Abstract
Background
Point of care ultrasound (POCUS) is a useful diagnostic tool in medicine. POCUS provides an easy and reproducible method of diagnosis where conventional radiologic studies are unavailable. Telemedicine is also a great means of communication between educators and students throughout the world.
Hypothesis
Implementing POCUS with didactics and hands-on training, using portable ultrasound devices followed by telecommunication training, will impact the differential diagnosis and patient management in a rural community outside the United States.
Materials and methods
This is an observational prospective study implementing POCUS in Las Salinas, a small village in rural western Nicaragua. Ultrasound was used to confirm a diagnosis based on clinical exam, or uncover a new, previously unknown diagnosis. The primary endpoint was a change in patient management. International sonographic instructors conducted didactic and practical training of local practitioners in POCUS, subsequently followed by remote guidance and telecommunication for 3 months.
Results
A total of 132 patients underwent ultrasound examination. The most common presentation was for a prenatal exam (23.5 %), followed by abdominal pain (17 %). Of the 132 patients, 69 (52 %) were found to have a new diagnosis. Excluding pregnancy, 67 patients of 101 (66 %) were found to have a new diagnosis. A change in management occurred in a total of 64 (48 %) patients, and 62 (61 %) after excluding pregnancy.
Conclusion
Implementing POCUS in rural Nicaragua led to a change in management in about half of the patients examined. With the appropriate training of clinicians, POCUS combined with telemedicine can positively impact patient care.
Sommario
Background
La diagnostica ecografica (POCUS) é un utile strumento diagnostico in medicina. Fornisce un metodo semplice e riproducibile di diagnosi, dove studi radiologici convenzionali non siano disponibili. Anche la telemedicina é un grande mezzo di comunicazione tra docenti e studenti di tutto il mondo.
Ipotesi
L’implementazione della POCUS con formazione didattica diretta, utilizzando ecografi portatili, seguita da una formazione attraverso la telecomunicazione, avrà un impatto nella diagnosi differenziale e nella gestione del paziente in una comunità rurale fuori degli Stati Uniti.
Materiali e Metodi
Presentiamo uno studio prospettico sull’implementazione della POCUS a Las Salinas, un piccolo villaggio rurale del Nicaragua occidentale. L’ecografia è stata utilizzata per confermare la diagnosi clinica, o per nuove diagnosi. Il punto primario era un cambiamento nella gestione del paziente. Istruttori internazionali hanno condotto una formazione didattica pratica locale, poi seguita da una guida a distanza con telecomunicazione, per tre mesi.
Risultati
Un totale di 132 pazienti sono stati sottoposti ad esame ecografico. L’esame più comune era per la diagnostica prenatale (23,5 %), seguito dal dolore addominale (17 %). Dei 132 pazienti, 69 (52 %) hanno avuto una nuova diagnosi. Nella diagnosi di esclusione di gravidanza 67 pazienti su 101 (66 %) hanno avuto una nuova diagnosi. Un cambiamento nella gestione si è verificato in un totale di 64 (48 %) pazienti, e in 62 (61 %) dopo aver escluso la gravidanza.
Conclusione
L’implementazione della POCUS nelle zone rurali del Nicaragua ha portato ad un cambiamento di gestione in circa la metà dei pazienti esaminati. Con la formazione adeguata dei medici, la POCUS, combinata con la telemedicina, può avere un impatto positivo nella cura del paziente.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As an evolving component of medicine, point of care ultrasound (POCUS) spans across multiple specialties and applications, such as military medical personnel, trauma evaluation, pediatric emergency departments and neonatal intensive care units, and even expanding its utility to aerospace science [1–8]. Recent studies have described POCUS as being easily taught to medical personnel with a high degree of accuracy [1, 9, 10]. Medical schools have integrated ultrasound into their teaching curriculum, and students are using it from basic anatomy to advanced imaging as an adjunct to diagnosis and physical examination [11, 12]. The use of POCUS in the pre-hospital setting is also increasing as an aid to early diagnosis and medical decision-making [13].
Its ease of use and reproducibility make it feasible to diffuse into smaller, rural communities with otherwise limited diagnostic resources [14, 15]. Further characteristics of POCUS, including a focused and goal-directed evaluation, an easily learned, quickly performed, and reproducible exam make it an ideal diagnostic tool to teach medical personnel in underserved areas of the world [16].
Telemedicine has become an integral part of the expanding medical community and a viable means of disseminating information to rural or difficult to access communities [17]. Telemedicine has helped expand ultrasound access and utility to even the most distant places in earth and aerospace including the international space center [18]. Little, however, has been described in the experience of combining POCUS training along with telemedicine in the rural community.
The aim of this study was to evaluate the feasibility of implementing a focused POCUS curriculum followed by telecommunication and the impact on patient care in a rural community setting.
Methods
This was a two-phase observational prospective study implementing POCUS in the community of Las Salinas, Nicaragua. Las Salinas is a small rural village with the closest major hospital over 7 h away by car. The Las Salinas one-room medical clinic was staffed by a charge nurse and nursing assistant to serve patients that traveled up to several hours to the clinic for medical care. The clinic has basic medical equipment; however, there is no medical imaging readily available. Any necessary ultrasound requires travel to a hospital where the price of imaging is per frame and the images are very limited.
The first phase of the study provided instruction in POCUS. The instructor team consisted of experienced ultrasonographers from different parts of the world (ultrasound mission group) accompanied by a local humanitarian mission, Mission of Grace, that provided personnel and equipment. An ultrasound machine (Sonosite, Titan, Seattle, WA, USA) was donated to the village clinic by the mission group. Three laptop computers were also donated by Mission of Grace to the project where they were stationed in Las Salinas.
Training was provided during daily morning didactic sessions and practical ultrasound workshops, followed by afternoon ultrasound scans of patients from the community. Table 1 demonstrates components of the ultrasound examination included in training. An ultrasound instructor proctored each patient encounter. The clinic trainees were provided with an ultrasound manual outlining the elements of the POCUS examination translated into Spanish, Fig. 1 [19]. The Nicaraguan personnel trained were two post-graduate physicians rotating in rural medicine, a head clinic nurse, as well as a nursing assistant. As the Nicaraguan clinicians evaluated each patient, a working diagnosis was established. Each patient was then evaluated using POCUS. The initial diagnosis was either confirmed or a new diagnosis was obtained based on the ultrasound findings. These new findings may or may not have lead to a change in management. A change in management was a new medical decision that was previously unplanned and was based on the ultrasound findings.
Phase II of the study took place over the subsequent 3 months via telemedicine communication network. The ultrasound images from Nicaragua were viewed real-time on a computer screen using epiphany technology through Epiphan VGA2USB (Ottawa, Ontario, Canada) by one of the ultrasound instructors. The instructors provided remote guidance via voice-over IP service Sky-Peer-to-Peer (Skype, 2003) once a week for 3 months for about 60–90 min each session. Examinations were initially guided by remote personnel until the clinicians in Nicaragua became adept in the examination. At that point, the ultrasound reviewer was able to grade the examination on a scale of 1–10 based on proficiency, where 1 was not proficient to 10 being highly proficient. Documentation of the ultrasound exam was done on a standardized work flow sheet. A sample examination worksheet can be seen in Fig. 2a along with examples of images through telecommunication in Fig. 2b. The report sheet was listed in Spanish for clinicians in Nicaragua and translated into English.
Data analysis
Analysis was performed using SAS 9.2 (Cary, NC, USA). Patient symptoms and diagnosis were used as descriptive variables. These were given as a number (%) for categorical variables and as Mean ± standard deviation (Min, Max) for continuous variables.
The proportion of patients who had a change in the management and the proportion of patients who had a new diagnosis after the ultrasound were calculated, along with 95 % confidence intervals for each. These were calculated with all patients included and also with the exclusion of pregnant patients. The exclusion of pregnant patients was based on the fact that most women knew they were pregnant upon presentation and wanted a prenatal examination, including the sex of the child. There was no new diagnosis in this group of patients.
Results
Throughout Phase I and II, a total of 132 patients were examined using POCUS. Pregnancy was the most common reason for patients presenting to the clinic prior to an ultrasound exam (23 %), followed by abdominal pain (17 %). After POCUS was performed, no pathology was identified in 43.9 % of patients, while ovarian cyst (6 %) and kidney stone (5 %) were the most common findings identified. The most common additional symptoms and diagnosis are described in Table 2.
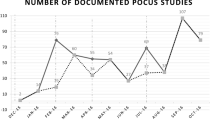
Fifty-two percent of patients had a new diagnosis after POCUS was performed, with a confidence interval of 44–61 %. New diagnosis led to change in management in 48 % (CI 40–57 %) of the patients, described in Table 3, Fig. 3. After excluding patients who were presented for prenatal checkup, the estimate of patients who had a new diagnosis after POCUS was 66 % (CI 57 %–76), and 61 % underwent a change in management (CI 52–71), as demonstrated in Table 4.
Seventy (52 %) of the 132 examinations were rated by the remote examiner. The scores ranged from 5 to 8.5 on a 1–10 rating scale. The average rating was 6.85 overall. The average rating for the first 6 weeks of the examinations was 6.54, and the average rating for the second 6 weeks of the exams rated was 7.17. Figure 4 demonstrates the trend in improvement of the performance score as the number of examinations reviewed increased.
Discussion
Curriculum and didactics are being implemented in emergency medicine, medical schools, and critical care programs throughout the United States and internationally with a high degree of accuracy and retention [1, 9, 10, 20–22]. Many programs are also being offered for postgraduate studies and for clinicians in the field. Mandavia et al. [9] looked at junior residents with limited previous knowledge of ultrasonography. After a two-phase didactic and practical training curriculum, residents were 94.6 % accurate in making a diagnosis based on POCUS findings. This demonstrated the ability of POCUS to be taught to clinicians with limited previous experience.
Pregnancy and prenatal visits were the most common patient encounters in Las Salinas. Patients presented to the clinic for a prenatal examination and to learn the sex and health of the fetus. Obstetric ultrasound is one component of the ultrasound examination that is teachable and reproducible [15]. Kimberly et al. [15] trained midwives in rural Zambia with a focused maternal ultrasound curriculum. They demonstrated an overall improvement in ultrasound skills of the midwives with a 17 % change in management based on ultrasonographic findings.
As ultrasound machines are becoming smaller and more portable, the utility of POCUS will continue to expand to remote places throughout the world where other imaging modalities are not readily available [14, 15, 23, 24]. Shah et al. [14] chose two rural hospitals in Rwanda to participate in a pilot ultrasound training program. A pre-study survey of local physicians identified the needs assessment of various ultrasound scans so didactic lectures could be tailored accordingly. Prior to the study intervention, the majority of physician ultrasound experience was in obstetrics and the average number of hours previously trained in ultrasound was <4. Barriers to obtaining ultrasound services included distance, cost of transfer, lack of monitoring, time for transfer, and price. Lectures and proctored curriculum were then implemented for a 9-week period, and an ultrasound machine was provided to each hospital. Afterward, one physician at each site was entrusted with the takeover of the ultrasonography program and its upkeep, which was found to be essential for the continuation of the program. Web-based teaching tools were also found to be valuable for ongoing quality assurance. Thus, ultrasound was concluded to be a teachable skill, useful for diagnosis and patient care in a rural setting.
A previous lack of international standardized ultrasound training prompted Neri et al. to propose an international ultrasound curriculum for critical care [20]. A modified international ultrasound curriculum was the basis for the ultrasound training to the Nicaraguan clinicians (Table 1). After the Nicaraguan trainees underwent Phase I, they were able to successfully scan patients and provide a diagnosis to guide their management with proctored help during Phase II. Over the course of the project, the influence of POCUS on identifying diagnosis was over 60 %. The ability and proficiency for using POCUS had an overall trend to improvement over the study period (Fig. 4).
Implementing an ultrasound program into a resource-limited area, like Las Salinas, leaves many logistic concerns. First and foremost, is there electricity to power the ultrasound machine? In a study by Blavais et al. [23], battery-powered ultrasound machines (Sonosite 180 Plus) were taken into the Amazon jungle with the premise of changing patient management. Of the 25 patients scanned, 28 % underwent a change in management. We identified a 62 % influence of POCUS leading to a change in management. The increase is multi-factorial; particularly the implementation of an ultrasound curriculum and the additional telemedicine reviews that improved performance of POCUS.
Internet connection is also an obstacle, although most remote areas are using wireless technology and it is becoming more accessible. Sustainability of the ultrasound machine is another concern. A person needs to be assigned to maintain some degree of upkeep. The machine needs to stay clean and de-contaminated. There is also care that goes into keeping it protected from theft and vandalism. With logistics being a barrier to any rural ultrasound program implemented, POCUS with telemedicine is a well-established tool for diagnostic evaluation and can be helpful in areas where other imaging is not readily available and wireless technology is becoming more accessible.
Conclusion
Ultimately, with appropriate didactic teaching and practical application and telemedicine, POCUS can be disseminated throughout rural areas of the world and implemented into everyday practice. Its use as a diagnostic adjunct to physical examination in places where other imaging modalities are not available can be invaluable. Training in POCUS for rural clinicians may provide the confidence for new diagnosis and even lead to a change in management in over half of the patients examined.
References
Langlois S (2007) Focused ultrasound training for clinicians. Crit Care Med 35(5):S138–S143
Evans N, Gournay V, Cabanas F et al (2001) Point-of-care ultrasound in the neonatal intensive care unit: international perspectives. Semin Fetal Neonatal Med 16(1):61–68
Vieira RL, Hsu D, Nagler J et al (2013) Pediatric emergency medicine fellow training in ultrasound: consensus educational guidelines. Acad Emerg Med 20(3):300–306
Dulchavsky SA, Henry SE, Diebel LN (2002) Advanced ultrasonic diagnosis of extremity trauma: the FASTER examination. J Trauma 53(1):28–32
Hile DC, Morgan AR, Laselle BT, Bothwell JD (2012) Is point-of-care ultrasound accurate and useful in the hands of military medical technicians? A review of the literature. Mil Med 177(8):983–987
Royse CF, Canty DJ, Faris J et al (2012) Core review: physician-performed ultrasound: the time has come for routine use in acute care medicine. Anesth Analg 115(5):1007–1028
Cohen JS, Teach SJ, Chapman JI (2012) Bedside ultrasound education in pediatric emergency medicine fellowship programs in the United States. Pediatr Emerg Care 28(9):845–850
Emergency Ultrasound Fellowship Programs. 2013. http://www.eusfellowships.com/programs.php. Accessed 1 June 2014
Mandavia DP, Aragona J, Chan L et al (2000) Ultrasound training for emergency physicians—A prospective study. Acad Emerg Med 7:1008–1014
Hoppman R, Rao V, Poston MB et al (2011) An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J 3(1):1–12
Swamy M, Searle RF (2012) Anatomy teaching with portable ultrasound to medical students. BMC Med Educ 22(12):99
Mouratev G, Howe D, Hoppmann R et al (2013) Teaching medical students ultrasound to measure liver size: comparison with experienced clinicians using physical examination alone. Teach Learn Med 25(1):84–88
Chin EJ, Chan CH, Mortazavi R et al (2013) A pilot study examining the viability of a Prehospital Assessment with Ultrasound for Emergencies (PAUSE) protocol. J Emerg Med 44(1):142–149
Shah S, Noble VE, Umulisa I et al (2008) Development of an ultrasound training curriculum in a limited resource international setting: successes and challenges of ultrasound training in rural Rwanda. Int J Emerg Med 1(3):193–196
Kimberly HH, Murray A, Mennicke M et al (2010) Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol 36(8):1267–1272
Kendall JL, Hoffenberg SR, Smith RS (2007) History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med 35(5):S126–S130
Alajmi D, Almansour S, Househ MS (2013) Recommendations for implementing telemedicine in the developing world. Stud Health Technol Inform 190:118–120
Marchburn TH, Hadfield CA, Sargsyan AE et al (2014) New heights in ultrasound: first report of spinal ultrasound from the international space station. J Emerg Med 46(1):61–70
Killu K, Dulchavsky S, Coba V (2010) The ICU ultrasound pocket book. Medical Imagineering 2010, iTunes, Rochester, NY
Neri L, Storti E, Lichtenstein D (2007) Towards ultrasound training curriculum for critical care medicine. Crit Care Med 35(5):S290–S304
Tanzola RC, Walsh S, Hopman WM et al (2013) Brief report: focused transthoracic echocardiography training in a cohort of Canadian anesthesiology residents: a pilot study. Can J Anaesth 60(1):32–37
Price S, Via G, Sloth E et al (2008) Echocardiography, practice, training and accreditation in the intensive care: document for the World Interactive Network Focused on Critical Ultrasound (WINFOCUS). Cardiovasc Ultrasound 6:49
Blaivas M, Kuhn W, Reynolds B, Brannam L (2005) Change in differential diagnosis and patient management with the use of portable ultrasound in a remote setting. Wilderness Environ Med 16(1):38–41
Conlon R (2012) Teaching ultrasound in tropical countries. J Ultrasound 15(3):144–150
Conflict of interest
The authors on this manuscript have no disclosures or conflicts of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to enrollment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kolbe, N., Killu, K., Coba, V. et al. Point of care ultrasound (POCUS) telemedicine project in rural Nicaragua and its impact on patient management. J Ultrasound 18, 179–185 (2015). https://doi.org/10.1007/s40477-014-0126-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-014-0126-1