Abstract
Aim
To improve the oral health of children and teenagers with autism spectrum disorder (ASD) by using an iPad®-based training programme.
Methods
Fifty-two children and teenagers with ASD (aged 3–19 years) educated in schools or in care centres participated in this cohort study and followed for 8 months. A training programme for teaching toothbrushing behaviours was proposed to the educational staff. Quotation grids enabled assessment of the programme’s efficacy.
Results
Showed an improvement in toothbrushing. The children’s autonomy increased and oral care was more easily implemented when steps were taken by the caregivers. Wilcoxon analysis showed significant improvement in each variable related to toothbrushing.
Conclusions
The iPad® is an attractive and easy device for people with ASD to use. Its use in a training programme for teaching toothbrushing behaviours was efficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a persistent neurodevelopmental condition with early childhood onset. ASD is characterised by a number of symptoms: impairments in social interactions and communication; restrictive, repetitive patterns of behaviour, interests or activities; and unusual sensory interests or sensitivities (American Psychiatric Association).
People with ASD are more likely to have behavioural difficulties regarding dental care (Stein et al. 2012; Weil et al. 2012; Lewis et al. 2015). Common behaviour-related barriers to dental care include the fact that children with ASD are prone to agitation, self-injury and emotional dysregulation. Hypersensitivity to sensory input (Baranek et al. 2007; Stein et al. 2013), which can be seen in their excellent attention to details (Baron-Cohen et al. 2009), can also interfere with dental and oral care. These features make it difficult for parents to care for their children’s teeth and for professionals to examine and treat children with ASD (Stein et al. 2012; Nelson et al. 2015). Compliance with regular oral hygiene may be difficult for children with ASD and for their parents (Bishop et al. 2013). These barriers are the underlying reasons for the unmet dental care needs of children with ASD as described by different studies (Brickhouse et al. 2009; Lai et al. 2012). Parents often give up toothbrushing and poor oral hygiene seems to be common in children with ASD (Loo et al. 2009; Marshall et al. 2010; Jaber 2011; Delli et al. 2013; Gandhi and Klein 2014). However, preventive measures (like toothbrushing) are essential for people with ASD, as they are considered at high risk for developing caries (Marshall et al. 2010; American Academy of Pediatric Dentistry 2013).
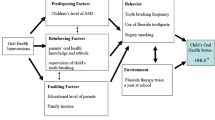
Learning new skills can be a challenge for children with ASD. We must use adapted strategies that have proven effective for these patients. Behavioural approaches can be of use. In a dental hygiene context, the use of these procedures has the potential to improve the results of traditional behavioural management (Kemp 2005; Marshall et al. 2010; Udhya et al. 2014). Different studies have also shown that visual pedagogy is a useful practice for children with ASD. Visual support is beneficial because these children process visual information better than auditory information (Hernandez and Ikkanda 2011; Knight et al. 2015). Some recent studies have also demonstrated that numeric devices (e.g., the iPad®) can be integrated into a learning programme for people with ASD, as the devices are efficient (Kagohara et al. 2013). The devices can facilitate the four key components (i.e., attention, retention, production, and motivation; Bandura 1977), are easy to use, and have become a common tool in many families.
Some authors have proposed training programmes for teaching toothbrushing behaviours using visual pedagogy and behavioural approaches (Pilebro and Bäckman 2005; Dias et al. 2010; Asma’a et al. 2013; Bishop et al. 2013; Popple et al. 2016). However, to the best of knowledge, no study has investigated teaching toothbrushing behaviours by breaking down the process into several steps using a digital tool, evaluating the success, difficulties and autonomy of the patients along the way. The aim of this study was to evaluate a training programme for teaching toothbrushing behaviours using an iPad® and a digital application based on these considerations.
Methods
Participants
Participants with ASD were recruited in different education centres located in the region of Nantes, France. Parents received an informative letter and oral explanation of the study. Fifty-five autistic patients (aged 3–19 years) educated in seven different schools or care centres were included in this cohort study. Written consent was obtained from each participant’s parents. During the programme, one child moved from the original care centre and two children missed more than 25% of the training sessions. The remaining 52 patients completed the programme and their data were analysed.
Training programme
Visual activity schedules were created on an iPad using an application called çATED. The çATED app is a digital diary used to help patients with autism to be more independent. Pictograms or photos can be personalised and autistic patients can organise their activities. The app allows the breakdown of a complex activity into several easy steps to complete. Several pictograms and photos were elaborated by the research team and were chosen with children and/or caregivers. The visual activity schedule for toothbrushing included 16 photos or pictograms for children up to 6 years old (Fig. 1). For children under 6, 12 pictograms or photos were inserted into the application (photos 9–13 were excluded).
Over 8 months, each participant met once per week with a dentist for toothbrushing training using the çATED app on an iPad. The training programme was conducted in the school or in the care centre and consisted of two different but complementary approaches, each of which were performed once a week with the research team: “table work” (pedagogic models of toothbrushing and the mouth, including sequence chronology, locating the different dental surfaces to brush, and understanding of pictograms) and “real-life” exercises (children’s toothbrushing activities in the bathroom). The other days of the week, after the children had lunch, their caregivers oversaw toothbrushing training using the app.
Evaluation
The participants were evaluated at the beginning of the study (baseline, T0), after 4 months (T1), and after 8 months (T2). Evaluations by a dentist were assessed using grids and scales, measuring achievement of the different steps and autonomy.
The 16 pictograms for toothbrushing are associated with 25 steps: 1: take the brush; 2: open the toothpaste; 3: press the toothpaste; 4: put toothpaste on the brush; 5: close the toothpaste; 6: brush the right lower occlusal surfaces; 7: brush the left lower occlusal surfaces; 8: brush the left upper occlusal surfaces; 9: brush the right upper occlusal surfaces; 10: brush the right lower buccal surfaces; 11: brush the front of the lower buccal surfaces; 12: brush the left lower buccal surfaces; 13: brush the right upper buccal surfaces; 14: brush the front of the upper buccal surfaces; 15: brush the left upper labial surfaces; 16: brush the right lower lingual surfaces; 17: brush the front of the lower lingual surfaces; 18: brush the left lower lingual surfaces; 19: brush the right upper lingual surfaces; 20: brush the front of the upper lingual surfaces; 21: brush the left upper lingual surfaces; 22: spit; 23: rinse the brush; 24: store the toothbrush and toothpaste; 25: wipe the mouth. Children under six years were not evaluated on steps 11–21.
For each step, autonomy was evaluated by attributing scores on quotation grids depending on whether the step was achieved alone, not achieved, or achieved with assistance.
1: Step was not performed; step was not achieved.
2: Step was performed by a caregiver with difficulty because the child was uncooperative.
3: Step was performed by a caregiver easily; the child was cooperative.
4: The child performed the step alone but with help (verbal or/and gestural assistance).
5: The child performed the step alone without help (verbal or gestural assistance); the step was achieved by the child.
The 25 steps were independently studied and grouped based on more general dimensions: toothbrushing preparation (steps 1–5), brushing of occlusal surfaces (steps 6–9), brushing of buccal surfaces (steps 10–15), brushing of lingual surfaces (steps 16–21) and the end of toothbrushing (steps 22–25). A global autonomy score for toothbrushing was also calculated for all the 25 steps. Scores of these dimensions were calculated by adding scores obtained in each step of the of the toothbrushing procedure (preparation, occlusal, buccal, lingual and end), and then dividing the global scores by the number of steps (5, 4, 6, 6, and 4 steps, respectively). These scores were defined as follows: SPrep (score for preparation), SOcc (score for brushing the occlusal surfaces), SBuc (score for brushing the buccal surfaces), SLing (score for brushing the lingual surfaces), SEnd (score for the end of toothbrushing). For instance, SPrep was calculated as follows: SPrep = (∑scores steps 1–5)/5). A total score was calculated by adding the 25 steps together. This score, defined as the score of autonomy (SAut), represents the autonomy of the child during toothbrushing.
Statistical analyses
Mean scores were calculated for each individual score of toothbrushing (SPrep, SOcc, SBuc, SLing, SEnd and SAut).
Due to the nature of the design and data, which were not normally distributed, the paired sample Wilcoxon signed rank test was used to compare the results and determine the significance of differences between the variables. The Bravais Pearson test was used to assess the correlation between variables. The statistical software SPSS version 16.0 was used for statistical analyses.
Results
The study sample included 7 girls and 45 boys, representing 13% and 87% of the total number of the participants, respectively. The mean age was 10.2 years old. Twenty-five percent of the children were under 6 years of age, 46% were 6–12 years old and 29% were 13–19 years old.
Baseline
Based on dentist evaluations, no child in the study achieved toothbrushing because no one performed the 25 steps of toothbrushing alone without any type of assistance (Fig. 2). Brushing of the various teeth surfaces (steps 6–21) was less commonly achieved than the preparation or ending steps. Brushing of the lingual surfaces was the most difficult and no child succeeded alone during these steps.
Autonomy during toothbrushing at T0 (beginning of the experiment). The 25 steps of toothbrushing are described with the different scores detailed in “Methods”
Longitudinal survey
The results showed that the cohort in this study gained autonomy during toothbrushing.
During several evaluations, it was observed that children were able to perform more steps alone and omitted less steps. If we consider the number of steps omitted by some children, at the beginning of the programme, 17 were omitted. After 8 months, only one step (spitting) was omitted by some of the children. Brushing of the buccal and lingual surfaces remained difficult for children to perform, but total failures (a score of one in all the component steps) decreased progressively (Fig. 3).
Longitudinal survey of autonomy during toothbrushing. The 25 steps of toothbrushing are described with the different scores detailed in “Methods”. a Evaluation at T1 (4 months after the beginning of the experiment); b Evaluation at T2 (8 months after the beginning of the experiment)
If we consider the different tooth surfaces, brushing was not performed for the occlusal surfaces in 6% of the sample at T0 and 0% at T4, the buccal surfaces in 10% at T0 and 0% at T4, the buccal surfaces 31% at T0 and 0% at T4. The preparatory steps were performed well from T0 to T4. The children’s success in performing the ending steps varied, mostly due to failure of the spitting step.
Toothbrushing was considered achieved when the child had a score of 5 in all 25 steps. No child performed all the steps alone at the beginning of the programme. After 4 months, 7.7% (4 children) were successful and at the end of the training programme, 19% (10 children) were successful.
Statistical analyses
The results showed an increase in all of the means of the variables (SPrep, SOcc, SBuc, SLing, SEnd, SAut) and a decrease in the standard deviations (Table 1). Over time, scores improved and became more homogeneous. However, the means of SBucand SLing were lower compared to the other variables (SPrep, SEnd and SAut).
This positive evolution was statistically significant as shown by the results of the Wilcoxon test. Toothbrushing was performed better and more autonomy was observed. This significant increase in autonomy was seen between each evaluation and in each variable, except in T1 versus T2 for SEnd (Table 2).
Statistical analyses also demonstrated that all the steps were correlated, as shown by the results of the Bravais Pearson test. The preparatory and ending steps were more easily implemented than brushing all the tooth surfaces. Brushing the occlusal surfaces was easier than brushing the buccal or lingual surfaces (Table 3).
Discussion
Individuals with ASD are impaired in social interaction and communication and have repetitive, restricted, and stereotyped behaviour patterns and interests. Early diagnosis and effective interventions through structured programmes and educational methods result in significant progress for people with ASD. The present study training programme was based on a behavioural approach and visual pedagogy mediated by a digital tool. Both of these techniques have shown their effectiveness for training children with ASD to learn new skills (Bishop et al. 2013; Kagohara et al. 2013; Knight et al. 2015). The originality of the present study consists of the combined use of these three different strategies for teaching toothbrushing behaviours.
The çATED application was chosen to implement the training programme. It is a digital diary used for organising and structuring activities for people with ASD. More broadly, it is aimed at increasing an individual’s autonomy, stimulating self-reassurance, increasing organisation, and improving space- and time-awareness for daily activities, including learning activities. The app breaks down complex tasks into simpler sub-tasks. Tasks can rapidly be created by children (and adults), by using pictograms and pictures (and/or sounds), directly inserted into the iPad®. Previous studies have shown that this app enhances communication between children with ASD and other children and adults (Mercier et al. 2016). The app provides a platform for visual pedagogy. The use of a visual activity schedule (VAS) is helpful for people with ASD, as previously described by Koyama and Wang (2011). These authors explained that VAS allows for behavioural changes, reduces prompt-dependency, maintenance, and generalisation, and presents social validity. The çATED app also takes part in behavioural support, as the use of an iPad® is attractive for children with ASD and can be considered positive reinforcement. The iPad® was used with the hypothesis that it would increase children’s motivation for learning, and, more specifically in people with autism, ease their difficulties with social communication.
Fifty-five children and adolescents were enrolled, and data from 52 children and adolescents were analysed in this study. The present study sample, which was elaborated without a probability sampling technique (i.e., individuals were not randomly selected) can be considered as a convenience sample. However, the following inclusion criteria were used: clinical diagnosis of ASD, educated in one of the educational institutions that were participating in the study, and written consent from the child’s parents. The study sample included 7 girls and 45 boys, which is representative of the gender ratio of ASD. The sample was also representative of ASD because it included children with mild to severe autism.
With regard to toothbrushing technique, based on French practice, the simplest method was chosen for children under six years old (using 12 pictograms instead of 16). They were only required to brush their occlusal surfaces with a horizontal movement and were not trained or evaluated on brushing the buccal and lingual surfaces of their teeth (steps 10–21).
The present study results showed a global improvement over time in toothbrushing behaviours. Children with ASD performed better and learned the different steps involved in toothbrushing, even if some of the steps remained difficult for them to implement. The present study had similar results to a previous study that showed that training programmes were effective for improving toothbrushing behaviours and oral health in people with ASD (Pilebro and Bäckman 2005; Dias et al. 2010; Asma’a et al. 2013; Bishop et al. 2013; Popple et al. 2016). Toothbrushing is a difficult activity for children with ASD, but a training programme can desensitize them to this activity, which allows better brushing behaviours. Children showed gains in compliance and/or autonomy. The use-adapted strategy (visual pedagogy and behavioural techniques) was helpful.
Regarding the acquisition of brushing dimensions, significant differences were noticed between the means. One could argue that children need time at the beginning to better understand the expected psychomotor gestures. This hypothesis can also explain the differences observed in varying improvements in the steps for brushing the different tooth surfaces.
The differences in the means also suggest that a developmental pattern can be distinguished during the acquisition of the phases of toothbrushing autonomy. The means of the preparation steps were higher than the occlusal steps, which were higher in comparison with next dimensions. One interpretation could be that the first phases is necessary for the acquisition of the second phase, which is then necessary for the acquisition of the third phase, etc. This developmental hypothesis of toothbrushing acquisition is linked with psychomotor perspectives, in as much as the gestures required for each brushing stage seem to be distinguishable from each other. Indeed, for brushing the occlusal surfaces of the teeth, a horizontal gesture is required, whereas for brushing the buccal and lingual surfaces, vertical and rotational gestures from top to bottom are needed. In the literature, we have not found studies supporting or rejecting these hypotheses. However, this developmental approach has been described by Campbell and Richie (1983) in the field of cognitive development, and they posit that first steps are required for acquisition of more complex steps that follow. The first step (for instance, acquisition of a horizontal gesture) can be considered a prerequisite for the acquisition of the second step (for instance, vertical and rotational gestures).
Another hypothesis, based on cognitive publications, highlights the fact that attention and concentration decrease during the session, therefore, children are less successful in the end stages of the experiment compared with the beginning stages (Ash 1946). This hypothesis cannot be studied through the present study results, however, due to the limitations of the research protocol in which the different stages were not balanced (i.e., first brush the buccal surfaces, then the occlusal, etc.). Additional research, taking this limitation into account, would help in generating a developmental hypothesis and/or a hypothesis regarding cognitive attention.
Another hypothesis is that the steps for brushing the tooth surfaces are more difficult to accomplish due to the particular sensory profile of people with ASD. During this step, the toothbrush must be introduced into the mouth and this can be an aggressive movement for children with ASD. The sensation of the brush touching the mouth and lips and the presence of toothpaste can be difficult for some. The sensitivities of children with ASD are well documented and often include hyper-responsive sensory patterns (Baranek et al. 2007; Stein et al. 2013). This may explain the remaining difficulties that the present cohort experienced. The use of stimulus-fading procedures for those with major difficulties could also be helpful (Bishop et al. 2013).
Finally, the present study highlights that the acquisition of toothbrushing needs to be further assessed through additional research. More comprehensive research with typical children, for example, may confirm the present study hypothesis and the results and may allow modelling a more general pattern for the acquisition of toothbrushing behaviours in children with or without ASD. Age and severity of ASD can also influence the process of learning toothbrushing behaviours, and must also be investigated.
Conclusion
Use of the çATED application on an iPad®, within a training programme, enabled improvement in the oral health of the study cohort of patients. Toothbrushing, as a preventive measure for oral healthcare, was performed better, with improved compliance and autonomy.
The positive results of the present research supports establishing early prevention programmes for toothbrushing support for children with ADS, in collaboration with healthcare and education professionals and using adapted and specific strategies. The iPad® is an attractive and simple tool which enables setting up and using visual pedagogy for patients with ASD. It can easily be used with various training programmes for acquisition of new skills in a dental context.
References
American Academy of Pediatric Dentistry. Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent. 2013;35:E157–64.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn. Washington: American Psychiatric Publishing; 2013.
Ash ES. Forming Impressions of Personality. J Abnorm Soc Psychol. 1946;41:258–90.
Asma’a MS, Badr SB, Rashed MA. Effectiveness of audiovisual modeling on the behavioral change toward oral and dental care in children with autism. Indian J Dent. 2013;4:184–90.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191.
Baranek GT, Boyd BA, Poe MD, et al. Hyperresponsive sensory patterns in young children with autism, developmental delay, and typical development. Am J Ment Retard. 2007;112:233–45.
Baron-Cohen S, Ashwin E, Ashwin C, et al. Talent in autism: hyper-systemising, hyper-attention to detail and sensory hypersensitivity. Philos Trans R Soc Lond B Biol Sci. 2009;364:1377–83.
Bishop MR, Kenzer AL, Coffman CM, et al. Using stimulus fading without escape extinction to increase compliance with toothbrushing in children with autism. Res Autism Spec Disord. 2013;7:680–6.
Brickhouse TH, Farrington FH, Best AM, Ellsworth CW. Barriers to dental care for children in Virginia with autism spectrum disorders. J Dent Child (Chic). 2009;76:188–93.
Campbell RL, Richie DM. Problems in the theory of developmental sequences. Hum Dev. 1983;26:156–72.
Delli K, Reichart PA, Bornstein MM, Livas C. Management of children with autism spectrum disorder in the dental setting: concerns, behavioural approaches and recommendations. Med Oral Patol Oral Cir Bucal. 2013;18:e862.
Dias GG, Prado EF, Vadasz E, Siqueira JTT. Evaluation of the efficacy of a dental plaque control program in autistic patients. J Autism Dev Disord. 2010;40:704–8.
Gandhi RP, Klein U. Autism spectrum disorders: an update on oral health management. J Evid Based Dent Pract. 2014;14:115–26.
Hernandez P, Ikkanda Z. Applied behavior analysis: behavior management of children with autism spectrum disorders in dental environments. J Am Dent Assoc. 2011;142:281–7.
Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011;19:212–7.
Kagohara DM, van der Meer L, Ramdoss, et al. Using iPods® and iPads® in teaching programs for individuals with developmental disabilities: a systematic review. Res Dev Disabil. 2013;34:147–56.
Kemp F. Alternatives: a review of non-pharmacologic approaches to increasing the cooperation of patients with special needs to inherently unpleasant dental procedures. Behav Anal Today. 2005;6:88.
Knight V, Sartini E, Spriggs AD. Evaluating visual activity schedules as evidence-based practice for individuals with autism spectrum disorders. J Autism Dev Disord. 2015;45:157–78.
Koyama T, Wang HT. Use of activity schedule to promote independent performance of individuals with autism and other intellectual disabilities: a review. Res Dev Disabil. 2011;32:2235–42.
Lai B, Milano M, Roberts MW, Hooper SR. Unmet dental needs and barriers to dental care among children with autism spectrum disorders. J Autism Dev Disord. 2012;42:1294–303.
Lewis C, Vigo L, Novak L, Klein EJ. Listening to parents: a qualitative look at the dental and oral care experiences of children with autism spectrum disorder. Pediatr Dent. 2015;37:98E–104E.
Loo CY, Graham RM, Hughes CV. Behaviour guidance in dental treatment of patients with autism spectrum disorder. Int J Paediatr Dent. 2009;19:390–8.
Marshall J, Sheller B, Mancl L. Caries-risk assessment and caries status of children with autism. Pediatr Dent. 2010;32:69–75.
Mercier C, Bourdon P, Bourdet JF. The time of the child with autism and the time of the professional: adopt the rhythm of the learner in order to facilitate the access to new learning. Distances et médiations des savoirs. Distance Mediat Knowl. 2016;16. (French).
Nelson TM, Sheller B, Friedman CS, et al. Educational and therapeutic behavioral approaches to providing dental care for patients with autism spectrum disorder. Spec Care Dent. 2015;35:105–13.
Pilebro C, Bäckman B. Teaching oral hygiene to children with autism. Int J Paediatr Dent. 2005;15:1–9.
Popple B, Wall C, Flink L, et al. Brief report: remotely delivered video modeling for improving oral hygiene in children with ASD: a pilot study. J Autism Dev Disord. 2016;46:2791–6.
Stein LI, Polido JC, Najera SOL, Cermak SA. Oral care experiences and challenges in children with autism spectrum disorders. Pediat Dent. 2012;34:387–91.
Stein LI, Polido JC, Cermak SA. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent. 2013;35:230–5.
Udhya J, Varadharaja MM, Parthiban J. Autism disorder (AD): an updated review for paediatric dentists. J Clin Diagn Res. 2014;8:275.
Weil TN, Inglehart MR. Three-to 21-year-old patients with autism spectrum disorders: parents’ perceptions of severity of symptoms, oral health and oral health-related behavior. Pediatr Dent. 2012;34:473–9.
Acknowledgements
This study was supported by grants from the International Foundation of Applied Disability Research (FIRAH). We would like to express our gratitude to the çATED-autisme team. The authors would like to thank children, parents and professionals who participated to the “çATED pour tes dents” programme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this study, written informed consent was obtained from all parents of children and adolescents included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lopez Cazaux, S., Lefer, G., Rouches, A. et al. Toothbrushing training programme using an iPad® for children and adolescents with autism. Eur Arch Paediatr Dent 20, 277–284 (2019). https://doi.org/10.1007/s40368-018-0396-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-018-0396-y