Abstract
Purpose of Review
Filling the root canal is necessary when the dental pulp is lost as the dead space will be colonised by bacteria, leading to reinfection of the root canal and treatment failure. Treatment methodology depends on the extent of root formation and the choice of materials available. This review looks at the classical clinical methods and also queries if the newer materials change the treatment rationale.
Recent Findings
There is considerable confusion with nomenclature for some classes of dental materials. The newer materials have specific features that may not address the treatment needs. Nonetheless, the use of bioceramics and related materials definitely modifies and improves treatment outcome.
Summary
The classical treatment methods for filling the root canals of both immature and mature teeth are quite well-established in clinical practice. Open apices are treated with calcium hydroxide paste for an extended period of time to stimulate barrier formation at the apex, and the roots are then obturated in a similar way to adult teeth using a solid cone and root canal sealer. With the introduction of bioceramics and related materials, treatment of the immature apex has been shortened to one to two visits. Bioceramic root canal sealers have changed the concept of root canal obturation from the concept of hermetic seal and inert materials to biological bonding and activity. The introduction of these materials has certainly changed the clinical outcomes of filling the root canals. Treatment time has been reduced, which is beneficial for the treatment of paediatric patients. The chemical bond and antimicrobial properties of the sealers in conjunction with hydraulic properties are promising and can potentially improve the clinical success of treatment. Further research is necessary to be able to define clinical protocols for the use of these materials in order to optimise their properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Root canal filling materials are necessary when the pulp no longer fills the root canal space. Removal of pulp tissue is necessary when its vitality is lost due to trauma, dental caries, iatrogenic damage to the pulp during dental procedures, or extensive tooth wear. Alternatively, the dental pulp may have to be removed electively to be able to use the pulp space. Depending on the age of the patient and development stage of the tooth roots, treatment methodologies have been devised to fill the root canal, thus obliterating the dead space resulting after pulp removal.
Two treatment methodologies exist for filling the root canal, with the choice depending on root development. These include apexification procedures for immature roots, and root canal obturation for fully formed roots. For both procedures, the classical treatment methodologies have changed in the last 2 decades by way of the introduction of a new class of dental materials, which were introduced to overcome the deterioration of material properties in contact with moisture. Therefore, in 1995, a new material, mineral trioxide aggregate (MTA), was introduced primarily to be used as a root-end filling material and for repair of root perforations. Its uses were later broadened to include its use as a root canal sealer, and also for apexification procedures [1].
Choices of Materials
Mineral Trioxide Aggregate and its Shortcomings
MTA is composed of Portland cement and bismuth oxide radiopacifier [2•]. Portland cement used in the construction industry is hydraulic. Since most dental procedures are performed in a wet environment, Portland cement was introduced as an endodontic material; it is patented and has became known as MTA [3, 4]. The first reported use of Portland cement in dental literature dates back to 1878 when Dr. Witte from Germany published a case report on using Portland cement to fill root canals [5•].
The first-generation materials were simple mixtures of cement and bismuth oxide; however, there were a number of concerns with these materials, including trace elements and the inclusion of aluminium when using Portland cement, stability of the bismuth oxide, and also problems with manipulation and placement.
Endodontic cements based on Portland cement have shown a higher level of trace elements, as waste materials are used as raw materials in its manufacturing for the construction industry. Additionally, waste materials are also used as replacement for primary fuels in order to keep manufacturing costs low. Traces of arsenic, lead and chromium have been reported in both grey and white MTA [6,7,8,9,10,11]. Although the levels of acid-extractable trace elements are high, the amounts leached in solution are negligible. The inclusion of heavy metals in Portland cement has raised concerns regarding its use as a base material for MTA since the latter is applied in contact with both hard and soft human tissues.
Aluminium is an integral part of the cement and cannot be removed as it is produced during manufacture of the cement. Aluminium is leached in solution from materials containing Portland cement, such as MTA [12], and it has been shown that aluminium released from the cement used for dental applications can be found in the liver and plasma of test animals [13••]. Furthermore, an aluminium peak was observed in the brain tissue of test animals 7 days after implantation in MTA Angelus, and 60 days after implantation in Theracal and MTA Fillapex. Oxidative stress was induced and antioxidant enzymes were transiently upregulated [14••]. Moreover, high levels of aluminium in contact with human tissues has been linked with Alzheimer’s disease [15].
Bismuth oxide, which is added to MTA to act as a radiopacifying agent, is unstable and interferes with the hydration reaction of the cement replacing the silicon from the calcium silicate hydrate structure [16]. The initial reports of tooth discolouration when using MTA were incidental findings [17,18,19,20,21,22]. The causative factors implicated in the change in colour of bismuth oxide from yellow to dark brown include its reaction with sodium hypochlorite [23••] and formaldehyde [24], as well as contact with collagen, and thus tooth structure [25]. Furthermore, light and the presence of oxygen have also been shown to be precipitating factors leading to material discoloration [26, 27]. The addition of zinc oxide to MTA was shown to eliminate discolouration, and the material properties did not deteriorate [28].
Another main concern with the original MTA formulation is the consistency of the freshly mixed material, which is usually termed as grainy or sandy. The original formulation is also hand spatulated and delivery to the operative site is difficult. MTA presents a longer setting time (2 h and 45 min) compared with other retrograde filling materials such as amalgam, Super-ethoxy benzoic acid (EBA), and intermediate restorative material (IRM) [29]. Furthermore, the long setting time makes MTA unsuitable for most clinical applications. Different powder-to-water ratios, which tend to be a frequent occurrence in clinical practice since the gram supplied is usually not used in one application, also exert influence on the properties of MTA, promoting a longer setting time [30, 31].
Bioceramics and Their Properties
Due to these clinical problems, second-generation materials were developed that addressed the issue of trace elements and aluminium by using pure tricalcium silicate cement rather than Portland cement. Furthermore, bismuth oxide is replaced by alternative radiopacifiers and handling is easier as these materials contain additives that enhance the material properties and are also presented in a variety of clinically friendly methods.
With the introduction of the second-generation materials, a new term has also been introduced—bioceramics. With bioceramics, the purity of the materials, inert behaviour and their biocompatibility needed to be stressed; however, the term may not be scientifically precise. Ceramics are defined as heat-resistant, nonmetallic, inorganic solids that are generally made up of compounds formed from metallic and nonmetallic elements. Although different types of ceramics can have very different properties, ceramics are, in general, corrosion-resistant and hard, but also brittle. In dentistry, ceramics broadly refers to all glasses, zirconia and porcelain; thus, the definition is too broad. It is necessary to identify the material types and their specific use.
The easiest classification is to include in this group materials that are based on tricalcium silicate or hydraulic calcium silicates (a proposed classification is shown in Fig. 1). This classification identifies the materials by their chemistry and specific uses. The most important classification is defining which of the materials are based on Portland cement as this would identify a specific chemistry that differs from that of pure tricalcium silicate. Portland cement is composed of both silicate and aluminate phases that produce different byproducts of hydration when the cement is mixed with water compared with the pure tricalcium silicate cement that contains only the tricalcium silicate phase [32]. As already indicated, the Portland cement-based materials may also incorporate trace elements. The classification shown in Fig. 1 also gives an indication of the clinical material uses. The material types clinically available are overviewed in Chapter 8 of Mineral Trioxide Aggregate in Dentistry: From Preparation to Application [33].
As indicated, the range of materials available is wide and the materials are quite distinct. For filling the root canal of mature adult teeth, the sealers are used together with a solid cone. All sealers are second-generation as they all show modifications to the classical cement/radiopacifier powder-to-water mix. For filling the immature apices, a range of second-generation materials exist. The term bioceramics is frequently used to describe the second-generation materials, to indicate that these materials are diverse from the simple cement/radiopacifier mixtures. The main query is, are all these materials bioceramic, and, if not, which are the bioceramics?
A search on MEDLINE [34], using the terms ‘bioceramic’ and ‘endodontics’ yielded 65 results. Excluding reviews and articles on materials not related to dentistry, the remainder were related to the Endosequence/TotalFill range of materials. The first published article was on DiaRoot BioAggregate, in 2009 [35], which compared the biological activity of BioAggregate with ProRoot MTA. This range of materials started by launching Bioaggregate (a powder/liquid formulation), iRoot SP (a sealer) and iRoot PB (a paste). These products were marketed by Innovative Bioceramix, Inc., Vancouver, BC, Canada; however, later, these materials were no longer available and Endosequence putty, paste and sealer were introduced by Brasseler, Savannah, GA, USA, which in Europe are sold as TotalFill by FKG Dentaire, La Chaux-de-Fonds, Switzerland. These materials are considerably different to MTA.
Bioceramics are composed of a cement phase that is tricalcium silicate cement rather than Portland cement present in MTA. This way they do not leach trace elements and aluminium in solution (this has been verified in recent studies) [11, 12]. The hydration reaction of both Portland cement and tricalcium silicate has been described and compared [32], and the hydration reaction is shown below:
All three reactions occur in Portland cement, but only the first occurs in tricalcium silicate cement, and also possibly the second reaction if some dicalcium silicate is present. Calcium hydroxide is formed as a byproduct of cement hydration, which is clinically relevant.
Bismuth oxide has also been replaced by tantalum oxide in paste and putty [36••] and zirconium oxide in the sealer [37, 38]. Thus, the two main concerns with the use of MTA have been addressed by the use of bioceramics. The other main concern was handling, however this has also been well-addressed as bioceramics are supplied in both putty and paste forms for root-end surgery and perforation repairs, and the sealer is premixed and dispensed through a syringe.
The chemical formulation of bioceramics is not only a cement and radiopacifier phase—a second cementitious phase is also present, i.e. calcium phosphate monobasic. This provides free phosphate ions in solution to enhance biomineralization, which occurs when the calcium ions formed from hydration of the tricalcium silicate come in contact with phosphates in tissue fluids and a calcium phosphate phase forms. This has been reported by a number of research papers and is the basis of biomineralization described for these material types [39,41,42,••, 40–43]. The presence of phosphate within the material provides freely available phosphate ions to induce this biomineralization. The effect of the addition of two types of phosphates to tricalcium silicate cement has been investigated [44]. Moreover, phosphate ions are released in solution from bioceramics [12]. The addition of calcium phosphate monobasic and hydroxyapatite to tricalcium silicate cement modifies the hydration reaction and reduces calcium ion leaching after material setting. This effects the cell growth of proliferation [44]; thus, having biphasic cements is hardly beneficial for biomineralization purposes.
Another feature of bioceramics is the use of fillers such as silicon oxide. The aim of the silicon oxide filler is to enhance the long-term physical properties of the material. The silicon oxide reacts with the calcium hydroxide formed during hydration, as indicated in Reactions 1 and 2. The reaction shown in Reaction 4 leads to the formation of more calcium silicate hydrate.
This reaction is well-documented in the Portland cement chemistry literature [45]. The silicon oxide acts as a pozzolana or latent hydraulic binder. This reaction has been shown to occur in Bioaggregate [12], and after 28 days of hydration the calcium hydroxide was shown to be depleted. The clinical uses of bioceramics where the calcium ions are needed may be jeopardised. This includes apexification procedures, pulp capping and all procedures where antimicrobial activity is necessary as formation of calcium silicate hydrate will lead to a reduction in pH, thus limiting the antimicrobial activity of the material. The physical properties of Bioaggregate are similar to those of other materials not containing the silicon oxide filler [46].
Other second-generation materials exist for the various uses described in Fig. 1. These materials all show modifications to the original Portland cement and bismuth oxide formulation in one way or another. The various material types are presented in Tables 1 and 2. Table 1 shows the materials based on tricalcium and dicalcium silicate, and also Portland cement, comparing them with the original MTA formulations from Dentsply and Angelus, and also the bioceramics from Innovative Bioceramix, Inc. and Brasseler/FKG. The Medcem Portland cement is a very simplified version of a second-generation material as it consists of Portland cement only, with no radiopacifier, additives or any modification to the dispensing method. The main change in the second-generation materials lies in the use of tricalcium silicate cement, a change that is seen in Biodentine. Endocem MTA and Endocem Zirconia are the only materials using dicalcium silicate, with the rest still using the Portland cement regardless of reports on trace element contamination [6,7,8,9,10,11] and aluminium leaching [12, 13••, 14••]. Most of the materials show the use of alternative radiopacifiers, with the most popular being tantalum oxide, calcium tungstate and zirconium oxide; some are combined with bismuth oxide. All the new generation of materials contain additives such as silicon dioxide, and a number contain calcium chloride, which is used to accelerate the materials, thus reducing the setting time, and a water soluble polymer to enhance the material flow, thus enabling easier manipulation. Calcium carbonate is also used as a filler and this has been reported to enhance material hydration by providing a nucleation site [47]. This works with the tricalcium silicate, and it was shown that the presence of calcium carbonate results in an earlier reaction peak in Biodentine [47]. MM MTA, which has a similar chemistry but contains Portland cement rather than tricalcium silicate, does not have this reaction. In fact, the addition of calcium carbonate interferes with the precipitation of calcium hydroxide in solution and may thus jeopardise the clinical use of this material [48]. The material chemistry is very specific and all additives play a major role in the hydration and development of material properties. The presentation of the materials and the method of mixing varies, as indicated in Table 1.
Regardless of the similar chemistry of the materials, not all manufacturers list apexification as a procedure for which they recommend material use, with MTA being suggested as the material of choice for apexification procedures [1]. The effectiveness of ProRoot MTA and MTA Angelus have been compared [49], with both materials showing suitability; however, less research has been conducted on Bioaggregate and Endosequence/TotalFill for use in apexification [50, 51]. Biodentine seems to be the material of choice for such procedures, with more cases of apexification being reported with this material [52,53,54,55,56,57,58,59].
All sealers are second-generation and all have additives to enhance the material properties, as shown in Table 2. Presentation varies and some are premixed. Bioceramics and Biodentine use tricalcium silicate rather than Portland cement.
Since all material formulations follow the same pattern and all show modifications to the original MTA formulation, they are either all bioceramics or none are bioceramics. Since the term bioceramic is not scientifically correct, these materials should be grouped together and a suitable name found to represent these material types. The most precise term to date has been hydraulic calcium silicates.
Treatment Methodologies
Classical Clinical Management of Immature Teeth
Once the pulp tissue is lost, it is necessary to fill the root canal space. Immature teeth present a problem due to their anatomy as the roots are short and thin and routine canal obturation is difficult due to the root canal configuration. The thin dentine walls are also at risk of fracture.
Apexification procedures allow the formation of a calcific barrier at the root apex, thus closing off the root end from the periapical space. A calcific bridge is created by providing an environment where calcium ions from the dentine form a calcific bridge. Such conditions are created by application of calcium hydroxide paste within the canal. Calcium hydroxide has been in use since 1920 when B.W. Hermann (Germany) described for the first time the use of calcium hydroxide to fill root canals. In his dissertation, he clearly demonstrated the antibacterial effect of calcium hydroxide in infected root canals without any adverse reactions [60•]. The aim of his work was to invent a method for ‘biological root canal treatments’.
Calcium hydroxide has been used for several decades to create a calcific bridge, leaving a stunted root. Treatment involves several visits over a number of months. The first paper describing this procedure in primates was published in 1971 [61] and the root-end closure techniques, including the apexification procedure, were described in 1974 [62]. Treatment time and success depended on the size of the apex and the presence of periapical infection. Older children having a narrow open apex had a shorter treatment time than younger children’s teeth, and teeth without periapical infection showed some amount of root growth and closing of the apex that was faster than those with periapical infection. The calcified bridge formed following apexification was a porous structure [63].
Calcium hydroxide releases calcium ions to create an ideal environment for the formation of a calcific bridge [64]. Another advantage of the calcium hydroxide paste is its antibacterial properties as pulpless root canals usually result from nonvital teeth that are prone to bacterial colonisation [65]. Calcium hydroxide paste shows limited antibacterial activity compared with other chemical reagents [66, 67], while elimination of bacteria requires long-term dressings [68]. Once the bridge is complete, the root canal is obturated routinely by methods that will be described for mature permanent teeth. The main disadvantage with the obturation is that the solid cone/sealer technique will not be able to adequately fill the root of an immature tooth due to its particular shape since the cones are tapered and shaped in the form of mature teeth.
Classical Clinical Management of Mature Teeth
When the pulp is lost, leaving a dead space behind, the mature roots in adult permanent teeth need to be obturated. Root canal treatment methodologies are very old and have changed very little over the years. The first gutta-percha available for clinical use was manufactured by S.S. White in 1887. The dental gutta-percha is mainly composed of zinc oxide, and was initially used as a single cone, together with root canal sealer. The techniques then evolved to lateral condensation and warm vertical compaction to enhance the three-dimensional quality of the root canal filling [69•]. The core acts as a piston on the flowable sealer, causing it to spread, fill voids, and to wet and attach to the instrumented dentin wall. It is the sealer that comes into contact with the dentine and periodical tissues, and it is thus important that the sealer possesses the ideal material properties as outlined by Grossman [70].
The three primary functions of a root filling are sealing against ingrowth of bacteria from the oral cavity, entombment of remaining microorganisms, and complete obturation at a microscopic level to prevent stagnant fluid from accumulating and serving as nutrients for bacteria from any source [71]. For this purpose, the gutta-percha solid cone-sealer association has had considerable success and an hermetic seal is provided by a warm, vertically compacted gutta-percha with a selection of sealers that interact with the dentine walls forming sealer tags. For this purpose, epoxy resin-based root canal sealers have been termed the gold standard for sealer cements.
To date, the only challenge to the gutta-percha sealer obturation has been the introduction of a synthetic resin cone and resin-based sealer which promised to create a monoblock obturation to a primed root canal wall. The Resilon/Epiphany system was not very successful as the synthetic resin was easily degraded by bacteria and their enzymes [72,73,74,75].
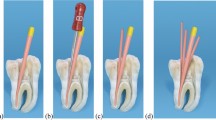
Single Visit Apexification Procedures
With the introduction of MTA, the lengthy apexification procedures needed to create a barrier at the root end were reduced to one or two clinical sessions where an apical barrier was created and the tooth could immediately be restored normally. A retrospective study on the efficiency of this treatment methodology shows that apexification in one step using an apical plug of MTA can be considered a predictable treatment, and may be an alternative to the use of calcium hydroxide [76]. The first reported multifaceted use of ProRoot MTA and its indications for apexification were first reported in 2001 [77, 78].
The main features of MTA that make it suitable for apexification procedures is its hydraulic nature and also the properties related to the formation and release of calcium hydroxide. The release of calcium hydroxide in MTA is very well-documented, as is interaction of the material with phosphates in tissue fluids, resulting in biomineralization [39,41,42,••, 40–43]. A phosphate-buffered saline intracanal dressing further enhanced the bond strength of the materials to dentine in MTA apical plugs [81]. In vivo, it has been shown from animal models, and even characterisation of explanted root-end filling material, that the formation of calcium phosphate on the material surface may not occur in vivo. Only calcium carbonate was deposited when MTA and bioceramics were in contact with blood and tissue fluids [36••, 79]. Whether or not biomineralization occurs, any reaction of calcium hydroxide with the surrounding media will result in a drop in pH and deterioration of antimicrobial properties of the material. This has been shown, even for ProRoot MTA in contact with blood [80]. Reduction of the availability of free calcium ions may also jeopardise the apical barrier formation.
Biodentine has been shown to release more calcium ions in solution than MTA [47], and its success when used as an apical plug in apexification cases has been reported [54,55,56,57,58,59]. Its hydration is optimised by the addition of calcium carbonate as a nucleating agent spiking up the reaction rate in the early stages, the addition of calcium chloride accelerator, and the water soluble polymer allowing low water/powder ratios. The addition of pozzolanic materials such as amorphous silicon oxide to second-generation materials, including those claimed to be bioceramics and the rest (as indicated in Table 1), aims at improving long-term material properties. These latent hydraulic binders deplete the free calcium ions and form more calcium silicate hydrate, as shown in Reaction 4. More depletion of free calcium occurs with the addition of calcium phosphate, as is the case with the Brasseler/FKG materials [44], and also by reaction of calcium carbonate in MM MTA, which affects the distribution of lime, alumina and sulfate of the Portland cement and alters the mineralogy of hydrated cement pastes. Calcite additions affect the amount of free calcium hydroxide, as well as the balance between the ettringite and monosulfate phases in the hydrated cement phases [48]. Depletion of calcium affects the biological properties of the set materials [44]. Moreover, these materials may not be suitable for apexification procedures.
Root Canal Obturation with Bioceramics
The classical root canal obturation of a mature adult tooth relies on an hermetic seal to prevent microbial recolonisation of the root canal. This is achieved through a barrier composed of gutta-percha and a sealer, which are impervious to percolation. The use of bioceramic sealers and other materials of the same family creates different challenges for the success of root canal therapy. The two main features of these materials are their hydraulic nature and their reactivity due to the formation of calcium hydroxide that is leached in solution.
Their hydraulic nature necessitates the presence of moisture in the root canal, which is further exacerbated by the existence of premixed sealers such as Root SP, Endosequence BC, TotalFill and Endoseal MTA. These sealers need moisture present in the root canal to set. Thus, the general principle applied to all classic sealer types to dry the canal after irrigation and remove the smear layer to have resin tags of the sealer, and therefore the hermetic seal, does not apply to bioceramics. A recent study where a low-pressure fluid column filled with simulated body fluid was applied to a root stump showed complete setting of the Endosequence BC sealer [37]. Nonetheless, the use of phosphate-buffered saline has been suggested as a final irrigant prior to root canal obturation. This increased the push-out bond strength of the obturation as the biomineralizing ability of the bioceramic sealer is enhanced [81, 82]. However, the use of a phosphate-buffered saline final wash reduces the antimicrobial activity of the bioceramic sealers. Even BioRoot, which registers the highest pH compared with Endosequence, and double the calcium ion release [37], still lost its antimicrobial activity when phosphate-buffered saline was used as a final irrigant [83].
Other root canal irrigating solutions may not be used with bioceramic sealers. Sodium hypochlorite leads to sealer discolouration, which in turn causes tooth discolouration by elemental migration of bismuth oxide from the material to the tooth [84] when used in the presence of bismuth oxide-containing sealers [23••]. Ethylenediaminetetraacetic acid (EDTA), a routine irritant used to remove the smear layer, affects the chemistry of these calcium-containing materials as it is an established calcium chelator [85]. EDTA reduces the interaction of calcium ions with dentine and the deposit of β-calcium phosphate in both BioRoot and Endosequence BC sealers; however, calcium ion depletion was more evident in BioRoot [85]. Therefore, the choice of irrigation protocol is important when using bioceramic sealers.
The bioceramic sealers bond to dentine by a process known as alkaline etching (caused by the alkalinity of the sealer), and a mineral infiltration zone develops at the interface of the dentine in contact with the material [86•]. The presence of a mineral infiltration zone and sealer tags was shown by confocal microscopy using fluorescent dyes to tag the sealer [86•, 87]. The development of the mineral infiltration zone has been discredited by other authors using micro-Raman and electron probe microanalyses [88]. The use of bioceramics has been shown to cause softening to collagen in dentine [89] and deterioration in the flexural strength of the tooth [90].
Bioceramic sealers can be used with either gutta-percha solid cones or bioceramic-coated cones. The bioceramic coating of gutta-percha is meant to enhance the bond strength of the sealer to the cone; however, no definite data are available as to whether this is true. Hygroscopic points (CPoints) have also been suggested for use with bioceramic sealers. The pressure derived from hygroscopic expansion of CPoints or warm vertical condensation did not enhance the penetration depths of the calcium silicate-based sealer. Sealer penetration into the dentinal tubules occurred independently of the obturation technique [91].
The single-cone obturation technique has been suggested for use with bioceramic sealers. Comparison of single-cone obturation with warm vertical compaction showed that the percentage volume of voids was similar in the two groups and was influenced by the obturation technique in the cervical third only [92]. A higher percentage of voids was shown in the cervical third when BioRoot was used in conjunction with gutta-percha compared with AH Plus sealer [87]. Both techniques produced similar tubule penetration at both the 1-mm and 5-mm level using bioceramic sealers [93]. Conversely, significantly less porosity was observed in root canals filled using the single-cone technique, with porosity near the crown of the tooth being reduced sixfold, whereas in the mid root region porosity was reduced to <10% of the values found in the lateral compaction filled teeth [94]. Single-cone obturation resulted in better bond strength than warm vertical compaction, with Endosequence BC giving better results than an MTA-based sealer [95]. Excessive heat in warm vertical compaction should be avoided as it tends to evaporate the water in the sealer and thus lead to changes in the physical properties, which may be detrimental to long-term success of the obturation [96].
Conclusions and Future Research
A variety of cements based on tricalcium silicate are available clinically. There is clearly a lot of confusion with nomenclature and material classification and further research is necessary to develop appropriate clinical protocols for using these materials to fill the root canal of both mature and immature teeth. MTA, particularly the ProRoot, is the most widely researched material of the hydraulic calcium silicates and is used for a number of applications in endodontics. The newer-generation materials include additives and are aimed at overcoming the basic difficulties encountered with the first-generation materials. The wide range of materials, whether they are called bioceramics or are not available to the clinician, enables high-quality dental care. The clinician should be aware of the specific material properties and should be able to choose the appropriate material for each clinical situation. The best filling for a root canal will always be dental pulp, and regenerative methods are already available to regrow pulps in teeth that are necrotic. The maintenance of pulp vitality is also of paramount importance.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197–205.
Camilleri J, Montesin FE, Brady K, Sweeney R, Curtis RV, Ford TR. The constitution of mineral trioxide aggregate. Dent Mater. 2005;21:297–303. This article is the first describing the hydration mechanism of MTA and the formation of calcium hydroxide, thus enabling further material development.
Torabinejad M, White DJ. Tooth filling material and method of use. US Patent. 1993;5:415,547.
Torabinejad M, White DJ. Tooth filling material and method of use. US Patent. 1995;5:769,638.
Witte. The filling of a root canal with Portland cement. German Quarterly for Dentistry. J Cent Assoc German Dent. 1878;18:153–154. The first article describing the use of Portland cement as a dental material.
Duarte MA, De Oliveira Demarchi AC, Yamashita JC, Kuga MC, De Campos Fraga S. Arsenic release provided by MTA and Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:648–50.
Monteiro Bramante C, Demarchi AC, de Moraes IG, et al. Presence of arsenic in different types of MTA and white and gray Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:909–13.
Schembri M, Peplow G, Camilleri J. Analyses of heavy metals in mineral trioxide aggregate and Portland cement. J Endod. 2010;36:1210–5.
Matsunaga T, Tsujimoto M, Kawashima T, et al. Analysis of arsenic in gray and white mineral trioxide aggregates by using atomic absorption spectrometry. J Endod. 2010;36:1988–90.
Chang SW, Baek SH, Yang HC, et al. Heavy metal analysis of ortho MTA and ProRoot MTA. J Endod. 2011;37:1673–6.
Camilleri J, Kralj P, Veber M, Sinagra E. Characterization and analyses of acid-extractable and leached trace elements in dental cements. Int Endod J. 2012;45:737–43.
Camilleri J, Sorrentino F, Damidot D. Characterization of un-hydrated and hydrated BioAggregate™ and MTA Angelus™. Clin Oral Investig. 2015;19(3):689–98.
Demirkaya K, Can Demirdöğen B, Öncel Torun Z, Erdem O, Çetinkaya S, Akay C. In vivo evaluation of the effects of hydraulic calcium silicate dental cements on plasma and liver aluminium levels in rats. Eur J Oral Sci. 2016;124(1):75–81. Paper shows the migration and toxicity of aluminium in test animals.
Demirkaya K, Demirdöğen BC, Torn ZÖ, Erdem O, Çırak E, Tunca YM. Brain aluminium accumulation and oxidative stress in the presence of calcium silicate dental cements. Hum Exp Toxicol. Paper shows the migration and toxicity of aluminium in test animals.
Forbes WF, Gentleman JF. Risk factors, causality, and policy initiatives: the case of aluminum and mental impairment. Exp Gerontol. 1998;33:141–54.
Camilleri J. Characterization of hydration products of mineral trioxide aggregate. Int Endod J. 2008;41:408–17.
Moore A, Howley MF, O'Connell AC. Treatment of open apex teeth using two types of white mineral trioxide aggregate after initial dressing with calcium hydroxide in children. Dent Traumatol. 2011;27:166–73.
Jacobovitz M, de Pontes Lima RK. The use of calcium hydroxide and mineral trioxide aggregate on apexification of a replanted tooth: a case report. Dent Traumatol. 2009;25:e32–6.
Erdem AP, Ozdas DO, Dincol E, Sepet E, Aren G. Case series: root healing with MTA after horizontal fracture. Eur Arch Paediatr Dent. 2009;10:110–3.
Jacobovitz M, de Lima RK. Treatment of inflammatory internal root resorption with mineral trioxide aggregate: a case report. Int Endod J. 2008;41:905–12.
Dabbagh B, Alvaro E, Vu DD, Rizkallah J, Schwartz S. Clinical complications in the revascularization of immature necrotic permanent teeth. Pediatr Dent. 2012;34:414–7.
Ioannidis K, Mistakidis I, Beltes P, Karagiannis V. Spectrophotometric analysis of coronal discoloration induced by grey and white MTA. Int Endod J. 2013;46:137–44.
Camilleri J. The color stability of white mineral trioxide aggregate in contact with sodium hypochlorite solution. J Endod. 2014;40:436–40. This paper describes the interaction of sodium hypochlorite with bismuth oxide for the first time, thus explaining the dental discolouration seen after root canal therapy.
Marciano MA, Camilleri J, LiaMondelli RF, et al. Potential dental staining of root canal sealers with formulations containing bismuth oxide and formaldehyde. ENDO-Endodontic Practice Today. 2015;9(1):39–45.
Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MAH. Assessment of color stability of white MTA Angelus and bismuth oxide in contact with tooth structure. J Endod. 2014;40:1235–40.
Vallés M, Mercadé M, Duran-Sindreu F, Bourdelande JL, Roig M. Color stability of white mineral trioxide aggregate. Clin Oral Investig. 2013;17:1155–9.
Vallés M, Mercadé M, Duran-Sindreu F, Bourdelande JL, Roig M. Influence of light and oxygen on the color stability of five calcium silicate-based materials. J Endod. 2013;39:525–8.
Marciano MA, Camilleri J, Costa RM, Matsumoto MA, Guimarães BM, Duarte MA. Zinc oxide inhibits dental discoloration caused by white MTA Angelus. J Endod. 2017;43(6):1001–7.
Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21:349–53.
Cutajar A, Mallia B, Abela S, Camilleri J. Replacement of radiopacifier in mineral trioxide aggregate; characterization and determination of physical properties. Dent Mater. 2011;27:879–91.
Cavenago BC, Pereira TC, Duarte MA, et al. Influence of powder-to-water ratio on radiopacity, setting time, pH, calcium ion release and a micro-CT volumetric solubility of white mineral trioxide aggregate. Int Endod J. 2014;47:120–6.
Camilleri J. Characterization and hydration kinetics of tricalcium silicate cement for use as a dental biomaterial. Dent Mater. 2011;27(8):836–44.
Primus C. Products and Distinctions. In: Camilleri J, editor. Mineral Trioxide Aggregate in Dentistry. From Preparation to Application”. Springer; 2014. p. 151–172
US National Library of Medicine, National Institutes of Health. Medline. Available at: https://www.ncbi.nlm.nih.gov/pubmed
De-Deus G, Canabarro A, Alves G, Linhares A, Senne MI, Granjeiro JM. Optimal cytocompatibility of a bioceramic nanoparticulate cement in primary human mesenchymal cells. J Endod. 2009;35(10):1387–90.
Moinzadeh AT, Aznar Portoles C, Schembri Wismayer P, Camilleri J. Bioactivity potential of EndoSequence BC RRM putty. J Endod. 2016;42(4):615–21. The first article discrediting the calcium phosphate formation shown in vitro for bioceramics by testing explanted material.
Brasseler USA. Endosequence BC sealer, material safety data sheet. Available at: http://brasselerusadental.com/wp-content/files/B_3114E_BC%20Sealer%20MSDS.pdf
Xuereb M, Vella P, Damidot D, Sammut CV, Camilleri J. In situ assessment of the setting of tricalcium silicate-based sealers using a dentin pressure model. J Endod. 2015;41(1):111–24.
Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod 2005;31:97–100. First article describing the biomineraliziation potential of MTA.
Bozeman TB, Lemon RR, Eleazer PD. Elemental analysis of crystal precipitate from gray and white MTA. J Endod. 2006;32:425–8.
Tay FR, Pashley DH, Rueggeberg FA, Loushine RJ, Weller RN. Calcium phosphate phase transformation produced by the interaction of the portland cement component of white mineral trioxide aggregate with a phosphate-containing fluid. J Endod. 2007;33:1347–51.
Reyes-Carmina JF, Felippe MS, Felippe WT. Biomineralization ability and interaction of mineral trioxide aggregate and white Portland cement with dentin in a phosphate-containing fluid. J Endod. 2009;35:731–6.
Gandolfi MG, Taddei P, Tinti A, De Stefano DE, Rossi PL, Prati C. Kinetics of apatite formation on a calcium-silicate cement for root-end filling during ageing in physiological-like phosphate solutions. Clin Oral Investig. 2010;14:659–68.
Schembri Wismayer P, Camilleri J. Why biphasic? Assessment of the effect on cell proliferation and expression. J Endod. 2017;43(5):751–9.
Lea FM, Hewlett PC. Lea's chemistry of cement and concrete. 4th ed. London, New York: Arnold; Co-published in North, Central, and South America by J. Wiley; 1998.
Grech L, Mallia B, Camilleri J. Investigation of the physical properties of tricalcium silicate cement-based root-end filling materials. Dent Mater. 2013;29(2):e20–8.
Camilleri J, Sorrentino F, Damidot D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent Mater. 2013;29(5):580–93.
Khalil I, Naaman A, Camilleri J. Investigation of a novel mechanically mixed mineral trioxide aggregate (MM-MTA™). Int Endod J. 2015;48(8):757–67.
Lolayekar N, Bhat SS, Hegde S. Sealing ability of ProRoot MTA and MTA-Angelus simulating a one-step apical barrier technique: an in vitro study. J Clin Pediatr Dent. 2009;33(4):305–10.
Memiş Özgül B, Bezgin T, Şahin C, Sarı Ş. Resistance to leakage of various thicknesses of apical plugs of Bioaggregate using liquid filtration model. Dent Traumatol. 2015;31(3):250–4.
Tran D, He J, Glickman GN, Woodmansey KF. Comparative analysis of calcium silicate-based root filling materials using an open apex model. J Endod. 2016;42(4):654–8.
Nayak G, Hasan MF. Biodentine-a novel dentinal substitute for single visit apexification. Restor Dent Endod. 2014;39(2):120–5.
Caronna V, Himel V, Yu Q, Zhang JF, Sabey K. Comparison of the surface hardness among 3 materials used in an experimental apexification model under moist and dry environments. J Endod. 2014;40(7):986–9.
Khetarpal A, Chaudhary S, Talwar S, Verma M. Endodontic management of open apex using Biodentine as a novel apical matrix. Indian J Dent Res. 2014;25(4):513–6.
Bajwa NK, Jingarwar MM, Pathak A. Single visit apexification procedure of a traumatically injured tooth with a novel bioinductive material (Biodentine). Int J Clin Pediatr Dent. 2015;8(1):58–61.
Martens L, Rajasekharan S, Cauwels R. Endodontic treatment of trauma-induced necrotic immature teeth using a tricalcium silicate-based bioactive cement. A report of 3 cases with 24-month follow-up. Eur J Paediatr Dent. 2016;17(1):24–8.
Vidal K, Martin G, Lozano O, Salas M, Trigueros J, Aguilar G. Apical closure in apexification: a review and case report of apexification treatment of an immature permanent tooth with Biodentine. J Endod. 2016;42(5):730–4.
Evren OK, Altunsoy M, Tanriver M, Capar ID, Kalkan A, Gok T. Fracture resistance of simulated immature teeth after apexification with calcium silicate-based materials. Eur J Dent. 2016;10(2):188–92.
Niranjan B, Shashikiran ND, Dubey A, Singla S, Gupta N. Biodentine: a new novel bio-inductive material for treatment of traumatically injured tooth (single visit apexification). J Clin Diagn Res. 2016;10(9):ZJ03–4.
Hermann, B. Kalziumhydroxid als Mittel zum Behandeln und Füllen von Zahnwurzelkanälen [dissertation]. Würzburg: 1920. The first use of calcium hydroxide in endodontic therapy.
Steiner JC, Van Hassel HJ. Experimental root apexification in primates. Oral Surg Oral Med Oral Pathol. 1971;31(3):409–15.
Goldman M. Root-end closure techniques including apexification. Dent Clin North Am. 1974;18(2):297–308.
Walia T, Chawla HS, Gauba K. Management of wide open apices in non-vital permanent teeth with Ca(OH)2 paste. J Clin Pediatr Dent. 2000;25(1):51–6.
Rehman K, Saunders WP, Foye RH, Sharkey SW. Calcium ion diffusion from calcium hydroxide-containing materials in endodontically-treated teeth: an in vitro study. Int Endod J. 1996;29(4):271–9.
Chong BS, Pitt Ford TR. The role of intracanal medication in root canal treatment. Int Endod J. 1992;25(2):97–106.
Bystrom A, Claesson R, Sundqvist G. The antibacterial effect of camphorated paramonochlorophenol, camphorated phenol and calcium hydroxide in the treatment of infected root canals. Endod Dent Traumatol. 1985;1(5):170–5.
DiFiore PM, Peters DD, Setterstrom JA, Lorton L. The antibacterial effects of calcium hydroxide apexification pastes on Streptococcus sanguis. Oral Surg Oral Med Oral Pathol. 1983;55(1):91–4.
Sjögren U, Figdor D, Spongebag L, Sundqvist G. The antimicrobial effect of calcium hydroxide as a short-term intracanal dressing. Int Endod J. 1991;24(3):119–25.
Schilder H. Filling root canals in three dimensions. Dent Clin North Am. 1967;723–44. Description of warm vertical compaction.
Grossman LI. Endodontic practice. Philadelphia, PA: Lea &Febiger; 1978.
Sundqvist G, Figdor D. Endodontic treatment of apical periodontitis. In: Orstavik D, Pitt Ford TR, editors. Essential endodontology. Prevention and treatment of apical periodontitis. Oxford: Blackwell; 1998.
Tay FR, Loushine RJ, Weller RN, et al. Ultrastructural evaluation of the apical seal in roots filled with a polycaprolactone-based root canal filling material. J Endod. 2005;31(7):514–9.
Tay FR, Pashley DH, Williams MC, et al. Susceptibility of a polycaprolactone-based root canal filling material to degradation: I. alkaline hydrolysis. J Endod. 2005;31(8):593–8.
Tay FR, Pashley DH, Yiu CK, et al. Susceptibility of a polycaprolactone-based root canal filling material to degradation: II. Gravimetric evaluation of enzymatic hydrolysis. J Endod. 2005;31(10):737–41.
Hiraishi N, Yau JY, Loushine RJ, et al. Susceptibility of a polycaprolactone-based root canal-filling material to degradation. III. Turbidimetric evaluation of enzymatic hydrolysis. J Endod. 2007;33(8):952–6.
Simon S, Rilliard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one-visit apexification treatment: a prospective study. Int Endod J. 2007;40(3):186–97.
Witherspoon DE, Ham K. One-visit apexification: technique for inducing root-end barrier formation in apical closures. Pract Proced Aesthet Dent. 2001;13(6):455–60. quiz 462.
Schmitt D, Lee J, Bogen G. Multifaceted use of ProRoot MTA root canal repair material. Pediatr Dent. 2001;23(4):326–30.
Schembri Wismayer P, Lung CY, Rappa F, Cappello F, Camilleri J. Assessment of the interaction of Portland cement-based materials with blood and tissue fluids using an animal model. Sci Rep. 2016;6:34547.
Farrugia C, Baca P, Camilleri J, Arias Moliz MT. Antimicrobial activity of ProRoot MTA in contact with blood. Sci Rep. 2017;7:41359.
Reyes-Carmona JF, Felippe MS, Felippe WT. A phosphate-buffered saline intracanal dressing improves the biomineralization ability of mineral trioxide aggregate apical plugs. J Endod. 2010;36(10):1648–52.
Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod. 2010;36(2):286–91.
Arias-Moliz MT, Camilleri J. The effect of the final irrigant on the antimicrobial activity of root canal sealers. J Dent. 2016;52:30–6.
Marciano MA, Duarte MA, Camilleri J. Dental discoloration caused by bismuth oxide in MTA in the presence of sodium hypochlorite. Clin Oral Investig. 2015;19(9):2201–9.
Harik R, Salameh Z, Habchi R, Camilleri J. The effect of irrigation with EDTA on calcium-based root canal sealers: a SEM-EDS and XRD study. J Leb Dent Assoc. 2016;49:12–23.
Atmeh AR, Chong EZ, Richard G, Festy F, Watson TF. Dentin-cement interfacial interaction: calcium silicates and polyalkenoates. J Dent Res. 2012;91(5):454–9. The first mention of the mineral infiltration zone.
Viapiana R, Moinzadeh AT, Camilleri L, Wesselink P, Tanomaru-Filho M, Camilleri J. Porosity and sealing ability of root fillings with gutta-percha and Bioroot RCS or AH Plus sealers. Evaluation by three ex vivo methods. Int Endod J. 2016;49(8):774–82.
Li X, Pongprueksa P, Van Landuyt K, et al. Correlative micro-Raman/EPMA analysis of the hydraulic calcium silicate cement interface with dentin. Clin Oral Investig. 2016;20(7):1663–73.
Leiendecker AP, Qi YP, Sawyer AN, et al. Effects of calcium silicate-based materials on collagen matrix integrity of mineralized dentin. J Endod. 2012;38(6):829–33.
Sawyer AN, Nikonov SY, Pancio AK, et al. Effects of calcium silicate-based materials on the flexural properties of dentin. J Endod. 2012;38(5):680–3.
Jeong JW, DeGraft-Johnson A, Dorn SO, Di Fiore PM. Dentinal tubule penetration of a calcium silicate-based root canal sealer with different obturation methods. J Endod. 2017;43(4):633–7.
Iglecias EF, Freire LG, de Miranda Candeiro GT, Dos Santos M, Antoniazzi JH, Gavini G. Presence of voids after continuous wave of condensation and single-cone obturation in mandibular molars: a micro-computed tomography analysis. J Endod. 2017;43(4):638–42.
McMichael GE, Primus CM, Opperman LA. Dentinal tubule penetration of tricalcium silicate sealers. J Endod. 2016;42(4):632–6.
Moinzadeh AT, Zerbst W, Boutsioukis C, Shemesh H, Zaslansky P. Porosity distribution in root canals filled with gutta percha and calcium silicate cement. Dent Mater. 2015;31(9):1100–8.
DeLong C, He J, Woodmansey KF. The effect of obturation technique on the push-out bond strength of calcium silicate sealers. J Endod. 2015;41(3):385–8.
Camilleri J. Sealers and warm gutta-percha obturation techniques. J Endod. 2015;41(1):72–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Josette Camilleri declares that she has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Dental Restorative Materials
Rights and permissions
About this article
Cite this article
Camilleri, J. Will Bioceramics be the Future Root Canal Filling Materials?. Curr Oral Health Rep 4, 228–238 (2017). https://doi.org/10.1007/s40496-017-0147-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-017-0147-x