Abstract
Aims
Primary aim was to investigate the value and safety of contrast-enhanced ultrasonography (CEUS) during follow-up (FU) of splenic, hepatic and renal post-traumatic injuries in a pediatric population. Secondary aim was to extrapolate appropriate timing of FU-CEUS.
Methods
In a retrospective study, post-traumatic parenchymal injuries diagnosed with CT or CEUS, were subjected to non-operative management and followed with CEUS.
Results
Forty-six patients were enrolled, with isolated or combined injuries, for a total of 30 splenic, 15 hepatic and 12 renal injuries. At admission 42/46 patients underwent CT and 4/46 underwent CEUS. During FU a total of 65 CEUS were performed: 16 within 72 h to check delayed active bleeding or parenchymal rupture; 24 between 5 and 10 days post admission, to pose indication to active mobilization or to discharge; 21 between 20 and 60 days post admission to document complete healing of the lesion or pose indication to discharge in most severe injuries. No complications related to CEUS were encountered.
Conclusions
CEUS is valuable and safe to follow patients with post-traumatic abdominal injuries, even if further data are needed for renal injuries. We propose a tailored approach based on injury grade and clinical course: in the first 3 days only in case of delayed bleeding or rupture suspect; between 5 and 10 days post trauma to ensure a safe active mobilization and/or pose indication to discharge, and over 20–30 days post trauma to pose indication to discharge in most severe injuries or document complete healing and permit return to sport activities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The diagnostic accuracy of contrast-enhanced ultrasonography (CEUS) for the study of patients with abdominal trauma and for the detection of presence and extension of parenchymal lesions has been demonstrated [1,2,3,4], but little is known about its value in the follow-up (FU) of these patients. A few studies investigated this aspect [5,6,7,8,9,10], mainly in adult population. However, results are inconsistent, data in the pediatric population are scarce and guide-lines on when and how often perform FU checks are lacking.
In order to fill these gaps, our study was designed to investigate the role of CEUS during FU of splenic, hepatic and renal post-traumatic injuries in a consistent pediatric population. The primary outcome of this study was to evaluate the value and safety of CEUS in the FU of post-traumatic parenchymal injuries. Secondary aim was to extrapolate appropriate timing of FU imaging.
Materials and methods
We retrospectively reviewed the charts of all patients admitted for trauma to our operative unit, starting from 2002. Indeed, in 2002 we started to perform CEUS in patients with abdominal trauma to study or follow possible parenchymal lesions. We included in the study population only patients with blunt abdominal trauma causing splenic, hepatic or renal injury, who underwent at least one CEUS.
Data were collected regarding age, sex, trauma mechanism, injured organ/organs, associated lesions, diagnostic examinations performed at admission (“T0”: time zero) or during FU and their timing, possible side effects of CEUS, need of hemotransfusions or operative procedures such as pleural drainage or surgery (for the abdominal injury or other reasons).
Non-operative management (NOM) was applied to hemodynamically stable patients. Indications for operative procedures were: important pneumothorax or pleural effusion for pleural drainage; hemodynamic instability due to severe and persistent active bleeding and/or growing intra-parenchymal or intra-abdominal hematomas with risk of infection, for surgery.
In case of high-energy trauma in hemodynamically stable patients, contrast enhanced computer tomography (CE-CT) was performed at T0. In case of low-energy trauma, a CE-CT or a CEUS was performed at T0, based on preliminary baseline ultrasonography (US), clinical conditions, trauma mechanism and other involved districts. Injuries were graded according to the revised American Association for the Surgery of Trauma (AAST) organ Injury Scoring Scales (ISS) [11, 12].
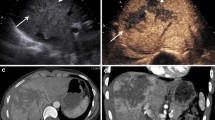
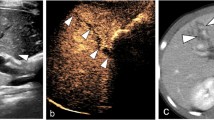
During FU, CEUS was performed to monitor possible complications, such as persistent or delayed bleeding and pseudoaneurysms (PA) or post-traumatic cysts formation, to pose indication to active mobilization and discharge of the patient, to monitor the healing of the lesions and ensure a safe reintroduction of sport activities, especially contact sports. Only in selected cases in which CEUS accuracy was not considered to be appropriate, CE-CT was repeated during FU.
T0-CEUS and early FU-CEUS were bedside performed, while late FU-CEUS were done in the office. CEUS was consistently performed by the same operator throughout the whole study period. CEUS was always done after baseline US of abdomen and pelvis, using the second-generation Ultrasound Contrast Agent (USCA) SonoVue® (Bracco, Milan, Italy) and a dedicated software. The USCA was administered intravenously and its amount depended both on the weight of the patient and on the number of organs to evaluate. According to FDA indications, a dose of 0.03 mL/Kg up to a maximum of 2.4 mL per injection was used [13]. USCA was usually administered in two split doses for T0-CEUS or FU-CEUS in case of multi-organ injuries, while a single dose was sufficient for FU-CEUS of single-organ injury. Sonovue® was “off label” used, after ethical committee’s approval and signed informed consent by parents. CEUS was contraindicated in patients with cardiac defects, history of severe allergy reactions or pulmonary hypertension.
Results
Between 2002 and July 2019, a total of 46 patients were admitted for blunt abdominal trauma with documented splenic, hepatic or renal injury and performed at least one CEUS. They were 33 males and 13 females. Median age was 11 years (age range 3–16). Out of 46, 21 had isolated splenic injury, 11 had isolated hepatic injury, three isolated kidney injury. The remaining 11 had combined lesions: seven combined splenic and left kidney injuries, two combined splenic and hepatic injuries and two hepatic and right kidney injuries. Overall there were 30 splenic, 15 hepatic and 12 renal injuries. Among splenic injuries, three were grade I, 11 were grade II, four were grade III, seven were grade IV, four were grade IV–V, and one was grade V. Among hepatic injuries, three were grade I, seven were grade II, three were grade III, and two were grade IV. Among renal injuries, five were grade I, one was grade II, one was grade III, and five were grade IV. Associated injuries were present in 21/46 patients: ten thoracic, eight neurologic, eight orthopaedic and two of the adrenal gland. The predominant mechanism of injury was fall off the bike in 14/46 cases, followed by road accidents in 10/46, fall from height in 7/46 (two off a wall, two down the stairs, one from a balcony, one out bed, one from a carousel), five sport accidents (two ski, one karting, one horseback riding, one soccer), ten others (six falls, one crush, one hit by train, one clash with other kid, one beaten by a schoolmate).
No patients had contraindications to perform CEUS. At T0 42/46 patients underwent CE-CT and 4/46 underwent CEUS. During FU 44/46 patients performed at least one CEUS: 32/44 performed one CEUS, 9/44 two CEUS, 1/44 three CEUS, 2/44 four CEUS. Regarding the timing of FU-CEUS, 16 were performed in the early FU (within 72 h after admission) to check delayed active bleeding or parenchymal rupture, based on clinical and laboratory findings; 24 were performed between 5 and 10 days post admission, to pose indication to active mobilization or to discharge; 21 were performed between 20 and 76 days post admission to document complete healing of the lesion or pose indication to discharge in most severe injuries. In 2/46 patient we did not perform FU-CEUS but only T0-CEUS was performed: they presented grade II splenic lesions, rapidly healing at the FU-US. In two cases a FU CE-CT was needed: in an obese boy with a IV–V grade splenic laceration we were more comfortable in repeating CE-CT 3 days post-trauma, then he performed two CEUS in the subsequent FU; in one patients with a grade IV renal laceration a CE-CT was performed 1 month post trauma to confirm a severe hypoperfusion of a hemi-kidney detected at FU-CEUS.
NOM was successful in 46/46 patients, as none required shift to operative treatment. Four/46 required blood transfusions, multiple in two cases. Seven/46 required operative treatments for other reasons: pleural drainage in 4 and orthopaedic surgery in 3. Median hospital stay was 12 days (range 6–24 days). During FU, one patient developed multiple splenic post-traumatic pseudoaneurysms. No side effects nor complications related to CEUS were encountered.
Discussion
Over the past two decades, there has been a shift toward NOM of patients undergoing a solid organ injury, thus requiring an increasing number of imaging studies to monitor potential complications and progressive healing of the lesions. The most used examination, since the very beginning, has been CE-CT. However, in consideration of the high number of children involved in blunt abdominal trauma, a need emerged to lower ionizing radiations exposure and potential adverse reactions to contrast media. At the same time, the introduction of CEUS improved US accuracy in general and US capability to detect and to better depict abdominal traumatic lesions, in particular. In details, as many studies reported [14,15,16], CEUS can easily highlight the number of detected lesions, enhancing some qualitative findings, such as lesion extension, margins, and its relationship with capsule and vessels. Moreover, over time, more refined software and USCAs have been developed, as well as operators’ confidence and ability have improved.
Many authors have investigated the beneficial role of CEUS for blunt abdominal trauma in the acute phase and demonstrated its extraordinary capabilities for detecting major hepatic, splenic and renal traumas [1, 2]. However, the usefulness of CEUS in high-energy traumas is limited by the need to perform whole-body CT for the purposes of neurological, thoracic and abdominal evaluation [6]. On the other side, in less severe and more localized traumas, CEUS could be a first-line imaging technique, even if literature data are controversial, with sensitivities of 90% and 41% both being reported. This remarkable variability depends not only on the operator’s skill and patient’s build but also on the patient’s clinical status, which may limit cooperation, and on the size and site of the lesion [6, 17, 18]. CEUS role seems to be really relevant in pediatric patients, as shown by Valentino et al. [19] who demonstrated that CEUS is almost as accurate as CT in the recognition of solid organ injuries. However, CEUS has shown some limits, such as the fact that it is operator-dependent, has a low panoramic view and a small operating window reducing visibility, and low capability to give useful information about some complications, such as abscesses, bilomas, lesions to the urinary tract and vascular complications, requiring the use of CE-CT [7, 20,21,22].
During the follow-up phase, these problems are in part overcome, as the lack of urgency and knowledge of the lesion site allows for a more detailed baseline US and selection of the best acoustic window for visualizing the region of interest. A CEUS examination may be performed subsequently, if needed [22,23,24]. If used in these conditions, CEUS achieves a detection power similar to that of CT or magnetic resonance imaging (MRI) while allowing real-time study of lesions [6]. However, the potential of CEUS for the detection of traumatic vascular injuries, including post-traumatic pseudoaneurysms, has not been clearly addressed [5, 17], while its low sensitivity for urinary tract lesions is fully known, because of lack of excretion of the contrast media by kidneys [3, 7].
No definitive data exist regarding complications rate and short- and long-term FU of patients subjected to NOM, and no clear indications regarding the most cost-effective imaging technique (US, Doppler-US, CEUS, CT scan) during FU. General surgeons tend to perform routinely imaging FU for children, differently from pediatric surgeons that only in selected cases suggest imaging FU, especially CE-CT [25]. Indeed, US or CEUS or Doppler-US FU seems reasonable to minimize the risk of life-threatening hemorrhage and its associated complications [23].
To our knowledge, a few studies reported the use of CEUS in the FU of blunt abdominal injuries and even less in exclusively pediatric population.
In the study by Manetta et al. [6], after a preliminary CE-CT, radiological monitoring of mild liver and spleen trauma, in a mixed adult and pediatric population, was performed by CEUS. CEUS was done at 12, 24 and 48 h after the trauma, together with laboratory parameters, to ensure a safe discharge from ICU to surgical ward. Following discharge, CEUS was performed at 30 days and, in the event of persistent structural parenchymal alterations related to the trauma, again at 90 days. In all cases, there was correlation between CT and early FU-CEUS in identifying lesion site, number and extent. Moreover, CEUS monitored the healing of the lesion until resolution. However, the small population of this study (11 patients), moreover a mixed adult and pediatric, limits very much its value.
Miele et al. [7] in 2015 compared MRI and CEUS in the FU of patients with blunt abdominal trauma managed conservatively. It was a mixed pediatric and adult population, with 27 (35%) pediatric patients. Their results showed that CEUS performed at 1 month from trauma missed only minimal or moderate organ injuries, without clinical implications, compared to MRI (3/15 in liver, 4/9 in spleen, and 3/14 in kidney). Moreover, this study confirmed also the low accuracy of CEUS in identifying adrenal and urinary tract lesions, both in the acute and in the FU period. However, we don’t suggest MRI as a valid alternative to systematically follow pediatric parenchymal injuries. MRI has some limits, indeed, such as the need to have compliant patients able to follow breath-hold commands during images acquisition, for a relatively long time, which is not always simple with pediatric patients; in some cases it requires sedation (for young pediatric patients) and it can’t be bedside-performed as CEUS.
In 2019, Tagliati et al. published three studies with the same adult population with splenic trauma, following patients with CEUS for a long time and very short time intervals [8,9,10]. In one paper the authors conclude that CEUS is a very useful imaging modality during FU of blunt splenic trauma non-operatively managed, allowing an efficient prediction of splenic injuries requiring only observation and monitoring during FU [8]. In another paper CEUS demonstrates to be valuable in detecting complications during NOM, such as delayed vascular injuries or active extravasation. The authors affirm that spleen injury complications could occur at any time—particularly in the first 7 days after trauma—but their incidence is not so frequent to justify several CT scans. Therefore, CEUS could fill this gap in diagnostic imaging and could represent the reference imaging modality in splenic injury FU [10]. In the third study CEUS was used to study mean spleen injury healing time and factors related to it: from the study emerged that AAST-SIS grade, subcapsular hematoma presence and spleen infarct development are significantly associated to healing time [9].
The only available study with a pure pediatric population is by Durkin et al. [5]. They followed with CEUS patients with splenic and hepatic injuries, even if in the majority of cases also CE-CT was performed at a median of 7 days post admission. Between 2002 and 2010 CEUS was performed only in case of symptoms; by 2011 CEUS was performed in every patient at 5–10 days post admission and then weekly, if needed. Seventeen out 101 children developed PA but only six developed symptoms. They concluded that FU imaging should be mandatory also in asymptomatic patients, as sudden acute rupture of PA is a well-recognized clinical scenario following an asymptomatic course. Their paper set off the reaction of several surgeons from United States [26], because routine screening of asymptomatic patients is not a widely accepted practice in the United States; moreover, experience with NOM showed it to be unnecessary, also because the majority of PA does not appear to be clinically relevant and spontaneously resolve. This argument is still matter of debate.
In summary, opinions regarding the need of FU examination in post-traumatic injuries are inconsistent, even if FU screening also in asymptomatic patients seem to be accepted and performed in Europe [5, 8,9,10]. However published experiences are few, most for hepatic and splenic injuries and in adult populations. Low experience is reported in pediatrics and for renal injuries.
Pediatric population suffers a higher risk of post-traumatic complications, compared to adults, because maintaining a bed rest is more difficult in the acute and post-acute phase and return to sport activity is requested with more urgency by children and families, in most of cases for contact sports. So, we prefer to document the complete healing of the lesion before removing contraindications to free sport activities. Using a radiation-free technique that we perform bedside or in our office and with negligible risk of side effects, we are confident this could be considered a valuable choice for our patients. Moreover, considering the economic point of view, great savings could be achieved using CEUS in the FU of already studied injuries. Lorusso et al. [27] performed a cost analysis comparing the use of CEUS to that of CT and MRI in the characterization of liver lesions, which showed that the cost of a CEUS was half the price of other diagnostic exams.
Regarding the timing of FU-CEUS, there are neither guidelines nor clear consensus. Manetta et al. performed early checks at 12, 24, and 48 h and late checks at 1 month and 3 months post-trauma [6]. Durkin et al. firstly posed indication to CEUS only in symptomatic cases, then considered better to perform a check at 5–10 days post admission and then weekly, if needed [5]. Tagliati et al. performed serial checks at short time intervals (1, 3, 8, 15, 30, 60, 90 and 180 days post-trauma) [8,9,10]. In our experience CEUS is a useful imaging technique to check early complications in the first 48–72 h post trauma, if needed; moreover it can be repeat to check the initial healing of the lesion or the hematoma status, in particular in splenic and hepatic parenchyma, to permit an initial mobilization of the child from bed after 5–10 days post-trauma, based on injury grade, and pose indication to discharge; eventually CEUS can be repeat for high grade injuries to monitor advanced healing at around 1 month post trauma or later, if necessary, to permit a safe return to sport activities. Anyway FU-CEUS should not follow a fixed schedule, but instead they should be tailored on injury grade and clinical course.
Conclusions
Our paper shows that CEUS is a valuable and safe imaging technique to follow patients with post-traumatic hepatic and splenic injuries. Even if we did not encounter complications in the management of renal injuries, a wider experience is needed to better depict the role of CEUS in NOM of renal trauma.
Regarding the timing of FU-CEUS, we propose a tailored approach based on injury grade and clinical course: in the first 3 days only in case of delayed bleeding or parenchymal rupture suspect; between 5 and 10 days post trauma to ensure a safe active mobilization and/or pose indication to discharge, and over 20–30 days post trauma to pose indication to discharge in most severe injuries and/or document complete healing and permit return to sport activities.
References
Zhang Z, Hong Y, Liu N et al (2017) Diagnostic accuracy of contrast enhanced ultrasound in patients with blunt abdominal trauma presenting to the emergency department: a systematic review and meta-analysis. Sci Rep 7:4446. https://doi.org/10.1038/s41598-017-04779-2
Laugesen NG, Nolsoe CP, Rosenberg J (2017) clinical applications of contrast-enhanced ultrasound in the pediatric work-up of focal liver lesions and blunt abdominal trauma: a systematic review. Ultrasound Int Open 3(1):E2–E7
Trinci M, Piccolo CL, Ferrari R et al (2019) Contrast-enhanced ultrasound (CEUS) in pediatric blunt abdominal trauma. J Ultrasound 22:27–40
Piccolo CL, Trinci M, Pinto A et al (2018) Role of contrast enhanced ultrasound (CEUS) in the diagnosis and management of traumatic splenic injuries. J Ultrasound 21(4):315–327
Durkin N, Deganello A, Sellars ME et al (2016) Post-traumatic liver and splenic pseudoaneurysms in children: diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS). J Pediatr Surg 5:289–292
Manetta R, Pistoia ML, Bultrini C et al (2009) Ultrasound enhanced with sulphur-hexafluoride-filled microbubbles agent (SonoVue) in the follow-up of mild liver and spleen trauma. Radiol Med 114(5):771–779
Miele V, Piccolo CL, Sessa B et al (2016) Comparison between MRI and CEUS in the follow up of patients with blunt abdominal trauma managed conservatively. Radiol Med 121(1):27–37
Tagliati C, Argalia G, Giuseppetti GM (2019) Contrast-enhanced ultrasound performance in predicting blunt splenic injuries requiring only observation and monitoring. Med Ultrason 21(1):16–21
Tagliati C, Argalia G, Graziani B et al (2019) Contrast-enhanced ultrasound in the evaluation of splenic injury healing time and grade. Radiol Med 124(3):163–169
Tagliati C, Argalia G, Polonara G et al (2019) Contrast enhanced ultrasound in delayed splenic vascular injury and active extravasation diagnosis. Radiol Med 124(3):170–175
Moore EE, Shackford SR, Pachter HL et al (1989) Organ injury scaling: spleen, liver and kidney. J Trauma 29(12):1664–1666
Kozar R, Crandall M, Shanmuganathan K et al (2018) Organ injury scaling 2018 update: spleen, liver and kidney. J Trauma Acute Care Surg 85(6):1119–1122
Lumason (2016) https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/203684s001lbl.pdf. Accessed 31 Aug 2019
Valentino M, De Luca C, Sartoni Galloni S et al (2010) Contrast-enhanced US evaluation in patients with blunt abdominal trauma. J Ultrasound 13:22–27
Miele V, Buffa V, Stasolla A et al (2004) Contrast enhanced ultrasound with second generation contrast agent in traumatic liver lesions. Radiol Med 108(1–2):82–91
Sessa B, Trinci M, Ianniello S et al (2015) Blunt abdominal trauma: role of contrast-enhanced ultrasound (CEUS) in the detection and staging of abdominal traumatic lesions compared to US and CE-MDCT. Radiol Med 120(2):180–189
Poletti PA, Becker CD, Arditi D et al (2013) Blunt splenic trauma: can contrast enhanced sonography be used for the screening of delayed pseudoaneurysm? Eur J Radiol 82:1846–1852
Catalano O, Aiani l, Barozzi L et al (2009) CEUS in abdominal trauma: a multi-center study. Abdom Imaging 34:225–234
Valentino M, Ansaloni L, Catena F et al (2009) Contrast-enhanced ultrasonography in blunt abdominal trauma: considerations after 5 years of experience. Radiol Med 114:1080–1093
Pinto F, Miele V, Scaglione M et al (2014) The use of contrast-enhanced ultrasound in blunt abdominal trauma: advantages and limitations. Acta Radiol 55(7):776–784
Pinto F, Valentino M, Romanini L et al (2015) The role of CEUS in the assessment of haemodynamically stable patients with blunt abdominal trauma. Radiol Med 120:3–11
Valentino M, Serra C, Zironi C et al (2006) Blunt abdominal trauma: emergency contrast-enhanced sonography for detection of solid organ injuries. AJR Am J Roentgenol 186:1361–1367
Minarik L, Slim M, Rachlin S et al (2002) Diagnostic imaging in the follow-up of nonoperative management of splenic trauma in children. Pediatr Surg Int 18(5–6):429–431
Regine G, Stasolla A, Miele V (2007) Multidetector computed tomography of the renal arteries in vascular emergencies. Eur J Radiol 64(1):83–91
Coccolini F, Montori G, Catena F et al (2017) Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 12:40
Letton RW, Campbell BT, Falcone RA et al (2017) Letter to the Editor: “Post-traumatic liver and splenic pseudoaneurysms in children: diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS)” by Durkin et al J Pediatr Surg 51 (2016) 289–292. J Pediatr Surg 52(2):367–368
Lorusso A, Quaia E, Poillucci G et al (2015) Activity-based cost analysis of contrast-enhanced ultrasonography (CEUS). Insights Imaging 6:499–508
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. AP performed all the CEUS examinations. Material preparation, data collection and analysis were performed by DR, MEM and GS. The first draft of the manuscript was written by DR and reviewed by GL and GL. All authors commented on previous versions of the manuscript. Supervision was conducted by PLC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This study involves human participants under 18 years of age; contrast media was “off label” used and informed consent was signed by parents/caregivers of children subjected included in the study.
Ethical approval
The study has been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975 and its late amendments.
Informed consent
Additional informed consent was obtained from all patients (by parents/caregivers) for which identifying information is not included in this article. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Renzo, D., Persico, A., Lisi, G. et al. Contrast-enhanced ultrasonography (CEUS) in the follow-up of pediatric abdominal injuries: value and timing. J Ultrasound 23, 151–155 (2020). https://doi.org/10.1007/s40477-019-00423-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00423-z