Abstract
Purpose of Review
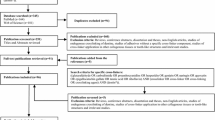
This paper reviews the complexity of the composition of dentin, and the repercussions of this composition on the stability of dentin over time, particularly in relation to adhesive dental procedures.
Recent Findings
Dentin is a complex and dynamic structure that comprises the major part of the tooth. Most adhesive procedures in dentistry involve bonding to dentin. The hybrid layer (HL) created on the very variable and dynamic organic dentin phase may fail over time, leading to the failure of dental restorations. Literature showed that the collagen fibers in the HL are prone to hydrolysis and mechanical strain, as well as endogenous proteolytic activity (collagenolytic activity of matrix metalloproteinases and cysteine cathepsins). Hydrolysis of the resin phase of the HL also occurs over time.
Summary
Advancements in the area of dental adhesion have been huge. Silencing of collagenolytic enzymes (protease inhibitors and cross-linking agents) is one of the main strategies to decrease the degradation of the HL. In the following years, new techniques will also probably be available, and efficacy of some of the available techniques will perhaps be further clarified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The major part of the tooth is comprised of dentin, a mineralized connective tissue that shows similarities with bone in terms of formation and composition. Dentin is a complex and dynamic structure. During the process of dentinogenesis, dentin extracellular organic matrix (ECM) is pivotal for the mineral phase formation since precipitation of the inorganic phase occurs on the formed collagen network [1]. More precisely, the intermolecular spaces between collagen fibrils are filled with tightly bound and evenly distributed water molecules [2]. With the progression of the mineralization process, minerals gradually replace the water molecules [3].
Adhesive procedures in dentistry, apart from a low percentage of cases, involve bonding to dentin. Adhesion on dentin is a type of in situ tissue engineering, where the collagen scaffold is enveloped in adhesive resin, creating the so-called hybrid layer (HL) [4]. The goal of adhesive procedures is to keep this bond stable for several years. However, despite the advances in dental materials, the HL created on the variable and dynamic organic dentin phase may fail over time [5, 6]. The weakening of resin-dentin bonds can lead to the failure of dental restorations [7] and, consequently, to high costs of dental restoration replacements [8].
This paper reviews the complexity of the composition of dentin and the repercussions of this composition on the stability of dentin over time, particularly in relation to adhesive dental procedures.
Dentin As a Substrate: Composition and Morphology
Human dentin is composed of approximately 70 w% inorganic material, 18 w% organic material, and 12 w% water. However, the volume percentage goes in favor of organic material and water, with up to 70% being attributed to these two components (30–50% organic, 20% water) [9]. Various factors, such as the location and condition of the dentin (presence of caries, demineralization), can significantly change the composition of dentin, which has profound implications in the mechanical properties of dentin, as well as in the success rate of the adhesive procedures [10].
As 45% of the sound dentinal tissue consists of the organic matrix [11], with the main component being type I collagen fibrils and proteoglycans and the minor component being other non-collagenous proteins (dentin sialoproteins, phosphoproteins, bone morphogenic proteins, and insulin-like growth factors 1 and 2), it is of great importance to understand its three-dimensional arrangement. This understanding could in fact clarify bonding mechanisms and the interaction between collagen fibrils and adhesive resin monomers. Transmission electron microscopy, field-emission scanning electron microscopy, and atomic force microscopy studies showed that the organic matrix is a complex network of fibrillar and globular structures. Mineral is further precipitated onto these structures during dentinogenesis, using it as a scaffold [12, 13].
The dentin ECM consists of an intricate network of fibrils (approximately 70–90 nm in diameter), with type I collagen fibrils representing the pillar of the structure, connected by branching of non-collagenous proteins (20–40 nm diameter) [13,14,15]. The main portion of the non-collagenous proteins in dentin matrix consists of proteoglycans and phosphoproteins [16,17,18], with the proteoglycans being considered as fundamental in the stabilization of the collagen fibrillar alignment [16, 18]. Proteoglycans are polyanions rich in carbohydrates with a high molecular weight (11,000–220,000 kD) [18]. These proteins have the ability to fill space and bind and organize water molecules, and could play a role in the organization of the three-dimensional appearance of the dentin organic matrix [19,20,21,22]. Furthermore, proteoglycans may determine the collagen water affinity and regulate water substitution during HL formation. Owing to the advances in reagent purification and the production of highly specific monoclonal antibodies, nowadays collagen [23] and proteoglycans [24] can be analyzed using precise and sensitive selective immune-labeling protocols [25]. During this double immunolabeling procedure, secondary antibodies are conjugated with gold particles of different sizes [26], allowing clarification of the three-dimensional relationships between the different molecules.
It has been shown that the application of phosphoric acid for 15 s exposes collagen fibrils without damaging their structural integrity [23, 24, 26]. On the other hand, the application of phosphoric acid to the dentin surface for more than 15 s caused weakening of the labeling index in collagen fibrils [23] and proteoglycans [19, 21]. This is probably an indication that structural changes occur within collagen or proteoglycans when exposed to prolonged acid etching. Since the introduction of structurally changed collagen or proteoglycans into the HL could jeopardize its stability, over-etching should be avoided [23].
Dentin Bonding Agents and Adhesion Strategies
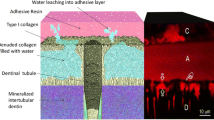
The goal of dentin bonding is to produce a homogenous and compact HL by impregnating the dentin substrate with the blends of resin monomers, which would in turn lead to durable tooth restorations. Resin monomers themselves cannot infiltrate mineralized dentin, hence the dentin surface must be previously treated with acidic agents [27]. Two different strategies can currently be employed in the bonding procedures: the etch-and-rinse technique (E&R) and the self-etch technique (SE) [Fig. 1].
FEISEM micrographs of an (a) E&R and (b) SE adhesive system. Bonded interfaces were created with Scotchbond 1 (3M ESPE) and Protect Bond (Kuraray) in deep dentin tissue. HLs were then exposed with a slow speed diamond saw and dentin was dissolved by sequential rinses in hydrochloric acid and sodium hypochlorite to reveal resin penetration. Resin tags are clearly detectable in the E&R adhesive systems (a) since they infiltrated dentin tubules funneled by the etching agent. SE adhesives often infiltrate no further than the smear layer and smear plugs, revealing a more homogenous morphology that is devoid of long resin tags. Reprinted from Breschi et al. [28•], with permission. FEISEM field emission in-lens scanning electron microscopy, E&R etch and rinse technique, SE self-etch technique, HL hybrid layer
In the E&R strategy, the adhesive systems remove the smear layer from the dentinal substrate and demineralize it through the process of etching. The main prerequisite for the achievement of stable bonds in this mode is full impregnation of the etched substrate by the adhesive blends. However, within this mode, the monomer diffusion within the acid-etched dentin has shown a decreasing gradient [29], with incompletely infiltrated zones noted along the bottom of the HL. Hence, this area contains denuded collagen fibrils [29,30,31]. This has been further confirmed by immunohistochemical labeling after staining with anti-type I collagen antibodies (Fig 2) [32]. The investigated E&R systems displayed weaker labeling on the superficial part of the HL, while intense labeling of collagen fibrils was found in the deepest parts of the HL (Fig. 2). These results indicate that the adhesive resin enveloped collagen fibrils in the superficial part of the HL, whereas denuded fibrils were present in the deeper areas due to the lack of penetration of the adhesives [32].
FEISEM images of the dentin-SB interface after immunohistochemical labeling of collagen with a monoclonal antibody. (a) FEISEM secondary electron image after applying phosphoric acid and SB. The typical HL (between white arrows), RTs, and PA infiltration formed by total etching systems are clearly visible. (b) FEISEM mixed image of secondary and back-scattered electrons. Intense labeling is detectable on the HL. The deeper areas of the HL appear to be specially labeled (arrows) compared with the superficial HL. (c) FEISEM mixed image of secondary and back-scattered electrons. The PA infiltrated by the resin agent reveals some labeling (arrows) at the base of the resin tag, then very weak labeling present entering the lumen of the tubule. (d) FEISEM mixed image of secondary and back-scattered electrons. The RT reveals almost no gold labeling on the surface. Reprinted from Breschi et al. [32], with permission. FEISEM field emission in-lens scanning electron microscopy, SB single bond, HL hybrid layer, RT resin tag, PA peritubular area
In the SE mode, the smear layer is maintained as the substrate for bonding. In this approach, the adhesive co-monomers simultaneously demineralize and infiltrate the dentinal substrate, and the stability of the bonding depends on the effectiveness of the coupling between the substrate and the co-monomers. This approach was also investigated using immunolabeling, showing, in contrast to the E&R adhesive, that the two-step SE adhesives express uniform weak labeling throughout the depth of the HL [32], allowing to hypothesize that collagen is more protected if SE adhesives are used to hybridize dentin.
It can be assumed that the collagen fibrils that are not enveloped in resin can be more prone to enzyme degradation and hydrolysis, given that free and loosely bound water from the internal and external water compartments of collagen fibrils cannot be completely replaced either by the E&R or SE bonding approaches [33].
Factors that can influence the longevity of the HL can be physical, such as the temperature changes within the oral cavity which produce expansion and contraction stresses, as well as the occlusal chewing forces [28,35,•, 34–36]. Chemical factors, such as acidic agents in food and beverages, dentinal fluid, saliva, and bacterial products, can affect the stability of the interface, and can lead to elution of resin monomers [37,38,39] and degradation of resin components [35,41,42,, 40–43], as well as degradation of the unprotected collagen fibrils [28•, 30, 35, 40, 44, 45]. Since the purpose of this review is the stability of dentin, the focus will be mainly on the degradation of the collagen fibrils, while the degradation patterns of the adhesive resin will be shortly addressed.
Degradation of the Adhesive Resin
In order to prevent the collapse of collagen fibrils after acid etching, the water-wet bonding technique, which entails keeping dentin fully hydrated during bonding, was established in the 1990s [46]. As adhesives contain hydrophobic resin monomers, two-hydroxyethyl methacrylate (HEMA) was incorporated into many adhesive systems. Moreover, many manufacturers incorporated hydrophilic and acidic resin monomers into adhesives, aiming to improve the wetting properties of adhesives to dentin [47]. This led to a substantial improvement of immediate bonding. However, the longevity of resin-dentin bonds seems to be compromised when these systems are used [48, 49].
Degradation of the HL involves the processes of hydrolysis and leaching of the resin [50,51,52]. The hydrophilic domains remain poorly polymerized and, consequently, water penetrates these week parts of the HL, which further facilitates leaching. The water movement and leaching continue along the HL, forming relatively large water channels [28•]. A larger amount of collagen matrix is exposed, leaving it susceptible to endogenous proteolytic activity [53•, 54].
Degradation of the Collagen Fibrils
As previously reported, it is difficult to achieve complete coverage of the collagen fibrils by passive monomer infiltration, which can leave them vulnerable to hydrolytic degradation. Loss of resin from the interfibrillar spaces and disorganization of fibrils have in fact been revealed as degradation patterns within the HL [30].
Pashley et al. [53•] presented the first evidence of intrinsic collagenolytic activity in human non-carious mineralized dentin. This pioneer study showed that degradation of the collagen matrices would occur in artificial saliva after 250 days, even in aseptic conditions. The authors hypothesized that matrix metalloproteinases (MMPs), previously found to be expressed in the dentin-pulp complex [55,56,57], could be responsible for this degradation. Their conclusion was based on the fact that the groups stored in artificial saliva with the addition of proteolytic enzyme inhibitors, or in pure mineral oil, were statistically significantly more preserved after storage time.
MMPs are endogenous Zn2+- and Ca2+-dependent enzymes. Dayan et al. [58] were the first to report dentinal collagenolytic activity, while Tjäderhane et al. [55] showed that this activity was attributable to the MMPs. In recent years, the presence of the gelatinases MMP-2 and -9, collagenase MMP-8, stromelysin MMP-3, and MMP-20 has been reported [56,60,61,62,63,64,65,, 59–66].
During the secretion of the dentin matrix, odontoblasts produce the MMPs [67], which supposedly play a role in dentin formation. The proforms of the MMPs remain inactive in the mineralized collagen matrix [68] but can be activated when re-exposed during the dentin caries process, and subsequently participate in disintegration of the dentin matrix. Hence, it can be hypothesized that these enzymes are directly involved in degradation of the HL [69,70,71].
This hypothesis was supported by the studies of Mazzoni et al. [72] and Nishitani et al. [73], which showed collagenolytic and gelatinolytic activity in dentin treated with the E&R and SE modes. Further studies confirmed these initial results using specific MMP-2 and -9 assays [70, 74], and additional clarification was provided by an in situ zymographic assay technique [75•, 76]. This method confirmed the hypothesis that the collagen fibrils at the bottom of the HL are not completely infiltrated by adhesive resin since enzymatic activity was noted in this area (Fig. 3).
(a, b) Three-dimensional model of the acquired image. (a) The intense fluorescence, meaning gelatin hydrolysis, throughout the entire extension of hybrid layer. (b) Higher magnification image model shows gelatinolytic activity inside dentinal tubules, shown as cylindrical tubes, in deep dentin. The high tubule density reveals this to be very deep dentin. Reprinted from Mazzoni et al. [75•], with permission. R resin composite, HL hybrid layer, D dentin
Cysteine cathepsins are another class of proteases more recently found in dentin [77, 78]. Cathepsins have been shown to participate in caries progression, as well as in degradation of the ECM alongside MMPs, leading to failure of adhesive restorations over time [4, 28•, 78, 79].
How to Improve Bond Stability and Maintain the Integrity of the Dentin Substrate?
As the preservation of the HL over time can be affected by hydrolytic degradation of the suboptimally polymerized hydrophilic resins and/or degradation of the collagen matrices by MMPs and cysteine cathepsins [28•], several approaches can be used to prevent HL degradation. One of the most efficient methods could be the use of MMP inhibitors. Those investigated in the literature include chlorhexidine (CHX) [4,81,, 80–82], quaternary ammonium methacrylates (QAMs), and benzalkonium chloride (BAC) [83, 84]. Furthermore, collagen cross-linkers were shown to inactivate MMPs and consequently improve the durability of dentin bonding [85]. Apart from the abovementioned, several other clinical approaches have been found to be useful in the preservation of the HL, including dentin remineralization and ethanol-wet bonding [4, 86].
Protease Inhibitors
The most commonly used and most investigated protease inhibitor to date is chlorhexidine, a powerful antimicrobial agent, shown to effectively inhibit MMP-2, -8, and -9 [87], as well as cysteine cathepsins [88]. Numerous in vivo and in vitro studies have demonstrated chlorhexidine-related preservation of the structural integrity of the collagen matrix within the HL, as well as a decreased reduction of bond strength over time [69,90,91,92,93,94,95,96,97,, 80, 89–98]. Another MMP inhibitor is galardin, a collagen-like synthetic structure that binds to the active sites of MMP-1, -2, -8, and -9. A study by Breschi et al. showed lower MMP expression in the zymographic assay, as well as a lower level of nanoleakage after 1 year of aging [81]. Galardin has the ability to inhibit MMP activity in concentrations 10–100 times lower compared with chlorhexidine [81].
Quaternary ammonium compounds are cationic at physiological pH, are efficient antimicrobial agents, and may also inhibit dentinal MMP activity. Due to their antimicrobial properties, polymerizable QAMs, particularly 12-methacryloyloxydodecylpyridinium bromide (MDPB) have previously been incorporated into SE primers [99, 100]. In vitro and clinical experiments have also indicated that QAMs may inhibit collagenolytic enzymes in the HL [101, 102].
Another cationic surface-acting agent with a quaternary ammonium group is BAC, a mixture of alkylbenzyldimethylammonium chlorides of various alkyl chains. It is used as an antimicrobial agent and surfactant [84]. This agent has recently come to the attention of investigators in the area of HL preservation and has shown good immediate results [84, 103] and promising long-term results [104, 105].
Furthermore, broad-spectrum antibiotics, such as the tetracyclines doxycycline and minocycline, have cationic properties and were shown to effectively inhibit MMPs [106,107,108]. The effect of these inhibitors on the durability of resin-dentin bonds should be further investigated. Moreover, bisphosphonates have the ability to inhibit proteases due to their chelating properties [109]. Tezvergil-Mutluay et al. showed strong inhibition of MMP-9 using polyvinylphosphonic acid (PVPA) [110]. The influence of this potent protease inhibitor group should be further investigated.
Collagen Cross-Linking Agents
Collagen cross-linking agents could inactivate the active sites of dentinal proteases as they form stable cross-links of the collagen fibrils [111, 112]. This presents an advantage over protease inhibitors, which may leach out of the HL within 18–24 months [40,114,115,116,117,118,, 113–119]. Until now, several cross-linking agents have been investigated: glutaraldehyde, proanthrocyanidin and genipin [120], riboflavin [121], as well as tannic acid [122] and carbodiimide [85]. All of the investigated agents seem to enhance the mechanical and structural stability of dentin collagen.
Among these, 1-Ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC), in particular, has been shown to reduce dentin collagen degradation and prevent degradation of the HL over time [76, 85, 123]. It has low cytotoxicity and the ability to change negatively charged ionized carboxyl groups into positively charged amides and reduce the molecular mobility of the active sites of the proteases, which could inactivate dentin proteases. Moreover, EDC can induce cross-linking of collagen [123], which in turn could prevent ‘unwinding’ of the collagen peptides by the MMPs [124] and therefore inhibit the functional activity of MMPs [4, 27, 28•, 125]. This cross-linking agent was recently investigated [126] and it was shown that the application of 0.3M EDC pretreatment with the two investigated E&R adhesives can prevent degradation of the HL. Furthermore, the same authors investigated the effect of EDC pretreatment, applied with two E&R adhesives, on the inactivation of MMPs using a zymographic assay and an in situ zymographic assay [76]. The application of the adhesives without pretreatment activated dentin MMP, while EDC pretreatment lead to almost complete inactivation.
Other Approaches
As mentioned earlier, residual water in the HL can result in matrix porosity and incomplete infiltration of hydrophobic monomers. In order to avoid this, ethanol-wet bonding with hydrophobic E&R systems has been proposed [127]. When a water-saturated collagen matrix is pretreated with 100% ethanol, matrix water is removed and the infiltration of hydrophobic monomers into the dentin matrix is facilitated. Using this approach, a relatively homogenous distribution of hydrophobic resin has been shown within the HL [128, 129]. Yet another concept to consider is biomimetic remineralization, indeed an interesting approach that uses nanotechnology in order to mimic natural biomineralization [130]. In an in vitro study, specimen slabs were immersed in a medium containing dissolved biomimetic analogs and remineralization occurred by means of lateral diffusion mechanism. This concept has not yet become clinically applicable.
Conclusions
Currently available dental adhesive systems seem to be quite efficient in terms of immediate bond retention and sealing of the bonded interfaces. However, long-term maintenance of these results was shown to be a very difficult task. The main mechanisms leading to degradation of the HL are hydrolysis and degradation by host-derived enzymes. Water sorption, promoted by the hydrophilic formulations of the new adhesives, causes slow hydrolysis of the resin. On the other hand, the endogenous MMPs and cysteine cathepsins, activated during the bonding procedures, degrade the resin uninfiltrated collagen fibrils in the bottom of the HL. Hence, it seems that the key to long-term preservation of resin-dentin bonds lies in the complete replacement of water within the collagen water compartments, as well as inactivation/inhibition of the dentinal endogenous enzymes. Advancements in the area of dental adhesion have been massive. The proposed strategies to address the issue of the durability of the HL showed promising results in in vitro studies, while some have also been established in in vivo studies. In the following years, new techniques will also probably be available, and efficacy of some of the available techniques will perhaps be further clarified.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Orsini G, Ruggeri Jr A, Mazzoni A, Nato F, Manzoli L, Putignano A, et al. A review of the nature, role, and function of dentin non-collagenous proteins. Part 1: proteoglycans and glycoproteins. Endod Top. 2009;21:1–18.
Bella J, Brodsky B, Berman HM. Hydration structure of a collagen peptide. Structure. 2017;3:893–906.
Tjäderhane L, Haapasalo M. The dentin–pulp border: a dynamic interface between hard and soft tissues. Endod Top. 2009;20:52–84.
Liu Y, Tjäderhane L, Breschi L, Mazzoni A, Li N, Mao J, et al. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J Dent Res. 2011;90:953–68.
Sano H. Microtensile testing, nanoleakage, and biodegradation of resin-dentin bonds. J Dent Res. 2006;85:11–4.
Spencer P, Ye Q, Park J, Topp EM, Misra A, Marangos O, et al. Adhesive/dentin interface: the weak link in the composite restoration. Ann Biomed Eng. 2010;38:1989–2003.
Amaral FLB, Colucci V, Palma-Dibb RG, Corona SAM. Assessment of in vitro methods used to promote adhesive interface degradation: a critical review. J Esthet Restor Dent. 2007;19:340–53.
Jokstad S, Blunck U, Tyas M, Wilson NAB. Quality of dental restorations. FDI Commission Project 2-95. Int Dent J. 2001;51:117–58.
Tjäderhane L, Carrilho MR, Breschi L, Tay FR, Pashley DH. Dentin basic structure and composition-an overview. Endod Top. 2009;20:3–29.
Carvalho RM, Tjäderhane L, Manso AP, Carrilho MR, Carvalho CAR. Dentin as a bonding substrate. Endod Top. 2012;21:62–88.
Kinney JH, Marshall Jr GW, Marshall SJ, Hohling H-J, Wiesmann UP, Arends J, et al. Three-dimensional mapping of mineral densities in carious dentin: theory and method. Scanning Microsc. 1994;8:197–205.
Perdigão J, Lambrechts P, Van Meerbeek B, Tomé ÂR, Vanherle G, Lopes AB. Morphological field emission-SEM study of the effect of six phosphoric acid etching agents on human dentin. Dent Mater. 1996;12:262–71.
Van Meerbeek B, Vargas M, Inque S, Yoshida Y, Perdigão J, Lambrechts P, et al. Microscopy investigations. Techniques, results, limitations. Am J Dent. 2000;13:3D–18.
Lin CP, Douglas WH, Erlandsen SL. Scanning electron microscopy of type I collagen at the dentin-enamel junction of human teeth. J Histochem Cytochem. 1993;41:381–8.
Breschi L, Gobbi P, Mazzotti G, Ellis T, Sacher E, Stangel I. A field emission SEM study of enamel and dentin. Biomed Mater Res. 1999;46:315–23.
Cheng H, Caterson B, Yamauchi M. Identification and immunolocalization of chondroitin sulfate proteoglycans in tooth cementum. Connect Tissue Res. 1999;40:37–47.
Marshall GW, Marshall SJ, Kinney JH, Balooch M. The dentin substrate: structure and properties related to bonding. J Dent. 1997;25:441–58.
Goldberg M, Takagi M. Dentine proteoglycans: composition, ultrastructure and functions. Histochem J. 1993;25:781–806.
Scott JE. Proteoglycan-fibrillar collagen interactions. Biochem J. 1988;252:313–23.
Vogel KG, Paulsson M, Heinegård D. Specific inhibition of type I and type II collagen fibrillogenesis by the small proteoglycan of tendon. Biochem J. 1984;223:587–97.
Hedbom E, Heinegård D. Binding of fibromodulin and decorin to separate sites on fibrillar collagens. J Biol Chem. 1993;268:27307–12.
Oyarzún A, Rathkamp H, Dreyer E. Immunohistochemical and ultrastructural evaluation of the effects of phosphoric acid etching on dentin proteoglycans. Eur J Oral Sci. 2000;108:546–54.
Breschi L, Perdigão J, Gobbi P, Mazzotti G, Falconi M, Lopes M. Immunocytochemical identification of type I collagen in acid-etched dentin. J Biomed Mater Res A. 2003;66:764–9.
Breschi L, Lopes M, Gobbi P, Mazzotti G, Falconi M, Perdigão J. Dentin proteoglycans: an immunocytochemical FEISEM study. J Biomed Mater Res. 2002;61:40–6.
Tay FR, Pashley DH, Yoshiyama M. Two modes of nanoleakage expression in single-step adhesives. J Dent Res. 2002;81:472–6.
Breschi L, Gobbi P, Lopes M, Prati C, Falconi M, Teti G, et al. Immunocytochemical analysis of dentin: a double-labeling technique. J Biomed Mater Res A. 2003;67:11–7.
Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol ILS, Geraldeli S, et al. Optimizing dentin bond durability: control of collagen degradation by matrix metalloproteinases and cysteine cathepsins. Dent Mater. 2013;29:116–35.
Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. This manuscript critically discusses and gives valuable and detailed information related to formation, aging and stability of resin bonding.
Wang Y, Spencer P. Quantifying adhesive penetration in adhesive/dentin interface using confocal Raman microspectroscopy. J Biomed Mater Res. 2002;59:46–55.
Hashimoto M, Ohno H, Sano H, Kaga M, Oguchi H. In vitro degradation of resin-dentin bonds analyzed by microtensile bond test, scanning and transmission electron microscopy. Biomaterials. 2003;24:3795–803.
Armstrong SR, Keller JC, Boyer DB. The influence of water storage and C-factor on the dentin-resin composite microtensile bond strength and debond pathway utilizing a filled and unfilled adhesive resin. Dent Mater. 2001;17:268–76.
Breschi L, Prati C, Gobbi P, Pashley D, Mazzotti G, Teti G, et al. Immunohistochemical analysis of collagen fibrils within the hybrid layer: a FEISEM study. Oper Dent. 2004;29:538–46.
Kim YK, Gu L, Bryan TE, Kim JR, Chen L, Liu Y, et al. Mineralisation of reconstituted collagen using polyvinylphosphonic acid/polyacrylic acid templating matrix protein analogues in the presence of calcium, phosphate and hydroxyl ions. Biomaterials. 2010;31:6618–27.
De Munck J, Van Meerbeek B, Van Landuyt K, Lambrechts P. Influence of a shock absorbing layer on the fatigue resistance of a dentin–biomaterial interface. Eur J Oral Sci. 2005;113:1–6.
Tay FR, Pashley DH. Have dentin adhesives become too hydrophilic? J Can Dent Assoc. 2003;69:726–31.
De Munck J, Braem M, Wevers M, Yoshida Y, Inoue S, Suzuki K, et al. Micro-rotary fatigue of tooth–biomaterial interfaces. Biomaterials. 2005;26:1145–53.
Eick JD, Gwinnett AJ, Pashley DH, Robinson SJ. Current concepts on adhesion to dentin. Crit Rev Oral Biol Med. 1997;8:306–35.
Cadenaro M, Antoniolli F, Sauro S, Tay FR, Di Lenarda R, Prati C, et al. Degree of conversion and permeability of dental adhesives. Eur J Oral Sci. 2005;113:525–30.
Cadenaro M, Breschi L, Antoniolli F, Mazzoni A, Di Lenarda R. Influence of whitening on the degree of conversion of dental adhesives on dentin. Eur J Oral Sci. 2006;114:257–62.
Hashimoto M, Ohno H, Kaga M, Endo K, Sano H, Oguchi H. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res. 2000;79:1385–91.
De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84:118–32.
Santerre JP, Shajii L, Leung BW. Relation of dental composite formulations to their degradation and the release of hydrolyzed polymeric-resin-derived products. Crit Rev Oral Biol Med. 2001;12:136–51.
Jaffer F, Finer Y, Santerre JP. Interactions between resin monomers and commercial composite resins with human saliva derived esterases. Biomaterials. 2002;23:1707–19.
Hashimoto M, Ohno H, Sano H, Tay F, Kaga M, Kudou Y, et al. Micromorphological changes in resin–dentin bonds after 1 year of water storage. J Biomed Mater Res. 2002;63:306–11.
Hashimoto M, Tay FR, Ohno H, Sano H, Kaga M, Yiu C, et al. SEM and TEM analysis of water degradation of human dentinal collagen. J Biomed Mater Res. 2003;66:287–98.
Kanca J. Improving bond strength through acid etching of dentin and bonding to wet dentin surfaces. J Am Dent Assoc. 1992;123:35–43.
Marshall SJ, Bayne SC, Baier R, Tomsia AP, Marshall GW. A review of adhesion science. Dent Mater. 2010;26:e11–6.
Malacarne J, Carvalho RM, de Goes MF, Svizero N, Pashley DH, Tay FR, et al. Water sorption/solubility of dental adhesive resins. Dent Mater. 2006;22:973–80.
Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B. Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent Mater. 2005;21:864–81.
Hashimoto M. A review: micromorphological evidence of degradation in resin-dentin bonds and potential preventional solutions. J Biomed Mater Res Part B Appl Biomater. 2010;92:268–80.
Wang Y, Spencer P. Hybridization efficiency of the adhesive/dentin interface with wet bonding. J Dent Res. 2003;82:141–5.
Kermanshahi S, Santerre JP, Cvitkovitch DG, Finer Y. Biodegradation of resin-dentin interfaces increases bacterial microleakage. J Dent Res. 2010;89:996–1001.
Pashley D, Tay F, Yiu C, Hashimoto M, Breschi L, Carvalho R. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216–21. This manuscript represents the first study to highlight endogenous enzymes as responsible for dentinal collagen degradation over time.
Armstrong SRE, Vargas MA, Chung I, Pashley DH, Campbell JA, Laffoon JE, et al. Resin-dentin interfacial ultrastructure and microtensile dentin bond strength after five-year water storage. Oper Dent. 2004;29:705–12.
Tjäderhane L, Larjava H, Sorsa T, Uitto V-J, Larmas M, Salo T. The activation and function of host matrix metalloproteinases in dentin matrix breakdown in caries lesions. J Dent Res. 1998;77:1622–9.
Sulkala M, Larmas M, Sorsa T, Salo T, Tjäderhane L. The localization of matrix metalloproteinase-20 (MMP-20, enamelysin) in mature human teeth. J Dent Res. 2002;81:603–7.
Lee W, Aitken S, Sodek J, McCulloch CAG. Evidence of a direct relationship between neutrophil collagenase activity and periodontal tissue destruction in vivo: role of active enzyme in human periodontitis. J Periodontal Res. 1995;30:23–33.
Dayan D, Binderman I, Mechanic GL. A preliminary study of activation of collagenase in carious human dentine matrix. Arch Oral Biol. 1983;28:185–7.
Mazzoni A, Mannello F, Tay FR, Tonti GA, Papa S, Mazzotti G, et al. Zymographic analysis and characterization of MMP-2 and -9 forms in human sound dentin. J Dent Res. 2007;86:436–40.
Mazzoni A, Papa V, Nato F, Carrilho M, Tjäderhane L, Ruggeri A, et al. Immunohistochemical and biochemical assay of MMP-3 in human dentine. J Dent. 2011;39:231–7.
Santos J, Carrilho M, Tervahartiala T, Sorsa T, Breschi L, Mazzoni A, et al. Determination of matrix metalloproteinases in human radicular dentin. J Endod. 2009;35:686–9.
Sulkala M, Tervahartiala T, Sorsa T, Larmas M, Salo T, Tjäderhane L. Matrix metalloproteinase-8 (MMP-8) is the major collagenase in human dentin. Arch Oral Biol. 2007;52:121–7.
Martin-De Las Heras S, Valenzuela A, Overall C. The matrix metalloproteinase gelatinase A in human dentine. Arch Oral Biol. 2000;45:757–65.
Mazzoni A, Pashley DH, Tay FR, Gobbi P, Orsini G, Ruggeri A, et al. Immunohistochemical identification of MMP-2 and MMP-9 in human dentin: correlative FEI-SEM/TEM analysis. J Biomed Mater Res Part A. 2009;88:697–703.
Boushell LW, Nagaoka H, Nagaoka H, Yamauchi M. Increased matrix metalloproteinase-2 and bone sialoprotein response to human coronal caries. Caries Res. 2011;45:453–9.
Boukpessi T, Menashi S, Camoin L, TenCate JM, Goldberg M, Chaussain-Miller C. The effect of stromelysin-1 (MMP-3) on non-collagenous extracellular matrix proteins of demineralized dentin and the adhesive properties of restorative resins. Biomaterials. 2008;29:4367–73.
Palosaari H, Pennington C, Larmas M, Tjäderhane L, Salo T. Expression profile of matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs in mature human odontoblasts and pulp tissue. Eur J Oral Sci. 2003;111:117–27.
Hannas AR, Pereira JC, Granjeiro JM, Tjäderhane L, Hannas AR, Pereira JC, et al. The role of matrix metalloproteinases in the oral environment. Acta Odontol Scand. 2007;65:1–13.
Carrilho M, Geraldeli S, Tay F, de Goes M, Carvalho R, Tjäderhane L. In vivo preservation of hybrid layer by chlorhexidine. J Dent Res. 2007;86:529–33.
Mazzoni A, Scaffa P, Carrilho M, Tjäderhane L, Di Lenarda R, Polimeni A, et al. Effects of etch-and-rinse and self-etch adhesives on dentin MMP-2 and MMP-9. J Dent Res. 2013;92:82–6.
Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol ILS, Geraldeli S, et al. Strategies to prevent hydrolytic degradation of the hybrid layer: a review. Dent Mater. 2013;29:999–1011.
Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjäderhane L, et al. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials. 2006;27:4470–6.
Nishitani Y, Yoshiyama M, Wadgaonkar B, Breschi L, Mannello F, Mazzoni A, et al. Activation of gelatinolytic/collagenolytic activity in dentin by selfetching adhesives. Eur J Oral Sci. 2006;114:160–6.
Mazzoni A, Carrilho M, Papa V, Tjäderhane L, Gobbi P, Nucci C, et al. MMP-2 assay within the hybrid layer created by a two-step etch-and-rinse adhesive: biochemical and immunohistochemical analysis. J Dent. 2011;39:470–7.
Mazzoni A, Nascimento F, Carrilho M, Tersariol I, Papa V, Tjäderhane L, et al. MMP activity in the hybrid layer detected with in situ zymography. J Dent Res. 2012;91:467–72. In this manuscript, a novel and valuable method for the analysis of MMPs activity was introduced.
Mazzoni A, Apolonio FM, Saboia VPA, Santi S, Angeloni V, Checchi V, et al. Carbodiimide inactivation of MMPs and effect on dentin bonding. J Dent Res. 2014;93:263–8.
Tersariol IL, Geraldeli S, Minciotti CL, Nascimento FD, Pääkkönen V, Martins MT, et al. Cysteine cathepsins in human dentin-pulp complex. J Endod. 2010;36:475–81.
Nascimento FD, Minciotti CL, Geraldeli S, Carrilho MR, Pashley DH, Tay FR, et al. Cysteine cathepsins in human carious dentin. J Dent Res. 2011;90:506–11.
Vidal CMP, Tjäderhane L, Scaffa PM, Tersariol IL, Pashley D, Nader HB, et al. Abundance of MMPs and cysteine cathepsins in caries-affected dentin. J Dent Res. 2014;93:269–74.
Breschi L, Mazzoni A, Nato F, Carrilho M, Tjäderhane L, Ruggeri Jr A, et al. Chlorhexidine stabilizes the adhesive interface: a 2 year in vitro study. Dent Mater. 2010;26:1–12.
Breschi L, Martin P, Mazzoni A, Nato F, Carrilho M, Tjäderhane L, et al. Use of a specific MMP-inhibitor (galardin) for preservation of hybrid layer. Dent Mater. 2010;26:571–8.
Almahdy A, Koller G, Sauro S, Bartsch JW, Sherriff M, Watson TF, et al. Effects of MMP inhibitors incorporated within dental adhesives. J Dent Res. 2012;91:605–11.
Tezvergil-Mutluay A, Agee KA, Uchiyama T, Imazato S, Mutluay MM, Cadenaro M, et al. The inhibitory effects of quaternary ammonium methacrylates on soluble and matrix-bound MMPs. J Dent Res. 2011;90:535–40.
Tezvergil-Mutluay A, Mutluay MM, Gu LS, Zhang K, Agee KA, Carvalho RM, et al. The anti-MMP activity of benzalkonium chloride. J Dent. 2011;39:57–64.
Bedran-Russo AKB, Vidal CMP, Dos Santos PH, Castellan CS. Long-term effect of carbodiimide on dentin matrix and resin-dentin bonds. J Biomed Mater Res Part B Appl Biomater. 2010;94:250–5.
Tay FR, Pashley DH. Biomimetic remineralization of resin-bonded acid-etched dentin. J Dent Res. 2009;88:719–24.
Gendron R, Grenier D, Sorsa T, Mayrand D. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol. 1999;6:437–9.
Scaffa PMC, Vidal CMP, Barros N, Gesteira TF, Carmona AK, Breschi L, et al. Chlorhexidine inhibits the activity of dental cysteine cathepsins. J Dent Res. 2012;91:420–5.
Breschi L, Cammelli F, Visintini E, Mazzoni A, Carrilho M, Cadenaro M, et al. Influence of chlorhexidine concentration on the durability of etch-and-rinse dentin bonds: a 12-month in vitro study. J Adhes Dent. 2009;11:191–8.
Campos EA, Correr GM, Leonardi DP, Barato-Filho F, Gonzaga CC, Zielak JC. Chlorhexidine diminishes the loss of bond strength over time under simulated pulpal pressure and thermo-mechanical stressing. J Dent. 2009;37:108–14.
Loguercio AD, Hass V, Gutierrez MF, Luque-Martinez IV, Szezs A, Stanislawczuk R, et al. Five-year effects of chlorhexidine on the in vitro durability of resin/dentin interfaces. J Adhes Dent. 2016;18:35–43.
Zheng P, Zaruba M, Attin T, Wiegand A. Effect of different matrix metalloproteinase inhibitors on microtensile bond strength of an etch-and-rinse and a self-etching adhesive to dentin. Oper Dent. 2014;40:80–6.
Stanislawczuk R, Pereira F, Muñoz MA, Luque I, Farago PV, Reis A, et al. Effects of chlorhexidine-containing adhesives on the durability of resin-dentine interfaces. J Dent. 2014;42:39–47.
Carrilho MRO, Carvalho RM, de Goes MF, di Hipólito V, Geraldeli S, Tay FR, et al. Chlorhexidine preserves dentin bond in vitro. J Dent Res. 2007;86:90–4.
Brackett MG, Tay FR, Brackett WW, Dib A, Dipp FA, Mai S, et al. In vivo chlorhexidine stabilization of hybrid layers of an acetone-based dentin adhesive. Oper Dent. 2009;34:379–83.
Mobarak EH. Effect of chlorhexidine pretreatment on bond strength durability of caries-affected dentin over 2-year aging in artificial saliva and under simulated intrapulpal pressure. Oper Dent. 2011;36:649–60.
Leitune VCB, Portella FF, Bohn PV, Collares FM, Samuel SMW. Influence of chlorhexidine application on longitudinal adhesive bond strength in deciduous teeth. Braz Oral Res. 2011;25:388–92.
Yiu CKY, Hiraishi N, Tay FR, King NM. Effect of chlorhexidine incorporation into dental adhesive resin on durability of resin-dentin bond. J Adhes Dent. 2012;14:355–62.
Imazato S, Kinomoto Y, Tarumi H, Ebisu S, Tay FR. Antibacterial activity and bonding characteristics of an adhesive resin containing antibacterial monomer MDPB. Dent Mater. 2017;19:313–9.
Imazato S, Tay FR, Kaneshiro AV, Takahashi Y, Ebisu S. An in vivo evaluation of bonding ability of comprehensive antibacterial adhesive system incorporating MDPB. Dent Mater. 2017;23:170–6.
Tezvergil-Mutluay A, Agee KA, Mazzoni A, Carvalho RM, Carrilho M, Tersariol IL, et al. Can quaternary ammonium methacrylates inhibit matrix MMPs and cathepsins? Dent Mater. 2017;31:e25–32.
Pashley D, Tay F, Imazato S. How to increase the durability of resin-dentin bonds. Compend Contin Educ Dent. 2011;32:60–4.
Kanca III J. One step bond strength to enamel and dentin. Am J Dent. 1997;10:5–8.
Sabatini C, Patel SK. Matrix metalloproteinase inhibitory properties of benzalkonium chloride stabilizes adhesive interfaces. Eur J Oral Sci. 2013;121:610–6.
Sabatini C, Ortiz PA, Pashley DH. Preservation of resin-dentin interfaces treated with benzalkonium chloride adhesive blends. Eur J Oral Sci. 2015;123:108–15.
Sulkala M, Wahlgren J, Larmas M, Sorsa T, Teronen O, Salo T, et al. The effects of MMP inhibitors on human salivary MMP activity and caries progression in rats. J Dent Res. 2001;80:1545–9.
Lauhio A, Salo T, Tjäderhane L, Lähdevirta J, Golub L, Sorsa T. Tetracyclines in treatment of rheumatoid arthritis. Lancet. 2017;346:645–6.
Sorsa T, Tjäderhane L, Konttinen YT, Lauhio A, Salo T, Lee H, et al. Matrix metalloproteinases: contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann Med. 2006;38:306–21.
Heikkilä P, Teronen O, Moilanen M, Konttinen YT, Hanemaaijer R, Laitinen M, et al. Bisphosphonates inhibit stromelysin-1 (MMP-3), matrix metalloelastase (MMP-12), collagenase-3 (MMP-13) and enamelysin (MMP-20), but not urokinase-type plasminogen activator, and diminish invasion and migration of human malignant and endothelial cell lines. Anticancer Drugs. 2002;13:245–54.
Tezvergil-Mutluay A, Agee KA, Hoshika T, Tay FR, Pashley DH. The inhibitory effect of polyvinylphosphonic acid on functional matrix metalloproteinase activities in human demineralized dentin. Acta Biomater. 2010;6:4136–42.
Bedran-Russo AKB, Pashley DH, Agee K, Drummond JL, Miescke KJ. Changes in stiffness of demineralized dentin following application of collagen crosslinkers. J Biomed Mater Res Part B Appl Biomater. 2008;86:330–4.
Xu C, Wang Y. Cross-linked demineralized dentin maintains its mechanical stability when challenged by bacterial collagenase. J Biomed Mater Res Part B Appl Biomater. 2011;96(B):242–8.
De Munck J, Mine A, den Steen PE, Van Landuyt KL, Poitevin A, Opdenakker G, et al. Enzymatic degradation of adhesive–dentin interfaces produced by mild self-etch adhesives. Eur J Oral Sci. 2010;118:494–501.
Donmez N, Belli S, Pashley DH, Tay FR. Ultrastructural correlates of in vivo/in vitro bond degradation in self-etch adhesives. J Dent Res. 2005;84:355–9.
Sadek FT, Braga RR, Muench A, Liu Y, Pashley DH, Tay FR. Ethanol wet-bonding challenges current anti-degradation strategy. J Dent Res. 2010;89:1499–504.
Komori PCP, Pashley DH, Tjäderhane L, Breschi L, Mazzoni A, de Goes MF, et al. Effect of 2% chlorhexidine digluconate on the bond strength to normal versus caries-affected dentin. Oper Dent. 2009;34:157–65.
Griffiths BM, Watson TF, Sherriff M. The influence of dentine bonding systems and their handling characteristics on the morphology and micropermeability of the dentine adhesive interface. J Dent. 2017;27:63–71.
Koshiro K, Inoue S, Tanaka T, Koase K, Fujita M, Hashimoto M, et al. In vivo degradation of resin–dentin bonds produced by a self-etch vs. a total-etch adhesive system. Eur J Oral Sci. 2004;112:368–75.
Ricci HA, Sanabe ME, de Souza Costa CA, Pashley DH, Hebling J. Chlorhexidine increases the longevity of in vivo resin-dentin bonds. Eur J Oral Sci. 2010;118:411–6.
Bedran-Russo AKB, Pereira PNR, Duarte WR, Drummond JL, Yamauchi M. Application of crosslinkers to dentin collagen enhances the ultimate tensile strength. J Biomed Mater Res Part B Appl Biomater. 2007;80B:268–72.
Cova A, Breschi L, Nato F, Ruggeri Jr A, Carrilho M, Tjaderhane L, et al. Effect of UVA-activated riboflavin on dentin bonding. J Dent Res. 2011;90:1439–45.
Bedran-Russo AKB, Yoo KJ, Ema KC, Pashley DH. Mechanical properties of tannic-acid-treated dentin matrix. J Dent Res. 2009;88:807–11.
Tezvergil-Mutluay A, Mutluay MM, Agee KA, Seseogullari-Dirihan R, Hoshika T, Cadenaro M, et al. Carbodiimide cross-linking inactivates soluble and matrix-bound MMPs, in vitro. J Dent Res. 2012;91:192–6.
Chung L, Dinakarpandian D, Yoshida N, Lauer-Fields JL, Fields GB, Visse R, et al. Collagenase unwinds triple-helical collagen prior to peptide bond hydrolysis. EMBO J. 2004;23:3020–30.
Pashley DH, Tay FR, Breschi L, Tjäderhane L, Carvalho RM, Carrilho M, et al. State of the art etch-and-rinse adhesives. Dent Mater. 2017;27:1–16.
Mazzoni A, Angeloni V, Apolonio FM, Scotti N, Tjäderhane L, Tezvergil-Mutluay A, et al. Effect of carbodiimide (EDC) on the bond stability of etch-and-rinse adhesive systems. Dent Mater. 2013;29:1040–7.
Pashley DH, Tay FR, Carvalho RM, Rueggeberg FA, Agee KA, Carrilho M, et al. From dry bonding to water-wet bonding to ethanol-wet bonding. A review of the interactions between dentin matrix and solvated resins using a macromodel of the hybrid layer. Am J Dent. 2007;20:7–20.
Sauro S, Watson TF, Mannocci F, Miyake K, Huffman BP, Tay FR, et al. Two-photon laser confocal microscopy of micropermeability of resin-dentin bonds made with water or ethanol wet bonding. J Biomed Mater Res Part B Appl Biomater. 2009;90:327–37.
Shin TP, Yao X, Huenergardt R, Walker MP, Wang Y. Morphological and chemical characterization of bonding hydrophobic adhesive to dentin using ethanol wet bonding technique. Dent Mater. 2017;25:1050–7.
Tay FR, Pashley DH. Guided tissue remineralisation of partially demineralised human dentine. Biomaterials. 2008;29:1127–37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Tatjana Maravic, Annalisa Mazzoni, Allegra Comba, Nicola Scotti, Vittorio Checchi and Lorenzo Breschi declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Additional information
This article is part of the Topical Collection on Dental Restorative Materials
Rights and permissions
About this article
Cite this article
Maravic, T., Mazzoni, A., Comba, A. et al. How Stable is Dentin As a Substrate for Bonding?. Curr Oral Health Rep 4, 248–257 (2017). https://doi.org/10.1007/s40496-017-0149-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-017-0149-8