Abstract
Purpose
Obesity is a multifactorial disease characterized by genetic, social, cultural and psychological factors. Currently, bariatric surgery represents the gold-standard intervention to treat morbid obesity in order to counteract associated disabling comorbidities. Several studies showed correlation between post-surgery weight loss and psychological factors. Also, the alexithymia may have a role in affecting post-surgery outcomes in bariatric patients, even if there are no studies investigating its role at 12-month follow-up. The purpose of the present study was to investigate the association between alexithymia and the postoperative weight loss 12 months after laparoscopic sleeve gastrectomy.
Methods
Seventy-five patients undergoing laparoscopic sleeve gastrectomy were enrolled. The Toronto Alexithymia Scale (TAS-20) was administered to patients. A postoperative weight loss check was performed at 3 and then 12 months after surgery.
Results
The TAS-20 total score was negatively correlated with the percent of excess weight loss (%EWL) at the 12-month follow-up (r = −0.24; p = 0.040). The analysis showed that non-alexithymic patients had a greater weight loss at 12 months after surgery compared to both probably alexithymics (71.88 ± 18.21 vs. 60.7 ± 12.5; p = 0.047) and probably alexithymic patients (71.88 ± 18.21 vs. 56 ± 22.8; p = 0.007). The preoperative BMI was a significant covariate [F(1,70) = 6.13 (p = 0.016)].
Conclusion
In the present study, the patients with higher preoperative BMI and identified as alexithymic showed lower %EWL at 12 months after laparoscopic sleeve gastrectomy. Findings point out the importance to take into consideration possible psychological treatments focused on improving emotional regulations of patients who are seeking bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays, the growing number of obese people in the Western world is recognized as one of the main concerns about health [1]. Obesity is a multifactorial disease characterized by genetic, social, cultural and psychological factors. Its complex nature requires a multidisciplinary intervention in order to guarantee the efficacy of the treatments. Currently, bariatric surgery represents the gold-standard intervention to treat morbid obesity [body mass index (BMI) >40 kg/m2] in terms of significant weight loss [2, 3] and resolution of comorbidities such as hypertension, type II diabetes, sleep apnea, dyslipidemia [4] as well as the improvement in quality of life [5]. The expected percent of excess weight loss (%EWL) after bariatric surgery is rated around 62 and 72%, respectively, at 1 and 2 years after surgery [6]. The literature shows that more than 30% of bariatric patients do not reach the expected weight loss and that about 20–30% of them re-gain substantial weight [7–9]. Several studies showed correlation between post-surgery weight loss or %EWL and personality disorders, eating disorders [10], psychiatric disorders, cognitive functions [11], adverse childhood experiences, mood disorders and anxiety disorders [12–14]. A recent study showed that also the alexithymia seems to have a role in affecting short-term post-surgery outcomes in bariatric patients [15]. The term alexithymia indicates the inability to identify and describe emotions, poor imagination, difficulty in differentiating between emotions and bodily sensations and concrete externally oriented thinking style [16]. As regards the relationship between obesity and alexithymia, studies are discordant. Elfhag and colleagues showed that obese patients had higher score on the Toronto Alexithymia Scale (TAS-20) compared to the control groups [17]; differently, Adami and colleagues did not find any significant differences between obese and non-obese patients [18]. Another study showed that only obese patients with psychopathological characteristics had significantly high score in TAS-20 questionnaire [19]. On the contrary, Da Ros and colleagues showed that a group of obese patients without diagnoses of binge eating disorder had higher scores in both TAS-20 and Beck Depression Inventory compared to the normal weight patients of the control group, highlighting that obese patients had both more depressive symptoms and difficulty in recognizing emotions [20]. A different study showed that the inability to communicate emotions in obese patients with an axis I (DSM-IV) diagnoses represents a negative predictor of weight loss during a behavioral weight loss program [21]. Another study found higher level of alexithymia in obese patients with binge eating compared to non-binge eating patients [22]. Coherently, Pinaguy et al. showed that alexithymia was a predictor of emotional eating in obese women with binge eating [23]. The emotional eating is the tendency to overeat in response to negative emotions [24], and it seems to be associated with the desire of eating in obese and binge eaters [25] and with lower weight loss after a non-surgical weight loss program in an obese sample [26].
The recent literature seems to show a general agreement on the role of the emotional dysregulation in individuals with obesity or eating disorder; however, the role of emotional dysregulation in the post-surgery outcome has been less investigated. Only a recent study showed that alexithymia is a predictor of weight loss at 6-month follow-up in obese patients underwent gastric bypass and that weight loss degree may affect quality of life [15]. Moreover, a higher BMI and an older age of the patients seem to be associated with a lower post-surgery weight loss [27, 28]. Today, there are no studies that tried to investigate the association between alexithymia and weight loss at 12-month follow-up in obese patients underwent laparoscopic sleeve gastrectomy.
The aim of the present study was to investigate the association between alexithymia and the postoperative weight loss after 3 and 12 months, also in relation to the preoperative age and BMI. The hypothesis was that alexithymic patients will show a lower %excess weight loss after surgery compared to non-alexithymic patients. Moreover, the role of the preoperative age and BMI as covariates will be tested.
Materials and methods
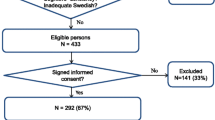
After local ethical committee approval, all patients underwent LSG from January to April 2015 were enrolled. Seventy-five patients (females n = 60, males n = 15) undergoing laparoscopic sleeve gastrectomy were selected in the final sample. The exclusion criteria were not being Italian citizenship, presence of psychiatric disorders and drugs/alcohol abuse evaluated through SCID I and II for DSM-IV [29–31], level of education less than 5 years. The presence of the exclusion criteria was evaluated during a preoperative psychological assessment consisting of three supportive sessions of 45 min each. The assessment was carried out by a trained clinical psychologist. The inclusion criteria were according to the European Guidelines on Metabolic and Bariatric Surgery [32] including age 18–65, BMI ≥40 kg/m2 or BMI 35–40 kg/m2 with comorbidities.
Informed consent was obtained by all individual patients included in the study.
In order to assess bariatric surgery outcomes, a postoperative interview was performed at 3 and then 12 months after surgery in order to collect post-surgery weight data.
The TAS-20 was administered. It is a self-administered questionnaire, consisting of 20 items. It measures three different dimensions defining alexithymia: difficulty in identifying emotions, difficulty in describing emotions and the externally oriented thinking as a measure of the tendency of individuals to focus their attention externally. Score analysis allows to identify alexithymic, not alexithymic and probably alexithymic patients [33]. The symptom checklist-90-R (SCL-90-R) was also administered [34]. The SCL-90-R is a 90-item self-reported symptom inventory oriented to measure levels of psychological symptoms. The SCL-90-R has nine primary symptom dimensions including somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism, and the Global Severity Index (GSI) that is used to describe the overall psychological distress level. The number of patients included in the study was based on previous results and a priori power analysis using G*Power 3.1.5. The sample size calculation was performed on the basis of the primary endpoint (%EWL) [35]. In a previous study, LSG patients with high %EWL (81 ± 18) reported significantly more “active coping” behavior prior to surgery than patients with moderate %EWL (49 ± 6) [36]. It was estimated that hypothesizing a prevalence of alexithymia by using TAS-20 in severely obese subjects of 17% [37], a minimum of 68 patients (total sample n) would be required to detect a difference of 15% in %EWL between alexithymic and no alexithymic patients (effect size d = 0.94) with a power of 85% assuming α = 0.05.
A correlation analysis between TAS-20 scores and the expected %EWL at 3 and 12 months after surgery was performed. The %EWL formula is: 100% × (preoperative weight − follow-up weight)/(preoperative weight − ideal body weight) [35]. Repeated-measures analysis (ANOVA, Fisher F) with post hoc tests was performed to check differences between alexithymic, no alexithymic and probably alexithymic patients on %EWL at 3 and 12 months after laparoscopic sleeve gastrectomy. A mathematical regression model was carried out with the variables that were significantly correlated with %EWL at 3 and 12 months. Statistical analysis was performed using the Statistica 10.0 software.
Results
The sample mean age was 40.8 (±6.12) with a range of 22–60 years. As regards the education level, 46.7% (n = 35) of bariatric patients had high school diploma, 45.3% (n = 34) had junior high school diploma and only 8% (n = 6) had a degree. The mean preoperative BMI and weight were, respectively, 41.89 kg/m2 (±5.54) and 116.8 kg (± 17.8).
There were no significant differences in gender distribution, age and preoperative BMI among alexithymic, probably alexithymic and no alexithymic patients (Table 1).
The TAS-20 total score was negatively correlated with the %EWL at the 12th month (r = −0.24; p = 0.040) as the preoperative BMI (r = −0.25; p = 0.030) (Table 2); moreover, the analysis showed a negative correlation between the difficulty in describing emotions scores and weight loss at 3 months after surgery (r = −0.25; p = 0.031) (Table 2). The regression model with TAS-20 total score and preoperative BMI as predictors on %EWL at 12 months as outcome was significant (adjusted R2 = 0.08; F(2,72) = 4.4; p = 0.016). The preoperative BMI was significantly associated with the %EWL at 12 months (beta = −0.23; t(72) = −2.0; p = 0.044), while the association between TAS-20 total score and %EWL at 12 months was at limit (beta = −0.21; t(72) = −1.9; p = 0.059). The regression model with difficulty in describing emotions scores as predictor on %EWL at 3 months was significant (adjusted R2 = 0.05; F(1,73) = 4.8; p = 0.031).
The ANOVA group (alexithymic, probably alexithymic, no alexithymic) per time (at 3 months, at 12 months) on %EWL showed an effect of group [F(2,72) = 3.27; p = 0.043] and time [F(1,72) = 126.77; p < 0.001] (Table 3); the ANCOVA, with age and preoperative BMI as covariates, maintained only the effect of time [F(1,70) = 9.73; p = 0.002] and revealed the effect of the covariate preoperative BMI [F(1,70) = 6.13 (p = 0.016)] (Table 3). Post hoc analysis did not show significant differences in weight loss between non-alexithymic and alexithymic subjects at 3 months after surgery, while non-alexithymic patients showed a greater weight loss at 12 months after surgery compared to both probably alexithymics (71.88 ± 18.21 vs. 60.7 ± 12.5 ; p = 0.047) and probably alexithymic patients (71.88 ± 18.21 vs. 56 ± 22.8; p = 0.007). There was no significant difference in weight loss at 12 months between probably alexithymics and alexithymic patients (p = 0.529) (Table 3).
The whole sample had a significantly greater excess weight loss 12 months compared to 3 months after surgery (68.4 ± 18.9 vs. 33.7 ± 13.9; p < 0.01) (Table 3).
Although the alexithymic patients showed a significantly higher impairment in all the nine subscales and the GSI of the SCL-90-R compared to the non-alexithymic patients (3.7 < F < 14.5; 0.000005 < p < 0.011), none of the SCL-90-R subscales was significantly correlated with the %EWL at 3 (−0.09 < r < 0.05; 0.395 < p < 0.965) and 12 months (−0.22 < r < 0.03; 0.055 < p < 0.776).
Discussion
The main finding of the present study was the significant difference among alexithymic, probably alexithymic and not alexithymic patients in terms of weight loss at 12 months after surgery. The results showed that alexithymic patients had significant lower weight loss than non-alexithymic subjects at 12-month follow-up. A significant negative association between the “difficulty in describing emotions” and weight loss at 3-month follow-up was found. The preoperative BMI was negatively associated with the percentage of excessive weight loss at 12 months after surgery. This finding was confirmed also by the effect of preoperative BMI as covariate in the multivariate analyses, where an higher preoperative BMI was associated with a poorer laparoscopic sleeve gastrectomy outcome. This finding is coherent with a recent study that showed an higher impact of obesity surgery in patients with a lower preoperative BMI [27]. In the present study, the predictive association between the alexithymia and the weight loss at 12 months became nonsignificant (p = 0.059) inserting the preoperative BMI as covariate, and it suggests to investigate their interaction more carefully in the future studies.
Alexithymic patients showed a general greater psychological impairment on all the SCL-90-R subscales compared to non-alexithymic patients; however, none of the SCL-90-R subscales was correlated with the weight loss at 3 and 12 months. In light of this finding, it seems that alexithymia has a specific role in eating habits of obese patients underwent bariatric surgery.
The findings of this study suggest that emotional difficulties may affect one-year outcomes of laparoscopic sleeve gastrectomy as showed by a six-month follow-up in obese patients who underwent gastric bypass [15].
Several studies have found high levels of alexithymia in obese population [17, 38–40]. Elfhag and Lundh (2007) found that the alexithymic obese patients ask more often for bariatric surgery treatment [17]. These patients specifically showed an inability in identifying and recognizing their emotions. Elfhag and Lundh (ibidem) also found the presence of significant differences between obese patients and the control group.
On the basis of our findings, it could be that alexithymic patients had lower weight loss than non-alexithymic patients because of their tendency to repeat past eating habits. This could have a negative impact on adherence to medical and dietetic recommendations. The association between alexithymia and adherence has been found in other clinical samples [41–44]. According to our interpretation, emotional difficulties have been previously associated with an excessive food intake that seems to improve the negative emotional status in obese patients [45, 46]. Similarly, Walfish et al. [47], in a pre-surgical sample, found that 40% of the bariatric patients were recognized as “emotional eaters” indicating the main role of negative emotional states in weight gain.
Findings of the present study highlighted an association between the inability in recognizing emotions and weight loss one year after surgery suggesting the importance to identify alexithymic patients in the preoperative bariatric assessment in order to prevent possible weight re-gain. A possible clinical strategy could be to plan supportive psychological interventions in order to promote patients ability in recognizing and regulating emotions and increasing adherence to the post-bariatric treatments [48].
The present study is not without limitations. The small sample could reduce the robustness of the data. Moreover, the effect of BMI as covariate in the comparison between %EWL of alexithymic and non-alexithymic patients suggests to replicate the study controlling more accurately the interaction of these two variables. Finally, the use of self-report measures could over- or underestimate own emotional ability due to social desirability.
Conclusion
In the present study, the patients with higher preoperative BMI and identified as alexithymic showed lower %EWL at 12 months after laparoscopic sleeve gastrectomy. This interesting result suggests that the preoperative BMI and the emotional regulation may have a role in eating habits in obese patients after bariatric surgery. Moreover, the “difficulty in describing emotions” was negatively associated with excess weight loss at 3 months suggesting a possible role of alexithymia also in the short-term postoperative period.
In light of these findings, the role of the BMI and of the emotional ability in bariatric surgery outcome could be further investigated in order to take into consideration possible psychological treatments focused on improving emotional regulations of patients who are seeking bariatric surgery.
References
James WP (2008) WHO recognition of the global obesity epidemic. Int J Obes 32:S120–S126. doi:10.1038/ijo.2008.247
Shi X, Karmali S, Sharma AM, Birch WD (2010) A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg 20(8):1171–1177. doi:10.1007/s11695-010-0145-8
Neovius M, Narbro K, Keating C, Peltonen M (2012) Health care use during 20 years following bariatric surgery. JAMA 308:1132–1141. doi:10.1001/2012
Sjöström L, Lindroos AK, Peltonen M et al (2004) Swedish obese study scientific group: lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351:2683–2693. doi:10.1056/NEJMoa035622
Nadalini L, Zenti MG, Masotto L et al (2014) Improved Quality of Life after bariatric surgery in morbidly obese patients. Interdisciplinary group of bariatric surgery of Verona (G.I.C.O.V.). G Chir 35(7–8):161–164. doi:10.11138/gchir/2014.35.7.161
Lee SY, Lim CH, Pasupathy S, Poopalalingam R, Tham KW, Ganguly S, Wai CHD, Wong WK (2011) Laparoscopic sleeve gastrectomy: a novel procedure for weight loss. Singapore Med J 52(11):794
Andersen JR, Aadland E, Nilsen RM, Våge V (2014) Predictors of weight loss are different in men and women after sleeve gastrectomy. Obes Surg 24(4):594–598. doi:10.1007/s11695-013-1124-7
Balsiger BM, Murr MM, Poggio JL et al (2000) Bariatric surgery. Surgery for weight control in patients with morbid obesity. Med Clin N Am 84:477–489. doi:10.1016/S0025-7125(05)70232-7
Courcoulas AP, Christian NJ, Belle SH et al (2013) Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 310:2416–2425. doi:10.1001/jama.2013.280928
Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, Ko CY, Maggard Gibbons M (2012) Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg 22(1):70–89. doi:10.1007/s11695-011-0472-4
Wimmelmann CL, Dela F, Mortensen EL (2013) Psychological predictors of weight loss after bariatric surgery: a review of the recent research. Obes Res Clin Pract 8(4):299–313. doi:10.1016/j.orcp.2013.09.003
Semanscin-Doerr DA, Windover A, Ashton K, Heinberg LJ (2010) Mood disorders in laparoscopic sleeve gastrectomy patients: does it affect early weight loss? Surg Obes Relat Dis 6(2):191–196. doi:10.1016/j.soard.2009.11.017
Kinzl JF, Schrattenecker M, Traweger C, Mattesich M, Fiala M, Biebl W (2006) Psychosocial predictors of weight lost after bariatric surgery. Obes Surg 16(12):1609–1614. doi:10.1381/096089206779319301
Van Hout GC, Verschure SK, van Heck GL (2005) Psychosocial predictors of success following bariatric surgery. Obes Surg 15(4):552–560. doi:10.1381/0960892053723484
Lai C, Aceto P, Petrucci I, Castelnuovo G, Callari C, Giustacchini P, Sollazzi L, Mingrone G, Bellantone R, Raffaelli M (2016) The influence of preoperative psychological factors on weight loss after bariatric surgery: a preliminary report. J Health Psychol. doi:10.1177/135910531677750
Sifneos PE (1996) Alexithymia: past and present. Am J Psychiatry 153(7):137–142. doi:10.1176/ajp.153.7.137
Elfhag K, Lundh L (2007) TAS-20 alexithymia in obesity, and its links to personality. Scand J Psychol 48:391–398. doi:10.1111/j.1467-9450.2007.00583
Adami GF, Campostano A, Ravera G, Leggieri M, Scopinaro N (2001) Alexithymia and body weight in obese patients. Behav Med 27:121–126. doi:10.1080/08964280109595778
Morosin A, Riva G (1997) Alexithymia in a clinical sample of obese women. Psychol Rep 80(2):387–394. doi:10.2466/pr0.1997.80.2.387
Da Ros A, Vinai P, Gentile N, Forza G, Cardetti S (2011) Evaluation of alexithymia and depression in severe obese patients not affected by eating disorders. Eating Weight Disord 16(1):24–29. doi:10.1007/BF03327517
De Panfilis C, Cero S, Dall’Aglio E, Salvatore P, Torre M, Maggini C (2007) Psychopathological predictors of compliance and outcome in weight-loss obesity treatment. Acta Biomed 78(1):22–28
Pinna F, Lai L, Pirarba S, Orrù W, Velluzzi F, Loviselli A, Carpiniello B (2011) Obesity, alexithymia and psychopathology: a case-control study. Eat Weight Disord 16(3):e164–e170. doi:10.3275/7509
Pinaquy S, Chabrol H, Simon C, Louvet JP, Barbe P (2003) Emotional eating, alexithymia, and binge eating disorder in obese women. Obes Res 11(2):195–201. doi:10.1038/oby.2003.31
VanStrien T, Cebolla A, Etchemendy E, Gutie ́rrez-Maldonado J, Ferrer-Garc ́ıa M, Botella C, Ban ̃os R (2013) Emotional eating and food intake after sadness and joy. Appetite 66:20–25. doi:10.1016/j.appet.2013.02.016
Zeeck A, Stelzer N, Linster HW, Joos A Hartmann A (2011) Emotion and eating in binge eating disorder and obesity. Eur Eat Disorder Rev 19(5):426–437. doi:10.1002/erv.1066
Braden A, Flatt SW, Boutelle KN, Strong D, Sherwood NE, Rock CL (2016) Emotional eating is associated with weight loss success among adults enrolled in a weight loss program. J Behav Med 39(4):727–732. doi:10.1007/s10865-016-9728-8
Ochner CN, Jochner M, Caruso EA, Teixeira J, Xavier Pi-Sunyer F (2013) Effect of preoperative body mass index on weight loss following obesity surgery. Surg Obes Relat Dis 9(3):423–427. doi:10.1016/j.soard.2012.12.009
Contreras JE, Santander C, Court I, Bravo J (2013) Correlation between age and weight loss after bariatric surgery. Obes Surg 23(8):1286–1289. doi:10.1007/s11695-013-0905-3
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn, Text Revised (DSM-IV-TR). American Psychiatric Association, Washington, DC
First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS (1997) User’s guide for structured clinical interview for DSM-IV axis II personality disorders (SCID-II). American Psychiatric Association, Washington, DC
First MB, Spitzer RL, Gibbon M, Williams JB (1995) Structured clinical interview for DSM-IV axis I disorders. New York State Psychiatric Institute, New York
Fried M,. Yumuk V, Oppert JM, Scopinaro N, Torres A, Weiner R, Yashkov Y, Frühbeck G (2014) Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg 24:42–55. doi:10.1007/s11695-013-1079-8
Bagby MR, Parker JDA, Taylor GJ (1994) The twenty-item Toronto Alexithymia scale. Item selection and cross-validation of the factor structure. J Psychosom Res 38(1):23–32. doi:10.1016/0022-3999(94)90005-1
Derogatis LR, Unger R (2010) Symptom checklist-90-revised. In: Corsini encyclopedia of psychology, vol 1–2. Wiley, Hoboken. doi:10.1002/9780470479216.corpsy0970
Scinta W (2012) Measuring success: a comparison of weight loss calculations. BT 9(7):18–20. doi:10.1016/0022-3999(94)90005-1
Figura A, Ahnis A, Stengel A, Hofmann T, Elbelt U, Ordemann J, Rose M (2015) Determinants of weight loss following laparoscopic sleeve gastrectomy: the role of psychological burden, coping style, and motivation to undergo surgery. J Obes. doi:10.1155/2015/626010
De Zwaan M, Bach M, Mitchell JE, Ackard D, Specker SM, Pyle RL, Pakesh G (1995) Alexithymia, obesity, and binge eating disorder. Int J Eat Disord 17(2):135–140. doi:10.1002/1098-108X(199503)17:2<135::AID-EAT2260170205>3.0.CO;2-7
Legorreta G, Bull RH, Kiely M (1988) Alexithymia and symbolic function in the obese. Psychother Psychosom 50:88–94. doi:10.1159/000288105
Marechal V, Loas G, Legrand A, Corcos M (2009) Alexithymia in severely obese patients seeking surgical treatment. Psychol Rep 105:935–944. doi:10.2466/PR0.105.3.935-944
Aceto P, Lai C, Perilli V, Sacco T, Modesti C, Raffaelli M, Sollazzi L (2016) Factors affecting acute pain perception and analgesics consumption in patients undergoing bariatric surgery. Physiol Behav 163:1–6. doi:10.1016/j.physbeh.2016.04.032
Calia R, Lai C, Aceto P, Luciani M, Camardese G, Lai S, Fantozzi C, Pietroni V, Salerno MP, Spagnoletti G, Pedroso JA, Romagnoli J, Citterio F (2015) Emotional self-efficacy and alexithymia may affect compliance, renal function and quality of life in kidney transplant recipients: results from a preliminary cross-sectional study. Physiol Behav 142:152–154. doi:10.1016/j.physbeh.2015.02.018
Calia R, Lai C, Aceto P, Luciani M, Saraceni C, Avolio AW, Agnes S (2011) Psychological risk factors for graft rejection among liver transplant recipients. Transpl Proc 43(4):1123–1127. doi:10.1016/j.transproceed.2011.01.159
Calia R, Lai C, Aceto P, Luciani M, Saraceni C, Lai S, Gargiulo A, Citterio F (2011) Preoperative psychological factors predicting graft rejection in patients undergoing kidney transplant: a pilot study. Transpl Proc 43(4):1006–1009. doi:10.1016/j.transproceed.2011.01.158
Lai C, Aceto P, Luciani M, Fazzari E, Cesari V, Luciano S, Fortini A, Berloco D, Canulla F, Calia R, Lai S (2016) Externally oriented thinking predicts phosphorus levels in dialyzed patients. Transpl Proc 48(2):309–310. doi:10.1016/j.transproceed.2015.12.056
Zijlstraa H, Van Middendorpb T, Devaereb L, Larsenc JK, Van Ramshorstd B, Geenen R (2012) Emotion processing and regulation in women with morbid obesity who apply for bariatric surgery. Psychol Health 27(12):1375–1387. doi:10.1080/08870446.2011.600761
Dingemans AE, Martijn C, Jansen AT, Van Furth EF (2009) The effect of suppressing negative emotions on eating behavior in binge eating disorder. Appetite 52:51–57. doi:10.1016/j.appet.2008.08.004
Walfish S (2004) Self-assessed emotional factors contributing to increased weight gain in pre-surgical bariatric patients. Obes Surg 14:1402–1405. doi:10.1381/0960892042583897
Lumley MA (2004) Alexithymia, emotional disclosure, and health: a program of research. J Pers 72:1271–1300. doi:10.1111/j.1467-6494.2004.00297
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Emanuela Paone, Laura Pierro, Angela Damico, Paola Aceto, Fabio Cesare Campanile, Gianfranco Silecchia, Carlo Lai declare that no funding source is involved in this study.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual patients included in the study.
Rights and permissions
About this article
Cite this article
Paone, E., Pierro, L., Damico, A. et al. Alexithymia and weight loss in obese patients underwent laparoscopic sleeve gastrectomy. Eat Weight Disord 24, 129–134 (2019). https://doi.org/10.1007/s40519-017-0381-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-017-0381-1