representative of repeated and unsuccessful attempts to maintain weight. This hypothesis is supported by the findings of studies by Gearhardt et al. showing that weight cycling is associated with food addiction [11, 51]. Future studies should explore the relationship between food addiction and restrained eating in further detail, as it could potentially aid the understanding of the pathophysiological/behavioral mechanisms underlying the development and maintenance of food addiction.
Impulsivity and ADHD symptomatology in general were hypothesized to be convergent with food addiction. In this study, we found a moderately strong positive correlation between the dYFAS-C 2.0 score and the SCL-92 ADHD subscale. This is in agreement with prior studies reporting that food addiction correlates positively with impulsive personality traits, e.g., [34]. Considering that i) impulsivity is a key symptom in ADHD, ii) addiction disorders often co-occur with ADHD [54], and iii) obesity rates are elevated among individuals with ADHD [55], studying food addiction among individuals with ADHD would be of great relevance. Studies on ADHD and food addiction are, however, sparse, but the results are indeed indicative of a positive association [33]. Hence, targeting food addiction among individuals with ADHD could be a potential target in fighting obesity in this population [55].
Somewhat surprisingly, we found a significant, albeit weak, correlation between the dYFAS-C 2.0 score and the included measure of alcohol abuse and dependence (AUDIT score). We hypothesized that alcohol abuse/dependence would be a discriminant construct in relation to food addiction, as most studies have found either a negative association or no association between alcohol use disorder and food addiction [21]. The apparent co-existence of alcohol-related problems and food addiction among adolescents, which was also seen in a Dutch study [56], may be explained from a developmental perspective. Specifically, an emerging propensity towards addiction in adolescence [6] may manifest itself as problematic intake of both alcohol and highly processed foods because the “drug of choice” has not yet been consolidated. Longitudinal studies on the co-existence of alcohol and food addiction are needed to learn when and if these conditions separate—and to tease out the determinants of the outcome (alcohol and/or food addiction) of this development.
There are a number of limitations to this study, which should be taken into account. The limitations of the Food Addiction Denmark Project which provides data for this study are covered thoroughly elsewhere [27]. Here, we will predominantly focus on the limitations associated specifically with studying food addiction among adolescents based on the data at hand. First and foremost, the survey data are cross-sectional, which rules out the opportunity to investigate the temporality of the association between the measures collected in the survey. Additionally, the survey response rate was quite low (15.4%). Here, it is important to keep in mind that the adolescents were invited via their parents, which may have declined participation on behalf of their adolescent child (especially if he/she had problems related to eating). However, due to the availability of sociodemographic, socioeconomic and health-care data on both respondents and non-respondents, we were able to estimate the weighted mean dYFAS-C 2.0 score, which differed very little from the crude estimate. Notably however, we were not able to include BMI in the AIPW model used to calculate the weighted dYFAS-C 2.0 scores, as this measure was only available for respondents. Consequently, the weighted estimate does not account for the fact that the prevalence of overweight and obesity among the respondents (8.2% were overweight, 2.7% were obese) is lower than that of Danish adolescents in general. Indeed, in 2016 15% were overweight and 4% obese among the 14–16-year-olds [47]. Similarly, in 2017 among the 16–24-year-olds, 21.0% of the males and 15.6% of the females were overweight, while 6.6% of the males and 8.1% of the females were obese [48]. This suggests that the weighted mean dYFAS-C 2.0 score estimated in this study may be underestimated due to selection bias.
Furthermore, self-reported weight tends to be underestimated [57], which likely introduces a bias. However, it has also been shown that when young adults self-report height and weight, the resulting BMI does not differ substantially from that obtained by clinicians [58].
To ensure that all invitees could understand the questionnaire, only adolescents born in Denmark who had Danish-born parents were invited to participate. For this reason, the results of this study will mainly generalize to this fraction of the general population in Denmark. According to Statistics Denmark, approximately 86% of the Danish population is of Danish ethnicity. Adolescents who were i) living in an institution, or ii) had parents with protected address or name, or iii) parents who were legally incapacitated were also not invited for participation. This is, however, a quite small minority.
In conclusion, this is the first study to validate the dimensional dYFAS-C 2.0 in a random sample of adolescents drawn from a general population. The results from the confirmatory factor analysis and the evaluation of the construct validity indicated that the Danish version of the dYFAS-C 2.0 has psychometric properties comparable with, and in some cases better than, those of the original version (Schiestl et al.). Notably, the weighted mean dYFAS-C 2.0 score was very similar to the crude estimate, suggesting that attrition does not affect the dYFAS-C 2.0 score substantially. Taken together, these results clearly support that the dYFAS-C 2.0 is a useful tool for assessing emerging food addiction symptomatology in adolescents. Finally, the food addiction symptom load (dYFAS-C 2.0 score) was relatively low in the present study, suggesting that addictive behavior (at least with regard to food) may not by fully developed in Danish adolescents. Indeed, food addiction symptomatology may develop later in the Danish setting compared to the US—potentially due to differences in food culture including the degree of exposure to highly processed foods. Future investigations of food addiction symptomatology in the transition from adolescence to adulthood could help elucidating the underlying etiological mechanisms and perhaps identify specific risk factors for the development of food addiction.
What is already known on this subject?
The only prior study based on the dYFAS-C 2.0 found the scale to be a valid and sensitive measure of symptoms of food addiction in adolescents who were overweight or obese.
What this study adds?
The results of the present study suggest that the dYFAS-C 2.0 is also a psychometrically valid tool in the assessment of emerging symptoms of food addiction among adolescents from the general population.
Availability of data and material
In accordance with Danish legislation, the original (individual-level) data cannot be shared due to their personal sensitive nature.
References
World Health Organisation. (2018). World Health Organisation Fact sheet on Obesity and overweight. Retrieved February 14, 2019, from https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight
Lindgren E, Gray K, Miller G, Tyler R, Wiers CE, Volkow ND, Wang GJ (2018) Food addiction A common neurobiological mechanism with drug abuse. Frontiers in Bioscience 23(3):811–836. https://doi.org/10.2741/4618
Schulte E, Avena N, Gearhardt AN (2015) Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS ONE 10(2):e0117959. https://doi.org/10.1371/journal.pone.0117959
Parnarouskis L, Schulte EM, Lumeng JC, Gearhardt AN (2020) Development of the Highly Processed Food Withdrawal Scale for Children. Appetite 147:104553. https://doi.org/10.1016/j.appet.2019.104553
Small, D. M., & DiFeliceantonio, A. G. (2019). Processed foods and food reward. Science, 363(6425), 346 LP – 347. https://doi.org/https://doi.org/10.1126/science.aav0556
Casey BJ, Jones RM (2010) Neurobiology of the adolescent brain and behavior: Implications for substance use disorders. J Am Acad Child Adolesc Psychiatry 49(12):1189–1201. https://doi.org/10.1016/j.jaac.2010.08.017
Gearhardt, A. N., Davis, C., Kuschner, R., & Brownell, K. D. (2011). The addiction potential of hyperpalatable foods. Current drug abuse reviews, 4(3), 140–145.
Gearhardt AN, Corbin WR, Brownell KD (2009) Preliminary validation of the Yale Food Addiction Scale. Appetite 52(2):430–436. https://doi.org/10.1016/j.appet.2008.12.003
Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD (2013) Preliminary validation of the Yale Food Addiction Scale for children. Eat Behav 14(4):508–512. https://doi.org/10.1016/j.eatbeh.2013.07.002
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) (Revised 5t.). American Psychiatric Publishing.
Gearhardt, A. N., Corbin, W. R., & Brownell, K. D. (2016). Development of the Yale Food Addiction Scale Version 2.0. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 30(1), 113–121. https://doi.org/https://doi.org/10.1037/adb0000136
Horsager, C., Færk, E., Lauritsen, M. B., & Østergaard, S. D. (2020). Validation of the Yale Food Addiction Scale 2.0 and estimation of the population prevalence of food addiction. Clinical Nutrition, 39(9), 2917–2928. https://doi.org/10.1016/j.clnu.2019.12.030.
Meule, A., Muller, A., Gearhardt, A. N., & Blechert, J. (2017). German version of the Yale Food Addiction Scale 2.0: Prevalence and correlates of “food addiction” in students and obese individuals. Appetite, 115, 54–61.
Granero, R., Jimenez-Murcia, S., Gearhardt, A. N., Aguera, Z., Aymami, N., Gomez-Pena, M., Fernandez-Aranda, F. (2018). Validation of the Spanish Version of the Yale Food Addiction Scale 2.0 (YFAS 2.0) and Clinical Correlates in a Sample of Eating Disorder, Gambling Disorder, and Healthy Control Participants. Frontiers in psychiatry, 9, 208. https://doi.org/https://doi.org/10.3389/fpsyt.2018.00208
Piontek D, Kraus L, Legleye S, Bühringer G (2011) The validity of DSM-IV cannabis abuse and dependence criteria in adolescents and the value of additional cannabis use indicators. Addiction 106(6):1137–1145. https://doi.org/10.1111/j.1360-0443.2010.03359.x
Liu RT (2017) Substance Use Disorders in Adolescence Exist along Continua: Taxometric Evidence in an Epidemiological Sample. J Abnorm Child Psychol 45(8):1577–1586. https://doi.org/10.1007/s10802-017-0269-6
Schiestl, E. T., & Gearhardt, A. N. (2018). Preliminary validation of the Yale Food Addiction Scale for Children 2.0: A dimensional approach to scoring. European Eating Disorders Review, 26(6), 605–617. https://doi.org/https://doi.org/10.1002/erv.2648
Penzenstadler L, Soares C, Karila L, Khazaal Y (2018) Systematic Review of Food Addiction as Measured with the Yale Food Addiction Scale: Implications for the Food Addiction Construct. Curr Neuropharmacol 17(6):526–538. https://doi.org/10.2174/1570159x16666181108093520
Meule, & Gearhardt, A. N. (2019). Ten Years of the Yale Food Addiction Scale: a Review of Version 2.0. Current Addiction Reports, 6(3), 218–228. https://doi.org/https://doi.org/10.1007/s40429-019-00261-3
Aloi, M., Rania, M., Rodríguez Muñoz, R. C., Jiménez Murcia, S., Fernández-Aranda, F., De Fazio, P., & Segura-Garcia, C. (2017). Validation of the Italian version of the Yale Food Addiction Scale 2.0 (I-YFAS 2.0) in a sample of undergraduate students. Eating and Weight Disorders, 22(3), 527–533. https://doi.org/https://doi.org/10.1007/s40519-017-0421-x
Nunes-Neto, P. R., Kohler, C. A., Schuch, F. B., Solmi, M., Quevedo, J., Maes, M., Carvalho, A. F. (2017). Food addiction: Prevalence, psychopathological correlates and associations with quality of life in a large sample. Journal of psychiatric research, 96, 145–152.
Burrows, T., Hides, L., Brown, R., Dayas, C. V, & Kay-Lambkin, F. (2017). Differences in Dietary Preferences, Personality and Mental Health in Australian Adults with and without Food Addiction. Nutrients, 9(3). https://doi.org/https://doi.org/10.3390/nu9030285
Chen G, Tang Z, Guo G, Liu X, Xiao S (2015) The Chinese version of the Yale Food Addiction Scale: An examination of its validation in a sample of female adolescents. Eat Behav 18:97–102. https://doi.org/10.1016/j.eatbeh.2015.05.002
Rodrigue C, Gearhardt AN, Bégin C (2019) Food Addiction in Adolescents: Exploration of psychological symptoms and executive functioning difficulties in a non-clinical sample. Appetite 141:104303. https://doi.org/10.1016/j.appet.2019.05.034
Zhao, Z., Ma, Y., Han, Y., Liu, Y., Yang, K., Zhen, S., & Wen, D. (2018). Psychosocial correlates of food addiction and its association with quality of life in a non-clinical adolescent sample. Nutrients, 10(7). https://doi.org/https://doi.org/10.3390/nu10070837
Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H, Bronnum-Hansen H (2011) Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scandinavian Journal of Public Health 39(7 Suppl):12–16. https://doi.org/10.1177/1403494811399956
Horsager C, Østergaard SD, Lauritsen MB (2019) The Food Addiction Denmark (FADK) Project: A combined survey- And register-based study. Acta Neuropsychiatrica 31(6):325–336. https://doi.org/10.1017/neu.2019.34
Schmidt M, Pedersen L, Sørensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29(8):541–549. https://doi.org/10.1007/s10654-014-9930-3
The Agency for Digitisation, M. of F. D. (2020). Mandatory Digital Post from public authorities, eBoks. Retrieved May 1, 2020, from https://en.digst.dk/policy-and-strategy/mandatory-digitisation/digital-post/
Sartorius, N., & Kuyken, W. (1994). Translation of Health Status Instruments. In Quality of Life Assessment: International Perspectives (pp. 3–18). Berlin Heidelberg: Springer Berlin Heidelberg. https://doi.org/https://doi.org/10.1007/978-3-642-79123-9_1
Berg KC, Peterson CB, Frazier P, Crow SJ (2012) Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. The International journal of eating disorders 45(3):428–438. https://doi.org/10.1002/eat.20931
Carrozzino D, Vassend O, Bjørndal F, Pignolo C, Olsen LR, Bech P (2016) A clinimetric analysis of the Hopkins Symptom Checklist (SCL-90-R) in general population studies (Denmark, Norway, and Italy). Nord J Psychiatry 70(5):374–379. https://doi.org/10.3109/08039488.2016.1155235
Brunault FJ, Montaudon P, De Luca A, Hankard R, Ducluzeau PH, Ballon N (2019) Adulthood and childhood ADHD in patients consulting for obesity is associated with food addiction and binge eating, but not sleep apnea syndrome. Appetite 136:25–32. https://doi.org/10.1016/j.appet.2019.01.013
VanderBroek-Stice, L., Stojek, M. K., Beach, S. R., VanDellen, M. R., & MacKillop, J. (2017). Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite, 112, 59–68.
Rumpf HJ, Wohlert T, Freyer-Adam J, Grothues J, Bischof G (2013) Screening questionnaires for problem drinking in adolescents: Performance of AUDIT, AUDIT-C. CRAFFT and POSIT European Addiction Research 19(3):121–127. https://doi.org/10.1159/000342331
World Health Organization Geneva. (2007). Growth reference 5–19 years - BMI for age. Retrieved February 3, 2020, from https://www.who.int/growthref/who2007_bmi_for_age/en/
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scandinavian Journal of Public Health 39(7):30–33. https://doi.org/10.1177/1403494811401482
Munk-Jørgensen P, Østergaard SD (2011) Register-based studies of mental disorders. Scandinavian Journal of Public Health 39(7):170–174. https://doi.org/10.1177/1403494810390728
Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M (2017) Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol 46(3):798–798f. https://doi.org/10.1093/ije/dyw213
Barrett P (2007) Structural equation modelling: Adjudging model fit. Personality Individ Differ 42(5):815–824. https://doi.org/10.1016/j.paid.2006.09.018
Streiner DL (2003) Starting at the beginning: An introduction to coefficient alpha and internal consistency. J Pers Assess 80(1):99–103. https://doi.org/10.1207/S15327752JPA8001_18
Li C-H (2016) Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods 48(3):936–949. https://doi.org/10.3758/s13428-015-0619-7
Glynn N, A., & Quinn, K. (2010) An Introduction to the Augmented Inverse Propensity Weighted Estimator. Political Analysis. https://doi.org/10.1093/pan/mpp036
Kelley K, Preacher KJ (2012) On effect size. Psychol Methods 17(2):137–152. https://doi.org/10.1037/a0028086
Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2017). Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief, No. 288. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db288.pdf
Danish Health Authority. (2018). Forebyggelsespakke – Overvægt. (Lene Halmø Terkelsen, Ed.). Copenhagen, Denmark: Danish Health Authority. Retrieved September 24, 2020, from https://www.sst.dk/-/media/Udgivelser/2018/Forebyggelsespakker/Overvægt.ashx?la=da&hash=F191DE073B818B27B87236507E3B4011B95580DA
Danish Health Authority. (2017). Danskernes Sundhed - Den Nationale Sundhedsprofil 2017. Copenhagen, Denmark: Danish Health Authority. Retrieved September 24, 2020, from https://www.sst.dk/-/media/Udgivelser/2018/Den-Nationale-Sundhedsprofil-2017.ashx?la=da&hash=421C482AEDC718D3B4846FC5E2B0EED2725AF517
Abarca-Gómez, L., Abdeen, Z. A., Hamid, Z. A., Abu-Rmeileh, N. M., Acosta-Cazares, B., Acuin, C., … Ezzati, M. (2017). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. The Lancet, 390(10113), 2627–2642. https://doi.org/https://doi.org/10.1016/S0140-6736(17)32129-3
Crews F, He J, Hodge C (2007) Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav 86(2):189–199. https://doi.org/10.1016/j.pbb.2006.12.001
Gearhardt AN, Boswell RG, White MA (2014) The association of “food addiction” with disordered eating and body mass index. Eat Behav 15(3):427–433. https://doi.org/10.1016/j.eatbeh.2014.05.001
Burrows T, Kay-Lambkin F, Pursey K, Skinner J, Dayas C (2018) Food addiction and associations with mental health symptoms: a systematic review with meta-analysis. Journal of human nutrition and dietetics: the official journal of the British Dietetic Association 31(4):544–572. https://doi.org/10.1111/jhn.12532
Price, M., Higgs, S., & Lee, M. (2015). Self-reported eating traits: Underlying components of food responsivity and dietary restriction are positively related to BMI. Appetite, 95, 203–210.https://doi.org/10.1016/j.appet.2015.07.006
van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, Schoevers RA (2012) Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: A meta-analysis and meta-regression analysis. Drug Alcohol Depend 122(1–2):11–19. https://doi.org/10.1016/j.drugalcdep.2011.12.007
Hanć T, Cortese S (2018) Attention deficit/hyperactivity-disorder and obesity: A review and model of current hypotheses explaining their comorbidity. Neurosci Biobehav Rev 92:16–28. https://doi.org/10.1016/j.neubiorev.2018.05.017
Mies, G. W., Treur, J. L., Larsen, J. K., Halberstadt, J., Pasman, J. A., & Vink, J. M. (2017). The prevalence of food addiction in a large sample of adolescents and its association with addictive substances. Appetite, 118, 97–105.
Stommel M, Schoenborn CA (2009) Accuracy and usefulness of BMI measures based on self-reported weight and height: Findings from the NHANES & NHIS 2001–2006. BMC Public Health 9:421. https://doi.org/10.1186/1471-2458-9-421
Pursey K, Burrows TL, Stanwell P, Collins CE (2014) How accurate is web-based self-reported height, weight, and body mass index in young adults. Journal of Medical Internet Research 16(1):e4. https://doi.org/10.2196/jmir.2909
Acknowledgments
We thank Helle Jakobsen for statistical advice, and Dr. Christian Uggerby, MD for contributing to the translation of the YFAS-C 2.0.
Funding
This work is supported by grants from the Beckett Foundation (17-0-0822), the A.P Møller Foundation of Medical Science (17-L-0013) and the Heinrich Kopps Grant (all to CH), and a PhD fellowship from Aalborg University Hospital, Psychiatry (to CH). SDØ is supported by the Novo Nordisk Foundation (grant number: NNF20SA0062874), the Lundbeck Foundation (grant numbers: R358-2020-2341 and R344-2020-1073) and Independent Research Fund Denmark (grant number: 7016-00048B). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
The study was designed by CH, MBL and SDØ. The data was analyzed by CH and EF. Results were interpreted by CH, AGN, MBL and SDØ. The first version of this manuscript was drafted by CH and revised critically for important intellectual content by EF, ANG, MBL and SDØ. The final version of the manuscript was approved by all authors prior to submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The included adolescents were invited via their parents (legal guardians) to ensure, that the parents were informed on the purpose of the study. This procedure ensured, that the parents were able to decide whether their child should have the opportunity to participate in the survey, and that it was the parents who provided informed consent. The parents (and the adolescents) were informed that participation in the survey was voluntary and that the consent to participate could be withdrawn at any time. The study was therefore performed in accordance with the principles of the Declaration of Helsinki. The questionnaire and survey methodology were approved by the Danish Health Data Authority, and approval of the use of data from the Danish registers was granted by Statistics Denmark and the Danish Health Data Authority. In Denmark, ethical review board approval is not required for survey and register-based studies if they do not include collection of biological material. Data obtained from the survey and data from the Danish registers were de-identified by Statistics Denmark before being made available to the authors of this study. The project was registered with the Danish Data Protection Agency (record number 2008-58-0028).
Informed consent
The adolescents were invited via their parents (legal guardians) to ensure, that the parents were informed on the purpose of the study. This procedure ensured that the parents were able to decide whether their child should have the opportunity to participate in the survey. Furthermore, the invitees were informed, that survey participation was voluntary and that their consent to participate could be withdrawn at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Horsager, C., Færk, E., Gearhardt, A.N. et al. Validation of the dimensional Yale Food Addiction Scale for Children 2.0 and estimation of the weighted food addiction score in a sample of adolescents from the general population. Eat Weight Disord 26, 2563–2576 (2021). https://doi.org/10.1007/s40519-021-01113-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01113-8