Abstract
Purpose
Idiopathic granulomatous mastitis is a rare relapsing benign inflammatory breast disease with unknown etiology. Its clinical features and imaging signs may mimic inflammatory breast cancer or some other inflammatory breast disease. This may interfere with correct and timely diagnosis and thus impose an additional burden on the costs of diagnosis and therapy, as well as patient anxiety. We aimed to characterize the imaging findings of this disease and introduce two new imaging signs.
Materials and methods
This prospective study examined 36 patients with imaging and a clinical diagnosis of mastitis granulomatosis who were untreated and then confirmed by pathology. Demographic information, clinical data, imaging findings, and signs were recorded.
Results
The age range of the patients was 22–60 years with an average of 36 years. Most of the patients (78%) were at reproductive age. None of the patients had a family history of granulomatous mastitis. Most patients with granulomatous mastitis (89%) lived in regions with low socioeconomic status. For most patients, sonography indicated a heterogeneous hypoechoic mass with irregular shape and ill-defined margin (26 cases; 72.2%). Focal asymmetry (36%) and obscured mass (36%) were the most common mammographic findings. Two signs of duct ectasia containing secretion and high-flow pseudocyst appearance were described.
Conclusion
Mammographic and ultrasound findings can highly suggest a diagnosis of granulomatous mastitis in an appropriate clinical context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic granulomatous mastitis (IGM) is a rare relapsing benign inflammatory breast disease that was described first by Kessler and Wolloch in 1972 [1]. The condition is called granulomatous lobular mastitis or non-puerperal mastitis [2]. Its etiology is unknown. One proposed mechanism involves a localized inflammatory response to leakage of protein and lipid-rich secretions or milk from the duct. Other potential etiologies include the autoimmune disease, oral contraceptive (OCP), unknown organisms, breast trauma, diabetes, cigarette smoking, galactorrhea, hyperprolactinemia, and alpha-1 antitrypsin deficiency [2,3,4]. There is a strong correlation between IGM and the history of pregnancy and lactation, with more patients having a pregnancy within 5 years before diagnosis [2].
Because of the diverse histopathologic features, radiological manifestations of IGM are both non-specific and different, but radiologists can suggest a diagnosis in appropriate clinical settings [1, 2]. Generally, granulomatous mastitis involves an inflammatory process of the breast that can mimic an inflammatory cancer or abscess [3]. Since the disease can mimic both clinically and radiologically breast cancer, there may be delays in obtaining correct and timely diagnoses. This can impose additional burdens in terms of diagnostic and therapeutic costs, as well as cause anxiety and concern for the patient. Therefore, correct and timely diagnosis of the disease is necessary.
It seems that IGM should be considered as an important item in the differential diagnosis of breast cancer to prevent extensive surgical excisions, at least in the referral centers. The diagnosis is based on the histological pattern and ruling out other granulomatous reactions, such as tuberculosis, sarcoidosis, granulomatosis with polyangiitis (formerly known as Wegener granulomatosis), fungal infections, and benign inflammatory lesions [2]. The diagnosis can be confirmed with a needle biopsy, which is much more accurate than fine needle aspiration (FNA) [2]. There is a low prevalence of granulomatous mastitis in Western countries, but a few other countries have a higher prevalence [2, 5, 6]. In this study, we present the imaging findings of a relatively large series of patients.
Materials and methods
This prospective study was approved by the institutional review board. The study included patients with imaging and a clinical diagnosis of untreated mastitis and a confirmed pathology of mastitis granulomatosis. Patients were excluded if they had a history of any other previous breast disease, biopsy, surgery, or chemotherapy. Cases were also excluded if they had any other type of mastitis, such as those related to infection, autoimmunity, and trauma. Ultimately, 36 subjects were included, and after explaining the research project to them, a predesigned written consent form was signed by all included cases.
Demographic information about the patients were recorded in the embedded forms, including age, educational level, marital status, type of residence, family history of similar diseases, history of breast cancer in first-degree relatives, history of pregnancy, duration of breastfeeding, history of hormonal use, and clinical complaints. Based on the clinician’s request, sonography was performed for all patients, and mammography was obtained for some of them who were 40 years old or beyond if they consented to undergo the procedure. Grayscale and color Doppler ultrasound was performed with a 9–12-MHz linear probe using an Esaote lab machine. The mammographic findings were obtained through digital images with a fully digital Hologic mammography device.
We collected and recorded ultrasound imaging findings, including the lesion’s location, shape, echo, margin, associated findings, axillary region, and BI-RADS results [7]. The mammographic findings of the location of the lesion, its shape, and BI-RADS were also recorded. All patients had a 14-gauge core needle biopsy. The pathology of these patients was followed up and recorded. In cases of any clinical suspicion of tuberculosis, a TB PCR test was also requested and carried out.
Results
The age range of patients was 22–60 years old with an average of 36 years. The majority were 30–40 years old (about 60%). All 36 patients underwent ultrasound, and 11 patients had mammographies. The pathologies of all the cases were confirmed by core needle biopsy. None of the patients had a history of collagen vascular disease, autoimmune disease, or diabetes.
All except one of the 36 patients were married. Most of the patients (78%) were at reproductive age and under 40 years old. None of the patients had a family history of granulomatous mastitis, and only one of them had a family history of breast cancer in one of their first-degree relatives. The classification of the patients with granulomatous mastitis based on educational levels is shown in Table 1.
Most patients with granulomatous mastitis (89%) lived in downstream areas, the suburbs of the capital city, or small towns around the capital city. Only 11% (4 people) were living within the capital city or other big cities. The classification of patients with granulomatous mastitis based on residence is shown in Table 2.
All participants except for one woman had a history of pregnancy (1–6 pregnancies with an average of 2). Except for three cases, all patients had a history of lactation with an average of 3–4 years. Two people were diagnosed with granulomatous mastitis during the lactation period, and the rest of the patients showed symptoms after the end of the lactation period. Furthermore, 56% of patients (20 out of 36) had a history of oral contraceptive intake, of which 10 had a history of taking hormones for less than 5 months, while 10 people took them for over 5 months.
The most common clinical complaints were palpable mass (75%) and mastalgia (73%). Other clinical complaints were reported as skin changes, fistulization, fever, and nipple inversion. The duration of patients’ symptoms was 1 week to 3 months before the imaging. In only two cases, both breasts were involved, while 94% had only one breast involved. Among the rest of the cases, 19 (53%) involved the left breast, and 15 cases (47%) involved the right breast.
Only five cases were in a retroareolar location or had retroareolar extension. The rest of the lesions were located in the peripheral part of the breast. The patients’ imaging was reported according to the Breast Imaging Reporting and Data System (BI-RADS) lexicon version 5 from the American College of Radiology (ACR) [6]. Most of the cases (80%) showed a mass in ultrasound. About 92% of the lesions (33 cases) had an irregular shape with an ill-defined or indistinct margin, while only 8% (3 people) had an oval shape with a circumscribed margin. Except for one case, all the lesions (97%) had a heterogeneous hypoechoic pattern.
Ultrasound findings showed a heterogeneous hypoechoic mass with irregular shape and an ill-defined margin in 26 cases (72.2%), while non-mass shape lesions occurred in seven cases (19.4%), and a heterogeneous hypoechoic mass with an oval and circumscribed shape occurred in three cases (8.3%). Of the 36 patients, 50% (18 patients) had a tubular extension, connecting tracts, and tunneling around the lesions. Fluid collection and floating debris were observed in 27.8% of the lesions (10 people). The presence of anechoic cystic components in the lesions was observed in only five cases (13.9%), while 30 cases (83.3%) had significant hypoechoic area with pseudocystic appearance. Ductal ectasia was reported in 9 of the 36 patients, of which 6 had it on the same side, 2 had it on both sides, and 1 had it on only the opposite side.
Color Doppler ultrasound was performed for all patients as part of sonography. In all cases, increased vascular structures were observed (both arterial and venous structures). Interestingly, even completely hypoechoic areas (with pseudocyst appearance) all had flow in simultaneous ultrasound. An increase in skin thickness was observed in 17% of the patients (6 cases), ultrasound indicated edema in 17% (6 cases) of the cases, and lymph nodes with a thick cortex occurred in 33% (12 patients). Of the 36 patients with ultrasound, 50% of the cases (18 patients) were classified as BI-RADS 4a, 22% (8 patients) were classified as BI-RADS 4, nearly 3% (1 patient) was classified as BI-RADS 4b, and 25% (9 patients) were classified as BI-RADS 3.
There were 11 patients who underwent mammography, and the findings are shown in Table 3. No evidence of suspicious microcalcifications was observed. Routine follow-up was recommended for the two patients classified as BI-RADS 1. This was because of dense breast tissue and overlapping tissue that obscured the lesions. Biopsy was recommended for the nine with BI-RADS 4a.
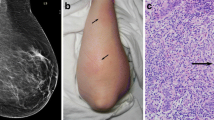
Most patients with retroareolar involvement were under 30 years of age, while cases over 30 years of age had peripheral lesions, and this relationship was statistically significant (P = 0.029). In addition, 27 people (75%) had an involvement of 1–3 quadrants, 5 patients (14%) had retroareolar lesions, and 4 (11%) had disseminated lesions in the breast. In patients with more pregnancies (> 3), a greater percentage of the lesions had cystic components, while patients with fewer pregnancies had a lower percentage of cystic components, and this difference was statistically significant (P = 0.021). The majority of patients showing significant edema in breast ultrasound were under 30 years of age, while most cases without significant edema were over 30 years of age, and this difference was statistically significant (P = 0.020). Figures 1 and 2 show various imaging features of the patients with a diagnosis of mastitis granulomatosis.
Discussion
There are various inflammatory diseases of the breast, which include puerperal mastitis, fat necrosis, breast infarction, plasma cell mastitis, collagen vascular disease, autoimmune, tuberculosis, and diabetic mastopathy. Granulomatous lobular mastitis is a rare, benign, inflammatory chronic disease of unclear etiology. According to the literature, it seems that the condition is more common in some countries in the Middle East, such as Iran and Turkey [5, 6, 8]. In various studies, the average age was 32–34 years, and most patients were at child-bearing age [2]. In our study, most patients (about 78%) were also at reproductive age and under 40 years of age. This contrasts with the higher mean age in cases of inflammatory breast carcinoma (with an average of 58 years), which is important to exclude in differential diagnosis [2].
All except for one case had a history of pregnancy, and all except for three cases had a history of lactation with an average for 3–4 years. This supports the strong relationship between granulomatous mastitis and the history of pregnancy and lactation, and the etiologic role of these factors has been highlighted [2, 9]. Only two people were diagnosed with granulomatous mastitis during the lactation period, and the rest showed symptoms after the end of lactation. According to most studies, the presentation of granulomatous mastitis during pregnancy and lactation is uncommon, and most IGM patients have symptoms at least 6 months to 2 years after lactation [2]. Approximately, 56% (20 of 36 patients) had a history of oral contraceptive use. This relationship may support the hypothesis that hormonal agents are one of the risk factors for IGM disease. However, in the study by Mehmet et al. only one patient had used oral contraceptives, and in studies by Ozel et al. and Neel et al., no patients had used them before [8, 10, 11]. None of the patients had a family history of granulomatous mastitis, and only one of them had a family history of breast cancer in one of their first-degree relatives. These findings are similar to those of previous studies, which did not show any genetic trends [2, 3, 5].
Most of the patients (about 92%) had lower levels of literacy and lower education (associate degree and lower). Most patients with granulomatous mastitis (about 89%) lived in downstream areas, the outskirts of the capital city, or small towns. Other studies have not examined the educational level and residency of patients and their relationships with granulomatous mastitis. However, due to the higher incidence of IGM in patients with lower educational level and those living in poor areas of the city and suburbs, these factors could be explored for their possible relations to etiologies. If their relationships could be confirmed in studies with larger sample sizes, they could help to reduce the incidence of granulomatous mastitis through education and the improvement of living and health conditions, such as the status of local water resources.
The most common clinical complaints were palpable mass (75%) and mastalgia (73%). According to several studies, the palpable mass has been reported as the most common clinical manifestation [5, 12,13,14]. In our study, other clinical complaints were reported as skin changes, fever, and nipple inversion. Most of the patients (19 cases, 53%) had left breast involvement. In the study by Omranipour et al., 43 patients (56%) reported involvement of the left breast, and 44% involved the right breast. In the study by Fatih et al., most cases 14 (53.8%) were seen in the right breast [5, 14] but several studies have reported more common occurrence in the right breast (61–69%) [2]. Bilateral breast involvement was observed in only two cases, and 94% of the cases had only unilateral breast involvement. According to most previous studies, bilateral cases are less frequent [1, 2, 5, 13].
Only 5 out of the 36 patients had retroareolar lesions. The rest of the lesions were in the peripheral breast, which is consistent with most studies [4, 6, 15]. Imaging features of mastitis granulomatosis are not specific and have a differential diagnosis with malignant lesions. Rare cases of simultaneous mastitis granulomatosis and breast cancer have been reported in the literature [16, 17]. So, histopathology is necessary to rule out cancer before proceeding to treatment [2, 18]. Based on our experience in a high-volume referral center in a country where IGM is not so rare [4,5,6, 8], we believe that although most of the imaging signs of IGM are non specific, it is possible to suggest a diagnosis using imaging features with an acceptable degree of certainty with a constellation of signs in the appropriate clinical context.
Furthermore, mammography and ultrasound are often sufficient for imaging evaluations of granulomatous mastitis and no other imaging modalities would be necessary.
The ultrasound findings are diverse in IGM. Various studies have reported that the most common manifestation is an irregular hypoechoic mass with tubular extension and interconnecting tracts [1, 2, 6, 15]. In our study, the most common ultrasound finding was an irregular, heterogeneous, significantly hypoechoic mass with an ill-defined border, which was seen in 26 cases (72.2%), while 50% of lesions had tubular extensions and subcutaneous tunneling.
Fluid collection and floating debris (28%) and ductal ectasia (25%) were other ultrasound findings in our cases that are valuable for the diagnosis of IGM and differentiation from cancer. Other sonographic findings were edema and increased skin thickness (17%) as well as lymph nodes with thick cortex but with a preserved normal shape (33%). However, these findings are not specific and can also be seen in malignant cases as well [2]. Most patients received a BI-RADS 4 classification in sonography reports. However, in the study by Yildiz et al., 27 cases were classified as BI-RADS 3, and 3 cases were classified as BI-RADS 4 in ultrasound [4].
There are two imaging findings in this study that we want to focus attention on, which have been given little attention in the literature. One of them is duct ectasia containing secretion, which was seen in 9 out of the 36 patients, of which 6 had it on the same side, 2 had it on both sides, and one had it on only the opposite side. This finding is in favor of the theory that an initial insult to the ductal epithelial cells starts a cascade of the breast inflammatory response with a spectrum of multiple inflammatory diseases (Fig. 3) [14]. This finding seems to be different from the inflammatory disease of mammary duct ectasia, which is more common in perimenopausal and postmenopausal women. In this condition, the ducts are central retroareolar, and the patient has less painful lesions [15].
Another important finding in our study was in the color Doppler ultrasound. In hypoechoic areas with floating debris, there was a high-flow pseudocyst appearance, which not only still had flow, it even showed increased flow compared to nearby normal tissue. These signs may be specific to IGM, although larger studies are required to confirm this finding (Fig. 4).
In most studies, focal asymmetry has been described as the most common mammographic presentation [2, 6, 13, 19]. In a small number of studies, an obscured or irregularly shaped mass has been reported as the most common mammographic finding [20]. In our study, both focal asymmetry (36%) and obscured mass (36%) were seen as the most common mammographic findings and had the same frequency. Other mammographic findings included two cases of false negative (normal) and one case of global asymmetry with trabecular thickening. No suspicious microcalcifications were observed in either (Table 4). As mentioned, IGM radiological symptoms overlap with locally advanced and inflammatory breast carcinoma. However, there are some differences between them that would make it possible to suggest IGM versus breast cancer (Table 5). The positive points of this study are the use of detailed imaging approaches and the acceptable number of cases. The study was conducted in a prospective manner, and all images were described by one radiologist specialized in breast imaging. Furthermore, the study focused on some less noticed points in the imaging of IGM. One limitation of this study is the number of cases, which was due to the rarity of the disease.
Conclusion
IGM is a rare inflammatory condition that mimics inflammatory breast carcinoma in clinical findings, which can lead to incorrect or delayed diagnosis. IGM imaging findings are diverse, but the diagnosis of granulomatous mastitis can be suggested in appropriate clinical conditions through ultrasound findings such as an irregular hypoechoic mass with ill-defined margin, along with tubular extensions and tunneling, as well as mammographic findings including focal asymmetry or an obscured mass. However, histopathology is required to confirm the diagnosis.
References
Kessler E, Wolloch Y (1972) Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 58(6):642–646. https://doi.org/10.1093/ajcp/58.6.642
Pluguez-Turull CW, Nanyes FE, Quintero CF et al (2018) Idiopathic granulomatous mastitis: manifestations at multimodality imaging and pitfalls. RadioGraphics 38:330–356. https://doi.org/10.1148/rg.2018170095
Pistolese CA, Di Trapano R, Girardi V, Costanzo E, Di Poce I, Simonetti G (2013) An unusual case of bilateral granulomatous mastitis. Case Rep Radiol 694697:6 pp https://doi.org/10.1155/2013/694697
Yildiz S, Aralasmak A, Kadioglu H et al (2015) Radiologic findings of idiopathic granulomatous mastitis. Med Ultrason 17(1):39–44. https://doi.org/10.11152/mu.2013.2066.171.rfm
Omranipour R, Mohammadi SF, Samimi P (2013) Idiopathic granulomatous lobular mastitis-report of 43 cases from Iran; introducing a preliminary clinical practice guideline. Breast Care (Basel) 8(6):439–443. https://doi.org/10.1159/000357320
Oztekin PS, Durhan G, Nercis Kosar P, Erel S, Hucumenoglu S (2016) Imaging findings in patients with granulomatous mastitis. Iran J Radiol 13(3):e33900. https://doi.org/10.5812/iranjradiol.33900
D’Orsi CJ, Mendelson EN, Ikeda DM et al (2013) Breast imaging reporting and data system, ACR BI-RADS, 5th edn. American College of Radiology, Reston
Velidedeoglu M, Kilic F, Mete B, Yemisen M, Gazioglu VCE, Ferahman M, Ozaras R, Yilmaz MH, Aydogan F (2016) Bilateral idiopathic granulomatous mastitis. Asian J Surg 39(1):12–20. https://doi.org/10.1016/j.asjsur.2015.02.003
Kadivar M, Rashidi S, Jollaii A, Dabiran S (2016) The frequency of idiopathic granulomatous mastitis and the underlying factors in recent 5-year period. Razi J Med Sci 23(143):18–25
Ozel L, Unal A, Unal E et al (2012) Granulomatous mastitis: is it an autoimmune disease? Diagnostic and therapeutic dilemmas. Surg Today 42:729–733. https://doi.org/10.1007/s00595-011-0046-z
Neel A, Hello M, Cottereau A et al (2013) Long-term outcome in idiopathic granulomatous mastitis: a Western multicentre study. QJM 106:433–441. https://doi.org/10.1093/qjmed/hct040
Akcan A, Öz AB, Dogan S, Akgün H, Akyüz M, Ok E, Gök M, Talih T (2014) Idiopathic granulomatous mastitis: comparison of wide local excision with or without corticosteroid therapy. Breast Care 9:111. https://doi.org/10.1159/000360926SejalS
Fazzio OT, Shah SS, Sandhu NP, Glazebrook KN (2016) Idiopathic granulomatous mastitis: imaging update and review. Insights Imaging 7:531–539. https://doi.org/10.1007/s13244-016-0499-0
Altintoprak F, Karakece E, Kivilcim T et al (2013) Idiopathic granulomatous mastitis: an autoimmune disease? Sci World J 2013:148727. https://doi.org/10.1155/2013/148727
D’Alfonso TM, Ginter PS, Shin SJ (2015) A review of inflammatory processes of the breast with a focus on diagnosis in core biopsy samples. J Pathol Transl Med 49(4):279–287. https://doi.org/10.4132/jptm.2015.06.11
Oddó D, Domínguez F, Gómez N, Méndez GP, Navarro ME (2019) Granulomatous lobular mastitis associated with ductal carcinoma in situ of the breast. SAGE Open Med Case Rep 7. https://doi.org/10.1177/2050313x19836583
Özşen M, Tolunay Ş, Gökgöz MŞ (2018) Case report: ductal carcinoma in situ within a granulomatous mastitis. Eur J Breast Health 14(3):186–188. https://doi.org/10.5152/ejbh.2018.3894
Kiyak G, Dumlu EG, Kilinc I et al (2014) Management of idiopathic granulomatous mastitis: dilemmas in diagnosis and treatment. BMC Surg 14(1):66. https://doi.org/10.1186/1471-2482-14-66
Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G (2009) Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR 193:574–581. https://doi.org/10.2214/AJR.08.1528
Aghajanzadeh M, Hassanzadeh R, Sefat SA, Alavi A, Hemmati H, Delshad MSE et al (2015) Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast 24(4):456–460. https://doi.org/10.1016/j.breast.2015.04.003
Funding
Nothing to declare.
Author information
Authors and Affiliations
Contributions
Study concept and design: AA; acquisition of data: AA, FA; data analysis: FA; interpretation of data: AA, FE; drafting of the manuscript: FA; critical revision of the manuscript for important intellectual content: AA, FE
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical approval
Ethical approval has been approved by Tehran University of medical Science, Research ethics committee. The approval ID is IR.TUMS.IKHC.REC.1396.3845.
Financial disclosure
None of the authors have any financial interests relevant to the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alikhassi, A., Azizi, F. & Ensani, F. Imaging features of granulomatous mastitis in 36 patients with new sonographic signs. J Ultrasound 23, 61–68 (2020). https://doi.org/10.1007/s40477-019-00392-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00392-3