Abstract
Purpose
Several studies evaluated the associations between specific beverages and cardio-metabolic risks among children. However, the evidence on the association between patterns of the beverage consumption and children’s anthropometric indices is rare. Therefore, this study was conducted to examine the association between Healthy Beverage Index (HBI) and anthropometric measures among 6-year-old girl children.
Methods
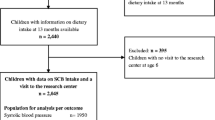
In this cross-sectional study, 788 children selected from health centers in Tehran, Iran. Data on beverage intake, socio-demographic, physical activity, and anthropometric characteristics were evaluated using reliable and validated standard protocols. The predefined HBI was calculated based on the previous research.
Results
After controlling for several confounders [mother age, mother body mass index, mother physical activity, socioeconomic status, children physical activity and energy intake, total oils (all kinds of oils like animal and plant oils), and total sweet foods (sweet foods except sweetened beverages)], being in the third compared to the first tertile of HBI among children was associated with increased odds of wasting (OR: 5.16; 95% CI 1.5–17.79) and underweight/wasting (OR: 1.81; 95% CI 1.07–3.07). Among the HBI components, just being in the third compared to the first tertile of high-fat milk was inversely associated with decreased odds of wasting (OR: 0.18; 95% CI 0.04–0.73).
Conclusions
The HBI among children was associated with higher odds of wasting and underweight/wasting. In addition, high-fat milk consumption decreased the odds of wasting among children. Further prospective studies need to confirm these results.
Level of evidence
Level V, descriptive cross-sectional study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) reported that childhood overweight and obesity are becoming more prevalent across the world and the worldwide prevalence of overweight/obesity in children living in developing countries is 12.9% for boys and 13.4% for girls [1]. According to a national study, in 2014, about 5.1 and 10.8 of Iranian children had overweight and obesity, respectively [2]. Childhood obesity has been shown to be a precursor to adult obesity, and subsequent adverse health outcomes (such as diabetes, cardiovascular diseases, dyslipidemia), disability, and even mortality [3, 4]. Therefore, this vital health issue requires immediate intervention. A combination of genetic, metabolic, and lifestyle factors are contributing to the etiology of obesity [5, 6]. Studies conducted in the Middle East regions reported that among all of the behavioral components, childhood obesity exhibited significant associations with physical inactivity, consumption of breakfast, vegetables and sugar-sweetened beverage (SSB) [7].
To date, extensive research has been done on the association between individual beverage consumption, particularly sugar-sweetened beverages, with overweight/obesity [8,9,10]. However, few publications have examined the overall quality of daily beverage consumption within a broader context of evaluating all consumed beverages as a pattern [11, 12]. Therefore, the HBI has been introduced as a holistic concept to evaluate the quality of overall beverage intake and its association with health-related outcomes in nutritional epidemiological studies [13]. This index included eight beverage categories, total beverage energy, and fluid consumption [14]. The cumulative effects of multiple beverages included in a holistic dietary index may provide better identification as the effect of a single beverage may be too small to be detectable [15]. Moreover, the HBI may have important public health implications since it can be implemented as a counseling tool to improve healthy beverage selection [15].
Some of the previous reviews showed that SSB consumption was associated with weight gain, overweight, and obesity [16, 17]; however, evidence from well-conducted meta-analyses provided inconsistent results regarding the association between SSB and weight status [18,19,20]. Data on the association between milk intake and children’s weight status are scarce and conflicting. While some studies have shown no association between milk intake with weight status and body fat mass [21], others have provided either an inverse [22, 23] or a positive association [24] in this regard. Some studies have shown a positive association between fruit juice consumption with adiposity gain [25] and short stature [26]. However, others have failed to provide an association between fruit juice consumption with over-weight [27], weight change [28], height [29] and anthropometric indices [26] among children. A previous publication has shown that both the amount and the types of beverages consumed can be influenced by heredity and environmental factors [30]. Beverages in Iran are commonly sweetened with sucrose, not high-fructose maize syrup as is the case in most western countries [31]. As high-fructose syrup in most beverages has been supposed to be a vital factor which might affect adiposity [32], findings from western studies might not be generalizable to other countries. Therefore, due to this geographical variation, our objective was to evaluate the association of the HBI with anthropometric measures among Iranian children.
Materials and methods
Study population
A total sample of 788 healthy children was recruited from those who attended public health centers in Southern Tehran, Iran. A cluster random sampling method was applied to select subjects who referred to ten health and treatment centers. Girls who were 6 years old who did not have the previous diagnosis of chronic or malignant diseases were eligible for inclusion in our study.
Dietary assessment and definition of HBI
Children’s usual dietary intakes were gathered via a face-to-face interview with their mothers using a 168-item semi-quantitative food frequency questionnaire (FFQ). The reliability and validity of the FFQ have been documented in previous research. Mothers were asked to report children’s portion sizes of consumed foods based on predefined categories (based on daily, weekly, or monthly frequency) during the preceding year. Household measures were then translated to grams. To compute average energy and nutrients intake, an adapted version of NUTRITIONIST IV that makes corrections for Iranian foods (version 7.0; N-Squared Computing, Salem, OR, USA) was used.
The HBI was calculated based on a method developed by Duffey and Davy [13]. Consumed beverages were grouped into eight categories including water, unsweetened coffee and tea, low-fat milk (< 1.5% fat, fat-free, and/or soy milk), diet drinks (including non-calorically sweetened coffee and tea and other artificially sweetened beverages), 100% fruit juice, alcohol (including beer, wine, and liquor), full-fat milk (1.5% fat), and sugar-sweetened beverages (including fruit drinks, sweetened coffee, and tea, soda) [13].
The final HBI score ranges between 0 and 100, with a higher value demonstrating better adherence to beverage guidelines and healthier beverage intake pattern [13]. However, as in the current study, diet drinks (ranging from 0 to 5 score) and alcohol (ranging from 0 to 5 score) were not consumed by our target population, the maximum final HBI score was 90. As the aim of the present study was to investigate adherence to healthy beverage intake guidelines, not total fluid consumption, liquids consumed as part of a food (such as soup) were not taken into account.
Anthropometric measurements
Anthropometric measures (body weight and height) were assessed and recorded by a trained assistant. Children’s weight was measured using a portable digital scale (SECA 753E; Seca, Hamburg, Germany) while they were in light and minimal clothing. To record height, children were instructed to stand comfortably against a wall and to keep their shoulders in a normal position. The measurement precision of weight and height were 0.1 kg, and 0.5 cm, respectively. BMI was computed as the participant’s body mass (kg) divided by stature squared (m2). Children were categorized into five groups based on their BMI for age (BAZ) using WHO cut-off point as follows: obese [BAZ ≥ 2 standard deviation (SD)], over-weight (BAZ ≥ 1SD), normal nutritional status (BAZ ≥ -1SD and < 1SD), underweight (BAZ < -1SD), and wasting (BAZ < -2SD) [33].
Socio-demographic and lifestyle variables
Applying a valid and reliable questionnaire, the socioeconomic status (SES) of each participant was estimated [34]. This scale allowed us to categorize participants according to answers they provided to several questions regarding occupation, academic attainment, vehicle ownership, owner occupancy, trendy household appliances, the number of people living in a single home, the number of rooms in the house, and domestic and international trips during the previous year. A demographic questionnaire with questions regarding mothers’ age and weight was completed for each participant. Both children and their mothers were asked to provide the average amount of time they spent on various inside- and outside-home activities during a day. Then to determine the level of physical activity (PA) for each participant, the registered amount of time for different activities was multiplied by their corresponding metabolic equivalent task value (MET-h/wk), and the final values were summed [35].
Statistical analysis
Statistical analyses were performed using SPSS software (version 23, SPSS Inc., Chicago, IL, USA) and p < 0.05 was set as statistically significant. Kolmogorov–Smirnov test was used for checking the normality of the data. A comparison of the continuous variables across tertiles of the Healthy Beverage Index was performed using analysis of variance (ANOVA) test. The analysis of covariance (ANCOVA) was used for estimating energy-adjusted children’s dietary intakes across tertiles of a Healthy Beverage Index. Multivariate logistic regression test was performed for assessing the associations between Healthy Beverage Index and its components and children anthropometric measures in three different models: crude model; model 1, adjusted for children’s energy intake, children’s physical activity, socioeconomic status; mother’s age, mother’s BMI and mother’s physical activity; model 2, adjusted for model 1 plus total oils (all kinds of oils like animal and plant oils) and total sweet foods (sweet foods except sweetened beverages).
Results
Participants’ characteristics across HBI are shown in Table 1. There was a significant association between BMI-for-age (p = 0.04) and HBI intake. The results for other variables were not significant.
Dietary intake of participants in each tertile of HBI are shown in Table 2. The dietary fat (p < 0.001), carbohydrate (p < 0.001), SFA (p < 0.001), total fiber (p = 0.001), some vitamins (A (p < 0.001), D (p < 0.001), K (p = 0.001), C (p < 0.001), B3 (p < 0.001), B9 (p < 0.001), and B12 (p < 0.001)), iron (p < 0.001), calcium (p < 0.001), magnesium (p < 0.001), and zinc (p < 0.001) decreased significantly across tertiles of HBI. In addition, participants in the highest tertile of HBI had significantly higher energy intake (p < 0.001).
Odds ratios (OR) and 95% confidence intervals (CI) for childhood wasting, underweight/wasting, obesity, and overweight/obesity are provided in Tables 3 and 4, respectively. After adjusting for several confounders in different models, participants in the highest compared to the lowest tertile of HBI had a higher risk of wasting (OR: 5.16; 95% CI 1.50–17.79) and underweight/wasting (OR: 1.81; 95% CI 1.07–3.07). Besides, compared to the lowest tertile, being in the highest tertile of high-fat dairy was associated with a lower risk of wasting (OR: 0.18; 95% CI 0.04–0.73).
Discussion
In the present study, a positive association was observed between The HBI and wasting and underweight/wasting. Further analysis showed that high-fat milk consumption was inversely associated with wasting.
The HBI was designed to evaluate overall beverage intake quality and to determine whether improvements in healthy beverage selection are associated with improvements in health-related outcomes [13]. It included eight beverage categories, total beverage energy, and fluid consumption [14]. The cumulative effects of multiple beverages included in a holistic dietary index may provide better identification as the effect of a single beverage may be too small to be detectable [15]. To date, few studies evaluated the association between the HBI and different outcomes [13]. In this study that was conducted to evaluate the association of HBI with cardiometabolic risk among US adults, a positive association was seen between higher the HBI scores and more favorable lipid profiles and hypertension risk [13]. In the present study, a positive association was observed between HBI and the risk of wasting and underweight/wasting. Decreased intake of macronutrients was observed at the highest level of adherence to the HBI in our study which might explain the casualty of these findings. Besides, high-fat milk consumption was inversely associated with wasting. These findings are consistent with a prospective study conducted by Braun et al. [36]. This study found that higher total dairy protein intake was associated with an increase in weight during 8-year follow-up among children in Netherlands [36]. In another study, Dubois et al. after a 5-year follow-up showed that milk consumption at 9 years was positively associated with positive BMI change from 9 to 14 years [37]. In contrast, DeBoer et al. did not see an association between milk consumption and BMI z score or weight-for-height z score [38]. It has been demonstrated that an increase in dietary calcium via its influence on circulating calcitropic hormones can lead to a decrease in the concentration of intracellular ionized calcium in human adipocytes. Following this decrement, the lipolysis and fat oxidation is stimulated [39]. On the other hand, high protein intake can stimulate insulin-like growth factor 1 (IGF-1) release and other growth hormones, which in turn enhances muscle and fat mass [40].
No association emerged between HBI and overweight and overweight/obesity. By contrast, a cross-sectional study on children and adolescents revealed that Canadian boys aged 6–11 years whose beverage pattern (included fruit drinks, regular soft drinks, sweetened coffees, and sweetened teas) was positively associated with odds of overweight and obesity [41]. A prospective study by Libuda et al. which was conducted on German children and adolescents (aged 9–18 years old) reported a positive association between energetic beverages with BMI standard deviation scores in girls, but not boys [11]. Moreover, a cross-sectional study which identified three beverage patterns among 19,800 Korean adults showed a negative relationship between alcoholic beverage pattern (included a high intake of alcoholic beverages and low intake of unsweetened coffee and tea, dairy products, and 100% fruit and vegetable juices) with both obesity and abdominal obesity. This study also showed a positive association between SSB pattern (included a high intake of sodas, sweetened coffee and tea, fruit drinks and sports/energy drinks) with abdominal obesity [42]. In line with our results, in the mentioned study, no association was observed between unsweetened beverage pattern (included a high intake of unsweetened coffee) with anthropometric measures [42].
In the current study, no association was observed between SSB and weight status. In line with our findings, a cross-sectional study did not show any association between SSB and weight status among U.S children of 2–5 years old [43]. A prospective study on 1203 children aged 5–7 years revealed no association between SSB at age 5–7 years and BMI at the age of 9 years [44]. Another cross-sectional study on Norwegian children (aged 8–14 years old) did not provide any association between sweetened soft drink and BMI [45]. Such associations were also replicated in studies conducted in other European countries [46, 47]. In this direction, several review studies have shown a weak association between SSB intake and weight outcomes [48, 49]. By contrast, a prospective study on U.S preschool children aged 3–5 years revealed that soda and all SSB intake were positively associated with BMI z scores at baseline of the study [50]. Moreover, in the mentioned study, fruit drinks, and all SSB intakes were associated with higher odds of overweight after 2 years of follow-up [50].
We found no association between fruit juice and weight status. In the study by Skinner et al. no significant association was shown between fruit juice intake (100% juice only) and children’s height and body mass index [29]. A prospective study which was conducted on children and adolescents showed that fruit and fruit juice intake (not determined) was not associated with significant changes in BMI z score during 3 years of follow-up [51]. It is noteworthy that a cross-sectional study by Faith et al. showed that higher fruit juice intake (not determined) was associated with increased adiposity among children (aged 1 to 4 years) who were initially overweight or at risk for overweight, but not normal-weight children [25]. Their findings were in line with recent evidence that the association between juice intake and weight gain is limited to overweight and obese children [52]. A reason why we failed to observe any association between fruit juice and weight status might be due to the overall normal weight of our participants.
The reason why we did not find any beverage-weight association contrary to previous studies might be attributable to several factors. Dietary fat intake has an important role as a dense source of energy and essential fatty acids like alpha-linolenic and linoleic acids, which have a critical role in growth and development [53]. Also, fat intake could facilitate the absorption of the fat-soluble vitamins needed in normal growth [54]. Dietary intake of protein is vital to the normal development of muscles and bones of children [55]. On the other side, carbohydrates function as an important and immediate source of daily activity energy and provide glucose needs for the brain [56]. As mentioned above, decreased intake of macronutrients was observed at the highest level of adherence to the HBI in our study, which might explain the casualty of this finding. Besides, it is well understood that the development of obesity and overweight or underweight weight status occurs because of a long-term energy imbalance. It is also well established that parents of overweight and obese children reported greater feeding restrictions than parents of healthy-weight children. Since many parents were employees, they do not have accurate information about their children’s food intake during the day. An unavoidable limitation of the study is the natural reporting errors that occur using an FFQ such as misclassification of data and that information that relies on correct reports by the mother.
To our knowledge, this is the first study conducted in children that addresses the relationships between HBI and anthropometric measures. The limited available research on this subject especially among children, due to the high prevalence of SSB consumption, and large sample size outline a few principle strengths of our current findings. First, the cross-sectional design of the study prevents us to draw conclusive associations between HBI and anthropometric status. Therefore, prospective studies are needed to evaluate these associations over longer periods. Second, since our study only included girls, we were not able to extrapolate our findings to both sexes. Third, in this study, dietary intake was assessed by taking FFQ from parents, which might lead to under- or over-reporting of food intake.
In conclusion, the findings of this study showed that HBI was positively associated with wasting and underweight/wasting, however, was not associated with other anthropometric measures. Also, this study showed that high-fat milk consumption was inversely associated with wasting. Future prospective studies are required to evaluate the association between HBI and anthropometric status in both genders, to characterize gender differences in the long period.
What is already known on this subject?
To date, several studies investigated the associations between specific beverages intake and risk of cardiovascular diseases and abnormal growth status among children with inconclusive results. Also, few studies performed on the associations between healthy and unhealthy beverages pattern and risk of diseases in this population. However, there is no study investigating the associations between the HBI, as a more comprehensive beverage index including approximately all of the healthy beverages in a diet, and growth status and obesity among this vulnerable group.
What does this study add?
Based on the results of the studies in adult population, it seems that higher adherence to the HBI is associated with more favorable metabolic profiles. However, our results showed that higher adherence to this index might be harmful for the children population because of potential nutrient deficiency following adherence to index that might lead to abnormal growth status in children. Therefore, it seems that the application of this dietary recommendation should be encouraged with caution in this population.
References
Mazidi M et al (2018) Prevalence of childhood and adolescent overweight and obesity in Asian countries: a systematic review and meta-analysis. AMS 14(6):1185. https://doi.org/10.5114/aoms.2018.79001
Kelishadi R et al (2014) Trend in the prevalence of obesity and overweight among Iranian children and adolescents: a systematic review and meta-analysis. Nutrition 30(4):393–400. https://doi.org/10.1016/j.nut.2013.08.011
Biro FM, Wien M (2010) Childhood obesity and adult morbidities. Am J Clin Nutr 91(5):1499S–1505S. https://doi.org/10.3945/ajcn.2010.28701B
Ferraro AA, Fernandes MTB (2013) Relationship between childhood growth and later outcomes, in recent advances in growth research: nutritional, molecular and endocrine perspectives. Karger Publishers, Basel, pp 191–197. https://doi.org/10.1159/000342615
Lytle LA (2009) Examining the etiology of childhood obesity: the IDEA study. Am J Community Psychol 44(3–4):338–349. https://doi.org/10.1007/s10464-009-9269-1
Philippas NG, Lo CW (2005) Childhood obesity: etiology, prevention, and treatment. Nutr Clin Care 8(2):77–88
Al-Hazzaa HM et al (2014) Prevalence of overweight, obesity, and abdominal obesity among urban Saudi adolescents: gender and regional variations. J Health Popul Nutr 32(4):634
Gui Z-H et al (2017) Sugar-sweetened beverage consumption and risks of obesity and hypertension in chinese children and adolescents: a national cross-sectional analysis. Nutrients 9(12):1302. https://doi.org/10.3390/nu9121302
Auerbach BJ et al (2017) Fruit juice and change in BMI: a meta-analysis. Pediatrics 139(4):e20162454. https://doi.org/10.1542/peds.2016-2454
Mirmiran P et al (2015) Consumption of sugar sweetened beverage is associated with incidence of metabolic syndrome in Tehranian children and adolescents. Nutr Metabol 12(1):25. https://doi.org/10.1186/s12986-015-0021-6
Libuda L et al (2008) Pattern of beverage consumption and long-term association with body-weight status in German adolescents–results from the DONALD study. Br J Nutr 99(6):1370–1379. https://doi.org/10.1017/S0007114507862362
LaRowe TL, Moeller SM, Adams AK (2007) Beverage patterns, diet quality, and body mass index of US preschool and school-aged children. J Am Diet Assoc 107(7):1124–1133. https://doi.org/10.1016/j.jada.2007.04.013
Duffey KJ, Davy BM (2015) The healthy beverage index is associated with reduced cardiometabolic risk in US adults: a preliminary analysis. J Acad Nutr Diet 115(10):1682–1689. https://doi.org/10.1016/j.jand.2015.05.005
Hedrick V et al (2015) Changes in the healthy beverage index in response to an intervention targeting a reduction in sugar-sweetened beverage consumption as compared to an intervention targeting improvements in physical activity: results from the talking health trial. Nutrients 7(12):10168–10178. https://doi.org/10.3390/nu7125525
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002
Lim S et al (2009) Obesity and sugar-sweetened beverages in African–American preschool children: a longitudinal study. Obesity 17(6):1262–1268. https://doi.org/10.1038/oby.2008.656
Ludwig DS, Peterson KE, Gortmaker SL (2001) Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 357(9255):505–508. https://doi.org/10.1016/S0140-6736(00)04041-1
Forshee RA, Anderson PA, Storey ML (2008) Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr 87(6):1662–1671. https://doi.org/10.1093/ajcn/87.6.1662
Malik VS et al (2013) Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 98(4):1084–1102. https://doi.org/10.3945/ajcn.113.058362
Keller A, Bucher Della Torre S (2015) Sugar-sweetened beverages and obesity among children and adolescents: a review of systematic literature reviews. Childhood Obes 11(4):338–346. https://doi.org/10.1089/chi.2014.0117
Venti CA, Tataranni PA, Salbe AD (2005) Lack of relationship between calcium intake and body size in an obesity-prone population. J Am Diet Assoc 105(9):1401–1407. https://doi.org/10.1016/j.jada.2005.06.004
Barba G et al (2005) Inverse association between body mass and frequency of milk consumption in children. Br J Nutr 93(1):15–19. https://doi.org/10.1079/BJN20041300
Skinner JD et al (2003) Longitudinal calcium intake is negatively related to children’s body fat indexes. J Am Diet Assoc 103(12):1626–1631. https://doi.org/10.1016/j.jada.2003.09.018
Berkey CS et al (2005) Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Arch Pediatr Adolesc Med 159(6):543–550. https://doi.org/10.1001/archpedi.159.6.543
Faith MS et al (2006) Fruit juice intake predicts increased adiposity gain in children from low-income families: weight status-by-environment interaction. Pediatrics 118(5):2066–2075. https://doi.org/10.1542/peds.2006-1117
Alexy U et al (1999) Fruit juice consumption and the prevalence of obesity and short stature in German preschool children: results of the DONALD study. J Pediatr Gastroenterol Nutr 29(3):343–349. https://doi.org/10.1097/00005176-199909000-00019
Skinner D, Carruth BR (2001) A longitudinal study of children’s juice intake and growth: the juice controversy revisited. J Am Diet Assoc 101(4):432–437. https://doi.org/10.1016/S0002-8223(01)00111-0
Newby P et al (2004) Beverage consumption is not associated with changes in weight and body mass index among low-income preschool children in North Dakota. J Am Diet Assoc 104(7):1086–1094. https://doi.org/10.1016/j.jada.2004.04.020
Skinner JD et al (1999) Fruit juice intake is not related to children’s growth. Pediatrics 103(1):58–64. https://doi.org/10.1542/peds.103.1.58
de Castro JM (1993) A twin study of genetic and environmental influences on the intake of fluids and beverages. Physiol Behav 54(4):677–687. https://doi.org/10.1016/0031-9384(93)90076-R
Kmietowicz Z (2012) Countries that use large amounts of high fructose corn syrup have higher rates of type 2 diabetes. BMJ 345:1. https://doi.org/10.1136/bmj.e7994
Jürgens H et al (2005) Consuming fructose-sweetened beverages increases body adiposity in mice. Obes Res 13(7):1146–1156. https://doi.org/10.1038/oby.2005.136
WHO (2006) WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. WHO, Geneva
Saraf-Bank S et al (2017) Adherence to Healthy Eating Index-2010 is inversely associated with metabolic syndrome and its features among Iranian adult women. Eur J Clin Nutr 71(3):425–430. https://doi.org/10.1038/ejcn.2016.173
Ainsworth BE et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9):S498–S504. https://doi.org/10.1097/00005768-200009001-00009
Braun KV et al (2016) Dietary intake of protein in early childhood is associated with growth trajectories between 1 and 9 years of age. J Nutr 146(11):2361–2367. https://doi.org/10.3945/jn.116.237164
Dubois L et al (2016) Dietary intake at 9 years and subsequent body mass index in adolescent boys and girls: a study of monozygotic twin pairs. Twin Res Hum Genet 19(1):47–59. https://doi.org/10.1017/thg.2015.97
DeBoer MD, Agard HE, Scharf RJ (2015) Milk intake, height and body mass index in preschool children. Arch Dis Child 100(5):460–465. https://doi.org/10.1136/archdischild-2014-306958
Zemel MBJL (2003) Role of dietary calcium and dairy products in modulating adiposity. Lipids 38(2):139–146. https://doi.org/10.1007/s11745-003-1044-6
Voortman T et al (2016) Protein intake in early childhood and body composition at the age of 6 years: the Generation R Study. Int J Obes 40(6):1018–1025. https://doi.org/10.1038/ijo.2016.29
Danyliw AD et al (2012) Beverage patterns among Canadian children and relationship to overweight and obesity. Appl Physiol Nutr Metabol 37(5):900–906. https://doi.org/10.1139/h2012-074
Lee KW, Shin D (2017) A healthy beverage consumption pattern is inversely associated with the risk of obesity and metabolic abnormalities in Korean adults. J Med Food 31(1):797.22. https://doi.org/10.1089/jmf.2017.0119
Mathias KC, Slining MM, Popkin BM (2013) Foods and beverages associated with higher intake of sugar-sweetened beverages. Am J Prev Med 44(4):351–357. https://doi.org/10.1016/j.amepre.2012.11.036
Johnson L, Mander AP, Jones LR, Emmett PM, Jebb SA (2007) Is sugar-sweetened beverage consumption associated with increased fatness in children? Nutrition. 23(7–8):557–563. https://doi.org/10.1016/j.nut.2007.05.005
Andersen LF et al (2005) Overweight and obesity among Norwegian schoolchildren: changes from 1993 to 2000. Scand J Public Health 33(2):99–106. https://doi.org/10.1080/140349404100410019172
Grandjean AC et al (2000) The effect of caffeinated, non-caffeinated, caloric and non-caloric beverages on hydration. J Am Coll Nutr 19(5):591–600. https://doi.org/10.1080/07315724.2000.10718956
Van Wymelbeke V et al (2004) Influence of repeated consumption of beverages containing sucrose or intense sweeteners on food intake. Eur J Clin Nutr 58(1):154. https://doi.org/10.1038/sj.ejcn.1601762
Harrington S (2008) The role of sugar-sweetened beverage consumption in adolescent obesity: a review of the literature. J School Nurs 24(1):3–12. https://doi.org/10.1177/10598405080240010201
Trumbo PR, Rivers CR (2014) Systematic review of the evidence for an association between sugar-sweetened beverage consumption and risk of obesity. Nutr Rev 72(9):566–574. https://doi.org/10.1111/nure.12128
DeBoer MD, Scharf RJ, Demmer RT (2013) Sugar-sweetened beverages and weight gain in 2- to 5-year-old children. Pediatrics 132(3):413–420. https://doi.org/10.1542/peds.2013-0570
Field AE et al (2003) Association between fruit and vegetable intake and change in body mass index among a large sample of children and adolescents in the United States. Int J Obes 27(7):821. https://doi.org/10.1038/sj.ijo.0802297
Welsh JA et al (2005) Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics 115(2):e223–e229. https://doi.org/10.1542/peds.2004-1148
EFSA Panel on Dietetic Products, N. and A.J.E. Journal (2010) Scientific Opinion on Dietary Reference Values for fats, including saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol. EFSA J 8(3):1461. https://doi.org/10.2903/j.efsa.2010.1461
Joint F (2010) Fats and fatty acids in human nutrition. Report of an expert consultation, 10–14 November 2008, Geneva
Bresson J-L et al (2008) Animal protein and bone growth-Scientific substantiation of a health claim related to animal protein and bone growth pursuant to Article 14 of Regulation (EC) No 1924/2006 [1]: scientific opinion of the panel on dietetic products. Nutr Allerg 6(11):858. https://doi.org/10.2903/j.efsa.2008.858
Stephen A et al (2012) The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur J Clin Nutr 66(7):765. https://doi.org/10.1038/ejcn.2012.27
Acknowledgements
The authors thank the subjects who participated in the study. This study was funded by the National Institute for Medical Research Development (Grant Number: 94-04-161-31112).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study ethically approved by National Institute for Medical Research Development of Tehran University of medical science, Tehran, Iran (IR. TUMS. VCR.REC.94-04-161-31 112).
Informed consent
Informed consent was obtained from each participant prior to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jalilpiran, Y., Mozaffari, H., Askari, M. et al. The association between Healthy Beverage Index and anthropometric measures among children: a cross-sectional study. Eat Weight Disord 26, 1437–1445 (2021). https://doi.org/10.1007/s40519-020-00954-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00954-z